
1
Fifth stage
Radiology
Lec-4
.د
ه
ديل
11/11/2015
Joint Diseases
ARTHRITIS
Types of Arthritis
There are three types of arthritis (which often can be distinguished radiologically):
1- Degenerative joint disease
Osteophytes,
Subchondral sclerosis
Uneven loss of articular space
2- Inflammatory arthritis
Unrnarginated erosions
Periarticular osteoporosis is common
Soft tissue swelling
Uniform loss of articular space
3- Metabolic arthritis
Lumpy bumpy soft tissue swelling
Marginated bony erosions with
overhanging edges
Degenerative Arthritis
Degenerative joint disease (DJD) = osteoarthritis (OA).
80% of population > 50 years have radiological evidence of OA.
types:
--Primary OA
* No underlying local etiological factors
2
*Abnormally high mechanical forces on normal joint
*Age related
--Secondary OA
Underlying etiological factors:
* trauma, inflammatory arthritis, hemochromatosis, acromegaly, congenital hipdysplasia,
osteonecrosis, loose bodies
*Normal forces on abnormal joint
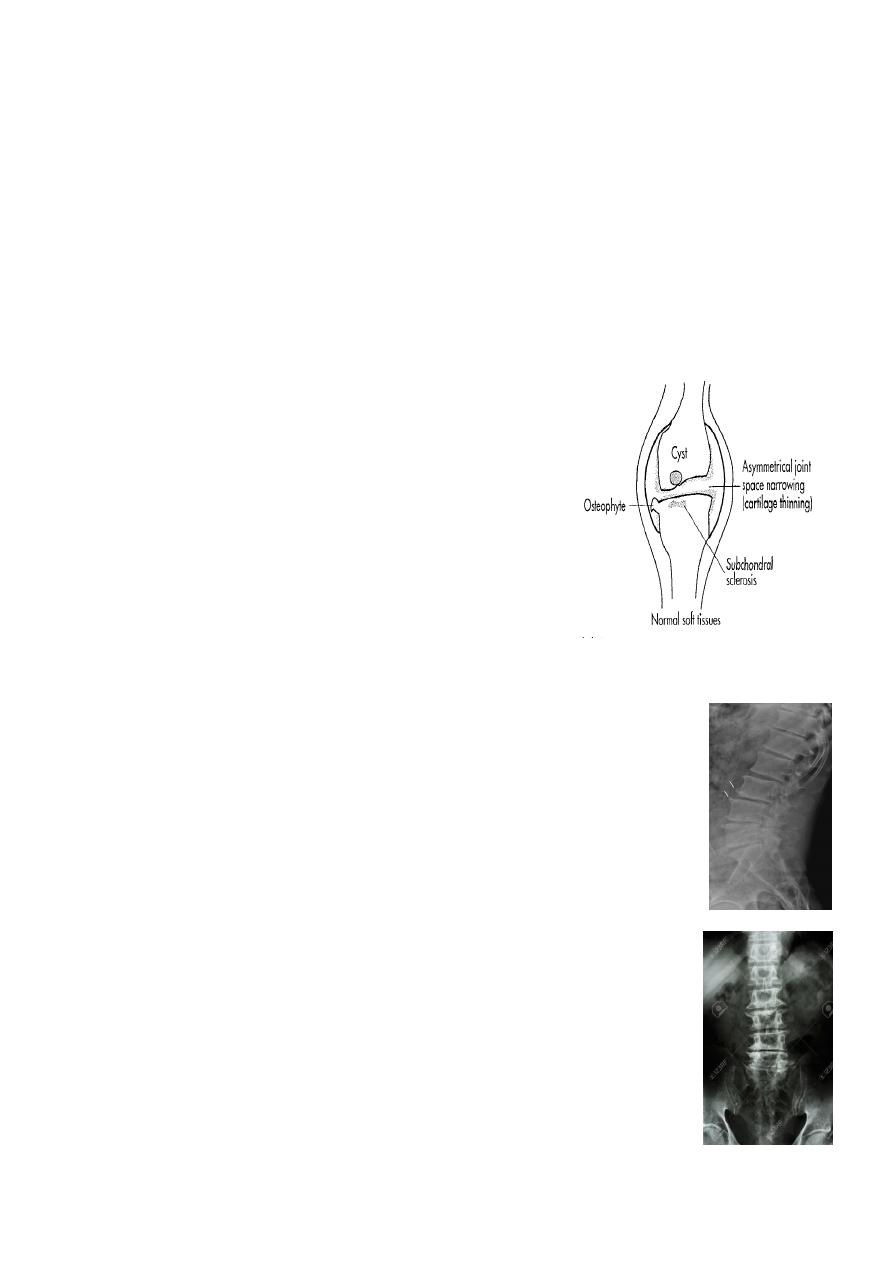
Radiographic features
Five hallmarks:
* Narrowing of joint space, usually asymmetrical
* Subchondral sclerosis
* Subchondral cysts (true cysts or pseudocysts)
* Osteophytes
* Lack of osteoporosis
In the Spine :
* Lower cervical and low lumbar spine are most comonly affected.
* Osteophytes may encroach on neural foramina (best seen on oblique
views).
* Vacuum phenomenon: gas (N2),is pathognomonic of the degenerative
process.
* OA of the spine occurs in the apophyseal joints .
* Degenerative spondylolisthesis (pseudospondylolithesis)
Lumbar spondylosis. There is distal narrowing and a vacuum phenomenon
is present in the degenerative discs. Marginal osteophytes are present.
