
1
Lectures In community
Medicine
(LEC4,5,6)
4th Stage
BY:
DR Zaid
October 2015
2
4th stage
طب مجتمع
Lec-4
د.زيد
28/10/2015
Tetanus
Tetanus is an acute disease induced by an exotoxin of the tetanus
bacillus, which grows anaerobically at the site of an injury.
*Characterized by :
1.Painful muscular contractions
Masseter and neck Trunk
muscles muscles
*It can cause abdominal rigidity
2.Generlized spasms frequently induced by
sensory stimuli.
3.Typical features are position of opisthotonus
and risus sardonicus expression.
*Case fatality rate is 10–90% according to: Age
(high among infants and elderly), Incubation
period, and Availability of experienced intensive
care.
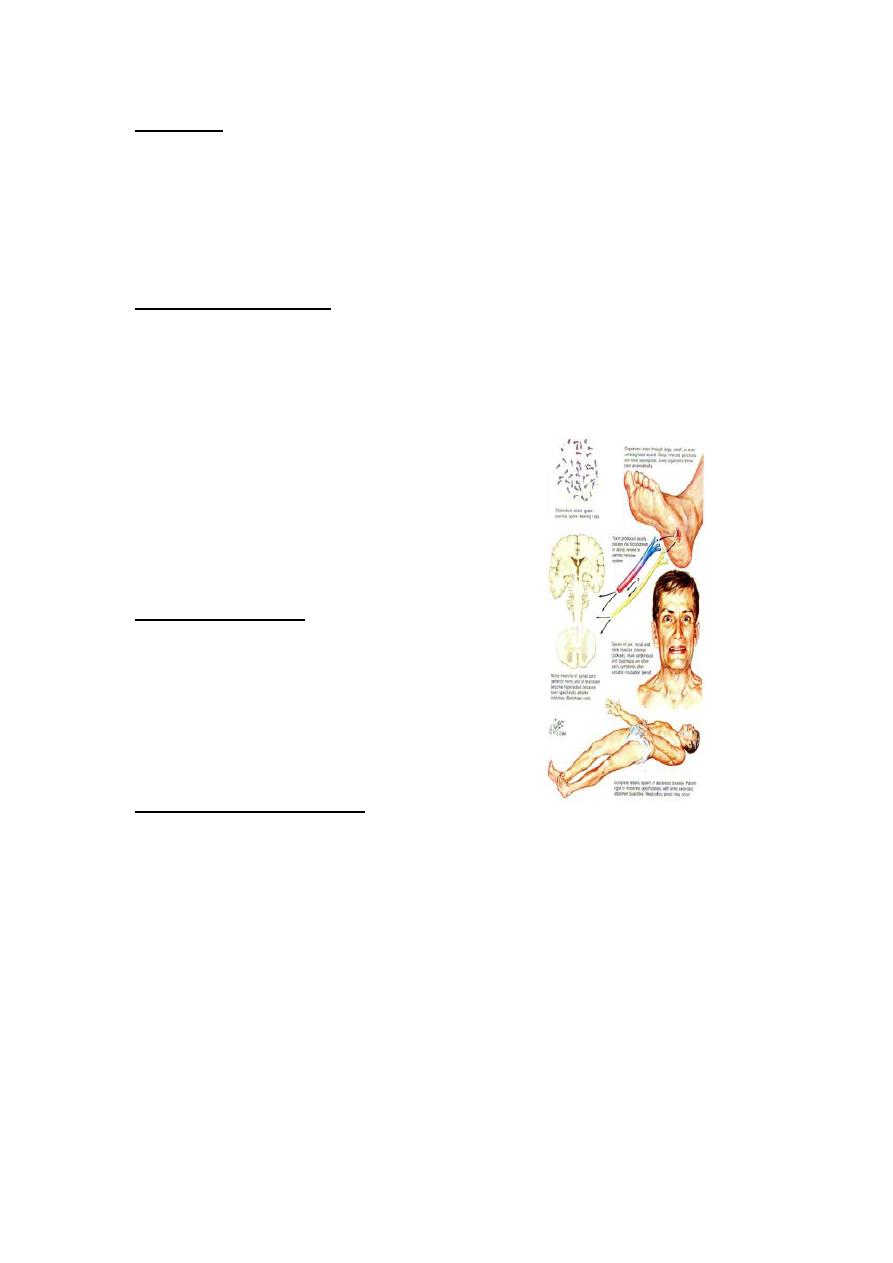
*Infections agent: Clostridium Tetani.
Occurrence :
*World wide sporadic disease.
*More common in agriculture regions and underdeveloped areas.
*Addiction on parental drugs can result in individual cases.
3
Reservoir:
1-Intestine of horses and other animals.
2-humans(the MO is normal harmless inhabitant).
3-Soil contaminated with animal and human feces.
