Dermatology
For
5
th
stage
http://goo.gl/rjRf4F
I
LOKA
©
http://www.muhadharaty.com/dermatology
I

Content
Topics:
Page:
Dermatological History
3
Physical examination
7
Symptoms and definitions
11
Lesion identification
Specific skin lesions
17
22
See photos @ WWW.muhadharaty.com/lecture/3472
Part1
: Dermatological History
Identifying data:
Age
some lesions or diseases occur in specific age group, infectious diseases are
more common in children but malignancy gets more common with advancing age.
Sex
some conditions are more common in men or more common in women.
Race and country of origin.
Current residence
important in an infectious outbreak.
Occupation.
History of presenting lesion:
Ask when, where and how the eruption or lesions began, about the initial appearance
and what changes have occurred with time.
Note associated features, such as itch and systemic upset, together with aggravating
and relieving factors.
Use SOCRATES to remember what to ask.
"Seven key questions"
When? Onset
Where? Site of onset
Does it itch or hurt? Symptoms
How has it spread (pattern of spread)? Evolution
How have individual lesions changed? Evolution
Provocative factors? Heat, cold, sun, exercise, travel history, drug ingestion, pregnancy,
season
Previous treatment(s)? Topical and systemic.
Duration:
Onset sudden vs. gradual. Establish whether this is an acute presentation or an
ongoing chronic problem.
Previous episodes example: photodermatoses tend to recur every spring with the
onset of good weather.
Change fluctuation vs. persistence. Consider variation in severity - eg, occupational
contact allergic dermatitis may improve when on holiday. Urticaria may be quite
dynamic in its presentation but others are much more static.
Location
:
As well as skin, remember mucous membranes. The site of lesions is important. Eczema
tends to be on flexural surfaces (in adults and older children) whilst psoriasis tends to
be on extensor parts.
Lesions may have a specific distribution - around the genitals, in sweaty regions or sun-
exposed areas. Establish whether the lesion has spread.
Provoking or relieving factors
:
Example:
heat and cold may be either aggravating or relieving factors, especially with
urticaria; repeated drug exposures with fixed drug eruptions.
Associated symptoms
:
Itch some lesions are renowned for being itchy and others for not being so but this
can be misleading. Psoriasis is said to be non-itchy but there may be pruritus in the
genital area.
Tenderness inflammation is often tender.
Bleeding or discharge bleeding may indicate malignancy and discharge may occur
with an infected lesion.
Systemic symptoms such as pyrexia, malaise, joint pain and swelling or weight loss.
Some skin lesions are markers for underlying malignancy.
Response to treatment:
Both patient and doctor initiated.
A number of treatments may have been tried prior to consultation example antiseptic
lotions, calamine, antihistamines, over-the-counter (OTC) steroid or antifungal creams,
herbal remedies or medication prescribed for another family member or friend.
Complementary medicines such as Chinese herbs
may have unknown ingredients and potency.
Partially treated lesions are the most difficult to
diagnose.
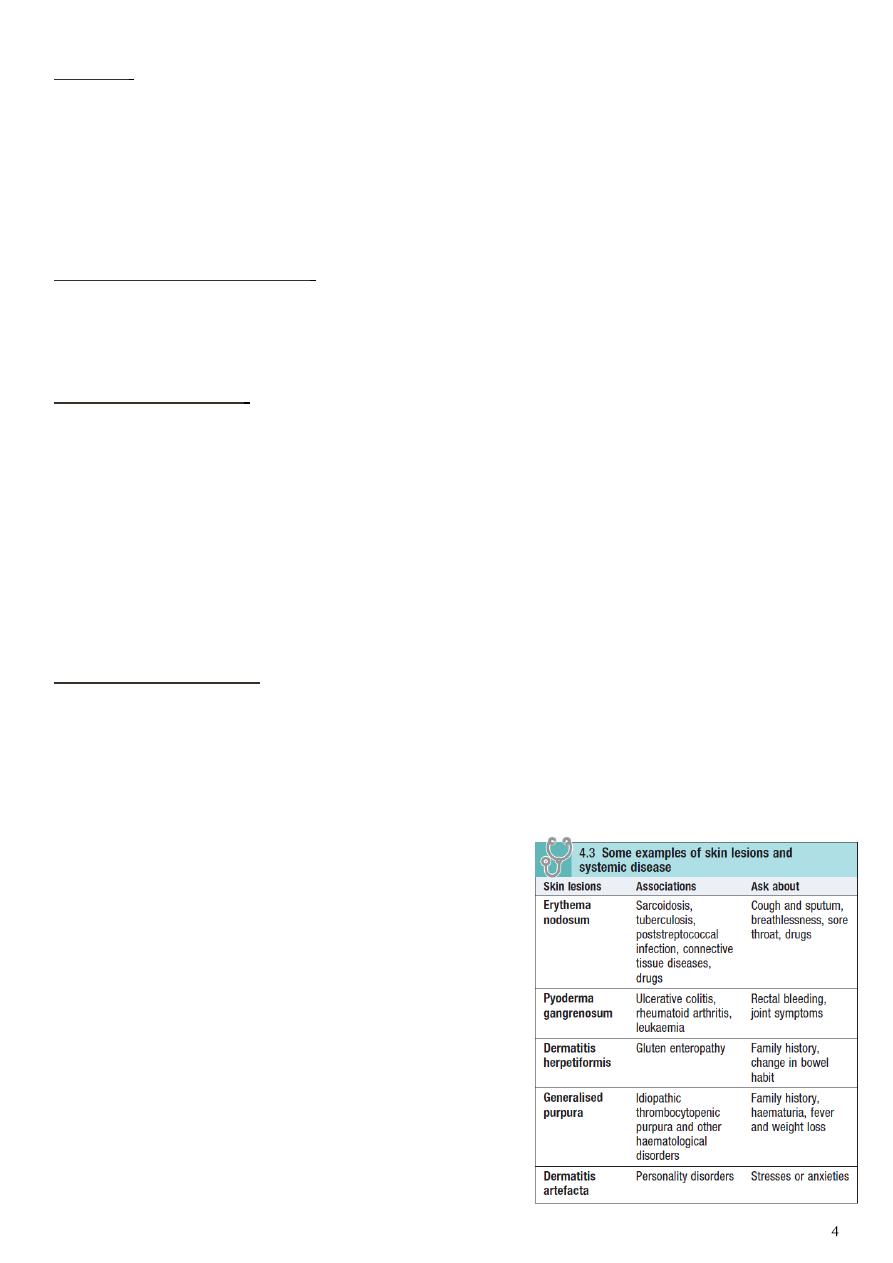
Systemic review:
Psoriasis ask about arthritis.
Verilgu ask about thyroid symptoms.
Eczema ask about asthma.

Past medical history:
Is often relevant - eg, diabetes may suggest necrobiosis lipoidica.
Any skin lesion or systemic diseases like DM may cause ulceration.
Atopic symptoms (hay fever, asthma, childhood eczema).
Surgical history.
Family history:
May indicate a familial trend for the disease.
Other family members will have been given a diagnosis.
A genetic predisposition is important in many diseases, including eczema and psoriasis.
Alternatively, concurrent and recent affliction of other members of the family suggests
a contagious or environmental aetiology.
Familial atypical mole and melanoma (FAMM) syndrome should be considered where
several family members have multiple melanocytic lesions, some atypical, with at least
one case of melanoma in the family.
Is there a family history of malignant melanoma or other skin cancer? A family history
is found in 10% of patients with malignant melanoma.
Psoriasis and atopic eczema also have strongly inherited traits.
Occupation, hobbies and pastimes:
Where there may be exposure to chemicals or a very hot environment.
Chemicals encountered at work or leisure may cause contact dermatitis.
Suspect industrial dermatitis if the eruption improves when the patient is away from
work.
Travel history:
Particularly to exotic locations, may increase the risk of rarer tropical diseases.
Consider cumulative exposure to sunlight or sunbeds and history of sunburn, as these
increase the risk of skin malignancies.
Foreign travel gives exposure to tropical infections or sunlight that could cause a
photosensitive eruption.
Drug history:
Prescribed, over-the-counter or other therapies.