Inferiorly the facet joints show features of degeneration and, with the
increase in lordosis, the spinous processes are in contact
3
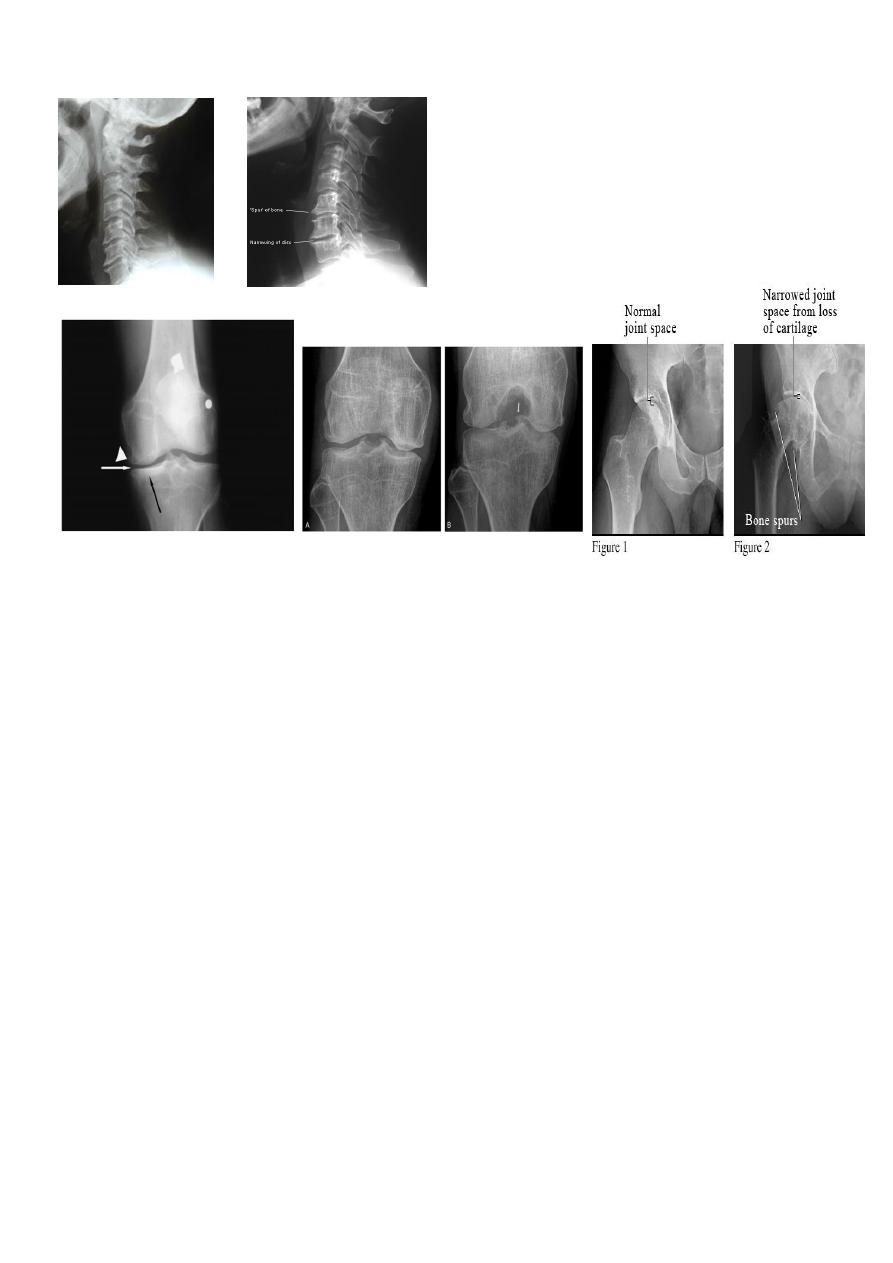
Cervical spondylosis
Inflammatory arthritis
There are three types of inflammatory arthritis
1- Autoimmune arthritis
RA
Scleroderma
Systemic lupus erythematosus (SLE)
Dermatomyositis
2- Seronegative spondylarthropathies
Ankylosing spondylitis
Reiter's syndrome
Psoriasis
Enteropathic arthropathies
3- Erosive OA
Rheumatoid Arthritis
Female: male = 3 : l
Radiographic features:
Early changes
* Peri articular soft tissue swelling (edema, synovial congestion)
4
* Peri articular osteoporosis in symmetrical distribution (hallmark)
* Preferred sites of early involvement
Hands: 2nd and 3rd MCP joint
Feet: 4th and 5th MTP joint
Late changes
* Erosions (pannus formation, granulation tissue) first attack joint portions in which
protective cartilage is absent (i.e., capsular insertion site).
* Erosions of the ulnar styloid and triquetrum are characteristic.
* Subchondral cysts formation results from synovial fluid, which is pressed into bone
marrow through destroyed cartilage.
* Subluxations, Carpal instability and ulnar deviation.
* Fibrous ankylosis is a late finding.
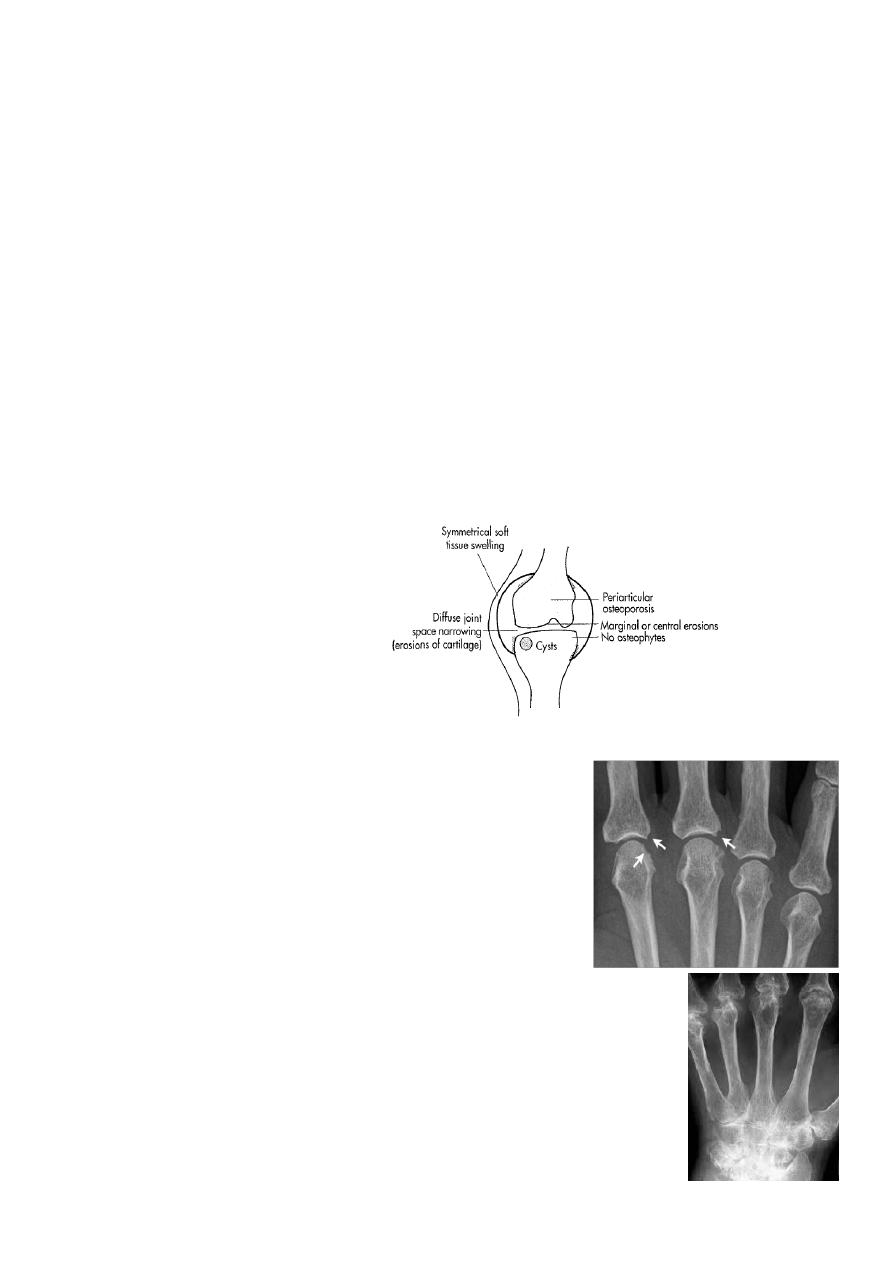
Rheumatoid arthritis.