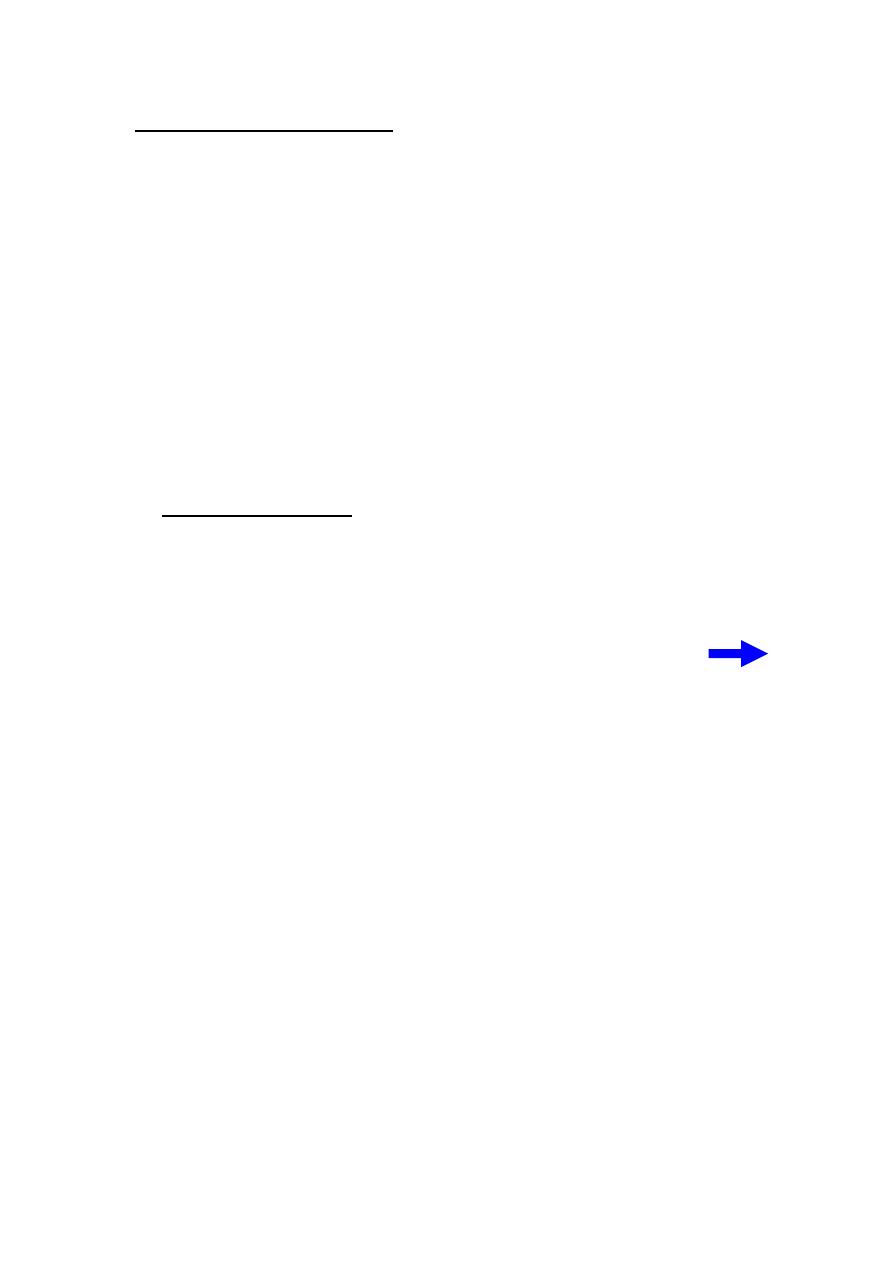
Mode of transmission:
1.Tetanus spores usually introduced through contaminated wound,
puncture or through lacerations ,burns, and trivial or unnoticed wounds.
2.Through injectable contaminated drugs.
3.Occasionaly follows surgical procedures
including circumcisions.
(Necrotic tissues favors the growth of the
pathogen)
Incubation periods:
Usually (3-21) days. However its range is (1day
–
several months) .
The shorter period means the worst
prognosis.
Period of communicability :
No person to person transmission .
4
Susceptibility and resistance :
• Susceptibility is general.
• Active immunity is by tetanus toxoid which persist for (10 years)
after full immunization.
• Transient passive immunity by tetanus immunoglobulin (TIG) or
tetanus antitoxin (equine origin ).
• Infants of actively immunized mothers acquire passive immunity
against neonatal tetanus.
• Recovery from tetanus not result immunity, thus a second attack
can occur so Primary immunization after recovery is indicated.
Preventive Measures:
1.Educate public about necessity of complete immunization and risk
of puncture wounds contamination that need active or passive
prophylaxis.