Drug eruptions can be highly variable.
Illegal drug use may have dermatological manifestations - eg, anabolic steroids and
acne.

Allergies example fixed drug eruption occur as a result of drug allergy.
Tetracycline yellowish of skin, nail, teeth.
Medical disorders that may involve the skin Stevens–Johnson syndrome caused by
drugs or have cutaneous features, and prescribed or self-medicated drugs, including
creams and cosmetics.
Personal history:
Does the patient have a fair skin type, i.e. does he burn easily and tan poorly or not at
all? Skin cancers are commoner with a pale skin.
Alcohol use has an association with psoriasis.
Smoking increases the risk of some malignancies and has a close association with
palmoplantar pustular psoriasis.
Sexual history History of risk factors of HIV: blood transfusions, IV drugs, sexually
active, multiple partners, sexually transmitted disease.
Psychological and social sequelae:
People with severe, chronic, visible and disfiguring skin disease may suffer from
anxiety, depression and social isolation, these issues require exploration.
Psychological problems may also cause skin disease - eg, dermatitis artefacta.
Part2
: Physical examination
General settings:
Ensure a warm, well-lit, private place is available.
Offer a chaperone; record the chaperone’s name or if the patient declines the offer.
Note whether the patient looks ill or well. Note whether there any clues as to
systemic illness.
Wipe off any creams, make-up or anything else that may obscure the true nature of
the lesions.
For widespread lesions ask the patient to undress to his underclothes.
Use a hand lens to examine individual lesions.
A dermoscope, using a ×10 magnification illuminated lens system, is helpful for
pigmented lesions
Examine the lesion:
1- Inspection:
Note the position of lesions:
o Consider whether the distribution is symmetrical or asymmetrical. (Symmetrical
distribution suggests an endogenous condition such as psoriasis, whilst
asymmetry is more typical of an exogenous condition such as tinea.) Some rashes
have a characteristic distribution such as with shingles.
o Note whether flexor or extensor surfaces are involved.
o Establish whether there are areas of friction or pressure.
o Note whether sweaty regions are involved.
o Note whether exposed regions are involved.
o Consider whether sexual contact is a factor (consider genital lesions but also the
lower abdomen and upper thighs).
Note the size of the lesion. Measure for accuracy.
Establish whether it is single or multiple.
If a rash exists, consider its morphology. Are individual lesions:
o Macular?
o Papular?
o Vesicular?
o Crusty?
o Urticarial?
Note colour, shape, regularity or irregularity. Note whether areas of inflammation
around it exist. Consider whether the edge is clearly demarcated or poorly defined.
The use of dermatoscopy may aid diagnosis beyond naked eye examination but
should only be used by those with appropriate training.
2- Palpation:
Tenderness.
Warmth.

Site within the skin.
Thickness.
Consistency (hard, soft, firm, fluctuant).
Note whether firm pressure leads to blanching.
Note whether it is friable and whether it bleeds easily.
Scaling - disorders of the epidermis may produce scale, which may be visible, or
gentle scratching of the skin may make it apparent.
If appropriate, look to see if there is any evidence of infestation - eg, scabies' burrows.
Note hair in the local skin and on the head.
Look at the nails.
Note whether mucous membranes are involved. Examine the genitals where
appropriate.
Note regional lymph nodes. This may be relevant for infectious or malignant lesions.
Moles:
If any pigmented lesion (mole) has recently changed, note the distribution of pigment
within it and whether it is inflamed or ulcerated.
Malignant melanoma commonly shows variation in pigmentation and has an irregular
or diffuse edge.
Remember ‘ABCDE’ – Asymmetry, Border irregular, Color irregular and Diameter >6
mm, Enlargement.
Examine the entire skin as abnormal moles are more common in patients with a
malignant melanoma.
Look at:
N
ails on hands and feet.
Different areas of the scalp (ask the patient to point to the problem to localise, then
part the patient’s hair to see).
Mucous membranes.
Examine local lymph nodes in any patient with a potential squamous cell cancer,
malignant melanoma or cutaneous T-cell lymphoma.
Take a skin scraping for microscopy and culture if you suspect fungal infection.
Findings of general examination:
1- General observation:
Distribution of rash
o Symmetrical — extensor, e.g. psoriasis — flexor, e.g. eczema
o Asymmetrical, e.g. granuloma annulare
o Facial, e.g. rosacea, seborrhoeic dermatitis
o Localized, e.g. morphoea
o Widespread, e.g. drug eruption

o Dermatomal, e.g. herpes zoster
o Truncal, e.g. guttate psoriasis
o Sun-exposed, e.g. drugs or SLE
Morphology of lesions macules, papules, vesicles, pustules, bullae, nodules,
plaques.
Configuration of lesions discrete, confluent, linear, grouped, annular.
2- Hands and fingernails:
Pitting in psoriasis and alopecia areata
Ridging in eczema
Fungal infection
Finger web burrows in scabies
3- Face and scalp:
Hair loss
Scalp changes, e.g. psoriasis
‘Butterfly’ rash, e.g. SLE
Central or hairline distribution
Conjunctivitis/blepharitis in rosacea
4- Mouth:
Lichen planus
Herpes simplex
Pemphigus
5- Genitalia:
Psoriasis
Intertrigo
Infestation
Lichen sclerosus
6- Feet and nails:
Pedal pulses
Tinea pedis
Toenail changes, e.g. fungal infection, psoriasis
7- Joints:
Psoriatic arthritis
Connective tissue disease
The Skin Exam:
"from: LearnDerm by visualdx.com"
Preparation First, make sure the patient is in a gown and there is adequate light in
the room.
Examination Carefully examine the entire skin surface, including the scalp, mouth,
eyes, nails, and genitals. You may find lesions related to the presenting complaint or
discover unrelated but important findings.
Palpation Palpate lesions to determine whether they are flat or elevated.

Texture Use a magnifying hand lens if necessary; this can help you determine the
texture of a lesion and evaluate for the presence of scale.
Scale A scalpel blade can be used to gently scrape a lesion to determine if subtle
scale is present. Scale scraped onto a glass slide can be microscopically examined if a
fungal infection is suspected.
Size Measure solitary lesions and record measurements in the patient record.
Follow over time.
Diascopy Differentiate between a blanching erythema and non-blanching purpura
by pressing with a glass slide, a procedure called diascopy.
Weighted seven-point scale for malignant lesions:
Major features of the lesions (score two points each):
o Change in size.
o Irregular shape.
o Irregular color.
Minor features of the lesions (score one point each):
o Largest diameter 7 mm or more.
o Inflammation.
o Oozing.
o Change in sensation.
Suspicion is greater for lesions scoring three points or more but, if there are strong
concerns, any one feature is sufficient to prompt urgent referral.
Investigations:
Swabs These can be taken for bacteriology and virology.
Skin scrapings Skin scrapings for microscopy, Nail clippings, Hair root samples.
Wood's light This is an ultraviolet light (wavelength 360-365 nm) used in a
darkened room. It should be held at least 10-15 cm from the skin and time should be
allowed for dark accommodation to occur. When shone on some fungal infections,
the light causes fluorescence.
Skin biopsy may be used to provide a histopathological specimen to aid diagnosis
and guide further management. Types (Shave and punch biopsy, Punch biopsies,
Excisional biopsies) Biopsy can also be used for immunofluorescence and culture.
Patch and skin prick tests These are used for the investigation of contact allergic
dermatitis and suspected latex and other allergies.
Other tests Blood tests (hematology and biochemistry), Serology, Microscopy,
fungal culture, Doppler studies, Photography.
Part3
: Symptoms and definitions
Terms used to describe skin lesions:
Primary skin lesions:
Macule
A localized area of color or textural change in the skin.
Papule
A solid elevation of skin <5 mm in diameter.
Plaque
A palpable elevation of skin >2 cm diameter and <5 mm in height.
Vesicle
A clear, fluid-filled blister <5 mm in diameter.
Bulla
A fluid-filled blister >5 mm in diameter.
Pustule
A visible collection of pus in a blister.
Abscess
A localized collection of pus.