(A) The initial radiograph shows a hint of early trabecular loss
around the proximal interphalangeal joint of a finger with
preservation of the joint space and early marginal cortical
loss at the base of the middle phalanx.
(B) The subsequent radiograph shows established erosive change in the
area of ill-defined demineralisation in association with joint space
narrowing.
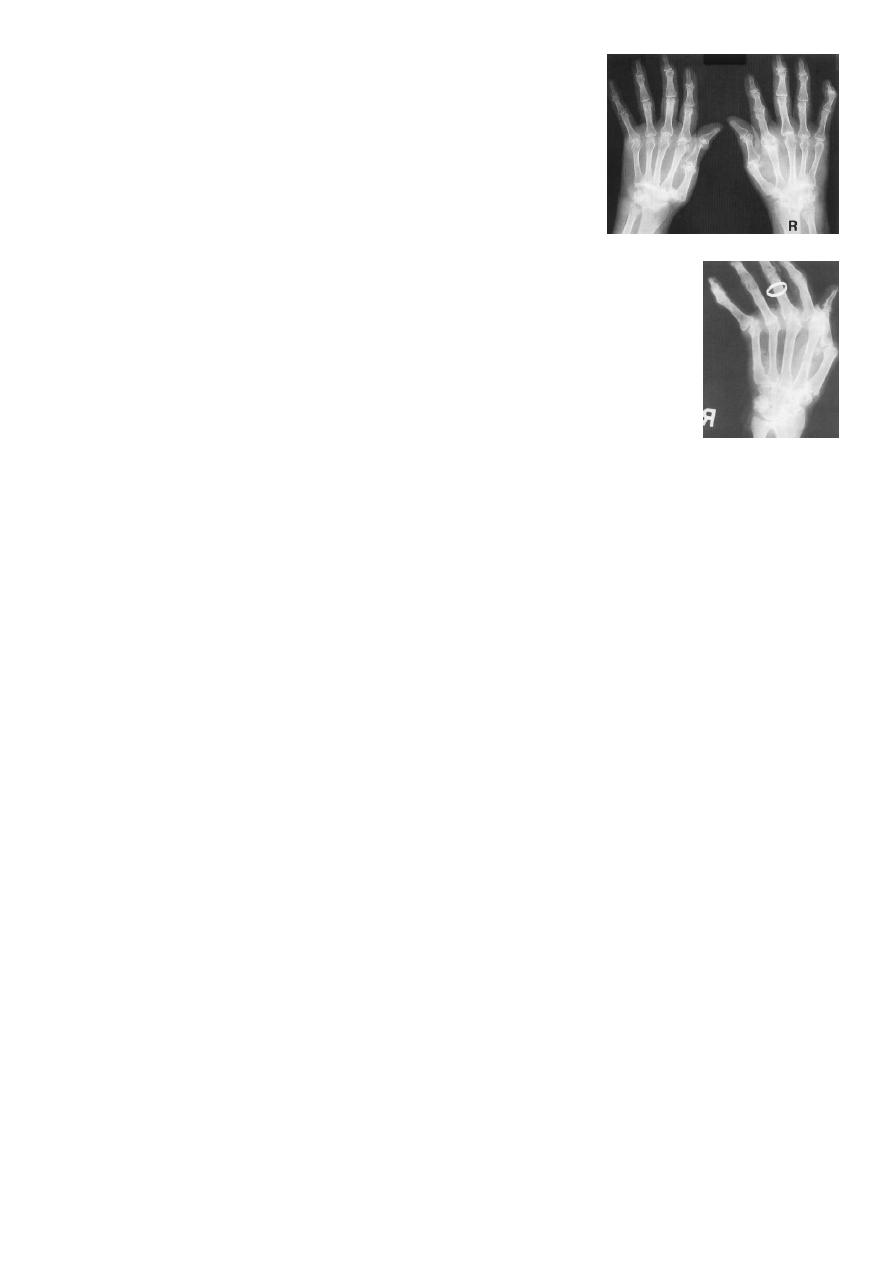
5
Rheumatoid arthritis. Bilateral changes are fairly symmetrical.
Soft-tissue swelling is demonstrated, especially over the ulnar
styloids. Erosions are demonstrated at the carpus, distal radius
and ulna, with joint space narrowing and collapse of bone.
Metacarpophalangeal erosions are also seen associated with
joint space narrowing. There is a swan-neck deformity of the
right fifth distal interphalangeal joint
Gross rheumatoid arthritis at the carpus with ulnar deviation, subluxation
and joint narrowing at the metacarpophalangeal joints.
Boutonniere deformities are present at the index and little fingers.
Ankylosing Spondylitis (AS)
Seronegative spondyloarthropathy of the axial skeleton and proximal large joints.
Clinical: males >> females. HLA-B27 in 95%. Insiduous onset of back pain and stiffness.
Onset: 20 years.