2.Universal active immunization with adsorbed tetanus toxoid
protection for at least (10 years). (TT, DTP, DT)
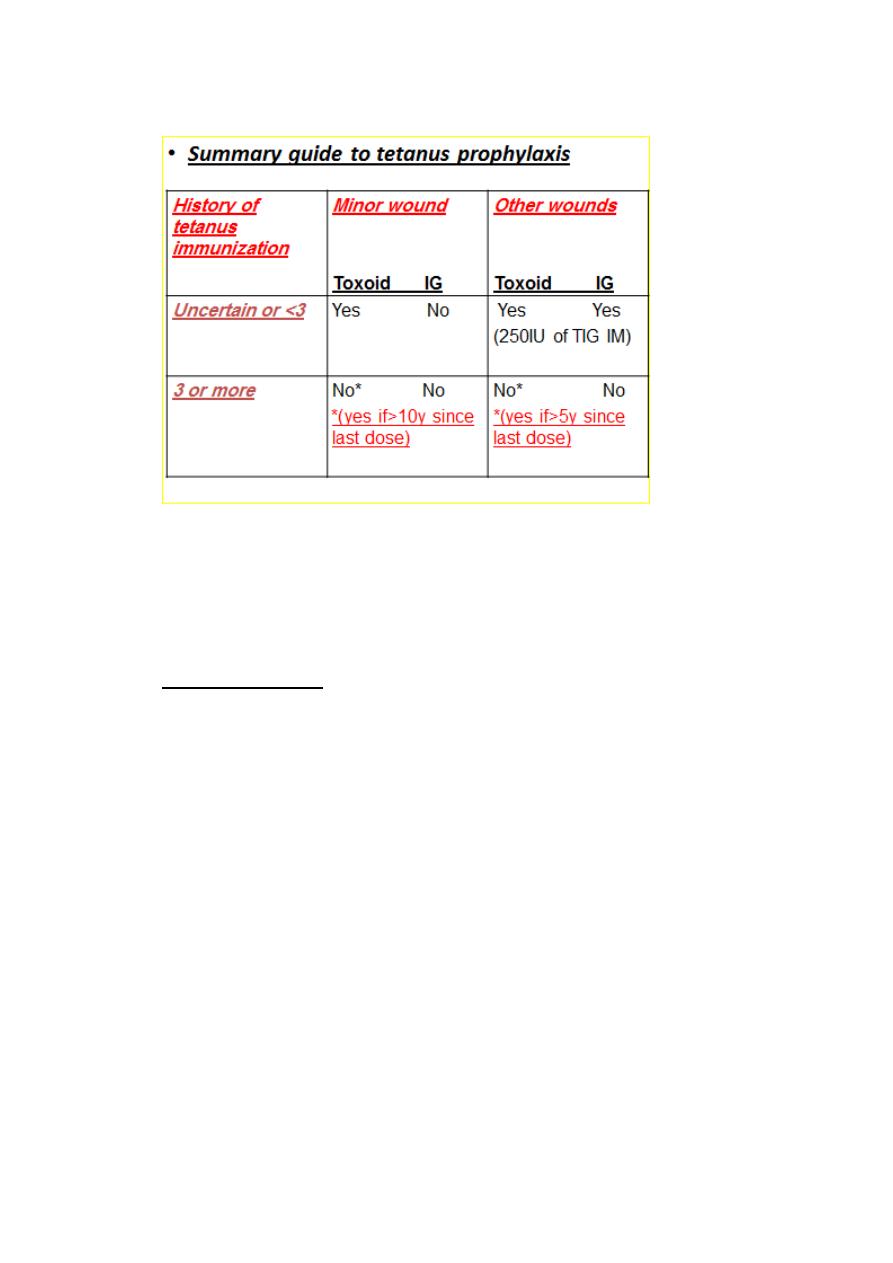
3.Prophylaxis in wound management through:-
a. Careful assessment of wound state of contamination.
b. Immunization status of patient.
c. Proper use of tetanus toxiod and /or tetanus immunoglobulin .
d. Wound cleaning.
e. Surgical debridement and antibiotics use.
5
• If both Tetanus toxoid and immunoglobulin are indicated,
they must be given:
concurrently, at different sites, and separate syringes must be used.
Control Measures:
1.Report to local health authority.
2.Investigation of contacts and source of infection (case investigation
to determine circumstances of injury).
3.Specific treatment:-
a. TIG (3000-6000IU) intramuscularly.( if not available give tetanus
antitoxin equine origin in single large dose I.V.
b. I.V. metronidazole large doses for (7-14) days.
c. Wound debridment if possible
d. Maintain adequate airway and give sedation.
e. Muscle relaxant drugs with tracheotomy or nasotracheal
intubation and mechanical respiration may be life saving .

6
f. Active immunization should be initiated.
Anthrax
It is an acute bacterial disease that usually affects skin but may very
rarely involve oropharynx, mediastinum, or intestinal tract.
A/Cutaneous Anthrax
Presented with itching of an exposed skin followed
by papular then vesicular lesion which within (2-
6)days proceed into a depressed black Escher with
extensive edema. usually it is painless.
B/Inhalation Anthrax
Presented initially with mild nonspecific symptoms (flulike) followed
by acute symptoms of respiratory distress with x-ray evidence of
mediastinal widening, fever and shock within (3-5)days with death
shortly thereafter.
7
C/Intestinal Anthrax
It is rare and difficult to recognize. Abdominal distress followed by
fever, signs of septicemia and death.