Wheal
A transitory, compressible papule or plaque of dermal edema, red or white,
indicating urticarial.
Angioedema a diffuse swelling of edema that extend to the subcutaneous tissue.
Nodule
A solid elevation of skin >5 mm in diameter.
Papilloma
A nipple-like projection from the surface of the skin.
Purpura
Extravasation of blood resulting in redness of skin or mucous membranes.
Ecchymosis
A macular red or purple haemorrhage, >2 mm in diameter, in skin or
mucous membrane.
Hematoma: a swelling form gross bleeding.
Burrow
A tunnel in epidermis caused by a parasite, e.g. Acarus in scabies.
Comedo
A plug of sebum and keratin wedged in a dilated pilosebaceous orifice on
the face.
Telangiectasia
Dilated dermal blood vessels resulting in a visible lesion.
Secondary skin lesions:
Scale
Accumulation of easily detached fragments of thickened keratin.
Crust
Dried exudate, e.g. serum, blood or pus, on the skin surface.
Ulcer
A circumscribed area of skin loss extending into the dermis.
Excoriation
A superficial abrasion, often linear, due to scratching.
Erosion
A superficial break in the epidermis, not extending into dermis, heals
without scarring.
Fissure
A linear split in epidermis, often just extending into dermis.
Sinus
a cavity or channel that permit the escape of pus or fluid.
Scar
Replacement of normal tissue by fibrous connective tissue at the site of an
injury.
Atrophy
Loss of epidermis, dermis or both, thin, translucent and wrinkled skin,
visible blood vessels.
Stria
Atrophic linear band in skin, white, pink or purple, from connective tissue
changes.

Other skin lesions:
Callus
Local hyperplasia of horny layer on palm or sole, due to pressure.
Cyst
A nodule consisting of an epithelial-lined cavity filled with fluid or semisolid
material.
Erythema
Redness of the skin due to vascular dilatation.
Freckle
A macular area showing increased pigment formation by melanocytes.
Lichenification
Chronic thickening of skin with increased skin markings, from rubbing
or scratching.
Milium
A small white cyst that contains keratin.
Petechia
A haemorrhagic punctate spot 1–2 mm in diameter.
Symptoms include:
• Rash.
• Itch (pruritus) and sleep disturbance.
• A growth or lump.
• Discharge, crusting and smell.
• Scales falling from the skin or scalp.
• Disfigurement and psychological distress.
• Inability to work or pursue leisure activities, e.g. swimming.
Rashes:
• Distribution patterns:
o Symmetrical or universal eruptions suggest systemic or constitutional causes.
o Asymmetrical rashes that spread from one focus are more likely to be due to
fungal, bacterial or viral infection.
o An itchy rash typically involving the flexures of the popliteal fossa, antecubital
fossa, neck and face occurs in atopic eczema.
o Extensor plaques on elbows and knees, the scalp and the sacrum suggest
psoriasis.
o Face Seborrhoeic dermatitis, Acne vulgaris, Sun damage, malignant tumours
(BCC), Psoriasis.
o Truncal Guttate psoriasis, Pityriasis rosea, Tinea versicolor, Urticaria.
o Peripheral lichen planus, necrobiosis lipoidica, erythema nodosum, vasculitis,
athlete’s foot.
o Sun-exposed (face, the V of the neck or the posterior neck, exposed areas of the
arms and legs) connective tissue diseases (SLE), photosensitising drugs
(thiazide diuretics, NSAID), cutaneous porphyrias or a primary sun sensitivity
condition (polymorphic light eruption or a photosensitive eczema).
o Dermatomal herpes zoster.
• Morphology:
o Monomorphic (all have the same appearance), as in guttate psoriasis.
o Pleomorphic (of differing appearance), as in chickenpox.
• Configuration:

o Linear, grouped, annular (in a ring), or the Koebner phenomenon (an eruption in
an area of local trauma).
o Secondary changes of crusting, erosion and excoriation complicate primary
lesions.
• Duration:
o Actinic keratoses present for several years and slowly increase in number.
o Basal cell cancers develop over 1–2 years and may show ulceration.
o Squamous cell cancers form more rapidly over weeks or months.
• Associated features:
o In a patient with a hand eruption, look for skin lesions elsewhere, e.g. atopic
eczema affecting the antecubital or popliteal fossae or psoriasis on the elbows,
knees orvscalp, and for burrows of scabies between the fingers or genitalia.
o The vulva and penis can be affected by psoriasis but only rarely by eczema.
o Asymmetrical arthritis of large joints and of distal interphalangeal joints is found in
up to 30% of patients with psoriasis.
Causes of severe pruritus:
• Parasites Pediculosis, flea bites, Scabies (Burrows on hands or feet).
• Dermatitis herpetiformis Small blisters on extensor sites.
• Urticaria Intermittent wheals on limbs or trunk.
• Eczema Scaly, crusted, excoriated or lichenified patches.
• Insect bites Linear or grouped patterns of recent onset.
• Lichen planus Typical purplish papules on wrists.
• Generalised itch If no rash, check blood tests for renal, haematological or hepatic
diseases.
• Simplex chronicus.
• Systematic causes obstructive jaundice, chronic renal failure, lymphoma,
carcinoma (bronchial CA), iron deficiency, hypo or hyperthyroidism.
Eczema:
• It is distinctive inflammatory response of the skin.
• Characterized by spongiosis (epidermoloedema) histologically and clinically by
clustered papul-vesicles with erythema and scaling.
• Many cases have multifactorial etiology.
Causes of palmer erythema:
• Dermatosis eczema, psoriasis.
• Increased estrogen pregnancy, coholic cirrhosis.
• Rheumatoid arthritis.
• Shoulder-hand syndrome.
• Polycythemia.

Causes of erythema nodosum:
• Sarcoidosis.
• T.B.
• Streptococcal infection.
• Ulcerative colitis.
• Other infections leprosy, toxoplasmosis.
Causes of mouth ulceration:
• Aphthus ulcers minor, major, herpetiform.
• Squamous carcinoma.
• Herpes simplex.
• Lichen planus and peinphigus.
• Trauma from dentures.
• Behcet's, Reiter's, Stevens-Johnson.
Clinical features of Reiter's syndrome:
• Urethritis, hematuria, sterile pyuria.
• Uveitis, recurrent conjunctivitis.
• Subacute arthritis.
• Balanitis (inflammation of penis).
• Buccal ulcers.
Hair loss (alopecia):
• Diffuse alopecia:
o In common male-pattern hair loss.
o Terminal scalp hairs undergo miniaturisation to vellus hairs.
o This ageing phenomenon is strongly inherited and depends on androgens.
o Age-related hair loss in women is more diffuse.
• Non-scarring diffuse hair loss:
o Hypothyroidism, hypopituitarism.
o Iron deficiency, connective tissue diseases (SLE).
o Postpartum or postmenopausal.
o Drug-induced (cytotoxic agents).
• Localized non-scarring alopecia:
o In alopecia areata there is circumscribed loss of scalp, beard or eyebrow hair.
o Alopecia areata may involve the whole scalp (alopecia totalis) or all body hair
(alopecia universalis).
o Localized hair loss can be caused by fungal infection, hair pulling, traction from
braiding and secondary syphilis.
• Scarring alopecia:
o Burns, severe infections (herpes zoster), lichen planus, SLE permanently scar
the scalp with permanent hair loss.
• Loss of secondary sexual hair:
o In old age, cirrhosis and hypopituitarism, axillary and pubic hair is lost.

Excess hair growth:
• Hirsutism:
o In females with male-pattern growth of terminal hair, including facial and pubic
hair extending towards the umbilicus (male escutcheon).
o In these cases there are other features of virilisation, e.g. male-pattern hair loss,
clitoromegaly or a deep voice.
o Causes:
Pituitary: Acromegaly.
Adrenal: Cushing’s syndrome, virilising tumors, congenital adrenal hyperplasia.
Ovarian: Polycystic ovary syndrome, virilising tumors.
Drugs: Androgens, progestogens.
Idiopathic: End-organ hypersensitivity to androgens.