Radiographic features
* SI joint is the initial site of involvement:
bilateral, symmetrical
Erosions: Early, Sclerosis: intermediate, ankylosis: late
* Contiguous thoracolumbar involvement
Vertebral body "squaring": early osteitis
* Syndesmophytes
* Bamboo spine: late fusion and Bamboo spine
ligamentous ossification
* ankylosed spine (fracture)
* Enthesopathy is common (whiskering of tuberosities)
* Arthritis of proximal joints (hip > shoulder) in 50%, erosions and osteophytes
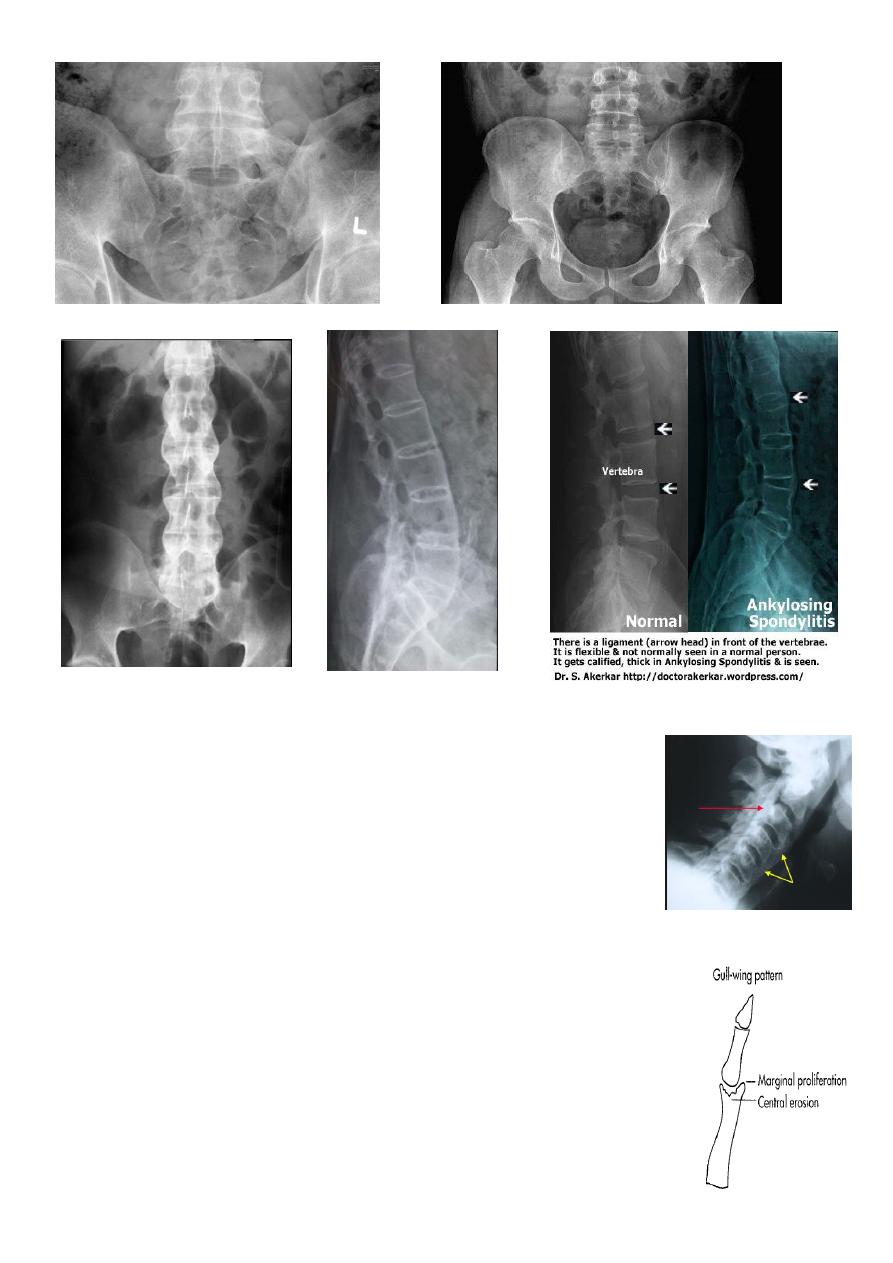
6
Diffuse Idiopathic Skeletal Hyperostosis (DISH)
Radiographic features
*Flowing osteophytes of at least four contiguous vertebral bodies
*Preserved disk height
*No sacroiliitis or facet ankylosis
*Calcification of ligaments and tendons
*Associated with hypertrophic DJD
Erosive Osteoarthritis
OA with superimposed inflammatory, erosive changes. Characteristically
affects middle-aged women.
Radiographic features
7
* Erosive and productive changes of DIP and PIP
* Gull-wing pattern: secondary to central erosions and Marginal
proliferation osteophytes.
Typical involvement of first CMC may help distinguish erosive OA from
rheumatoid arthritis (RA), psoriatic arthritis, and adult Still's disease.
* Interphalangeal fusion may occur.
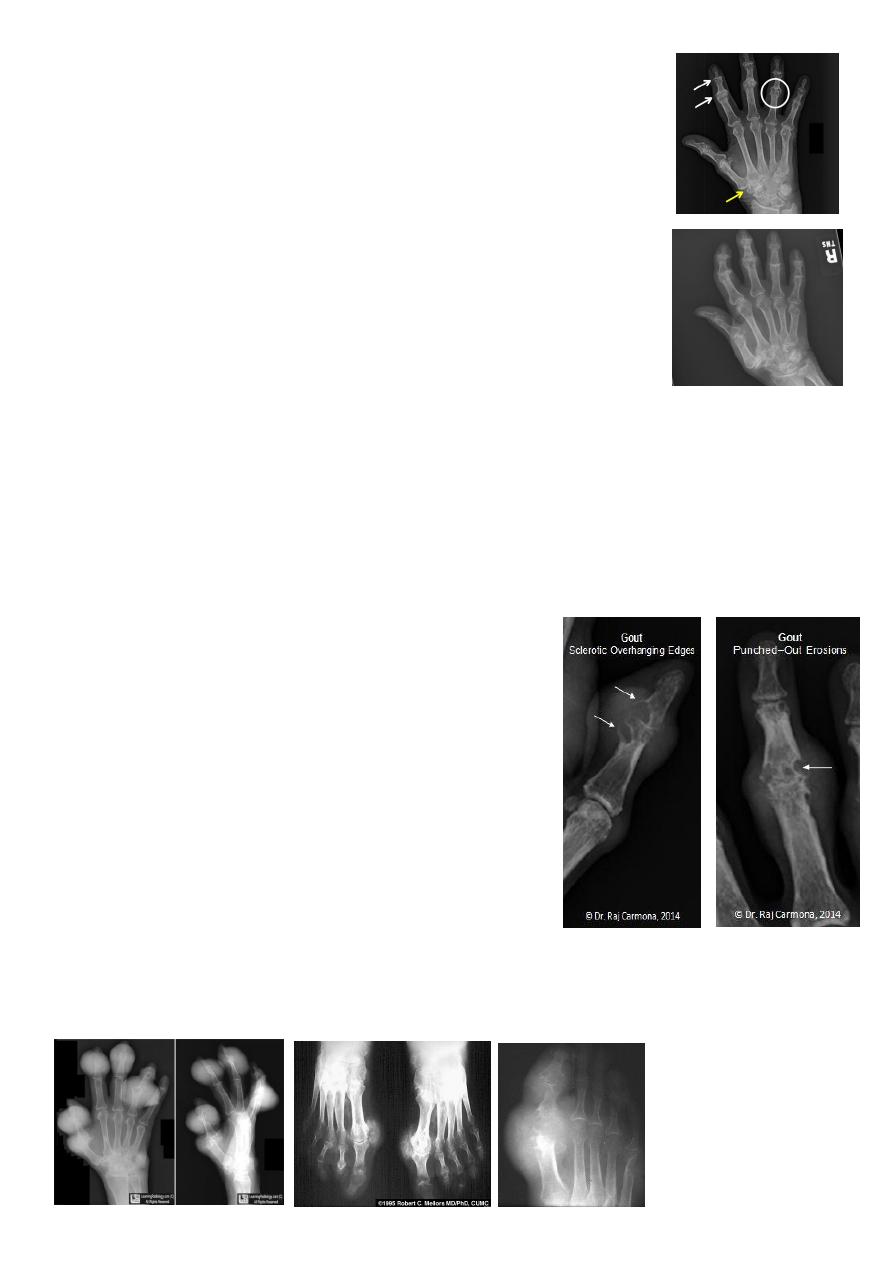
Gout
Heterogeneous group of entities characterized by recurrent attacks of arthritis secondary to
deposition of sodium urate crystals in and around joints.