*Infectious agent: Bacillus Anthracis
(gram positive, encapsulate, spore forming non motile rods).
Occurrence :
Human is an incidental host.
Sporadic infrequent human infections in most industrialized
countries.
Endemic in agricultural regions.
*It is an occupational hazards primarily of :-
1.Workers with animal hair, bone, and wool processing.
2.Veterinarians and agriculture and wild life workers.
Reservoir:
Animals shed bacilli in terminal hemorrhages or blood at death.
On exposure to air, vegetative cells sporulate, the spores are
resistant to adverse environmental conditions and disinfections.
It may remain viable in soil for many years.

8
Mode of transmission :
*Cutaneous infection is by :
1.Contact with tissues of animals dying of the disease .Possibly by fly
bite.
2.Contact with hair, and wool or products.
3.Contact with contaminated soil .
*Inhalational type through inhalation of spores in risky industrial
processes (wool).
*Intestinal and or pharyngeal is through ingestion of undercooked
contaminated meat.
Incubation period :
(1-7) days ( may be up to 60 days).
Period of communicability :
Person to person transmission is very rare.
Articles and soil contaminated with spores may remain infective for
decades.
Susceptibility and resistance:
Uncertain ,there is some evidence of inapparant infection among
people in frequent contact with infectious agent.
Second attack can occur but rare.

9
Preventive Measures :
1.Immunize high risk persons with a cell –free vaccine containing
protective antigen.
2.Eduacte employees about mode of transmission, care of skin
abrasions and personal cleanliness.
3.Control dust and properly ventilate work areas.
4.Thoroughly wash, disinfect or sterilize hair, wool, and bone meal.
5.If anthrax is suspected in animals aseptically collect blood sample
for culture then autoclave, incinerate, or chemical disinfection of all
instruments or materials used.
6.Prompthly immunize and annually re immunize all animals at risk.
Control Measures :
1.Report to locate health authority .Obligatory case report.
2.Isolation .Standard precautious for the duration of illness.
3.Concurrent disinfection of discharges from lesions and articles.
4.Investigation of contacts and source of infection.
5.Specific treatment.
Penicillin is drug of choice for (5-7) days .
Alternatives are tetracycline, erythromycin, chloramphenicol, and
ciprofloxacin.
11
4th stage
طب مجتمع
Lec-5
د.زيد
28/10/2015
Rabies
Fatal acute viral encephalomyelitis
Characterized by Sense of apprehension, headache ,fever, malaise
&indefinite sensory changes referred to the site of preceding
animal bite. Excitability &aerophobia are frequent symptoms.
Spasm of swallowing muscles leads to fear of water (hydro
phobia)
Delirium &convulsions follow
The usual duration is 2-6 days
Death due to respiratory paralysis
Infectious agent:-
Rabies virus (Rhabdovirus).
Occurrence:-
World wide with an estimated 35.000-40,000 deaths/ year almost
in developing countries
It is a disease primarily of animals
The only areas currently free of rabies in the animal population
include:
لالطالعAustralians, Newzeland, New guniea, Japan, Hawaii ,Taiwan , Uk,
Iceland , Norway, Sweden , Finland, Portugal, Greece , west Indies
&Atlantic islands.
11
Reservoir:
Many wild &domestic canidae dogs, foxes, wolves,&
other biting animals
Infected population of bats.
Rabbits ,rats &mice are rarely infected &their bites
rarely , if ever call for rabies prophylaxis.
Mode of transmission:-
Direct by bite of rabid animal (most common)
Air borne spread in caves where millions of bats were present &in
lab. Settings
Person-to-person is theoretically possible
Organ transplants (corneal)
Incubation period :
Usually : 3 -8 weeks
Rarely :as short as 9 days or as long as 7 years
Severity of wound
Site of the wound
Strain of virus introduced
Protection provided by clothing
Prolonged I.P have occurred in prepubertal individuals
Period of communicability :
In dogs &cats usually 3-7 days before the onset of illness
&throughout the course of the disease.
12
Susceptibility & resistance:
All mammals are susceptible to varying degree which may be
influenced by virus strain
Humans are more resistant to infection
Prevention:
Prevention in animals
1. Register, license &immunize all dogs , collect &kill ownerless
animals. Immunize all cats
2. Active surveillance for rabies in animals
3. Detain and observe for 10 days any healthy appearing dogs or
cats known to have bitten a person (unwanted dogs &cats may be
killed immediately &examined for rabies by fluorescent
microscopy) (Viral antigen, Negri bodies).
