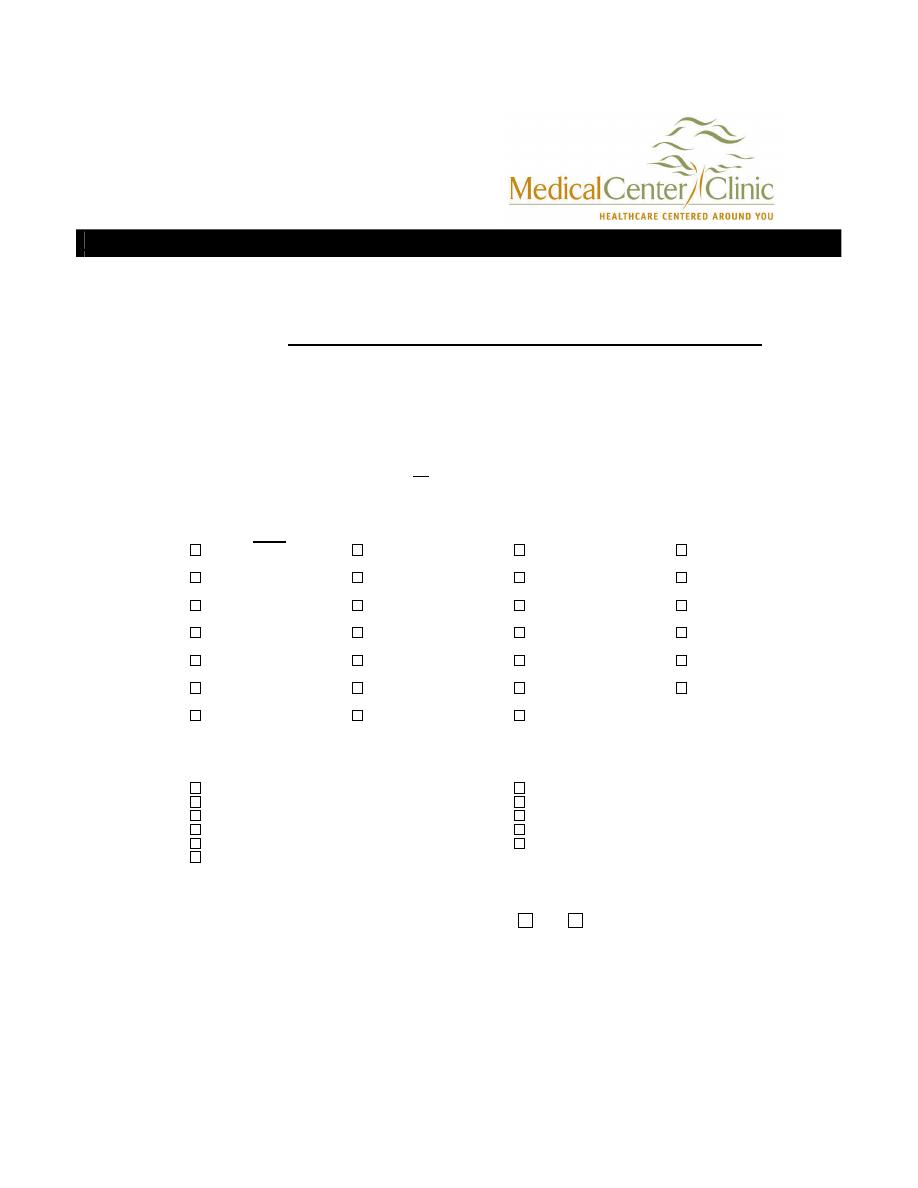
ENT History Form Max Kattner, M.D. ● Derek Jones, M.D.
NAME:
___________________________________________________
Each of the following items is important in helping us find out about and treat the illness that
brought you to see us. Please answer each question as completely and accurately as you can. If
you are unsure about a question, please as one of our medical staff to clarify it.