*90% of patients are male
*Causes due to either Uric acid overproduction, 10% or under excretion, 90%.
Radiographic features
* Lower extremity > upper extremity; small joints > large joints
* First MTP is most common site
* Marginal, peri articular erosions: overhanging edge
* Erosions may have sclerotic borders
* Joint space is preserved
* Soft tissue and bursa deposition
Tophi: juxtaarticular, helix of ear
Bursitis: olecranon, prepatellar
* Erosions and tophi only seen in longstanding disease
* Tophi calcification, 50%
* Chondrocalcinosis
8
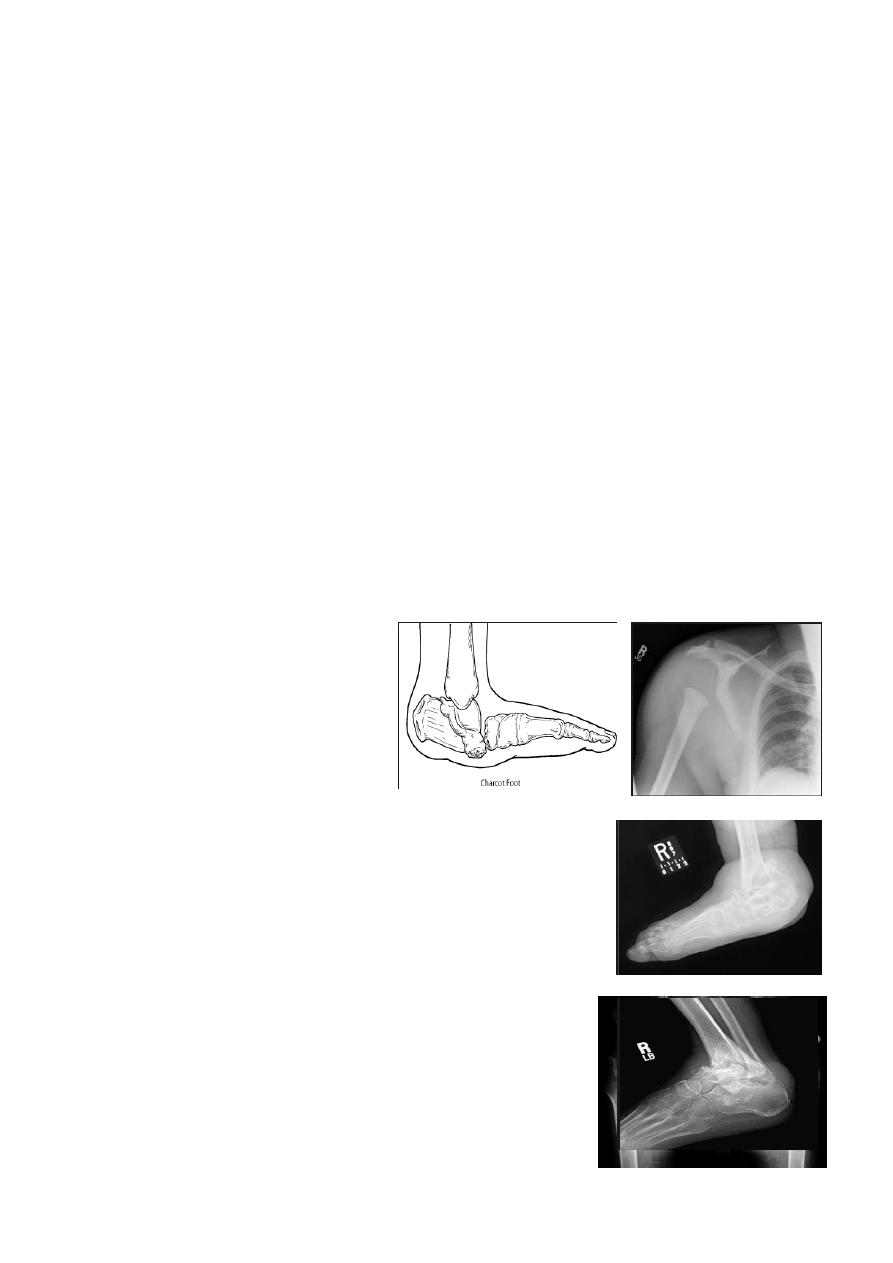
Infectious arthritis (septic arthritis)
Infectious arthritis usually results from hematogenous spread to synovium and subsequent
spread into the joint.
Direct spread of osteomyelitis into the joint is much less common.
The diagnosis is made by joint aspiration.
Organism , Staphylococcus aureus (most common) ,B-Streptococcus in infants , Salmonella
is seen in sickle cell patients ; however, the most common infection in sickle cell patients is
Staphylococcus.
Radiographic features
Plain film
* Joint effusion
* Juxtaarticular osteoporosis
* Destruction of subchondral bone on both sides of the joint
Neuropathic Arthritis (Charcot's Joint)
Primary loss of sensation in a joint leads to arthropathy. Distribution helps determine
etiology.
Causes
Diabetes neuropathy: usually foot
Tertiary syphilis: usually knee
Syringomyelia: usually shoulder
Radiographic features
Common to all types
*Joint instability: subluxation or dislocation
*Prominent joint effusion
--- Hypertrophic type, 20%
Marked fragmentation of articular bone
Much reactive bone
--- Atrophic type, 40%
Bone resorption of articular portion
--- Combined type, 40%
9
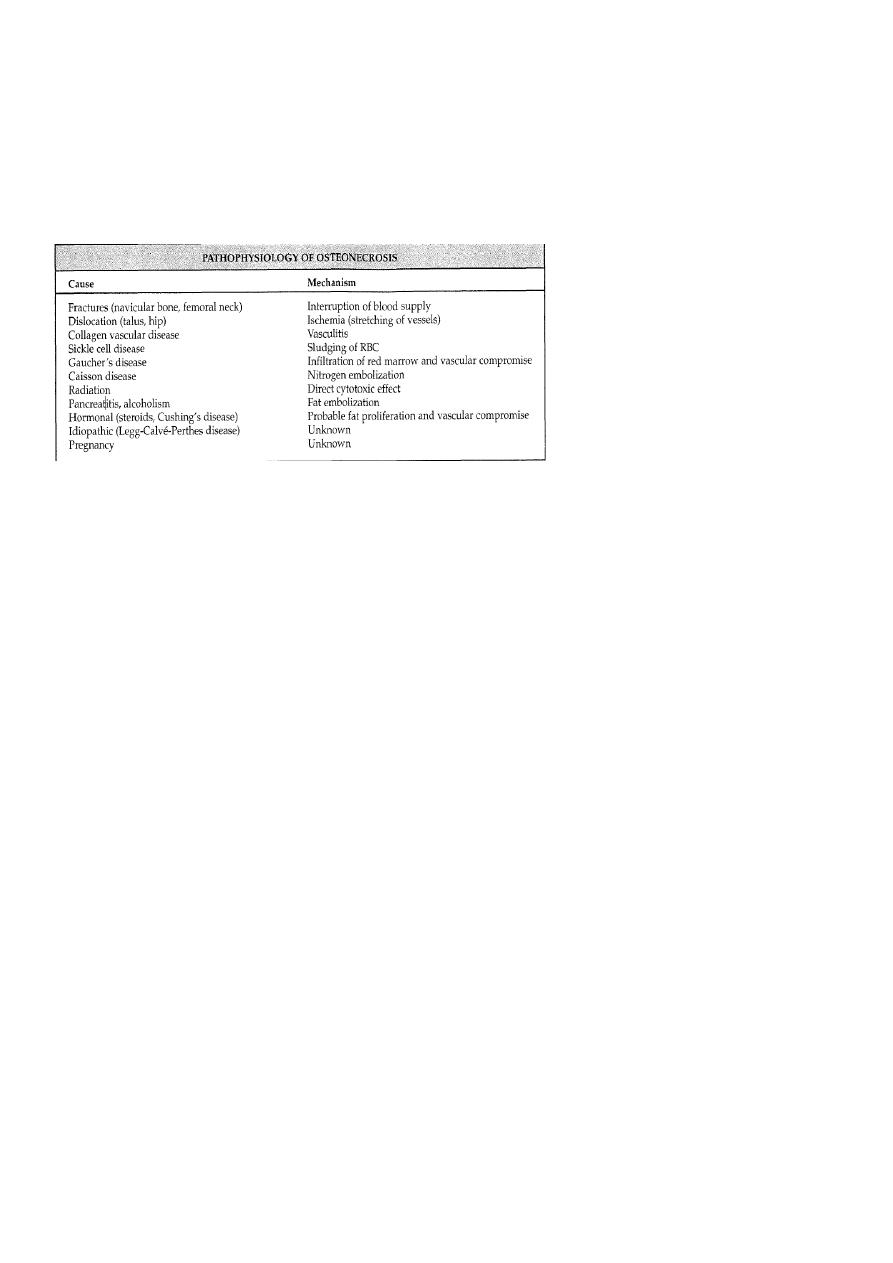
Osteonecrosis
Osteonecrosis (avascular necrosis, ischemic necrosis, aseptic necrosis) may be caused by
two mechanisms:
* Interruption of arterial supply
* Intra/extraosseous venous insufficiency.
The pathophysiology of all osteonecrosis is the same:
Ischemia > revascularization >repair > deformity> osteoarthrosis
Plain films
Findings lag several months behind time of injury.
These findings include areas of radiolucency, fissuring , fragmentation , bone collapse and
condensation , end with dense and flat bone with loss of bone contour and secondary
osteoarthritis
MRI
Most sensitive imaging modality: 95%-100% sensitivity
Osteochodrosis:
These osteonecroses are usually idiopathic in origin. The following are the most common
Legg-Calve-Perthes disease : osteochodrosis of the femur head
Usually affects 5-10 years, started as hip pain , if not treated it will ends with mushroom