Prevention in human
( Individuals at high risk)
A.. Pre-exposure prophylaxis
Human diploid cell vaccine (HDCV) in inactivated vaccine grown on
human diploid cell culture
Rabies vaccine adsorbed (RVA)
Purified check embryo cell vaccine (PCEC) an inactivated grown in
primary cultures of chicken fibroblasts
Each vaccine 3 doses 1ml IM on days 0,7 & 21 or 28
If risk of exposure continues , either booster doses are given or
serum is tested for neutralizing antibodies every 2 years
13
B.. Prevention of rabies after animal bites (post exposure prophylaxis)
consist of the following:
a. Treatment of bite wound:
Clean &flush the wound immediately
Thorough wound cleaning under medical supervision
No suture or wound closure advised unless unavoidable
Rabies immune globulin &/or vaccine as indicated
Tetanus prophylaxis &antibacterial Rx when required
b. specific immunologic protection
10 IU( wounds)+ 10 IU (IM)
of human rabies immune globulin (HRIG)
OR
20 IU (wound)+ 20 IU (IM)
purified equine immune globulin (ERIG)
modern cell culture vaccines given
FIVE IM doses in the deltoid region
0,3,7,14 &28 days after the first dose
• If the person has had previous full course immunization Or
developed neutralizing antibodies After pre exposure
immunization Or after post exposure regimen only 2 doses
need (0,3)
• with severe exposure a third dose may be given on day 7 . HRIG
is not used with this regimen
14
control:
1. Reporting :obligatory
2. Isolation: contact isolation
3. Disinfection: of saliva &articles soiled with
4. Immunization of contacts who have an open wound or exposure
to the pt’s saliva should receive anti rabies specific treatment
5. No specific Rx :intensive supportive medical care
Streptococcal disease:
Group A (Beta hemolytic)
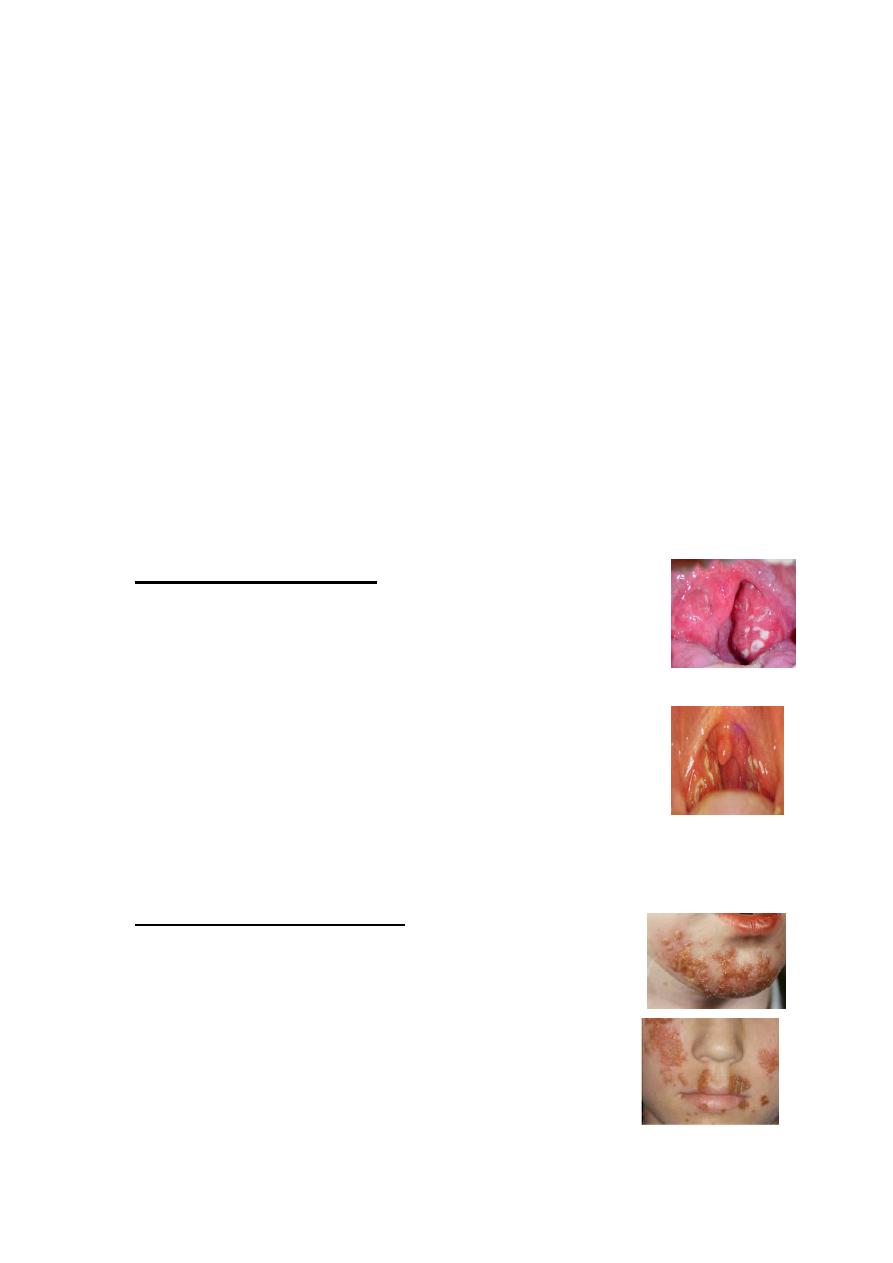
1.Strept. Sore Throat:
Presented with sudden onset fever, exudative tonsils or
pharynx, tender enlarged ant. Cervical LN, absence of cough
or rhinorrhea .