• Hypertrichosis:
o In males or females with excess terminal hair growth in a non-androgenic
distribution.
o Causes systemic disorder (porphyria cutanea tarda), malignancy, anorexia
nervosa, malnutrition or drugs (ciclosporin, minoxidil and phenytoin).
Common nail changes:
• koilonychia in chronic iron deficiency also the nails become brittle, flat and
eventually spoon-shaped.
• Leukonychia a sign of hypoalbuminaemia (chronic liver disease, nephrotic
syndrome, protein malnutrition, protein-losing enteropathy) .
• One or two splinter hemorrhages are commonly seen under the nails of manual
workers.
• Multiple splinter hemorrhages inbacterial endocarditis.
• Distal nail separation (onycholysis) in psoriasis.
• Dilated capillaries in the proximal nail fold in vasculitic conditions, such as SLE.
• Beau’s lines in severe illnesses ((Beau’s lines are due to arrest of nail growth, are
transverse white grooves)).
Part4
: Lesion identification
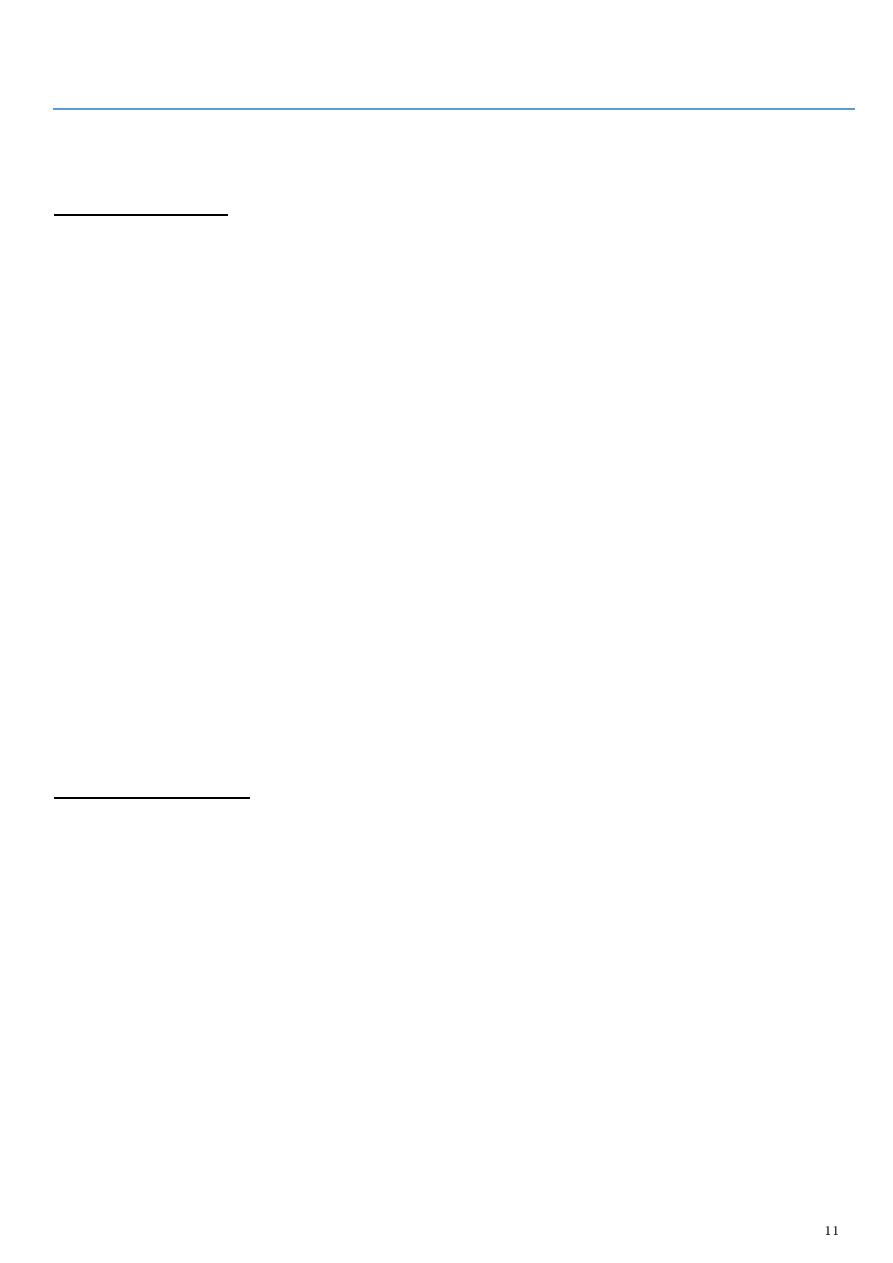
Lesion
Type
Notes
Photo
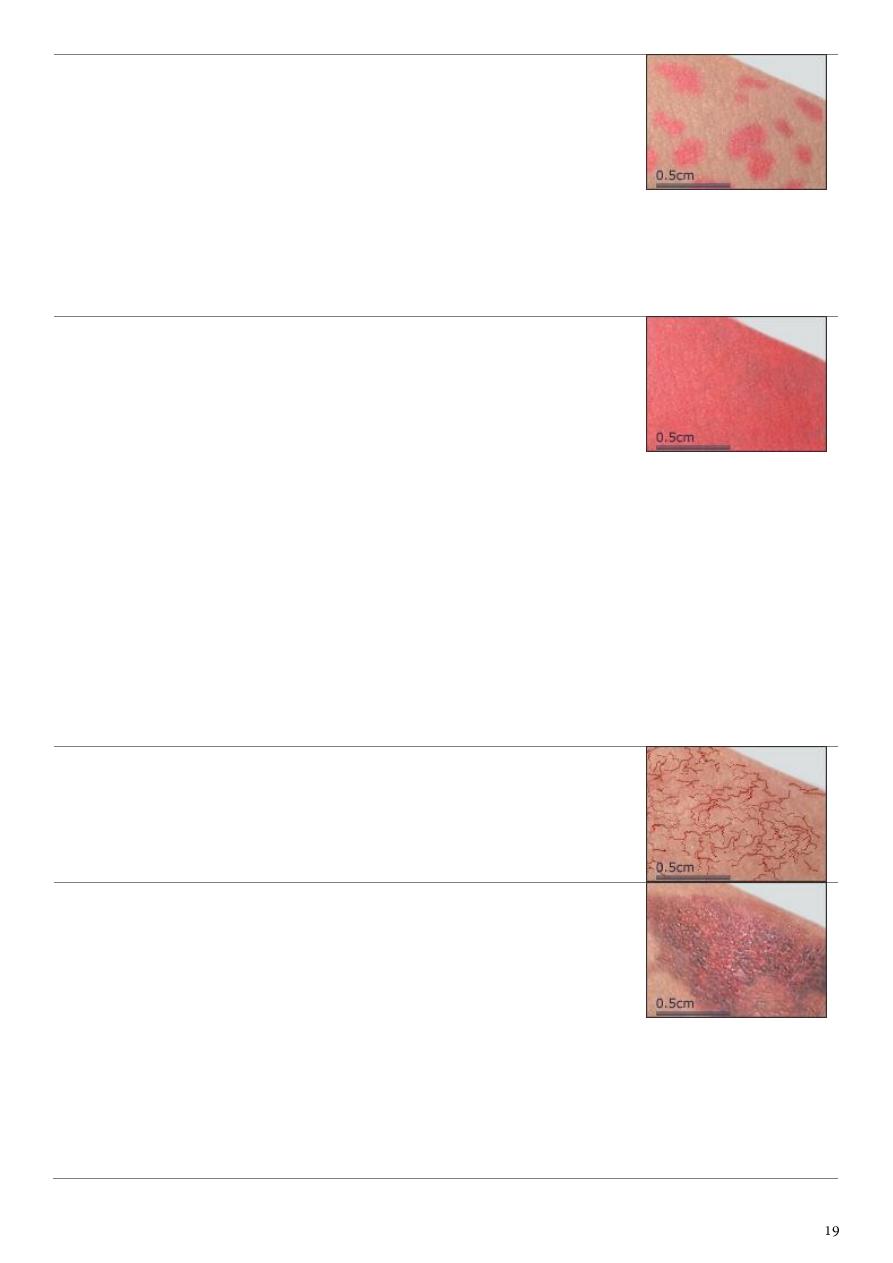
Macule
Flat
A flat, generally less than 0.5-cm area
of skin or mucous membrane with a
color different from that of
surrounding tissue. Macules may have
non-palpable fine scale.