deformity due to neglected and untreated perthis seen later on and is liable for early OA
chnges .
11
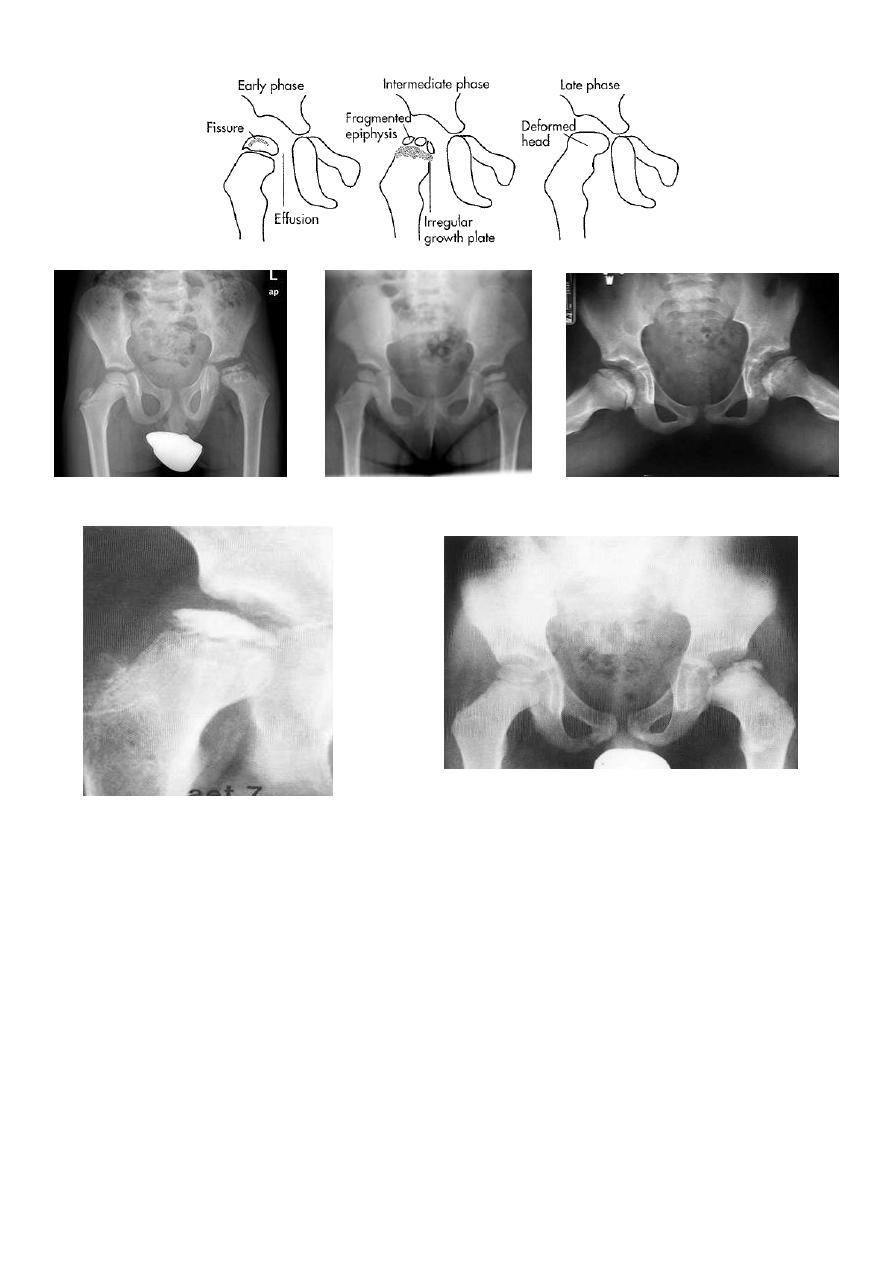
Perthes' disease. A series of
radiographs showing the stages
of healing. (A) The initial
radiograph shows a flattened,
sclerotic femoral head
The left femoral neck is broadened, the
metaphysis sclerotic with focal areas of
lucency, the growth plate irregular and the
femoral head flattened and sclerotic. It is
uncovered laterally. The joint space
appears widened
11
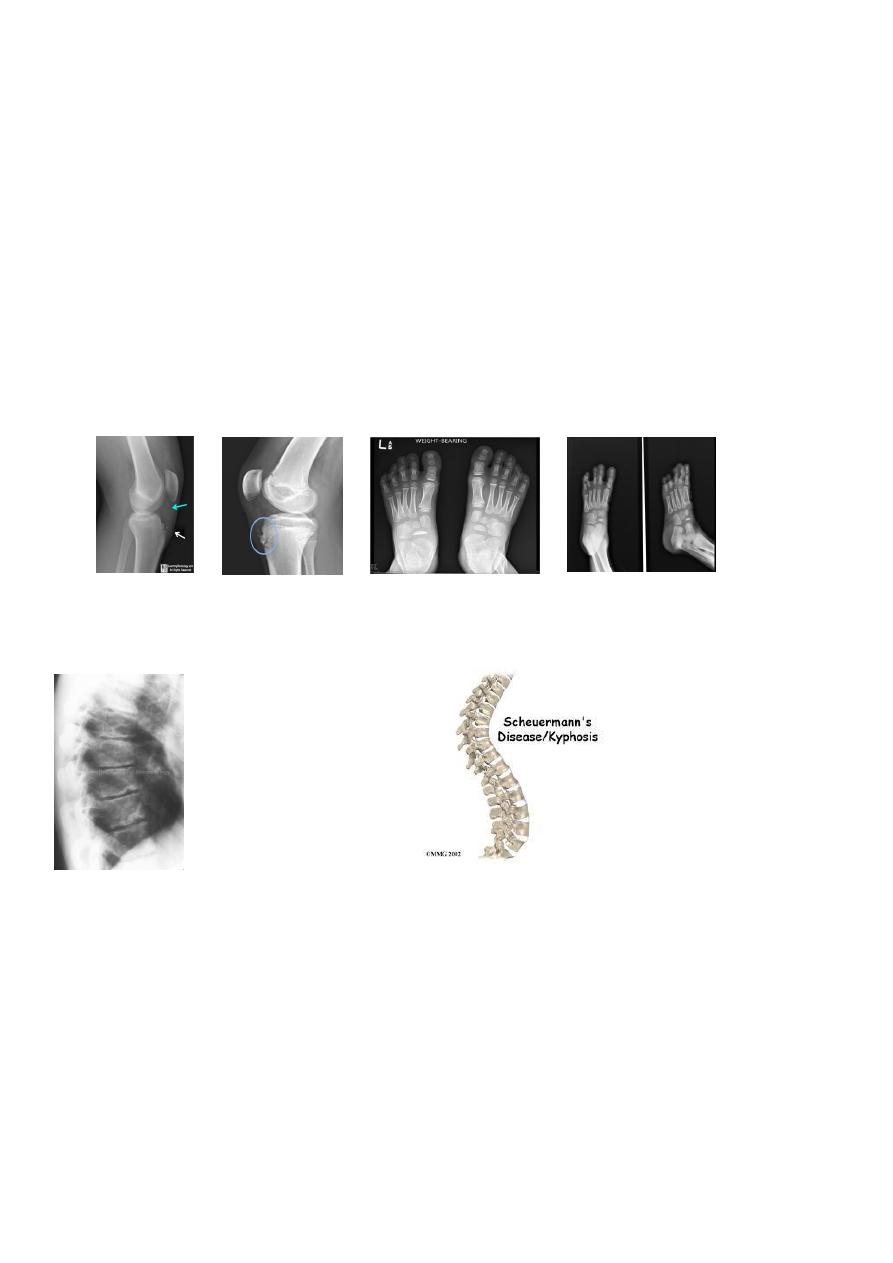
Scheuermann's disease: (adolecent Kyphosis).
osteochodrosis of the vertebral end plates .
Usually affects 8- 10 years , characterized by erosion of anterior superior and inferior
vertebral margin resulting in decrease in the height of anterior part of the vertebra
(vertebral wedging ) ending with kyphosis.
Osgood-Schlatter : 12-16 y,osteochodrosis of the tibial tuberocle.
Blount's disease: tibial epiphysis
Kohler's : 4-8 y ,osteochodrosis of the Navicular bone .
Kienbock's: adults, osteochodrosis of the lunate bone .
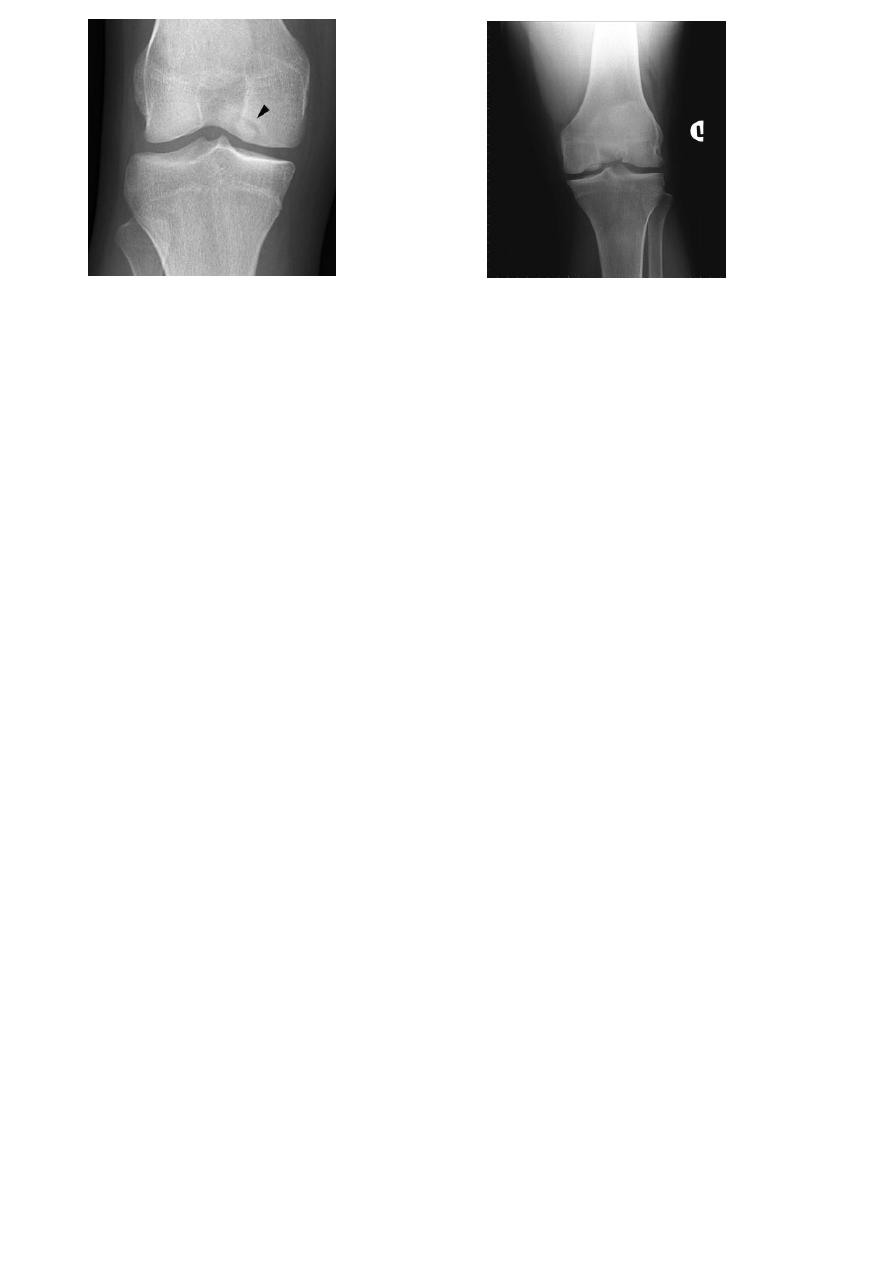
Osteochondritis dissecans:
affects the large articular surface, commomnly medial femural condylee, talus and trochlea.
