
Diuretic Drugs

Diuretic Drugs
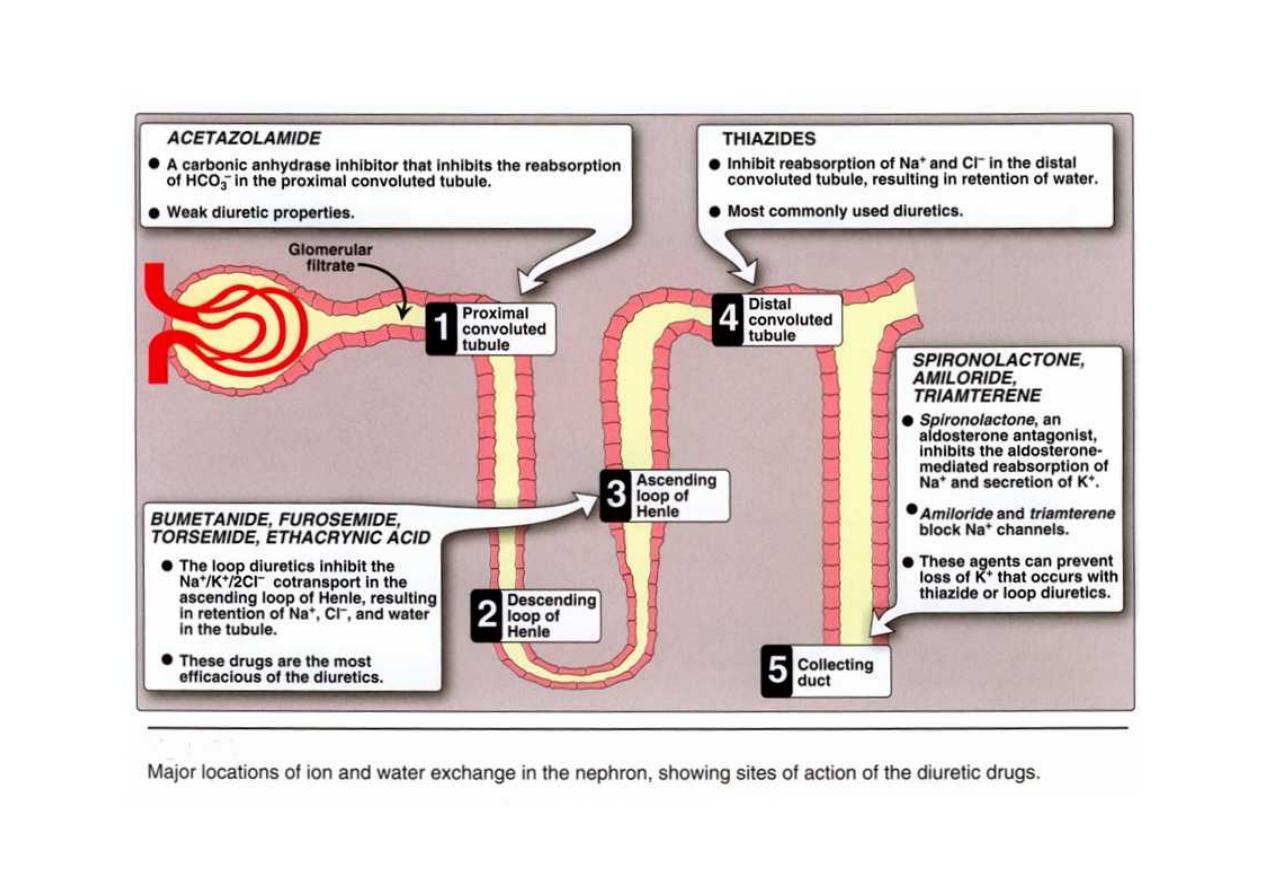
1. Thiazide Diuretics
2. Loop Diuretics
3. Potassium-Sparing Diuretics
4. Carbonic Anhydrase Inhibitors
5. Osmotic Diuretics
2
Diuretic Drugs
1. Thiazide Diuretics
2. Loop Diuretics
3. Potassium-Sparing Diuretics
4. Carbonic Anhydrase Inhibitors
5. Osmotic Diuretics
3