Chief Complaint:
1. In a few words, please describe why you are seeing the doctor today:
_________________________________________________________________________________________
2. How long have you had this problem?
___________________________________________________
3. Were you referred by another physician:
___________
Name:
______________________________
**If you have a Primary Care Physician, who is not the referring physician, please provide us with his/her name and
address, also:_________________________________________________________________________________
Past History:
4. Have you ever had any of the following: (please check all that apply)
high blood pressure
heart attack
abnormal heart rhythm
stroke
heart failure
heart murmur
seizures
asthma
syncope/fainting spells
kidney disease
liver disease/jaundice
cancer (type___)
hepatitis
thyroid problems
pneumonia
anemia
tuberculosis (TB)
arthritis
acid reflux
latex allergy
diabetes
blood transfusion
bleeding problems
depression
radiation treatment
substance abuse
deep vein thrombosis/ blood clots
Other conditions you have been treated for?_____________________________________________________
5. Have you ever had any of the following surgeries
(place approximate date of surgery in blank)
:
Tonsillectomy and/or Adenoidectomy____________
Thyroidectomy__________________________
Tympanostomy (Ear) tubes_____________________
Knee or Hand Surgery (circle)______________
Nose or Sinus Surgery________________________
Neck or Back Surgery (circle)______________
Open Heart Surgery__________________________
Wisdom Teeth Extracted__________________
Gall Bladder________________________________
Other ENT Surgery ______________________
Hysterectomy_______________________________
Please list all other
surgeries:_______________________________________________________________
Have you ever had problems with anesthesia?
