Obesity
Goals of the lecture• Explain the underlying causes of overweight and obesity.
• Identify parameters used to diagnose obesity.
• Identify desired therapeutic goals for patients who are overweight or obese.
• Recommend appropriate nonpharmacologic and pharmacologic therapeutic interventions for overweight or obese patients.
• Educate patients about the disease state and associated risks, appropriate lifestyle modifications, drug therapy, and surgical options necessary for effective treatment
Introduction
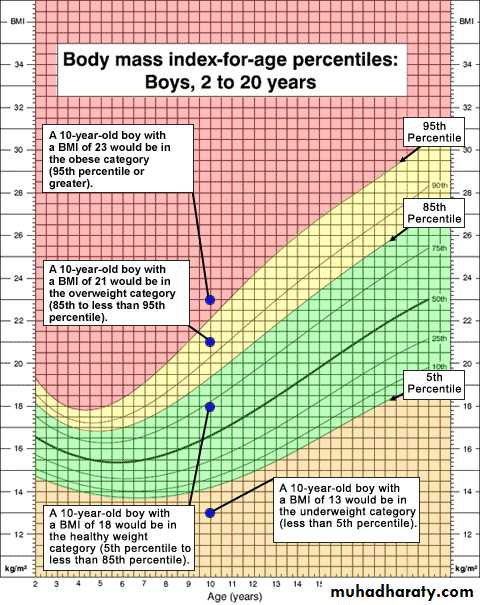
Overweight and obesity are terms used to describe weight measurements greater than what is considered healthy for a given height. Body mass index (BMI), waist circumference, comorbidities, and readiness to lose weight are used in the assessment of overweight or obese patients. The primary modality in defining overweight and obesity is the BMI. BMI does not reflect distribution of body fat; therefore, the measurement of waist circumference is a more practical method to evaluate abdominal fat before and during weight loss treatmentETIOLOGY
Obesity occurs when there is increased energy storage resulting from an imbalance between energy intake and energy expenditure over time. The specific etiology for this imbalance in the vast majority of individuals is multifactorial, with genetic and environmental factors contributing to various degrees. In a small minority of individuals, excess weight may be attributed to an underlying medical condition or an unintended effect of a medication.Genetic Influences
Observational studies in humans and experimental studies in animal models have demonstrated the strong role of genetics in determining both obesity and distribution of body fat. In some individuals, genetic factors are the primary determinants of obesity, whereas in others, obesity may be caused primarily by environmental factors. The genetic contribution to the actual variance in body mass index (BMI) and body fat distribution is estimated to be up to 80%.Environmental Factors
Many of the societal changes associated with economic development over the past 40 years have been implicated as potential causes for the increase in the prevalence of obesity. These include an abundant and easily accessible food supply and the material comforts of modern life, which have contributed to a reduction in physical activity.
Medical Conditions
Conditions associated with weight gain include iatrogenic and idiopathic Cushing’s syndrome, growth hormone deficiency, insulinoma, leptin deficiency, and various psychiatric disorders, such as depression, binge-eating disorder, and schizophrenia. Hypothyroidism is often included in this list, but it mostly causes fluid retention (myxedema) and is generally not a cause of significant obesity.Medications
An increasing number of medications are associated with unintended weight gain. These include several anticonvulsants (e.g., carbamazepine, gabapentin, pregabalin, and valproic acid), antidepressants (e.g., mirtazapine and tricyclic antidepressants), atypical antipsychotics (e.g., clozapine, olanzapine, quetiapine, and risperidone), conventional antipsychotics (e.g., haloperidol), and hormones (e.g., corticosteroids, insulin, and medroxyprogesterone). Although the pharmacologic mechanism responsible for weight gain is usually drug-specific, in most cases the precise mechanism is unknown.PATHOPHYSIOLOGY
Although a correlation between body weight in parents and children exists, the specific gene or genes contributing to obesity are unknown. The key factor in the development of overweight and obesity is the imbalance that occurs between energy intake and energy expenditure. The extent of obesity is determined by the length of time this imbalance has been present. Energy intake is affected by environmental influences, including social, behavioral, and cultural factors, whereas genetic composition and metabolism affect energy expenditurePATHOPHYSIOLOGY
Energy IntakeFood intake is regulated by various receptor systems. Direct stimulation of serotonin 1A subtype (5-HT1A) and noradrenergic α2-receptors increases food intake, serotonin 2C subtype (5-HT2C) and noradrenergic α1- or β2-receptor activation decreases food intake. Stimulation of histamine receptor subtypes 1 and 3 and dopamine receptors 1 and 2 results in lower food consumption. In addition to receptor-modulated food consumption, higher levels of the protein leptin are associated with decreased food intake. In contrast, elevated levels of neuropeptide Y increase food intake.