Note: If it is macular, you cannot feel
the involved area. That is, with your
eyes closed, you cannot discern a
boundary to the lesional area.
Patch
Flat
A flat, generally greater than 0.5-
cm area of skin or mucous membrane
with a color different from that of
surrounding tissue. Patches may have
non-palpable fine scale.
Cyst
A closed cavity or sac containing fluid
or semisolid material. A cyst may have
an epithelial, endothelial, or
membranous lining.
Nodule
A
dermal or subcutaneous
firm, well-
defined lesion usually
greater than
0.5
cm in diameter.
Papule
A
discrete, solid
, elevated body
usually
less than 0.5 cm
in diameter.
Papules are further classified by
shape, size, color, and surface change.
Plaque
A
discrete, solid
, elevated body
usually
broader than it is thick
,
measuring
more than 0.5 cm
in
diameter. Plaques may be further
classified by shape, size, color, and
surface change.
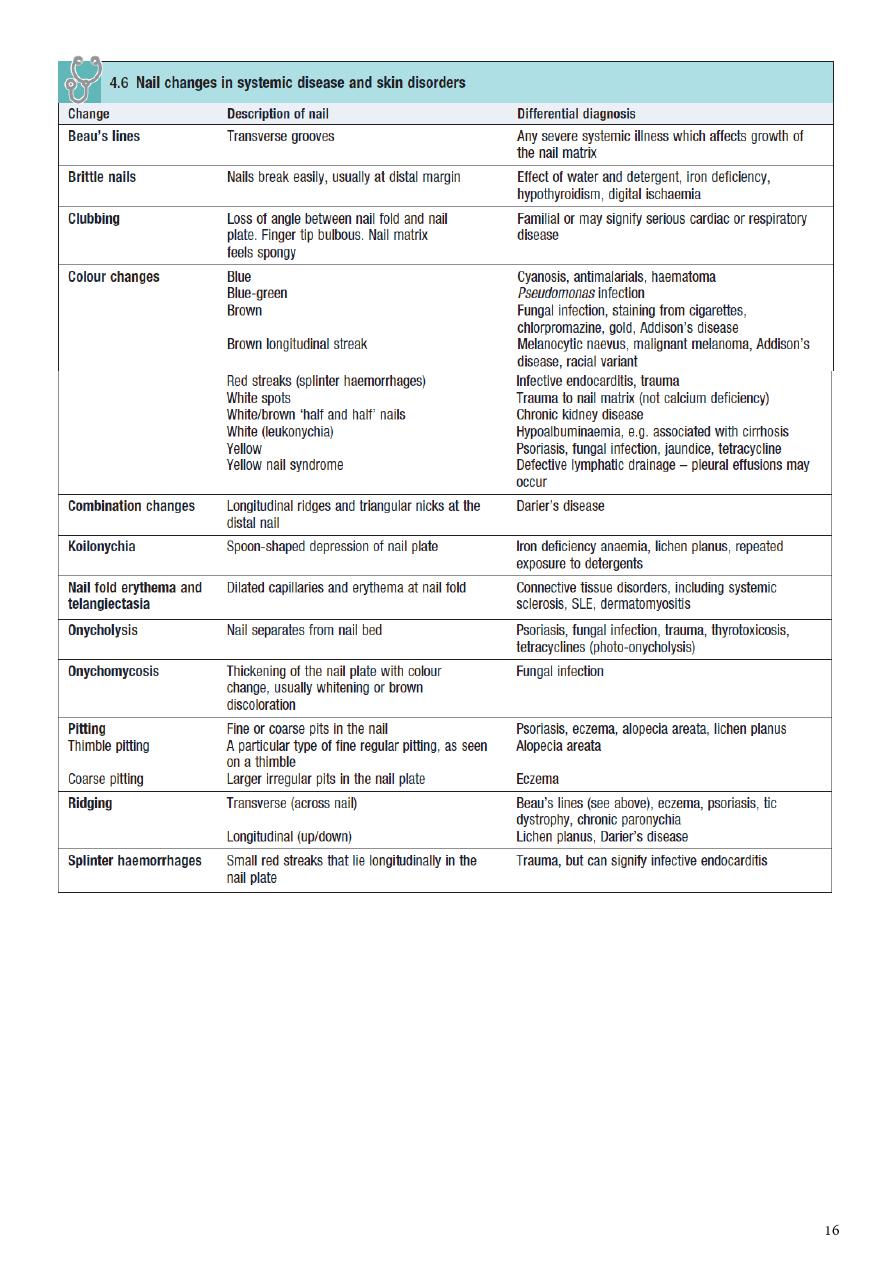
Crust
A hardened layer that results
when serum, blood, or purulent
exudate dries on the skin surface.
Crusts may be thin or thick and can
have varying color.
Crusts are yellow-brown when formed
from serum, green or yellow-green
when formed from purulent exudate,
or red-black when formed by blood.
Scale
A type of surface change. It results
from excess stratum corneum (the
most superficial layer of the skin) that
accumulates in flakes or plates. Scale
usually has a white or gray color.
It is important to note whether a
raised lesion is scaly or non-scaly, as
the differential diagnosis of raised
scaly lesions is quite different from
that of raised smooth lesions.
Bullae
Fluid-filled
blisters
greater than 0.5
cm
in diameter. Fluid can be clear,
serous, hemorrhagic, or pus filled.
Pustule
A circumscribed elevation
that
contains pus
. Pustules are
usually
less than 0.5 cm
in diameter.
Vesicle
A
fluid-filled
cavity or elevation
less
than 0.5 cm
in diameter. Fluid may be
clear, serous, hemorrhagic, or pus
filled.
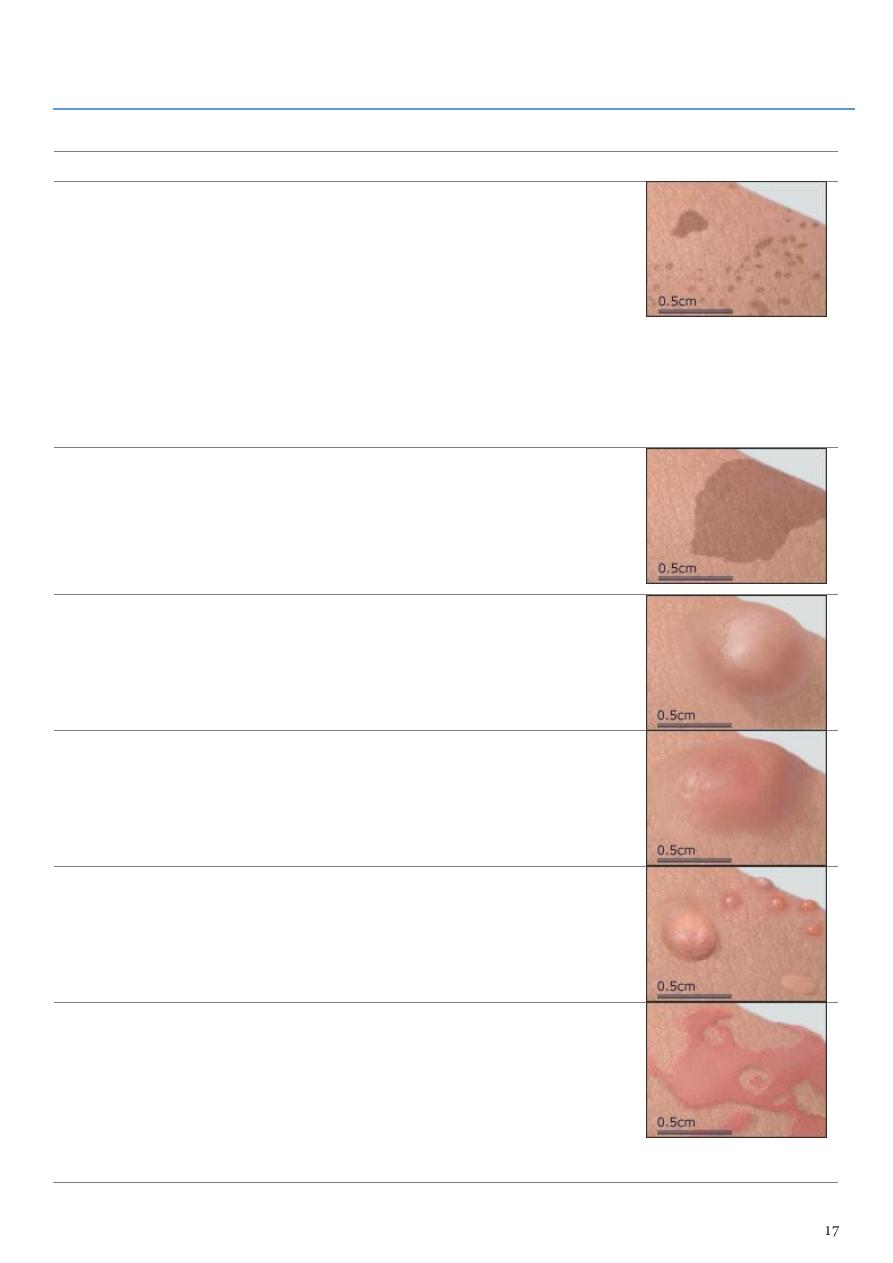
Erythema
Localized, blanchable redness of skin
or mucous membrane.
Erythema and erythroderma will
blanch because the color (ie, redness)
is due to increased blood flow, not
leakage of blood into the skin, as in
purpura.
Erythrode
rma
A generalized, blanchable redness of
the skin that may be associated
with desquamation. Desquamation is
a normal process in which the
cornified (outermost) layer of the
epidermis is sloughed in fine scales or
sheets.
Erythema and erythroderma will
blanch because the color (ie, redness)
is due to increased blood flow, not
leakage of blood into the skin, as in
purpura.
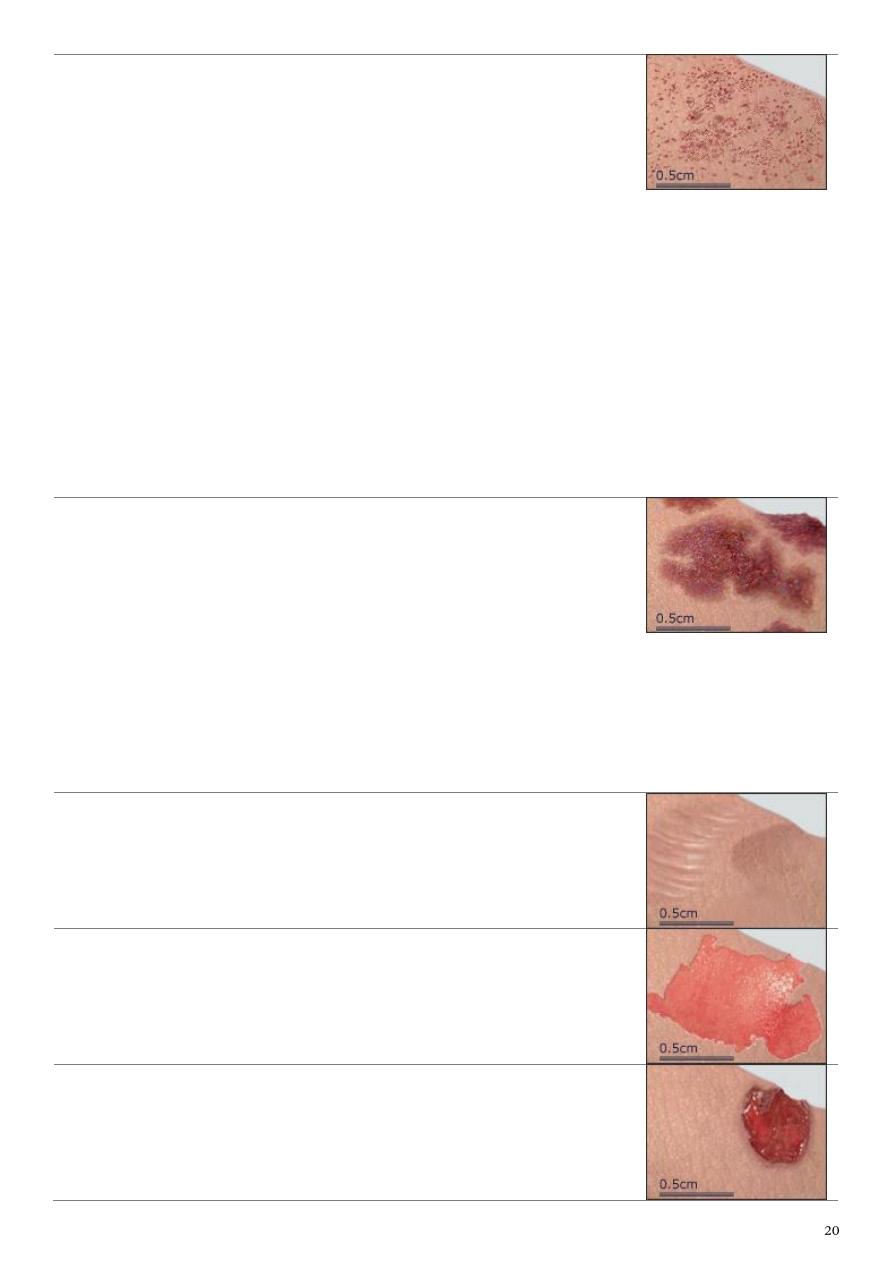
Telangiect
asia
A visible persistent
dilation of small,
superficial cutaneous blood vessels
.
Telangiectasias will blanch.
Ecchymosi
s
Extravasation of blood into the skin or
mucous membranes. Area of flat color
change may progress over time from
blue-black to brown-yellow or green.
Petechiae, ecchymosis, and palpable
purpura do not blanch because blood
has leaked outside the vessels into the
surrounding skin.
Petechiae
Tiny 1-2 mm, initially purpuric, non-
blanchable macules resulting from tiny
hemorrhages.
Purpura can be differentiated from
pigmented lesions by color. Pigmented
lesions are usually brown in color in
comparison to the violaceous color of
purpuric lesions.
Petechiae, ecchymoses, and palpable
purpura do not blanch because blood
has leaked outside the vessels into the
surrounding skin.
Palpable P
urpura
Raised, palpable discoloration of skin
or mucous membrane due to vascular
inflammation in the skin and
extravasation of blood.
Petechiae, ecchymosis, and palpable
purpura do not blanch because blood
has leaked outside the vessels into the
surrounding skin.