Yes
No
6. Allergies to
medications:_____________________________________________________________
7. Medications (please include non-prescription medications, such as aspirin, herbal
treatments, and vitamins, that you take on a regular basis):
No medications- go to next question
Name
Reason for taking
_________________________________________________________________________________________
_________________________________________________________________________________________
_________________________________________________________________________________________
_________________________________________________________________________________________
_________________________________________________________________________________________
(For additional medications, please write on the back of this page or provide a complete list)
8.
Are immunizations/ vaccines up to date?
Yes
No
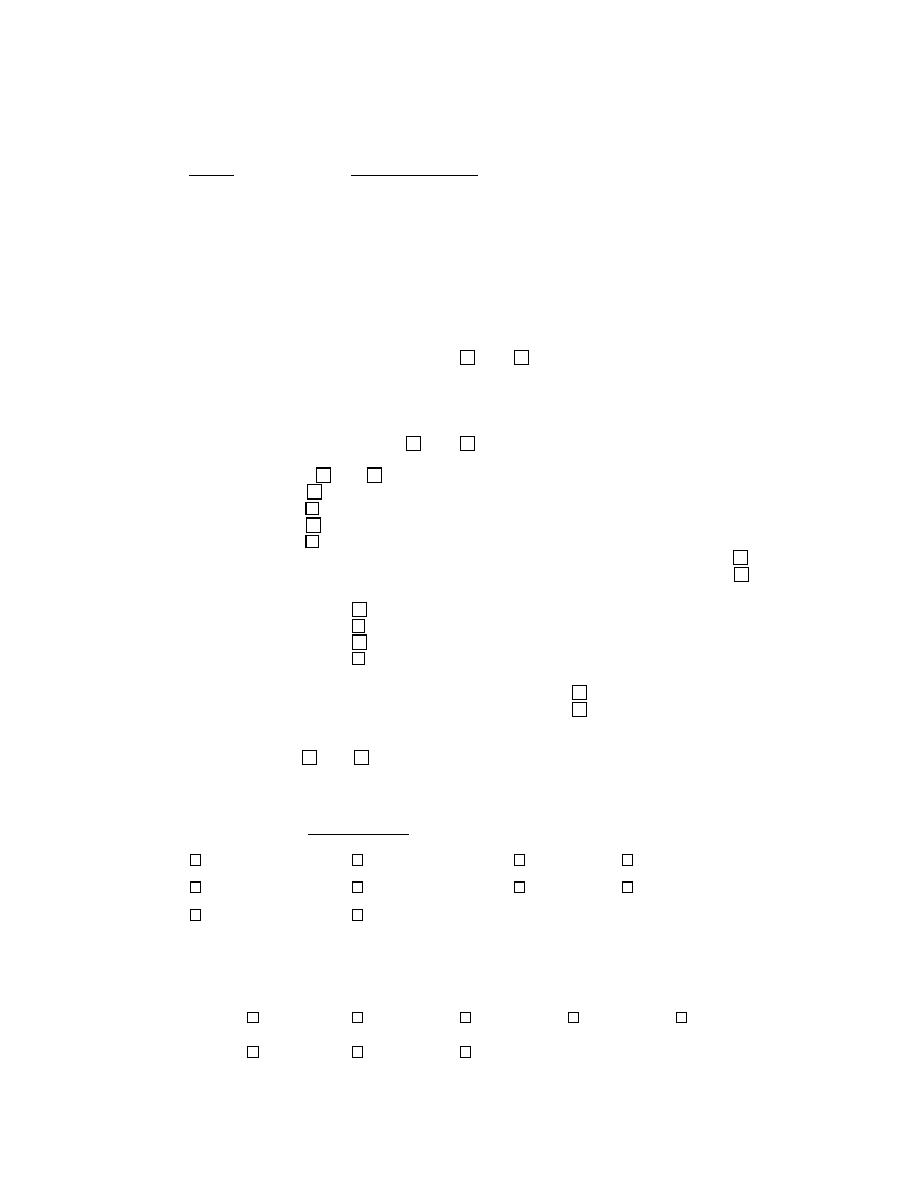
Social History:
9.a. Occupation
_________________________________________ Marital Status: Single_____ Divorced_____
b. Is the child in Daycare?
Yes
No
Married____ Widowed_____
10. Do you live alone?
Yes
No If No, who lives with you?
______________________
11. a. Do you smoke?
No, I never smoked
No, I quit__years ago. At that time, I was smoking packs per day for __years.
Yes, I smoke cigars or a pipe
Yes, I’ve smoked_______packs of cigarettes per day for _____years
b
.
Are you exposed to smoke from other members of your family on a daily basis?
Yes
No
12. a. Do you drink alcohol?
No, never (rarely)
No, but I used to
Yes, Daily 1 or more times a week
Yes. 1 or more times a month
b
.
Have you had a problem with alcoholism in the past?
Yes
No
13. Are you at risk for AIDS/ HIV/ Hepatitis (e.g. sexual orientation, drug abuse, previous
blood transfusions)?
Yes
No If Yes, who lives with you?
_____________________________
Family History:
14. Do you have any blood relatives who have any of the following conditions?
heart disease
problems with anesthesia
diabetes
allergies
high blood pressure
bleeding problems
asthma
stroke
cancer (type___)
hearing loss
Review of Systems:
15. Please check all symptoms which you have now:
General:
fatigue
chills
fever
night sweats
weight loss/gain
Eyes:
change in vision
double vision
wear glasses
Ears:
hearing loss
ear pain
ear drainage
ringing
dizziness
Nose:
nasal congestion
nasal bleeding
nasal drainage
sinus pain
Throat:
change in voice
lump in throat
throat pain
difficulty swallowing
Lungs:
shortness of breath
frequent cough
wheezing
coughing blood
Cardiovascular:
chest pain
irregular heart beat
ankle swelling
Gastrointestinal:
heartburn
nausea
vomiting
diarrhea
constipation
vomiting up blood
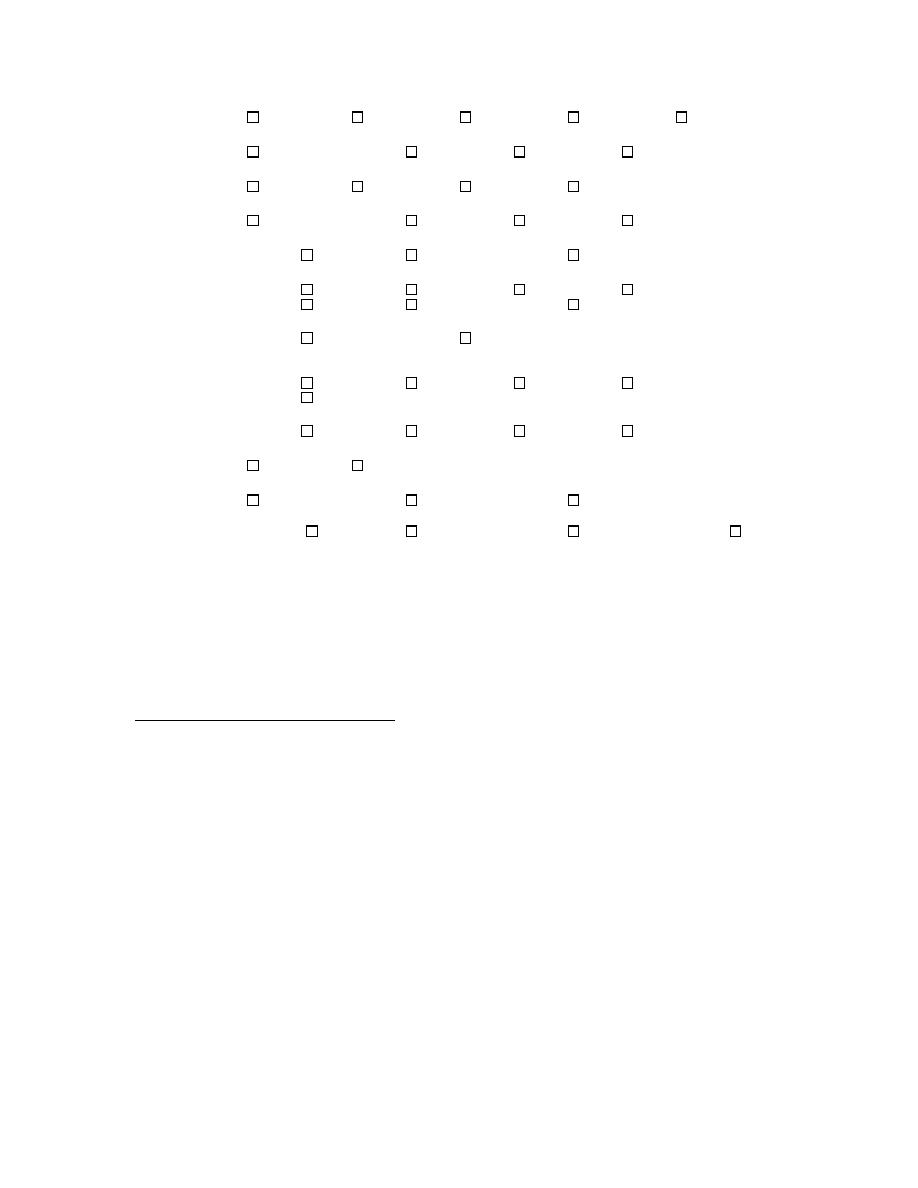
abdominal pain
Genitourinary:
difficulty urinating
blood in urine
Neurological:
depression
memory loss
weakness
numbness
tingling
Musculoskeletal:
back pain
joint pain
arm or leg pain
muscle weakness
Skin:
skin cancer
skin disease
Endocrine:
Increased appetite
excessive thirst
heat/cold intolerance
Allergy/ Immunology:
sneezing
itchy/watery eyes
facial swelling
hives
16. Age
__________
Height
__________
Weight
__________
Approximate Blood Pressure
__________
The above information is to the best of my knowledge.
________________________________
_______________
________________________________
Patient’s signature
Date
Physician’s signature
TO BE FILLED OUT BY THE NURSE:
