Objective
Review bilirubin pathway or metabolismExplore risk factor for neonatal jaundice
Outline causes of indirect hyperbilirubinemia
Outline causes of jaundice in 1st 24 hr of life and that persist more than 2-3 week
Distinguish between physiological vs pathological jaundice
Distinguish between breast milk vs breast feeding jaundice
Be able to diagnose kernicterus , discover risk factor and make prevention
1
Yellowish discolouration of skin and sclera because of increase serum level of bilirubin
indirect (unconjucated ) ordirect (conjucated )
occur in 60% of term infant &
80% of preterm infant
2
Neonatal jaundice
3
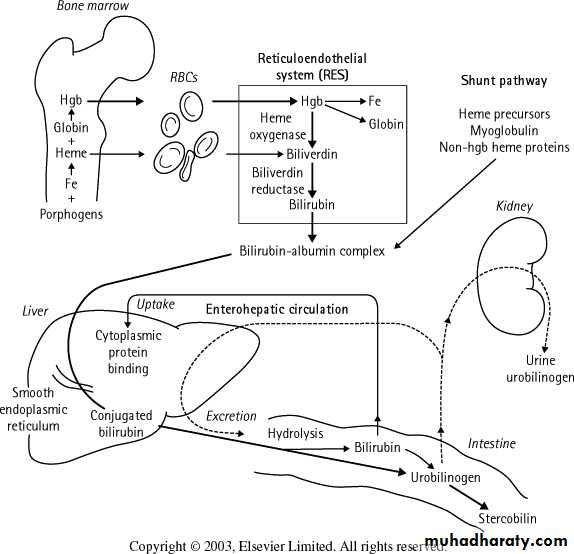
• Bilirubin derived from of heme containing proteins
• 75% of heme from senescent RBC Hb in RE system• 25% of heme from Hb of ineffective erythropoiesis in the BM & from myoglubin , cytochromes , catalase & free heme .
bilirubin metabolism
4Bilirubin metabolism
5Heme oxidized by heme oxygenas biliverdin which
reduced by biliverdin reductase indirect (unconjucated) bilirubine which is water insoluble (not excreted in urin )
bind to albumin. This albumin binded bilirubin is not toxic to CNS .
When binding sites become saturated with bilirubin if
free unconjucated bilirubin high or
competative compound as sulfonamide , & FFA ,these will lead to increase free bilirubin which may enter CNS & causing toxicity & kernicterus
6
indirect bilirubin dissociated from albumin at hepatocyte where bound to cytoplasmic ligandin (Y protein ) for transport to smooth endoplasmic reticulum
( phenobarbitone increase ligandin in endoplasmic reticulum that decrease bilirubin ).
Conjucation will occur in liver when indirect bilirubin converted by UDPGT (Uridin Diphosphate Glucuronyl Transferase) forming
direct bilirubin ( monoglucuronide & diglucuronide ) which is water soluble capable of biliary & renal excretion .
UDPGT & ligandin is lower in the new born
• ( especially preterm ) that increase bilirubin .
7
Conjugated bilirubin is excreted by the biliary tree & enters GIT
where some of it metabolised by colonic bacteria to form urobilinogen and then stercobilinogen, which may be further oxidized to stercobilin that give feces its brown color.
some of the urobilinogen is reabsorbed & excreted in the urine where some of it further oxidize to urobilin which gives urine it characteristic color
8
Some of the conjugated bilirubin in GIT may be reconverted to unconjugated bilirubin by intestinal bilirubin glucuronidase then again reabsorbed go back to liver ,this is called enterohepatic circulation . That increase indirect bilirubin
Enterohepatic circulation increase in some new born & in patients with pyloric stenosis, intestinal Atresia, meconium ileus , Hirschprung`s disease & decrease oral intake . but it decreased by intestinal bacteria
Risk Factors for Development of Severe Hyperbilirubinemia in Infants of 35 or More Week's Gestation
Major risk factors
Jaundice observed in the first 24 hr
Blood group incompatibility, other hemolytic disease
Gestational age 35–36 wk
Previous sibling received phototherapy
Cephalohematoma or significant bruising
Exclusive breast feeding, if nursing is not going well and weight loss is excessive
East Asian race
9
Risk Factors for Development of Severe Hyperbilirubinemia in Infants of 35 or More Week's Gestation
Minor risk factors
Gestational age 37–38 wk
Jaundice observed before discharge
Previous sibling with jaundice
Macrosomic infant of a diabetic mother
Maternal age ≥25 yr
Male gender
10
Risk Factors for Development of Severe Hyperbilirubinemia in Infants of 35 or More Week's Gestation
Decreased risk
Gestational age ≥41 wk
Exclusive bottle feeding
Black race
11
12
1. Physiolgical jaundice ( most common )2. Breast milk jaundice3. Over production (hemolysis ) include :-
Blood group incomp. ( Rh , ABO , subgroup as kell, Duffy )
RBC enzyme defect as G6PD deficiency , pyruvate kinase deficiency.
Herditory spherocytosis, elliptocytosis
Hb pathy (alpha thalasemia )
Acquired hemolysis (infection , drug vit K sulfonamide )
Extravascular bleeding as (peteache , hematoma , pulmonary cerebral ,or occult hemorrhage
Polycythemia as materno-fetal or feto-fetal transfusion , delay clamping of umbilical cord .
Indirect (unconjugated ) neonatal hyperbilirubinemia
13• Increase enterohepatic circulation as pyloric stenosis , meconium plug syndrom , hirschsprung disease , intestinal atresia or stenoses including annular pancreas, fasting or hypoperistalses, drug induce paralytic ileus, swallowed blood .
• damages or reduces the activity of the transferase enzyme or other related enzymes (hypoxia, infection, thyroid deficiency , genetic deficiency as Crigler najjar , also inhibition of conjugation by drug
• Decrease bilirubin uptake across hepatocyte due to competitive inhibition as drug or breast milk jaundice. Miscellaneous as hypothyroidism , hypoxia, acidosis
• Miscellaneous as sepsis, UTI ,hypoglycemia , infant of diabetic mother .
• drug such as oxytocin
• It is the most common cause of jaundice in the neonatal period ,
it is usually appear in
• 2nd or 3rd day of life in full term infant &
• 3rd or 4th day in premature
Level reach Peak
• usually (6-8 mg/dL ) & not > 12 mg / dL in 3rd day in full term
• and usually (10-12 mg/dL) & not > 15 mg/dL in 5th day in preterm .
14
Physiolgical jaundice
• usually disappear
• by 4 – 5 days ( rarely by 7 -10 days ) in full term• & usually by 7 - 9 days ( rarely by 10 days - 2wk ) in preterm .
• Increase of bilirubin should be not > 5mg/dL/ 24 hr
• or not > o.5 mg/dL/hr15
Physiolgical jaundice
16
causes
increase production of bilirubin due to increase RBC volume per kilogram & decrease RBC survival (70-90 ) days in infant versus 120 days in adult . and also increase ineffective erythropoiesis and increase turn over of non hemoglobin heme proteins .
increase enterohepatic circulation by high level of intestinal glucuronidase, decrease intestinal bacteria , decrease gut motility with poor evacuation of bilirubin laden meconium .
defective uptake of bilirubin from plasma by decrease ligandin
defective conjucation due to decrease of UDPG-T
decrease hepatic excretion of bilirubin .
17
Physiological jaundic may be exaggerated ( increase peak & duration )
when there is a risk factors as ; breast feeding , male sex , cephal hematoma , cutanouse bruising , polycythemia , weigh loss , dehydration , caloric deprivation , delay bowel movement , maternal DM , drug ( K3 , novobiocin oxytocin ), trisomy
Treatment
Self limitingEnsure feeding
Good follow up of jaundice and TSB level for abnormal increase or abnormal clinical finding that indicate pathological jaundice
18
The jaundic should not regarded as physiological and should regarded as pathological and should be investigated if
• It appeare in the 1st 24 houre
• TSB increasing > 5mg/dL/ 24 houre or > o.5 mg/dL/houre• TSB >12 mg /dL in full term or >14mg/ dL in preterm .
• Duration of jaundice > 10-14 days
• Jaundice appears excessive for infant's age or rising rapidly crossing percentiles
• Direct B >2 mg/ dL or pale stool, dark urin +ve bilirubin.
19
Cont.
• Sick infant or associated with vomiting lethergy poor feeding Weigh loss, apnea bradycardia hypothermia or When there is pallor ,Hsmegally ,• sign of kernicterus ,
• family History of hemolytic disease ,
• TSB concentration approaching exchange levels or not responding to phototherapy
• jaundice present at or beyond age 3 wk
20
21
Jaundice in the 1st 24 hours
• Erythroplastosis fetalis (hemolysis); ABO & Rh . other cause of hemolysis as G6PD , PK def , spherocytosis
• Concealed hemorrhage (cephal haematoma ,hepatic & spleenic - hemorrhage
• Sepsis .
• Congenital infection (CMV, Rubella, Toxoplasmosis
• Crigler najjar
22
• Prolonged jaundice duration more than 2 weeks & may persist in and beyond 1st month (pathological ) causes include
• Hemolysis
• Hypothyroidism
• Crigler najjar
• Breast milk jaundice .
• Intestinal obstruction , Pyloric stenosis
• idiopathic neonatal hepatitis
• Hyperalimentation .
• Hepatitis, CMV, Syphilis & toxoplasmosis , TORCH
• Galactossaemia .
• Biliary atresia .
• Inspissated bile syndrome follow hemolytic
23
one of the causes of prolonged neonatal unconj hyperB .
when patient may or may not has as physiological jaundice at beginning develop significance elevation of bilirubin between 1st & 2nd week (usually after 7th day ) of life reach maximum10-30 mg/ dL ( rarely more than 20 mg/dL ) during 2nd-3rd week.
The cause is unclear but in some the milk contain glucuronidase, that increase enterohepatic circulation .
if breast feeding continue the jaundice persist for 3-10 weeks at lower level ,
if we stop breast feeding there is rapid decrease reach normal within few days with out return when re-start breast feeding
Breast milk jaundice
24
Befor Dx of BMJ we have to exclude other causes of unconj hyperB as hemolysis ,hypothyroidism , sepsis .
treatment , stop breast feeding for 1-2 days .
some times phototherapy may be needed,
very rarely kernicterus has been reported
This breast milk jaundice should be distinguished from breast-feeding jaundice
Breast milk jaundice
breast-feeding jaundiceearly-onset, exaggerated phyasiolgical unconjugated hyperbilirubinemia, in 1st week of life, in breast-fed infants which may be due to
decreased milk intake with dehydration and/or reduced caloric intake.
giving glucose water (low calories ).
Prevented & reduce by frequent breast-feeding , night feeding, discouraging 5% dextrose or water supplementation .
25
26
Familial Non Haemolytic Uncojucated Hyperbilirubinaemia :( inherited deficient conjugation of bilirubin )
It is a group of inherited disease associated with different degrees of decrease in hepatic UDPG-T
Crigler Najjar type 1 syndrome abscence enzyme
Crigler Najjar type 2 syndrome partial defect in hepatic enzyme
27
Rare , transmitted as AR
clinically presented with severe unconj. Hyperbilirubinaemia with no hemolysis , develop in 1st 3 days of life which may reach 25 – 35 mg /dL during the 1st month & may continue after that .
kernicterus is a common complication .
absence of UDP-GT
Crigler Najjar type 1 syndrome
28
• Highe level of unconj. Bilirubin with no hemolysis
• No rseponse to phenobarbitone ( differentiated from type 2 )• Definitive Dx is established by measuring hepatic glucuronyl transferase activity in liver specimen .
• DNA Dx .
Diagnosis is based on
29
• Neonatal period may need continuous phototherapy & repeated exchange transfusion to prvent K . Even after neonatal period
• Cholestyramine or agar used to bind photobilirubin product & thus interfere with enterohepatic circulation .
• Rx of infection or any illness to prevent development of K
• Plasmaphoresis
• Metacloporphyrin can used to prevent heme oxygenase.
• Genetic engineered enz. Replacement
• hepatic transplant cure disease .
• Liver direct gene therapy
TREATMENT
30• It is AR , partial defect in hepatic UDPG-T, may be present similar to Type 1 or may be less severe even occasionally without neonatal manifestation .
• TSB range may compatible with physiological or pathological level ,
• Kernicterus is unusual
• Jaundice respond dramatically to phenobarbital
Crigler Najjar Syndrome Type 2
31
K. is a neurological syndrom result from the deposition of indirect B. in the brain cell especialy basal ganglia . when B. exceed B. Binding capacity of albumin ,free B. will cross B.B.B & diffuse to brain cell & cause cell damage & K.
The precise level of indirect B. which is toxic to the brain & duration of exposure was unknown
K is unusual & rare in healthy full term at B.< 25 mg/dL with no hemolysis .
Kernicterus
biIlirubin encephalopathy32
There is some risk factor that increase possibility of K. at lower level of B.which may damage B.B.B. or decrease B. binding capacity of albumin as
Hemolysis , hyperosmolality , IVH acidosis, hypoalbuminemia , FFA , hypothermia, drug ,hypoglycemia, hypoxia , sepsis, asphyxia , meningitis , prematurity
so for example premature LBW infant develop K. at lower B. level than 20-25 mg/dL or even 10mg/dL in VLBW.
33
Onset usually in the 1st wk of life, Signs & symptoms of K. usually appear at 2 –5 days in full term & 7th day in premature but it can occur at any time in neonatal period .
The early signs include poor feeding , lethargy , loss of moro reflex , hypotonia ,high pitch cry , irritability .
These signs are usually indistinguishable from sign of sepsis , asphyxia , hypoglycemia & intracranial Hemorrhage . early
Clinical manifestation
Then 2–3 days after the initial phase at end of 1st week & 2nd week the patient become severly ill , respiratory distress , bulging fontanelle , hypertonia , opisthotonos, retrocollis, shrill high pitch cry , convulsion .
34
35
Many infant who reach this stage are die & most of survival uaually develop later complete neurological syndroms but may appear to recover for 2–3 month (appear with little abnormality )
Later in the 1st year opisthotonos , muscle rigidity , irreguler movement , hypertonia , & convulsion .
36
Then gradual develoment of complete neurological syndrom which include
chorioathetosis , involuntary muscle spasm , extrapyramidal signs , fit , MR , dysarthritic speech , deafness , spastic quadriplegia , teeth discoloration , enamel dysplasia .PREVENTION.
Early Screening and follow-up any newborn after delivery and after discharge for hyperbilirubinemia & presence of risk factors by Hx , examination and lab on needearly measurment & follow up of serum bilirubin level in any jaundiced neonate treatment accordingly.
avoid (visual) assessment but ( by lab )
1st 24 hr jaundiced must evaluated for possible hemolytic disease .
37
PREVENTION.
Parental communication about infant's skin color & education about potential risks and neurotoxicity
Mothers should be advised to nurse infant every 2–3 hr in order to ensure adequate hydration and caloric intake
avoid supplementation glucose and water
Treatment of condition that increase risk of K. like sepsis , acidosis , asphyxia ,IVH ….etc .
Prevention of Rh isoimmunization where Any pregnant Rh –ve woman giving her human Anti D globuline when she delivered Rh +ve baby or develop abortion.
38