Subsequent OM or peritonsillar abscess may occur.
AGN can occur within1-5 weeks (mean 10days)
RF can occur within 3 weeks (mean 19 days)
2.Strept. Skin infection :
(pyoderma, impetigo). usually superficial may proceed to
vesicular, pustular, and encrusted stage.
RF is not an important complication, however AGN may
occur later usually 3 weeks after skin infection.

15
3.Scarlet fever :
It occurs when the infecting strain of Strept. Produces pyrogenic
exotoxine (erythrogenic toxin) & the patient is sensitized but not
immuned to the toxin.
It present with fever, nausea, vomiting, fine erythema punctate blanch
on pressure (sandpaper) sparing the face
4.Erysipelas and acute cellulites :
Red, Tender, edematous spreading lesion with definite raised border
Infection agent:
Streptococcus Pyogenes, (group A).
Of approximately 130 serologically distinct types.
Group A Strept. producing skin infection Are usually of different
serologic types from those associated with throat infection.
16
Occurrence :
Strept. sore throat &scarlet fever are common in temperate
zones.
In apparent infection is common
Strept. Sore throat is unusual <2-3 years. peak incidence in the age
group 6-12 years &declines there after .
Reservoir : Human
Mode of transmission :
Direct contact with patient or carriers
Large droplets
Indirect through contaminated articles (rare)
Nasal carriers are particularly likely to transmit diseases
Incubation period : 1-3 days
Period of communicability:
Untreated :10-21 days
Treated: 24 hours
The contagiousness of the carriers decreased sharply in 2-3 weeks after
onset of infection.
There is maternal immunity
There is tendency for repeated attack of RF with further cardiac
damage following each attack of Strept. Group A infection.
Recurrence of AGN is unusual
One attack of erysipelas predispose to subsequent attacks.
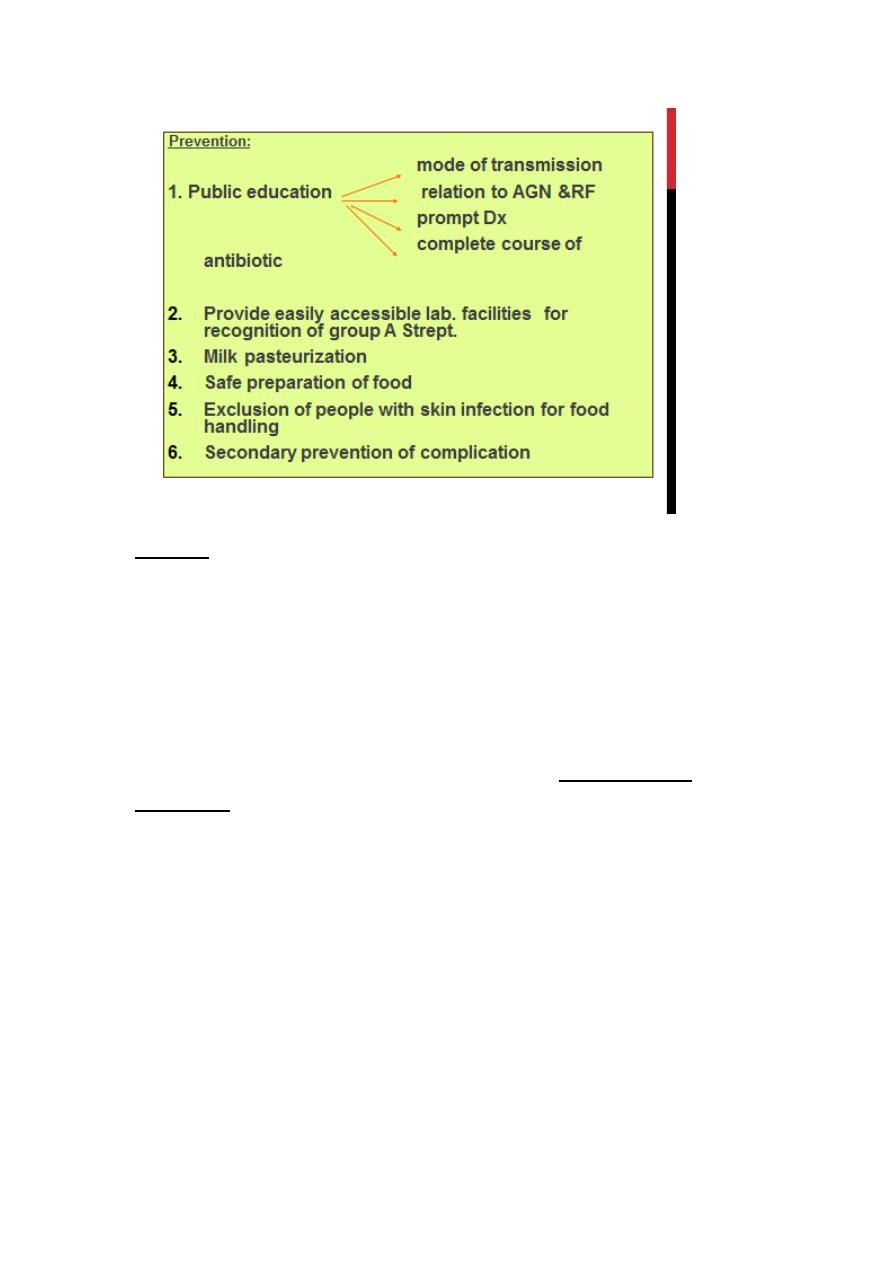
17
Control:
Reporting is not necessary except at time of epidemic.
