IMMUNOPATHOLOGY
Some Definitions■ Immunology is the study of our protection from foreign macromolecules or invading organisms (viruses, bacteria, protozoa or even larger parasites).
■ Immune response may develop against our own tissue (autoimmunity) or against our own tumor cells (tumor immunity).
Body Defense Mechanism
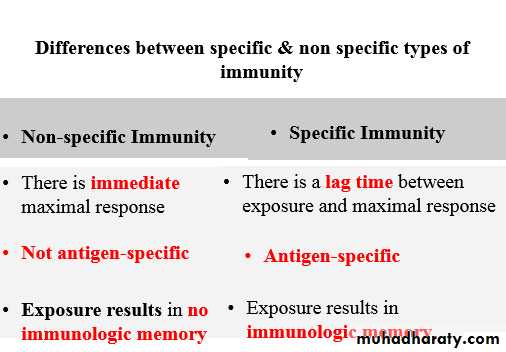
1- Nonspecific
2- Specific
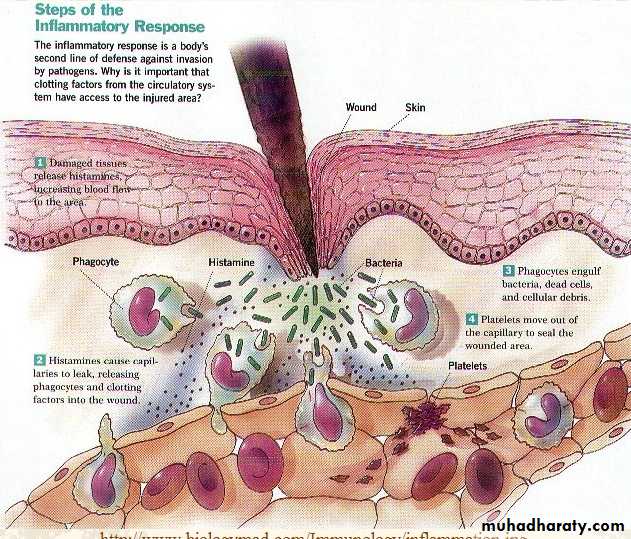
First Line Defense (Innate or non-specific immunity)
■ This form of immunity is always ready to respond to invasion.
■ The elements of the nonspecific (innate) immune system include:
Anatomical barriers (like skin, mucosa)
Secretory molecules (like mucus)
Cellular components of non specific inflammation {phagocytic cells}.
Second Line Defense Specific immune responses consist of:
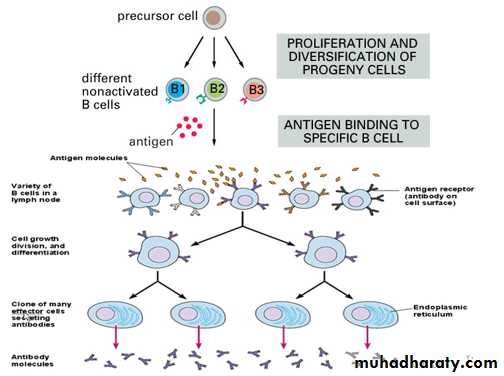
1- Recognition of antigen by specific lymphocytes
2- Activation of lymphocytes (consisting of their proliferation and differentiation into effector cells)
3- Elimination of antigen. The response declines as antigen is eliminated, and most of the antigen-stimulated lymphocytes die by apoptosis.
4- Specific immunity has a memory
(Specific immunity)
■ Specific response to the causative agent.
Characterized by:
1- Production of antibodies (soluble proteins that bind to foreign antigens) “humoral immunity”
2- Cell-mediated responses in which specific cells recognize foreign pathogens and destroy them
“ cell mediated immunity”.
Immunologic memory
The antigen-specific cells that survive are responsible for memory.