Ends by separation of the affected part in to the joint space resulting in intra-articular loose
body.
Osteochondritis of lumbar
vertebral bodies (advanced case).
Scheuemann's disease
Adolescent kyphosis
Osteochondritis of
lumbar vertebral
bodies (advanced
case).
12
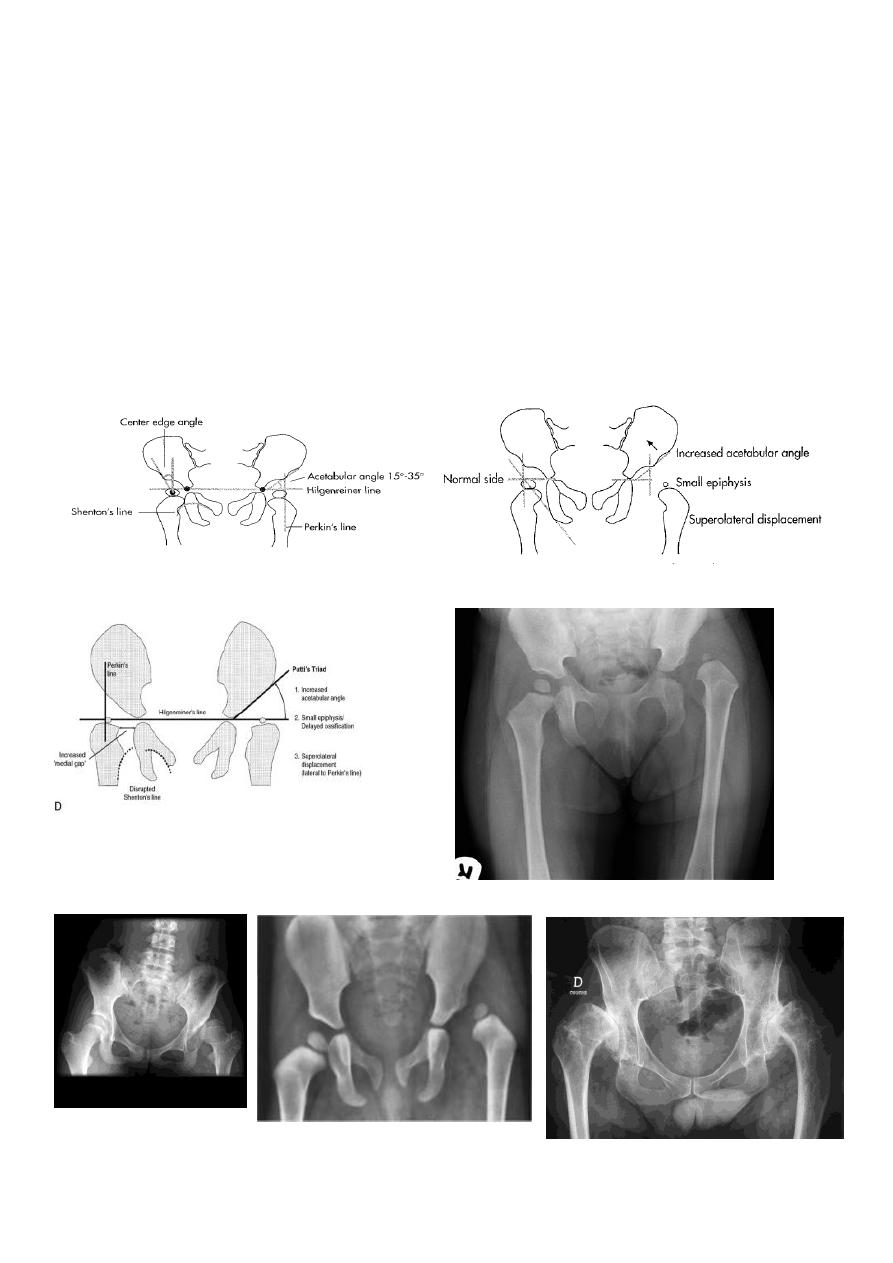
Developmental Dysplasia of Hip (Congenital Dislocation Of The Hip)
An abnormally lax joint capsule allows the femoral head to fall out of the acetabulum,
leading to deformation.
Predisposing factors for the development of CDH are:
* Abnormal ligamentous laxity (effect of estrogen; female:male = 6:l)
* Acetabular dysplasia .
CDH occurs most commonly (70%) in the left hip. Bilateral involvement is seen in 5%.
Radiographic features
US (commonly used today) at 1-3 months
* Normal femoral head is covered at least 50% by acetabulum , In CDH < 50% of femoral
head is covered by acetabulum .
Plain film
At 3-6 months :
By doing special veiw (Von Rosen veiw) by abduction of the thigh 45 degree and internal
rotation .
In DDH the lines that drown through the femura will meet in higher level than the normally
should at lumbosacral joint .
6 months and later
* AP veiw (femural epiphysis are visualized):
* Superolateral displacement of proximal femur (disturbed shenton’s line)
* Increase in acetabular angle
Osteochondritis dissecans of the medial
femoral condyle
Osteochondritis dissecans of the
medial part of the articular surface
13
* Small capital femoral epiphysis
• Femoral head is located lateral to Perkin's line
* Other features that are sometimes present
Abnormal sclerosis of the acetabulum
Shallow acetabulum
Formation of a false acetabulurn
Delayed ossification of femoral head