PATHOPHYSIOLOGY
Energy ExpenditureA person’s metabolic rate is the primary determinant of energy expenditure. The metabolic rate is enhanced after food consumption and is directly related to the amount and type. Physical inactivity may predispose an individual to overweight and obesity. In addition, endocrine-related disorders (e.g., hypothyroidism and Cushing’s syndrome) may lower the metabolic rate, further contributing to the development of overweight and obesity.
DIAGNOSIS
The parameters that use to determine obesity involve,
•BMI
•waist circumference
•The presence of comorbidities or associated risks.
The presence of comorbidities
The presence of comorbidities: (CHD, atherosclerosis, type 2 diabetes mellitus, and sleep apnea) and cardiovascular risk factors (cigarette smoking, hypertension, elevated low-density lipoprotein cholesterol, low high-density lipoprotein cholesterol, impaired fasting glucose, family historyof premature CHD, and age) requires identification and aggressive management for overall effective treatment of the overweight or obese patientTREATMENT
Desired OutcomeThe treatment goals for overweight and obesity are to prevent additional weight gain, reduce and maintain a lower body weight, and control related risks. Specific weight goals should be established that are consistent with medical needs and the patient’s personal desire.
Weight loss is indicated for patients with a BMI of 25 to 29.9 kg/m2 or an elevated waist circumference with two or more comorbidities or for any patient with a BMI of 30 kg/m2 or greater.
If weight loss has been achieved and/or maintained for 6 months, therapy promoting further weight loss may be considered.
TREATMENT
General Approach to Treatment• Before recommending any therapy, presence of secondary causes of obesity (medical conditions or medication) must evaluate.
• If no secondary cause exists, the presence of other cardiovascular risk factors and comorbidities must be determined to guide clinical decisions
• Treatment of obesity includes:
Lifestyle changes (dietary modification, enhanced physical activity, and behavioral therapy)
pharmacologic treatment
surgical intervention
Or a combination of modalities.
TREATMENT
Nonpharmacologic Therapy
Nonpharmacologic therapy, including reduced caloric intake, increased physical activity, and behavioral modification, is the mainstay of obesity management. This combination is recommended as first-line therapy
Reduced Caloric Intake
Current adult guidelines recommend reduced caloric intake through adherence to a low-calorie diet (LCD). The LCD should provide restricts daily calories to a range of 1000 to 1200 kcal for women weighing less than 75 kg and 1,400 to 1,600 kcal for all others.
TREATMENT
Nonpharmacologic TherapyExercise
Although diet and exercise contribute to weight loss, combining an LCD with physical activity results in greater weight loss compared with either therapy alone. In addition, physical activity can help to prevent weight regain and reduce related cardiovascular risks. Slow titration of both the amount and intensity of physical activity is recommended for most overweight and obese patients. A program that incorporates daily walking is a viable option for most patients.
Pharmacologic Therapy
Pharmacotherapy is not recommended for individuals with BMIs of less than 27 kg/m2. If lifestyle changes do not result in a 10% weight loss after 6 months, drug therapy in addition to a healthy lifestyle is warranted for overweight individuals with other related risks and for obese patients.Pharmacotherapy in addition to lifestyle modification is reserved for patients with a BMI of 30 kg/m2 or greater, or a BMI of 27 kg/m2 or greater with other obesity-related risk factors.
Pharmacologic products promoting weight loss are classified according to their mechanisms of action, including the suppression of appetite and the suppression of fat absorption
Pharmacologic Therapy
Because obesity-related risks resurface with weight regain, long-term treatment is recommended to minimize these sequelae.Prolonged use of both fenfluramine and dexfenfluramine monotherapy and fenfluramine and phentermine in combination resulted in cardiac valvular disease.