Isolation
Disinfection of discharge
Search and treat carriers among contacts
Specific Rx penicillin is drug of choice for 10 days (oral or IM) (no
resistance) and erythromycin if there is penicillin allergy
18
4th stage
طب مجتمع
Lec-6
د.زيد
28/10/2015
Malaria
• Parasitic infectious disease with four human species that have
similar clinical symptoms to be differentiated through laboratory.
• Fever pattern during the first few days is similar to early stages of
other bacterial, viral, or parasitic illness.
*Malignant tertian or falciparum malaria is the most serious.
• Case fatality rate is (10-40 %) or higher .
*Other human malarias (Vivax, malaria, ovale) are generally not life
threatening.
Usually it presented with malaise, slowly rising fever over several
days followed by shaking, chills and rapidly rising temperature
associated with headache, nausea, and end by profuse sweating.
After an interval free of fever, the cycle of chills, fever, and sweating
is repeated either daily, every other day or every third day.
19
Occurrence:
*Endemic malaria is a major cause for ill health in many tropical and
subtropical areas.
*It causes one million deaths per year in Africa , mostly in children.
Reservoir:
*Humans are the only important reservoir of human malaria.
Mode of transmission :
A/ Congenital transmission occurs rarely.
However still birth from infected mothers is more frequent.
B/Bite of infective female anopheles mosquito.
C/Injection or transfusion of blood from infected person.
D/Use of contaminated needles and syringes.
21
Incubation period :
A/Through bite of mosquito :
(9-14) days for falciparum.
(12-14) days for vivax and ovale .
(18-40) days for malaria.
B/Through blood transfusion : usually short incubation period .
Period of communicability:
*Untreated or insufficiently treated patients are considered the main
source of mosquito infection .( many years)
*Mosquito remains infective for life.
*Stored infected blood remains infective for one month.
Susceptibility & Resistance:
*Universal susceptibility except certain specific traits.
*Tolerance to clinical disease is present among adults in highly endemic
areas.

21
Preventive Measures:
Community Based Measures :
1.Insecticide treated Mosquito nets (most useful).
2.Indoor residual spraying with insecticides.
3.Control of larval stages by elimination of mosquito breeding sites
(increasing the speed of water)
4.Intermittent preventive treatment with full curative dose of
antimalarial drug.
5.In epidemic prone area Malaria surveillance should be based on
weekly reporting.
a. Prompt and effective malaria treatment for both acute and
chronic cases.
b. Questioning blood donors carefully.
Personal Protective Measures:
1.Measures to reduce the risk of mosquito bites:
a. Avoid going out at night .
b. Using insect repellents to exposed skin.
c. Staying inside well constructed and maintained building.
d. Using screen over doors ,windows and beds.
e. Using anti mosquito sprays or insecticides dispensers.
2.Information of those at risk to mosquito exposure.
a. Risk of getting malaria is variable between countries and regions.
b. Pregnant and children are risky for sever disease.
c. It is a life threatening disease.
d. May be with mild symptoms.
22
3.Advice for pregnant and parents of young children.
Chloroquine 5mg/kg/week and proguanil 3mg/kg/day
or Mefloquine 5mg/kg/week.
4.Advice persons traveling to endemic area to prepare stand by
treatment.
5.Prophylaxis.
Control of patients, contacts, and immediate environment:
1.Report to local health authority.
2.Patient isolation in mosquito proof areas and with blood
precautions for hospitalized patients.
3.Invistigate contacts and source of infection:
a. History of previous infection or possible exposure.
b. History of needle sharing.
c. Blood donors investigation.
4.Specific treatment
a. Chloroquine 25 mg/kg over 3 days .
(15 mg/kg in 1
st
day orally, 5mg/kg in the 2
nd
and 3rd day)
b. For emergency parental quinine dihydrochloride20mg/kg. After
8 hours 10mg/kg.
8 hours later lower maintenance dose
23
Schistosomiasis (Bilharziasis)
• A blood fluke (trematode) infection with adult male and female
worms living within mesenteric or vesicle veins of the host over a
life span of many years.
I. Schistosoma haematobium –> urinary manifestation (dysuria,
urinary frequency and haematuria at the end of micturation).
II. Schistosoma mansoni and japonicum -> hepatic and intestinal
signs and symptoms (diarrhea, abdominal pain, and
hepatosplenomegally).