•Vaccines depend on the memory cells
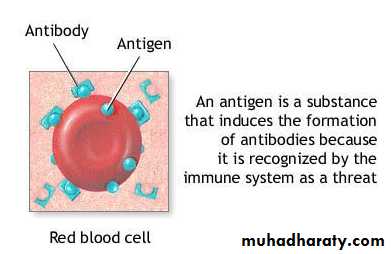
Antigen
Antibody“Immunoglobulin (Ig)”
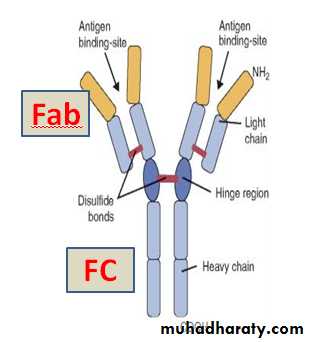
Immunoglobulins are glycoprotein molecules produced by plasma cells in response to an antigen.All immunoglobulins have 4 chain structure as their basic unit: 2 identical light chains & 2 identical heavy chains bound together by Disulfide bonds
Antigen binding site - Called the Fab. The combining site of the antibody is variable, created by both VH and VL. Different Ig molecules can have different antigen binding properties because of different VH and VL regions, & each is produced by a specific plasma cell.
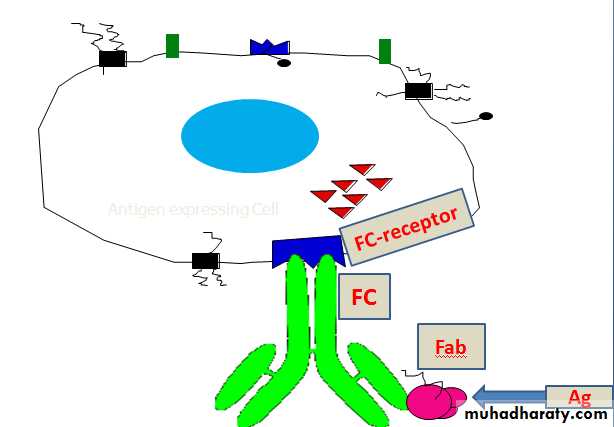
FC fragment composed of heavy chains only. The effector functions of immunoglobulins are mediated by this part of the molecule by binding to specific cells having receptors for FC portion.
Through the identification of specific cellular components, using specific monoclonal or polyclonal antibodies
through direct Ag-Ab reaction using labeled Ab.
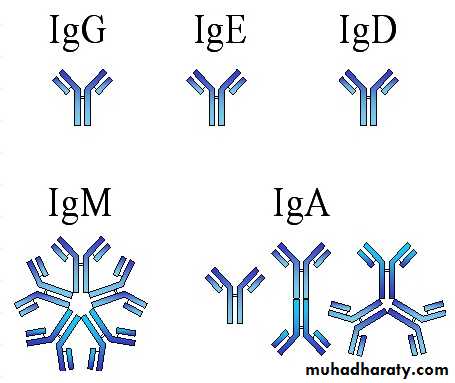
Immunoglobulin typesAccording to the heavy chain:-1. IgG - Gamma heavy chains
2. IgE - Epsilon heavy chains3. IgD - Delta heavy chains
4. IgM - Mu heavy chains
5. IgA - Alpha heavy chains
Immunoglobulin typesAccording to the light chain:-
● Other classification is according to the types of light chain into:-1. Kappa light chains
2. Lambda light chains
GENERAL FUNCTIONS OF IMMUNOGLOBULINS
1. Antigen binding. This is the primary function of antibodies and can result in protection of the host. Each Ig actually binds to a specific antigenic determinant at Fab portion.2. Fixation of complement - This results in lysis of cells and release of biologically active molecules.
3. Binding to various cell types - Phagocytic cells, lymphocytes, platelets, mast cells, and basophils have receptors to the FC portion of Ig that bind to it. This binding can activate the cells to perform some functions.
4. Some immunoglobulins also bind to receptors on placental trophoblasts, resulting in transfer of the Ig across the placenta. As a result, the transferred maternal antibodies provide immunity to the newborn.
Cells of immune system
1. T-lymphocytes
2. B- lymphocytes
3. Natural killer (NK) cells
4. Macrophages
TYPES OF SPECIFIC IMMUNITY
Humoral immunity ●● Cell mediated immunity
Humoral immunity
B-cell lymphocyte mediated via production of antibodies●
Often develops as a response to soluble antigens ●
Cellular immunityT-lymphocyte mediated immunity
● T-lymphocyte constitute 60 -70 % of peripheral lymphocytes. They are responsible for cellular immunity.
● Types of T-lymphocytes:
1- CD4+ helper lymphocytes
2- CD8+ suppressor lymphocytes: cytotoxic T-lymphocytes.
Other cells included & very important in cell mediated immunity are Macrophages
Macrophages
Function:
1- Process and present Ag to competent (specific) T-lymphocyte (so called Ag-presenting cells). This is crucial for induction of cell-mediated immunity.
2- Important as effector cells in certain forms of cell-mediated immunity such as the delayed hypersensitivity reaction.
3- Production & secretion of chemical mediators (cytokines)
4- Phagocytes microbes opsonized by IgG or C3b in innate (nonspecific) immunity.
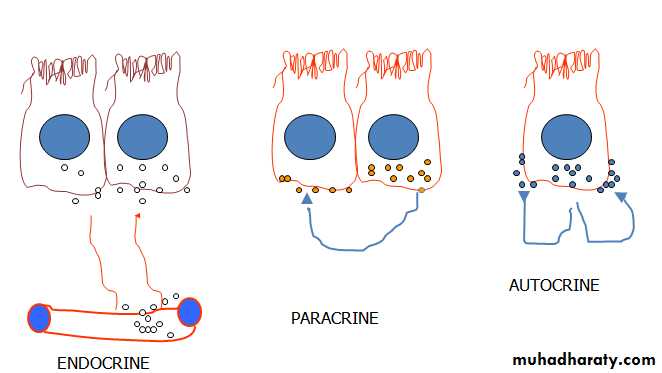
Cytokines are chemical mediators secreted from effector cells & induce their function through autocrine, parakrine & endocrine effects
Hypersensitivity reaction (HSR)
● Hypersensitivity (or allergy) is defined an exaggerated response of the immune system to an antigen.● The person must have become sensitized to the allergen by a prior exposure.
● Almost any substance capable of inducing an immune response is a potential allergen (antigen).
● Development of hypersensitivity to any particular allergen is due to a complex interaction of genetic susceptibility & exposure.
Types of HSR
The types are classified based on the mechanism by which the injury is caused.
Type I HSR (Atopic/anaphylactic reaction)●
Type II HSR (Antibody dependant cytotoxicity)●
● Type III HSR (Immune complex disease)
● Type IV HSR (Cell mediated HSR)
Type I hypersensitivity (IgE) “Atopy , immediate HSR, or anaphylactic HSR”
● Type I HSR occurs in 10-20% of the population.
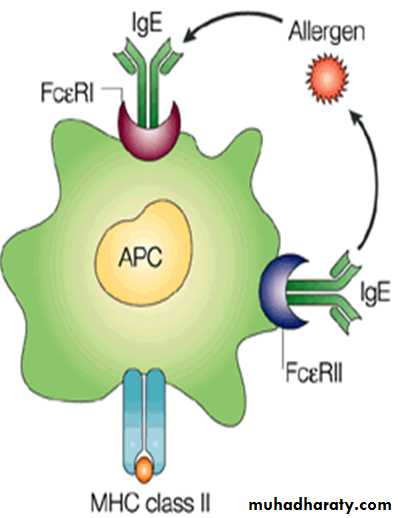
● Allergens induce the formation of antibodies of the IgE isotype. Atopic individuals thus exhibit elevated levels of serum IgE
● E.g. Bronchial asthma, hay fever, food allergies...
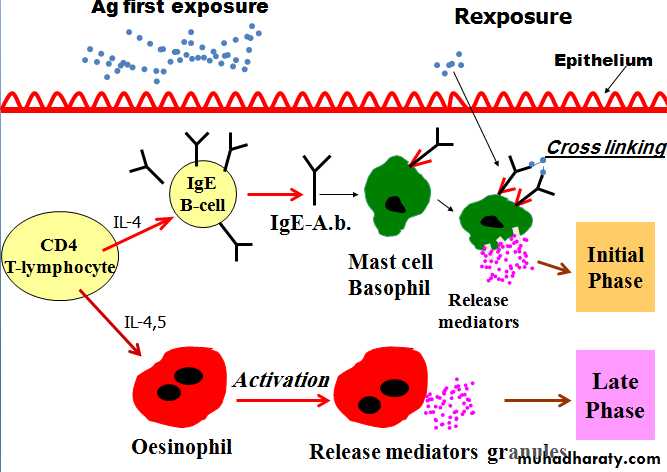
Mechanism of HSR I
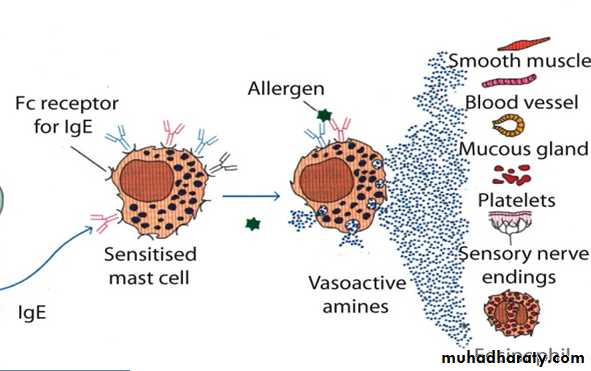
1- Sensitization: First the individual needs to be sensitized to an allergen (antigen). When the allergen enters the body for the first time it will activate CD4 T (T-helper) lymphocytes which stimulate B-lymphocytes, so initiate IgE production which bind by their FC portion to the tissue mast cells and the circulating basophils. This takes a time to develop.So in the first meeting between the allergen and the immune system, no reaction will happen.
The mast cell/Basophil is the effector cell in this response.
2- Cross linkage: On re-exposure to the allergen (it should be polyvalent antigen), it will cross link the IgE molecules on the surface of the mast cells or the basophils and this will lead to activation of the cells.
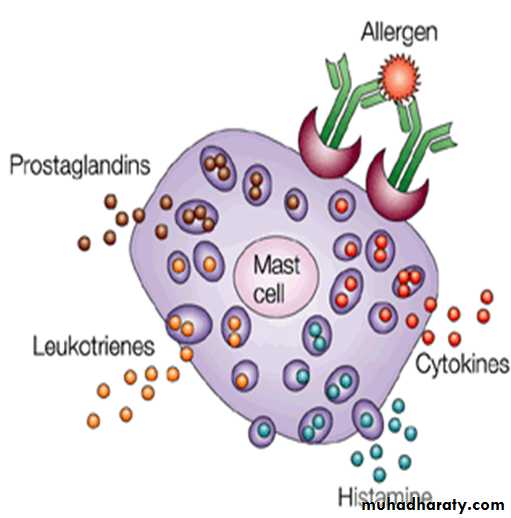
3- Degranulation: mast cells and basophils will release the contents of their granules to the exterior. These granules are mediators.
The mediators include histamine, cytokines, prostaglandins, and leukotrienes; they are responsible for the immediate features of atopy like vasodilatation, increased vascular permeability, increased glandular secretion and smooth muscle contraction.
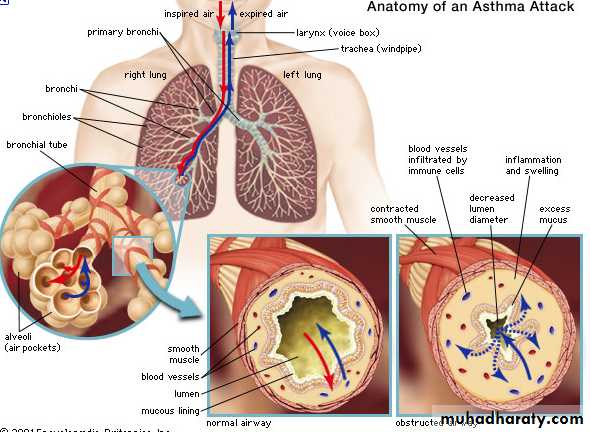
4- In some patients as those with bronchial asthma, after 2-6 hours, another set of mediators are synthesized. These together with the accumulated eosinophils are responsible for the late phase response.
Clinical Examples of Type I HSR
● The resulted reactions can be localized, i.e. affecting a single tissue or organ or systemic, i.e. affecting multiple organs or tissue (as in systemic anaphylaxis “anaphylactic shock”).● Localized type I HSR: the commonest examples are hay fever and extrinsic asthma both tend to run in families and often preceded by atopic eczema in infancy or childhood.
● Patients with hay fever develop acute inflammation of the nasal & conjunctival mucosae with sneezing and hypersecretion minutes (immediate) after exposure to the allergen like the grass pollen, food.
● Similarly, patients with bronchial asthma develop wheezes & acute respiratory distress due to bronchospasm and increased mucus secretion after exposure to house dust or animal dander.
● Systemic type I HSR: this is called anaphylactic reaction, which may result in anaphylactic shock characterized by hypotension, wide spread urticaria and dyspnea. Such shock may be seen following injection of a drug (like penicillin) to a sensitive patient and constitutes a medical emergency, which may be fatal.
End