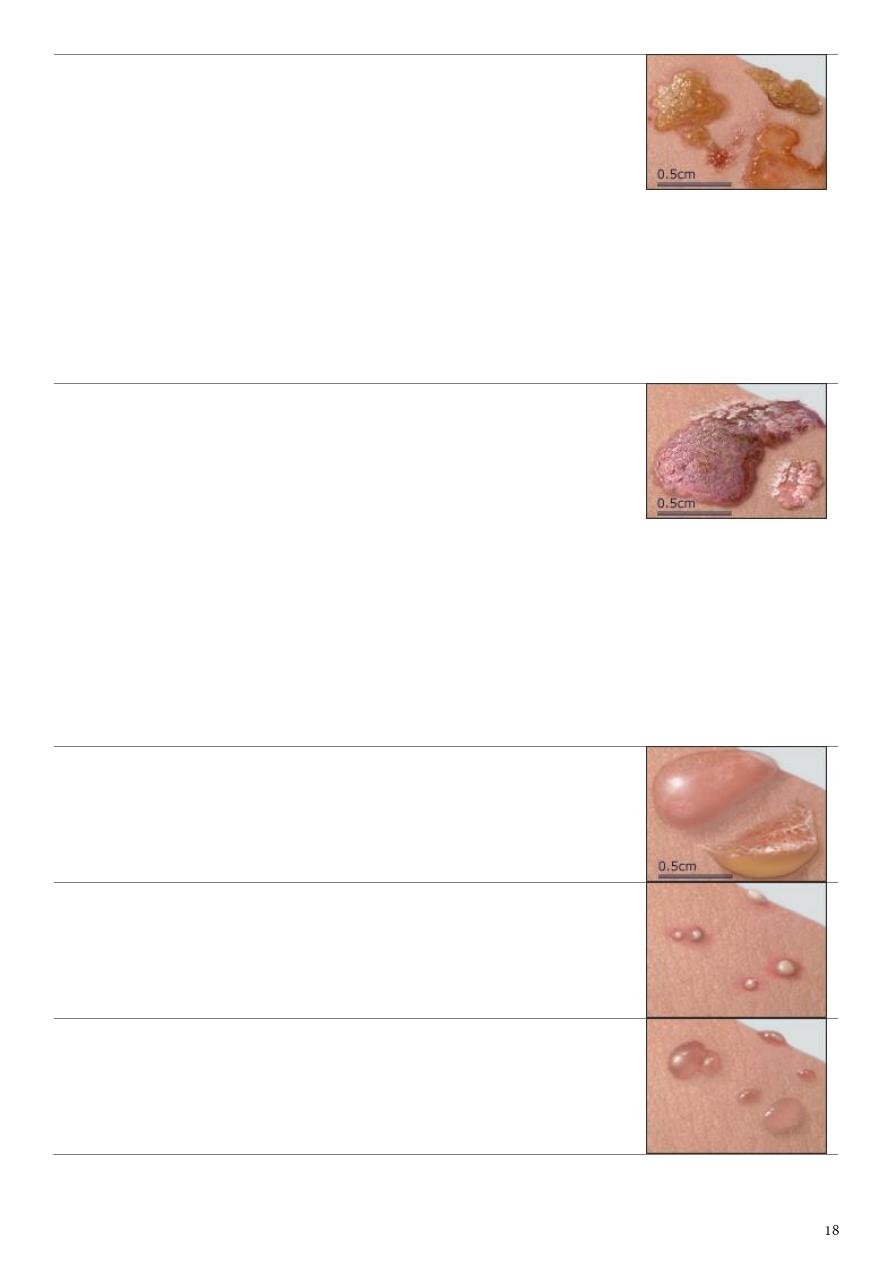
Atrophy
A
thinning
of tissue defined by its
location, such as epidermal atrophy,
dermal atrophy, or subcutaneous
atrophy.
Erosion
Localized
loss of the epidermal or
mucosal epithelium
.
Ulcer
A circumscribed
loss of the epidermis
and at least the upper dermis
. Ulcers
are further classified by depth,
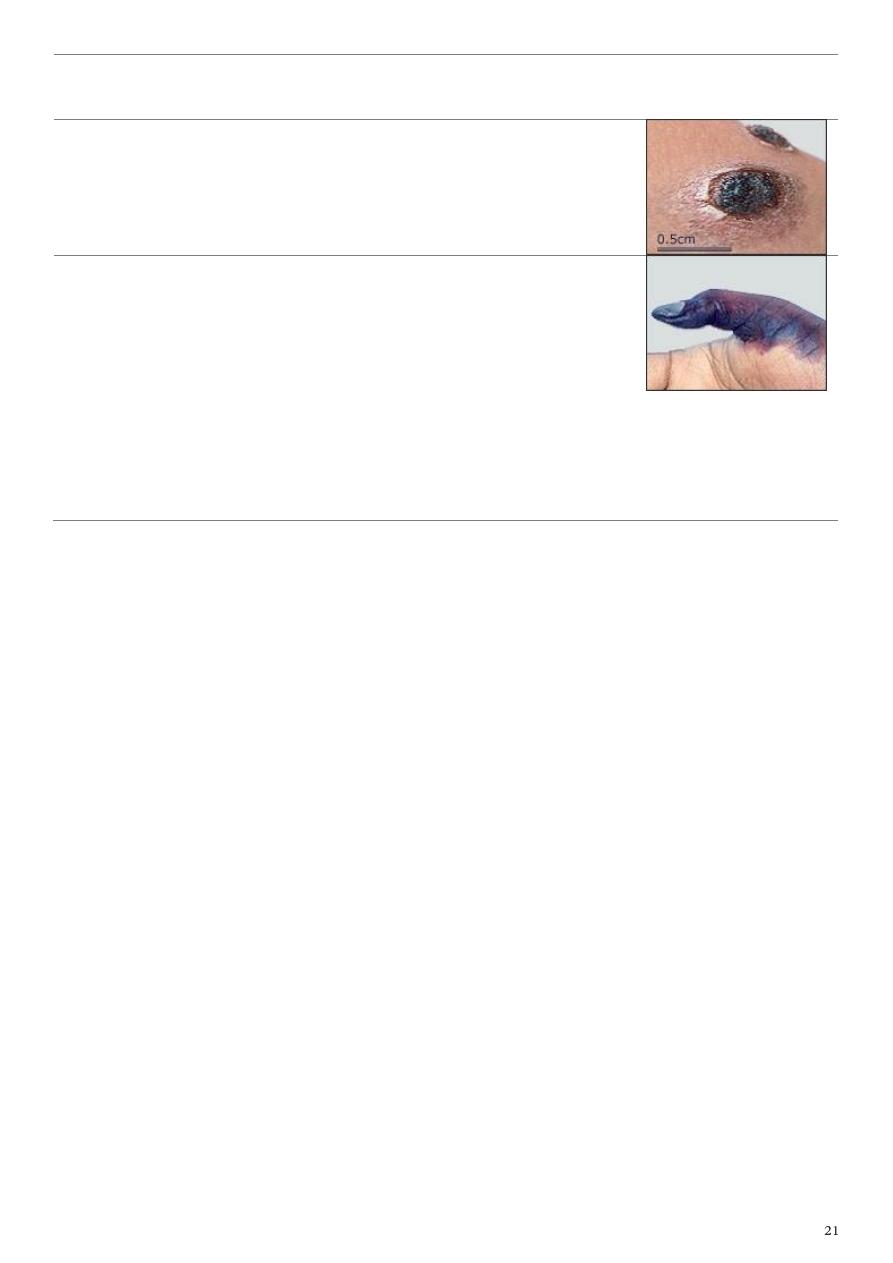
border/shape, edge, and tissue at
base.
Eschar
A
scab or dry crust
that results from
trauma, infection, or excoriating skin
disease.
Gangrene
Necrotic, usually black, tissue due to
obstruction, diminution, or loss of
blood supply. Gangrene may be wet or
dry.
Wet gangrene often follows a crushing
injury. It has an offensive odor and
spreads rapidly.Dry gangrene becomes
cold, dry, and shriveled and eventually
turns black.
Part5
: Specific skin lesions
1- Pitryasis alba:
Superficial dermatitis of unknown origin.
Hypopigmented patch +fine scale [usually on sun exposed areas (face, neck and hands)
+ in children].
Dermatitis heals (decrease melanocy, decrease melanosm).
Tinea vercicolor (hypopigmented macuels and patches with scales that is more
prominent upon stretching, usually on covered areas (trunk), in older age group),
Vetilligo (Hypo (early stage)
depigmented).
Management
Emollient, avoid sun light, topical steroid.
2- Vetilligo:
Hypo or depigmented patches, well demarcated with irregular margins.
The affected skin is non-scarring with NO scale.
May occur in hairy on non-hairy (difficult to treat)skin.
It is an autoimmune disease affecting the melanocyte.
DDx Pitryasis Alba, Tinea vercicolor, post. Inflammatory hypopigmentation.
Treatment topical or systemic steroid (depend on surface area affected),
photosensitizer (psoralin or PUVA), tacrolimus (immunomodulator).
3- Tinea versicolor:
Tinea vercicolor (hypopigmented macuels or patches with scales that is more
prominent upon stretching.
Caused by Malassezia furfur (a normal fungus that inhabit the skin), after swimming.
Occur in trunk, proximal extremity, in exposed and non-exposed areas (usually non-
esposed).
Increased in hot weather and after puberty.
Treatment Topical antifungal (ketoconazole 2 week), selenium shampoo.
may need systemic antifugal.
4- Hair loss:
Patchy:
Alopecia areata (patch) normal skin (non-scarring) (use the magnifier lens to see the
pilosebaceous orifices).
Tenia capitis thick scale, erythema, itching, pastule.
Discoid lupus dusky, erythematus, SCARRING.
Lichen planus 5P: plane, polypoidal, papule, purple and pruritic.
Generalized:
Androgenic progressive, hormonal, in female may be there is no increase in
androgen but increase in sensitization of receptors.
Chronic diseases anemia, hypothyroidism, organ failure, malnutrition.
Drugs chemotherapy (anagen), anticoagulants (heparin).
5- Alopecia Areata:
Patches of hair loss, normal skin, well demark.
Autoimmune – anagen.
Treatment topical anthralin, topical or intral-lesional steroid, cyclosporin.
6- Erythemia multiforme:
Multiple plaques, erythematus, well demarcated.
Rough, irregular margin.
Target lesion.
Infection, idiopathic, allergy, pregnancy.
DDx Chronic urticaria, serum sickness, SLE, lichen planus.
Treatment supportive measures, analgesics, anti-histamine, acyclovir (oral),
prednisolone.
1-2 weeks resolve spontaneously, recure multiple times in year.
7- Folliculitis:
Superficial infection of hair follicle.
Pastular lesion, erythematus, hair in center.
DDx Bacterial infection, T.corporis, dermitits.
Rx Topical antibiotics, systemic steroids, surgical drainage.
Carbuncles boils together, deep infection of hair follicles, need surgical drainage.
Sites of predilection: scalp, neck, buttock, extremities and trunk.
8- Scarlet fever:
Sand paper like.
Erythematous papules.
With white, red strawberry tongue.
Give antibiotics.
9- Urticaria:
Weal and flare Lesion with itching.
Erythematus well demark plagues.
Elevation (edema), no scale, no scar, scratching marks.
Treatment steroid, anti-histamine.
10- Skin tag:
Well demarked, flesh to brown color papules, pedenculated (has a neck), smooth or
rough surface.
In obese pt. at the sites of skin folding.
DDx Nevus, seborrheic Keratosis, BCC.
Rx Excision (due to irritation or cosmetic or in children).
Occur in the neck, inguinal region, axillae (common in female).
11- Seborrheic keratosis:
Brown to black, hyperpigmented plaques, rough, well demarcated.
Benign hereditary tumor.
DDx Malignant melanoma, BCC, acnitic keratosis.
Treatment Excision.
Occur in the face, scalp, upper limbs and trunk.
12- Baghdad boil (cut. Leshmaniasis):
Single or multiple Brown nodular lesion (indurated) with scale, crust and central
erosion or ulceration.
Not tender +/- satellite lesion, any site of sand fly bite.
Rx pentavalent antimonial compound (intralesional Na
+
stibogluconate)
13- Acne form rash:
Like acne but short duration of onset
Treated by steroid.
14- Eczema:
Papules and vesicles, scaly, erythmatus, itchy with oozing.
Inflammaory response to certain materials (contact or atopy) .
DDx psoriasis, scabies, dermatitis.
Treatment avoid precipitant agent then systemic antibiotics, anti-histamine (for
itching), steroids (to reduce inflammation), emollient (to avoid dryness), light
management.
15- Warts:
Rough surface, papule, scales, some time digitated [filliform wart (finger like)].
Of many types common wart, plane wart, planter wart or filliform wart.
Caused by HPV infection
Site: anywhere
DDx: planter wart (corn), common wart (Molluscum contangiosum).
Treatment Depend on: site, size, number and pt. preference.
Topical keratinolytic (salicylic acid), immunomodulator and curettage.
16- Plane warts:
Flat surface, skin or darker pigment, papule, well demarked.
HPV 10, 3, 41, 28.
Sites: forehead, face, arm.
Occur: children, young adult (mostly due to immune suppression).
DDxnevi, acne, 2ndry syphilis.
Treatment topical keratolytic, retin A chemotherapy.
17- Molluscam contagiosum:
Single or multiple fleshy or pearly white color large papule (sometimes erythematous)
with central umblication (a depression seen by magnifier lens).
Sites: face, trunk and gentilia.
Caused by: parapox viral infection.
Transmission (contagious) contact, STD.
DDxwarts.
Treatment topical salicylate or curettage (depend on the number).
18- Scabies:
Erythematous papules, vesicle, pastule, burrows, crust, itching (at night).
Mite infestation, sarcoptes scabes.
DDx Contact dermtits, pitryasis rosea, psoriasis.
Sites of predilection: genetalia, paraumbilical region, breast, gluteal region, flexor
surface, axillae and finger webs (burrows).
Note: the face palms and soles are spared in adults and only involved in infants.
Treatment
1. Boiling, ironing or putting on sun light (for3-4 days) of clothes and bed mattresses.
2. Treat all family members (even if have NO itching)
3. Good hygienic measures
4. Topical steroids, systemic anti-histamine for itching
5. Scabicidals topical permithrin or 10% sulfer preparation for 3 days + vasalin.
Failure of treatment may be due to inappropriate drug compliance, no family
treatment, resistance, no hygiene, recurrent infection or exposure to the same cause.
19- Ichthyosis:
Dry, rough, cracked, thickened.
Hereditary, decrease thyroid, AIDS, leprosy.
Treatment skin lubricant after bath, limit use soap, winter dryness, steroid.
20- Keloid:
Firm, smooth, dark or skin colored nodule or papule.
Excessive growth scar beyond the wound margins,
DDx Lipoma, neurofibromatosis, fiber of fibrosarcoma, sebaceous cyst and
sarcoidosis.
10-30 year, upper arm, neck, scalp, cheek, ear.
Treatment Intra-lesional steroid, surgery (increase keloid).
21- Psoriasis:
Bright pink plaques, well demarcated with silver scales.
Possible causes: Genetic, autoimmune, infection of unknown, increase keratinocyte.
Sites of predilection: Extensor surfaces (especially elbows and knees), scalp and nails.
Nail finding: coarse pitting, onycholysis, oily spot.
DDx scabies, contact dermatitis and teania corporis.
Treatment depend on severity, chronicity and age of pt. :
1. Topical therapy: steroid (Systemic steroid is contraindicated as it causes flaring up
of the disease), Vit. D, retinoic acid and salicylic acid (kerationlytic).
22- Acne vulgaris:
Papule, comedom (black), white head, pastule (pus + papule), hyperpigmented, and
scar.
If there is only comedom and white heads.
It is considered mild degree of acne, drug induce keratiniaztine (isotrismne).
The bacteria affect the face during acne colled (propino bacterium acne) can give
the patient topical antibiotics like azithromycin, clindamycin.
23- Taebia capitis:
Fungal infection in the head causing patchy hair loss.
Well-demarcated erythematous plaque with thick scales and +ve pulling test (the hair is
easily pulled) usually in older children or in adults.
DDx alopecia areata
Rx systemic antifungal (terbinafine).
Notes:
We can’t use cautery for treatment of facial lesions (e.g Molluscum contangiusm) as it
causes an ugly scar.
We don’t use antivirals for treatment of M. contangiousm and wart despite they are of
viral infection etiology.
We have to use a systemic antifungal (against dermatophytes) in cases of T.capitis and
T.pedis since the topical treatments do nothing (can’t reach the deep infected areas).
If the we have doubt about the Dx of skin discoloration lesion we can use wood’s light
for differentiation:
T.vercicolor will appear yellowish.
P.alba will appear lighter than skin color.
Vetilligo will appear whitish.
If it is still doubt do scraping test examine under the microscope.
If you haven’t the facilities and your diagnosis is between T.vercicolor and vetilligo
give topical antifungal as therapeutic trial check after 2 weeks if the
discoloration is got away, then it is T.vercicolor; but, if the discoloration is still or
progressed into other areas or becomes depigmention, then it is vetilligo.
Steroids (whether topical or systemic) is contraindicated in bacterial, fungal and viral
infections.
Never ever give steroid as therapeutic trial if there is suspicion of fungal infection.