Carbonic Anhydrase Inhibitors
Acetazolamide
Inhibits the enzyme carbonic anhydrase in the
proximal tubular epithelial cells.
Carbonic anhydrase inhibitors used for other
pharmacologic actions rather than for diuretic
effect(less efficacious than the thiazides or loop
diuretics)
4
Carbonic Anhydrase Inhibitors
Acetazolamide
Inhibits the enzyme carbonic anhydrase in the
proximal tubular epithelial cells.
Carbonic anhydrase inhibitors used for other
pharmacologic actions rather than for diuretic
effect(less efficacious than the thiazides or loop
diuretics)

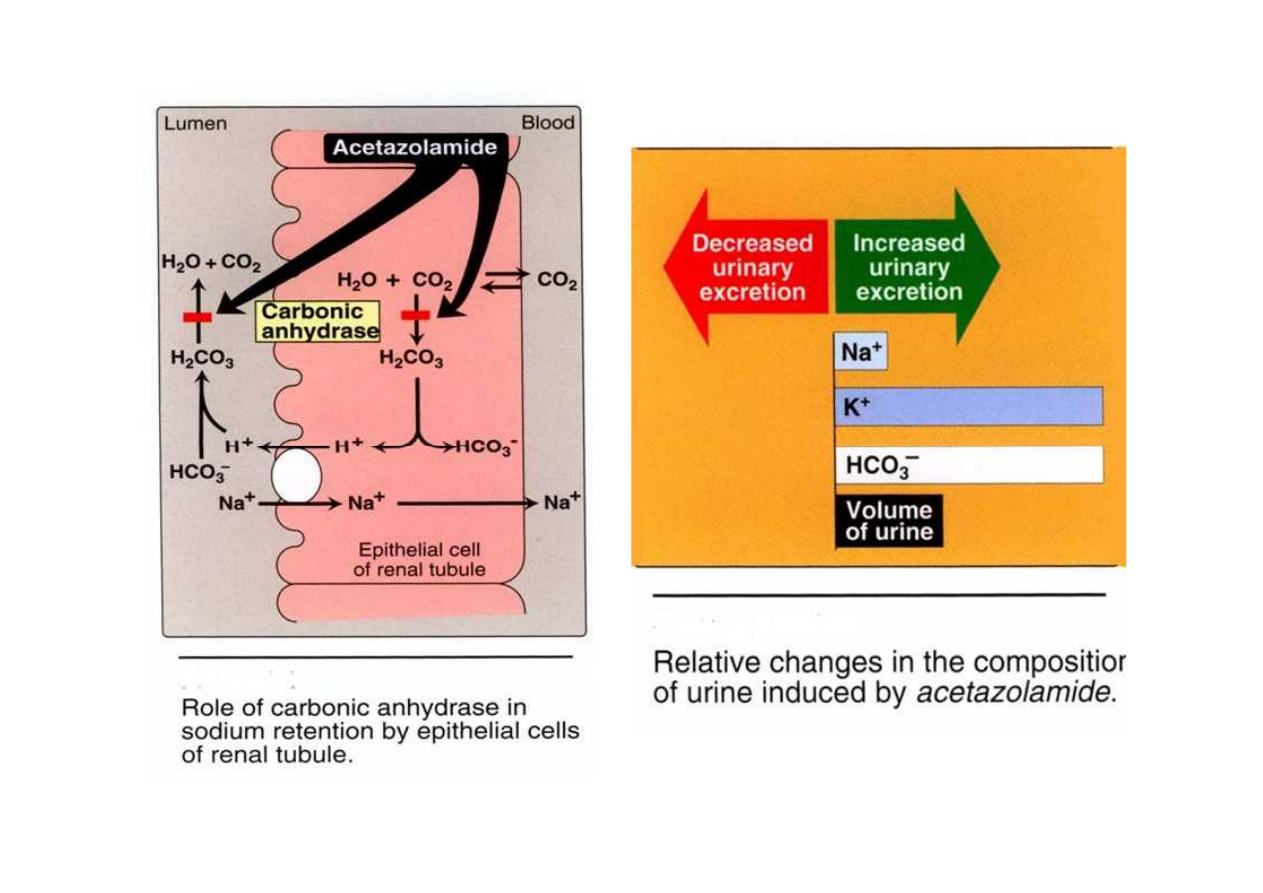
Acetazolamide
Mechanism of action:
Acetazolamide inhibits carbonic anhydrase located
intracellularly (cytoplasm) and on the apical
membrane of the proximal tubular epithelium.
Carbonic anhydrase catalyzes the reaction of CO2
(carbon dioxide) and H2O, leading to H2CO3
(carbonic acid). which spontaneously ionizes to H
+
and HCO3
-
(bicarbonate).
5
Acetazolamide
Mechanism of action:
Acetazolamide inhibits carbonic anhydrase located
intracellularly (cytoplasm) and on the apical
membrane of the proximal tubular epithelium.
Carbonic anhydrase catalyzes the reaction of CO2
(carbon dioxide) and H2O, leading to H2CO3
(carbonic acid). which spontaneously ionizes to H
+
and HCO3
-
(bicarbonate).

•
The decreased ability to exchange Na+ for H+
in the presence of acetazolamide results in a
mild diuresis. Additionally, HCO3
-
is retained
in the lumen, with marked elevation in
urinary pH.
6
•
The decreased ability to exchange Na+ for H+
in the presence of acetazolamide results in a
mild diuresis. Additionally, HCO3
-
is retained
in the lumen, with marked elevation in
urinary pH.
•
The loss of HCO3- causes a hyperchloremic
metabolic acidosis and decreased diuretic
efficacy following several days of therapy.
Therapeutic uses
1. Treatment of glaucoma (decreases the
production of aqueous humor by blocking
carbonic anhydrase in the ciliary body of the
eye ,this lead to reducing elevated
intraocular pressure).
2. Mountain sickness
7
•
The loss of HCO3- causes a hyperchloremic
metabolic acidosis and decreased diuretic
efficacy following several days of therapy.
Therapeutic uses
1. Treatment of glaucoma (decreases the
production of aqueous humor by blocking
carbonic anhydrase in the ciliary body of the
eye ,this lead to reducing elevated
intraocular pressure).
2. Mountain sickness
8

Treatment of glaucoma:
•
Acetazolamide decreases the production of
aqueous humor, probably by blocking
carbonic anhydrase in the ciliary body of the
eye (reducing elevated intraocular pressure).
9

•
It is useful in the chronic treatment of
glaucoma but should not be used for an acute
attack; pilocarpine is preferred for an acute
attack because of its immediate action. Topical
carbonic anhydrase inhibitors, such as
dorzolamide and brinzolamide, have the
advantage of not causing any systemic effects.
10
•
It is useful in the chronic treatment of
glaucoma but should not be used for an acute
attack; pilocarpine is preferred for an acute
attack because of its immediate action. Topical
carbonic anhydrase inhibitors, such as
dorzolamide and brinzolamide, have the
advantage of not causing any systemic effects.

Pharmacokinetics:
Acetazolamide is given orally once a day.
Adverse effects
1. Metabolic acidosis (mild)
2. Potassium depletion
3. Renal stone formation
4. Drowsiness
5. Paresthesia
6. The drug should be avoided in patients with
hepatic cirrhosis, because it could lead to a
decreased excretion of NH4 +.
11
Pharmacokinetics:
Acetazolamide is given orally once a day.
Adverse effects
1. Metabolic acidosis (mild)
2. Potassium depletion
3. Renal stone formation
4. Drowsiness
5. Paresthesia
6. The drug should be avoided in patients with
hepatic cirrhosis, because it could lead to a
decreased excretion of NH4 +.

Loop or High-Ceiling Diuretics
•
Bumetanide
•
Furosemide
•
Torsemide,
•
Ethacrynic acid
•
They have their major action on the
ascending limb of loop of Henle.
•
These drugs have highest efficacy in
mobilizing Na+ and CI- from the body. They
produce copious amounts of urine.
12
Loop or High-Ceiling Diuretics
•
Bumetanide
•
Furosemide
•
Torsemide,
•
Ethacrynic acid
•
They have their major action on the
ascending limb of loop of Henle.
•
These drugs have highest efficacy in
mobilizing Na+ and CI- from the body. They
produce copious amounts of urine.

•
Furosemide is the most commonly used of
these drugs.
•
Ethacrynic acid it shows greater side effects
than those seen with the other loop diuretics,
and its use is therefore limited.
•
Bumetanide is much more potent than
furosemide, and its use is increasing.
13
•
Furosemide is the most commonly used of
these drugs.
•
Ethacrynic acid it shows greater side effects
than those seen with the other loop diuretics,
and its use is therefore limited.
•
Bumetanide is much more potent than
furosemide, and its use is increasing.

Mechanism of action:
1. Loop diuretics inhibit cotransport of
Na+/K+/2CI- in luminal membrane in
ascending limb of loop of Henle. Therefore,
reabsorption of these ions is decreased.
2. The loop diuretics are the most efficacious
of the diuretic drugs
Mechanism of action:
1. Loop diuretics inhibit cotransport of
Na+/K+/2CI- in luminal membrane in
ascending limb of loop of Henle. Therefore,
reabsorption of these ions is decreased.
2. The loop diuretics are the most efficacious
of the diuretic drugs
14

Actions of loop diuretics
•
The loop diuretics act even among patients who
have poor renal function or have not responded to
thiazides or other diuretics.
•
Loop diuretics increase the Ca2+ content of urine,
whereas thiazide diuretics decrease the Ca2+
concentration of the urine.
15
Actions of loop diuretics
•
The loop diuretics act even among patients who
have poor renal function or have not responded to
thiazides or other diuretics.
•
Loop diuretics increase the Ca2+ content of urine,
whereas thiazide diuretics decrease the Ca2+
concentration of the urine.

•
In patients with normal serum Ca2+
concentrations, hypocalcemia does not result,
because Ca2+ is reabsorbed in the distal
convoluted tubule. However, hypomagnesemia
can occur due to loss of Mg2+.
16

The loop diuretics cause decreased renal
vascular resistance and increased renal
blood flow.
Loop diuretics increase prostaglandin
synthesis. PGs have a role in their diuretic
action, and substances such as
indomethacin that interfere in PG synthesis
can reduce diuretic action of these agents.
17
The loop diuretics cause decreased renal
vascular resistance and increased renal
blood flow.
Loop diuretics increase prostaglandin
synthesis. PGs have a role in their diuretic
action, and substances such as
indomethacin that interfere in PG synthesis
can reduce diuretic action of these agents.

Therapeutic uses:
1. acute pulmonary edema of heart failure( drugs of
choice). Because of their rapid onset of action,
particularly when given intravenously, (rapid,
intense diuresis).
2. hypercalcemia, because they stimulate tubular
Ca2+ excretion.
3. hyperkalemia.
18
Therapeutic uses:
1. acute pulmonary edema of heart failure( drugs of
choice). Because of their rapid onset of action,
particularly when given intravenously, (rapid,
intense diuresis).
2. hypercalcemia, because they stimulate tubular
Ca2+ excretion.
3. hyperkalemia.

Pharmacokinetics:
administered orally or parenterally.
Their duration of action 2-4 hours.
secreted into the urine.
Adverse effects:
1. Ototoxicity
2. Acute hypovolemia
3. Hyperuricemia
4. Potassium depletion
5. Hypomagnesemia
19
Pharmacokinetics:
administered orally or parenterally.
Their duration of action 2-4 hours.
secreted into the urine.
Adverse effects:
1. Ototoxicity
2. Acute hypovolemia
3. Hyperuricemia
4. Potassium depletion
5. Hypomagnesemia

Thiazides and Related Agents
They are most widely used of diuretic drugs.
They are sulfonamide derivatives and, as
such, are related in structure to the carbonic
anhydrase inhibitors.
20

All thiazides affect distal tubule
have equal maximum diuretic effects, differing
only in potency
They are called "ceiling diuretics" because
increasing dose above normal does not promote a
further diuretic response ( so called ceiling
diuretics)
Thiazides partly depend on renal prostaglandin
synthesis
21
All thiazides affect distal tubule
have equal maximum diuretic effects, differing
only in potency
They are called "ceiling diuretics" because
increasing dose above normal does not promote a
further diuretic response ( so called ceiling
diuretics)
Thiazides partly depend on renal prostaglandin
synthesis
Chlorothiazide
Active orally
Capable of affecting the severe edema of cirrhosis
and heart failure with a minimum of side effects.
Hydrochlorothiazide
More potent, so that the required dose is
considerably lower than that of chlorothiazide.
Note:
Chlorthalidone, indapamide, and metolazone
are referred to as thiazide-like diuretics,
because they contain the sulfonamide residue
in their chemical structures and their
mechanism of action is similar.
22
Chlorothiazide
Active orally
Capable of affecting the severe edema of cirrhosis
and heart failure with a minimum of side effects.
Hydrochlorothiazide
More potent, so that the required dose is
considerably lower than that of chlorothiazide.
Note:
Chlorthalidone, indapamide, and metolazone
are referred to as thiazide-like diuretics,
because they contain the sulfonamide residue
in their chemical structures and their
mechanism of action is similar.

Mechanism of action:
The thiazide derivatives act mainly in the distal
tubule to decrease the reabsorption of Na+
apparently by inhibition of a Na+/CI- cotransporter
on the luminal membrane of the distal convoluted
tubule. They have a lesser effect in the proximal
tubule.
23
Mechanism of action:
The thiazide derivatives act mainly in the distal
tubule to decrease the reabsorption of Na+
apparently by inhibition of a Na+/CI- cotransporter
on the luminal membrane of the distal convoluted
tubule. They have a lesser effect in the proximal
tubule.

•
These drugs increase concentration of Na+ and
Cl- in the tubular fluid. The acid-base balance is
not usually affected.
Note:
Because the site of action of the thiazide
derivatives is on luminal membrane, these
drugs must be excreted into tubular lumen
to be effective. Therefore, with decreased
renal function, thiazide diuretics lose
efficacy.
24
•
These drugs increase concentration of Na+ and
Cl- in the tubular fluid. The acid-base balance is
not usually affected.
Note:
Because the site of action of the thiazide
derivatives is on luminal membrane, these
drugs must be excreted into tubular lumen
to be effective. Therefore, with decreased
renal function, thiazide diuretics lose
efficacy.
Thiazides Actions
Increased excretion of Na+ and CI-
Loss of K+
Loss of Mg2+
Decreased urinary calcium excretion
Reduced peripheral vascular resistance
25

Therapeutic uses of thiazides
1. Hypertension
2. Heart failure
3. Hypercalciuria
4. Diabetes insipidus
26

Pharmacokinetics:
The drugs are effective orally.
prolonged biologic half-life (40 hours).
Most thiazides take 1-3 weeks to produce a
stable reduction in blood pressure
All thiazides are secreted by the organic
acid secretory system of the kidney.
27
Pharmacokinetics:
The drugs are effective orally.
prolonged biologic half-life (40 hours).
Most thiazides take 1-3 weeks to produce a
stable reduction in blood pressure
All thiazides are secreted by the organic
acid secretory system of the kidney.

Adverse effects
1. Potassium depletion
2. Hyponatremia
3. Hyperuricemia
4. Volume depletion
5. Hypercalcemia
6. Hyperglycemia
7. Hyperlipidemia
8. Hypersensitivity
28
Adverse effects
1. Potassium depletion
2. Hyponatremia
3. Hyperuricemia
4. Volume depletion
5. Hypercalcemia
6. Hyperglycemia
7. Hyperlipidemia
8. Hypersensitivity

Thiazide-like analogs
Chlorthalidone:
•
Has a very long duration of action
•
Used to treat hypertension. It is given once per day for
this indication.
Metolazone: Metolazone is more potent than the thiazides.
Indapamide:
lipid-soluble
Has a long duration of action. At low doses, it shows
significant antihypertensive action with minimal diuretic
effects.
It is metabolized and excreted by the gastrointestinal tract
and the kidneys. It is therefore less likely to accumulate in
patients with renal failure, and may be useful in their
treatment.
29
Thiazide-like analogs
Chlorthalidone:
•
Has a very long duration of action
•
Used to treat hypertension. It is given once per day for
this indication.
Metolazone: Metolazone is more potent than the thiazides.
Indapamide:
lipid-soluble
Has a long duration of action. At low doses, it shows
significant antihypertensive action with minimal diuretic
effects.
It is metabolized and excreted by the gastrointestinal tract
and the kidneys. It is therefore less likely to accumulate in
patients with renal failure, and may be useful in their
treatment.

Potassium-sparing Diuretics
They act in the collecting tubule to inhibit Na+
reabsorption and K+ excretion.
Potassium-sparing diuretics are used alone
primarily when aldosterone is present in
excess.
30

The major use of potassium-sparing agents is in
the treatment of hypertension, most often in
combination with a thiazide.
The patients who are treated with potassium-
sparing diuretic need monitoring for potassium
levels.
If the patients take supplementation is usually
discontinued when potassium-sparing diuretic
therapy is instituted.
31
The major use of potassium-sparing agents is in
the treatment of hypertension, most often in
combination with a thiazide.
The patients who are treated with potassium-
sparing diuretic need monitoring for potassium
levels.
If the patients take supplementation is usually
discontinued when potassium-sparing diuretic
therapy is instituted.

Spironolactone
Mechanism of action
Antagonizes aldosterone at intracellular
cytoplasmic receptor sites.
Prevents Na+ reabsorption and, therefore,
K+ and H+ secretion
32

Actions:
•
In most edematous states, spironolactone is
given to a patient with elevated circulating
levels of aldosterone, the drug antagonizes
the activity of the hormone, resulting in
retention of K+ and excretion of Na+.
33
Therapeutic uses:
1.Diuretic:
Spironolactone has a low efficacy in mobilizing
Na+ from the body in comparison with the
other drugs. Spironolactone has the useful
property of causing the retention of K+.
It is the diuretic of choice in patients with
hepatic cirrhosis.
34
Therapeutic uses:
1.Diuretic:
Spironolactone has a low efficacy in mobilizing
Na+ from the body in comparison with the
other drugs. Spironolactone has the useful
property of causing the retention of K+.
It is the diuretic of choice in patients with
hepatic cirrhosis.

2. Secondary hyperaldosteronism:
Spironolactone is the only potassium-sparing
diuretic that is routinely used alone to induce
a net negative salt balance. It is particularly
effective in clinical situations associated with
secondary hyperaldosteronism.
3. Heart failure: Spironolactone prevents the
remodeling that occurs as compensation for
the progressive failure of the heart.
35
2. Secondary hyperaldosteronism:
Spironolactone is the only potassium-sparing
diuretic that is routinely used alone to induce
a net negative salt balance. It is particularly
effective in clinical situations associated with
secondary hyperaldosteronism.
3. Heart failure: Spironolactone prevents the
remodeling that occurs as compensation for
the progressive failure of the heart.

Pharmacokinetics
Spironolactone
Absorbed orally
Strongly bound to proteins
Converted to an active metabolite
The action of spironolactone is largely due to the
effect of its active metaboliets, which has
mineralocorticoid-blocking activity.
Spironolactone is enzyme inducer
36
Pharmacokinetics
Spironolactone
Absorbed orally
Strongly bound to proteins
Converted to an active metabolite
The action of spironolactone is largely due to the
effect of its active metaboliets, which has
mineralocorticoid-blocking activity.
Spironolactone is enzyme inducer

Adverse effects
1. Gastric upsets and can cause peptic ulcers.
2. Because it chemically resembles some of the sex
steroids, spironolactone may act at receptors in
other organs to induce gynecomastia in males
and menstrual irregularities in females
37

Triamterene and amiloride
•
Triamterene and amiloride block Na+ transport
channels, resulting in a decrease in Na+/K+
exchange. Although they have a K+-sparing
diuretic action similar to that of
spironolactone, their ability to block the
Na+/K+-exchange site in the collecting tubule
does not depend on the presence of
aldosterone.
•
Thus, they have diuretic activity even in
individuals with Addison disease.
38
Triamterene and amiloride
•
Triamterene and amiloride block Na+ transport
channels, resulting in a decrease in Na+/K+
exchange. Although they have a K+-sparing
diuretic action similar to that of
spironolactone, their ability to block the
Na+/K+-exchange site in the collecting tubule
does not depend on the presence of
aldosterone.
•
Thus, they have diuretic activity even in
individuals with Addison disease.

Triamterene and amiloride
•
The side effects of triamterene are leg
cramps and the possibility of increased
blood urea nitrogen, as well as uric acid
and K+ retention.
39
Triamterene and amiloride
•
The side effects of triamterene are leg
cramps and the possibility of increased
blood urea nitrogen, as well as uric acid
and K+ retention.

Osmotic Diuretics
Mannitol and urea
Mannitol is not absorbed when given orally,
and should only be given intravenously.
They have ability to carry water with them
into the tubular fluid and will cause an
increase in urinary output.
Used to increased water excretion rather
than Na+ excretion
40
Osmotic Diuretics
Mannitol and urea
Mannitol is not absorbed when given orally,
and should only be given intravenously.
They have ability to carry water with them
into the tubular fluid and will cause an
increase in urinary output.
Used to increased water excretion rather
than Na+ excretion

Uses of Osmotic Diuretics
1. They are used to maintain urine flow following
acute toxic ingestion of substances capable of
producing acute renal
2. Increased intracranial pressure or acute renal
failure due to shock, drug toxicities, and
trauma.
3. Maintaining urine flow preserves long-term
kidney function and may save the patient
from dialysis.
41
Uses of Osmotic Diuretics
1. They are used to maintain urine flow following
acute toxic ingestion of substances capable of
producing acute renal
2. Increased intracranial pressure or acute renal
failure due to shock, drug toxicities, and
trauma.
3. Maintaining urine flow preserves long-term
kidney function and may save the patient
from dialysis.

Adverse effects
•
Extracellular water expansion and dehydration,
The expansion of extracellular water results
because the presence of mannitol in the
extracellular fluid extracts water from the cells
and causes hyponatremia until diuresis occurs.
Dehydration, on the other hand,' can occur if
water is not replaced adequately.
42
Adverse effects
•
Extracellular water expansion and dehydration,
The expansion of extracellular water results
because the presence of mannitol in the
extracellular fluid extracts water from the cells
and causes hyponatremia until diuresis occurs.
Dehydration, on the other hand,' can occur if
water is not replaced adequately.