Long-term treatment with sibutramine resulted in an increased risk for nonfatal heart attacks and nonfatal strokes in patients with preexisting cardiovascular disease.
Therefore, orlistat is the only drug currently approved for long-term use in promoting weight loss and preventing weight regain.
Orlistat
Mechanism of action: Orlistat promotes and maintains weight loss by acting locally in the GI tract. Orlistat is a chemically synthesized derivative of lipstatin, a natural product of Streptomyces toxytricini that inhibits pancreatic and gastric lipases, as well as triglyceride hydrolysis. As a result, undigested triglycerides are not absorbed, causing a caloric deficit and weight loss.
Dose: Initiate orlistat 120 mg three times a day. Orlistat may be taken during or up to 1 hour after the meal. Doses above 360 mg/day provide no greater benefit and thus are not recommended
Orlistat
Adverse effect: Common adverse reactions observed were fatty or oily stools, oily spotting, oily evacuation, or abdominal pain and/or flatulence with bowel movements. Soft stools, nausea, increased defecation, and fecal incontinence also were noted.Interactions
Orlistat reduces the absorption of some fat-soluble vitamins and β-carotene.
Hypothyroidism has been observed in patients taking both orlistat and levothyroxine.
Administration of orlistat in conjunction with cyclosporine can result in decreased cyclosporine plasma levels
Orlistat is contraindicated in patients with chronic malabsorption syndrome or cholestasis
Sibutramine
Sibutramine and its two active metabolites (M1 and M2) induce weight loss by inhibiting the reuptake of serotonin, norepinephrine, and dopamine. Appetite becomes suppressed because patients feel a sense of satiety. Because an increased risk for nonfatal myocardial infarction (MI) and nonfatal stroke was observed for sibutramine-treated patients, FDA withdraws sibutramine from the U.S.Phentermine
Mechanism of actions: Phentermine decreases food intake, and hence weight, by increasing norepinephrine and dopamine release in the central nervous system (CNS).Uses: This drug is indicated for short-term use—no more than a few
Doses In conjunction with a healthy lifestyle, 30 to 37.5 mg of phentermine is administered once daily, typically before breakfast or 1 to 2 hours after the morning meal; some patients may be managed adequately at 15 to 18.75 mg/day, but a dose of 18.75 mg twice daily may be used to minimize side effects, excluding insomnia.
Phentermine
Adverse reactions: Common adverse reactions seen with phentermine use include heart palpitations, tachycardia, elevated blood pressure, stimulation, restlessness, dizziness, insomnia, euphoria, dysphoria, tremor, headache, dry mouth, constipation, and diarrhea.Contraindication:
Phentermine should be avoided in patients with unstable cardiac status, hypertension, hyperthyroidism, agitated states, or glaucoma. Phentermine use should be avoided in patients concomitantly receiving or having received a monoamine oxidase inhibitor (MAOI) within the preceding 14 days. Because phentermine is related to the amphetamines, the potential for abuse is high
Diethylpropion
This sympathomimetic amine exudes similar pharmacologic activity as the amphetamines, resulting in CNS stimulation and appetite suppression.
Doses: Diethylpropion is available as both an immediate- and a controlled-release product. In conjunction with a reduced calorie diet and/or exercise, dose diethylpropion (immediate release) 25 mg three times a day before meals or 75 mg (controlled release) once a day, usually midmorning
Adverse effect:
Use of diethylpropion for a period longer than 3 months is associated with an increased risk for development of pulmonary hypertension.
common CNS adverse effects included overstimulation, restlessness, dizziness, insomnia, euphoria, dysphoria, tremor, nervousness, drowsiness, mydriasis, and blurred vision. In addition, diethylpropion can decrease the seizure threshold, subsequently increasing a patient’s risk for an epileptic event.
Other organ systems also can adversely be affected, resulting in tachycardia, elevated blood pressure, palpitations, dry mouth, GIT disturbance, impotence or change in libido, gynecomastia, and bone marrow suppression.
Contraindications:
Patients with pulmonary hypertension, advanced arteriosclerosis, severe hypertension, hyperthyroidism, agitated states, or glaucoma. Because diethylpropion is related to the amphetamines, the potential for abuse is high; therefore, its use is contraindicated in patients with a history of substance abuse.