Diagnosis:-
1.Demonstration of eggs in urine or stool or
biopsy.
2.Immunologic tests which indicate prior
infection but not prove a current one.
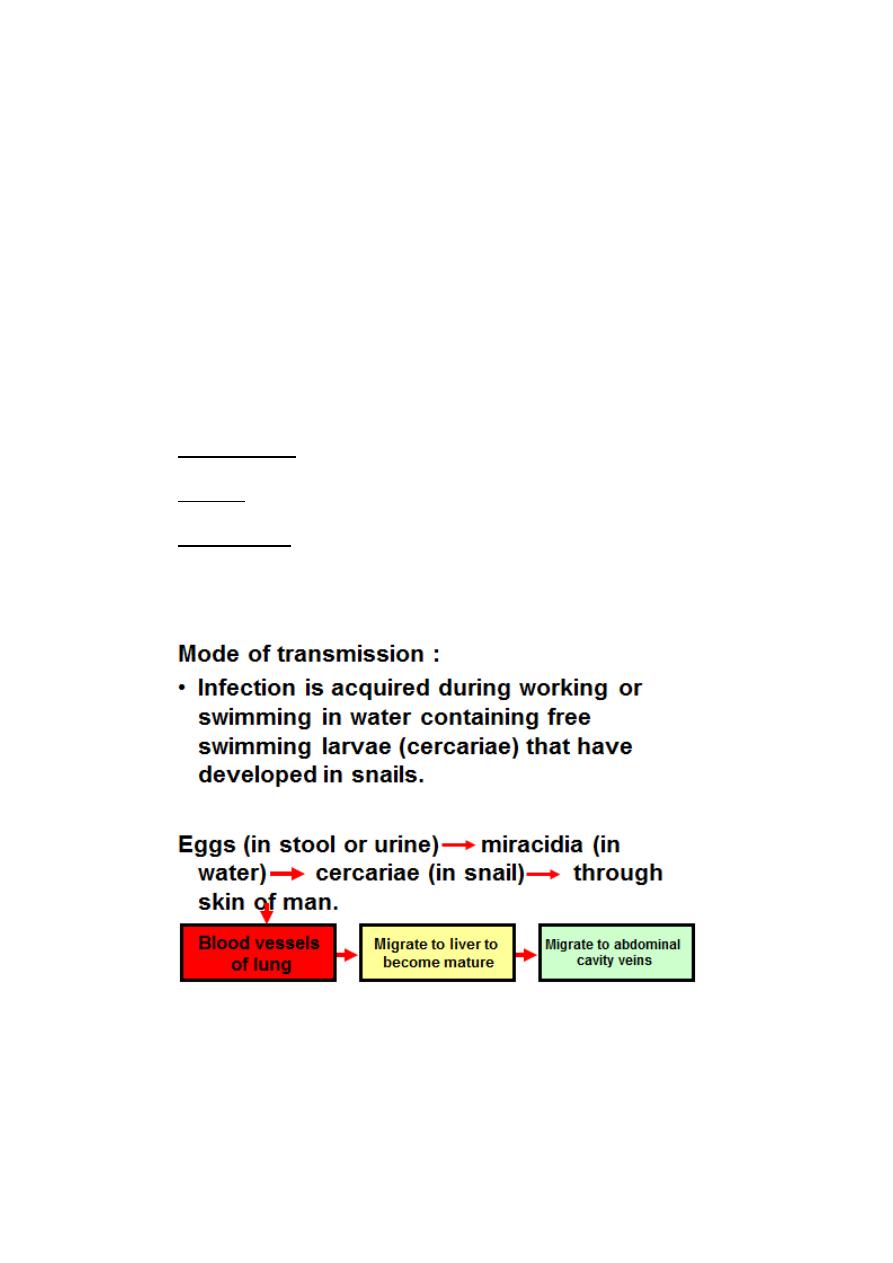
24
Reservoir:
1.Human is the principal reservoir for Schistosoma haematobium,
and mansoni.
2.Dogs, cats, cattle, horses and wild rodents are potential reservoirs
for Schistosoma japanocum.
intermediate host:
Snail species are :-
1.Biomphalaria for Schistosoma manosni.
2.Bulinus for Schistosoma haematobium .
3.Oncomelania for Schistosoma japanocum.
Incubation period :
Acute systemic manifestation may occur in primary infections (2-6)
weeks after exposure.

25
Period of communicability :
*No person to person transmission .
*Chronic schistosomiasis may spread eggs in urine and/or feces into
water for as long as 10 years.
*Infected snails release cercariae for several weeks–3 months.
Susceptibility and resistance :
Susceptibility is universal.
Preventive measures:
1.Public education in endemic areas.
2.Hygenic disposal of urine and feces.
3.Improve irrigation and agriculture practices.
4.Using molluscicides for snail breeding sites .
5.Prevent exposure to contaminated water. (Use rubber boot).
6.Safe water supply for all purposes.
7.Treating patients in endemic areas by praziquantel.
8.Advising travelers to endemic areas about risk and methods of
prevention.