As with phentermine, use of diethylpropion should be avoided in patients concomitantly receiving or having received an MAOI within the preceding 14 days to prevent hypertensive crisis.
Diethylpropion
This sympathomimetic amine exudes similar pharmacologic activity as the amphetamines, resulting in CNS stimulation and appetite suppression. This drug is indicated for shortterm use in conjunction with a reduced-calorie diet and exercise in obese patients with BMIs of 30 kg/m2 or greater after failed attempts of diet and exercise alone.Doses Diethylpropion is available as both an immediate- and a controlled-release product. In conjunction with a reduced calorie diet and/or exercise, dose diethylpropion (immediate release) 25 mg three times a day before meals or 75 mg (controlled release) once a day, usually midmorning
Adverse effect:
Use of diethylpropion for a period longer than 3 months is associated with an increased risk for development of pulmonary hypertension.
common CNS adverse effects included overstimulation, restlessness, dizziness, insomnia, euphoria, dysphoria, tremor, nervousness, drowsiness, mydriasis, and blurred vision. In addition, diethylpropion can decrease the seizure threshold, subsequently increasing a patient’s risk for an epileptic event.
Other organ systems also can adversely be affected, resulting in tachycardia, elevated blood pressure, palpitations, dry mouth, GIT disturbance, impotence or change in libido, gynecomastia, and bone marrow suppression.
Contraindications:
Patients with pulmonary hypertension, advanced arteriosclerosis, severe hypertension, hyperthyroidism, agitated states, or glaucoma.
Because diethylpropion is related to the amphetamines, the potential for abuse is high; therefore, its use is contraindicated in patients with a history of substance abuse.
As with phentermine, use of diethylpropion should be avoided in patients concomitantly receiving or having received an MAOI within the preceding 14 days to prevent hypertensive crisis.
Diethylpropion
Adverse effect:Use of diethylpropion for a period longer than 3 months is associated with an increased risk for development of pulmonary hypertension.
common CNS adverse effects included overstimulation, restlessness, dizziness, insomnia, euphoria, dysphoria, tremor, nervousness, drowsiness, mydriasis, and blurred vision.
Other organ systems also can adversely be affected, resulting in tachycardia, elevated blood pressure, palpitations, dry mouth, GIT disturbance, impotence or change in libido, gynecomastia, and bone marrow suppression.
Diethylpropion
Contraindications:Patients with pulmonary hypertension, advanced arteriosclerosis, severe hypertension, hyperthyroidism, agitated states, or glaucoma.
Because diethylpropion is related to the amphetamines, the potential for abuse is high; therefore, its use is contraindicated in patients with a history of substance abuse.
As with phentermine, use of diethylpropion should be avoided in patients concomitantly receiving or having received an MAOI within the preceding 14 days to prevent hypertensive crisis.
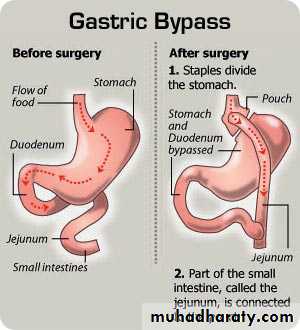
Surgical Intervention
Weight reduction (bariatric) surgery is an option for patients whose BMIs are 40 kg/m2 or greater, or 35 kg/m2 or greater in the presence of other comorbid conditions and who have failed more conventional approaches to weight loss.Surgery is warranted when other treatment attempts have failed in severely obese patients (BMI of 40 kg/m2 or greater, or 35 kg/m2 or greater with obesity-related risk factors).Surgical Intervention
There are two basic surgical techniques:
• gastric bypass—the full partitioning of the proximal gastric segment into a jejunal loop of the intestine—whereby weight loss is induced through both malabsorption of food and limited gastric capacityfigure below
• gastroplasty—incomplete partitioning at the proximal gastric segment
OUTCOME EVALUATION
Successful management of overweight and obesity is determined by the ability the treatment plan has to(a) Prevent weight gain
(b) Reduce and maintain a lower body weight,
(c) Decrease the risk of obesity-related comorbidities.