1
Fifth stage
Radiology
Lec-1
د.هديل
11/10/2015
Radiology of G.I.T
Radiological investigations
1. Contrast examination
a) Barium study
b) Ba. Swallow
c) Ba. Meal
d) Ba. Follow through
e) Ba enema
2. Endoscopic Ultrasound .
3. CT & MRI.
4. Nuclear medicine (FDG-PET):
flurodeoxyglucose positron emission
tomography
THE OESOPHAGUS
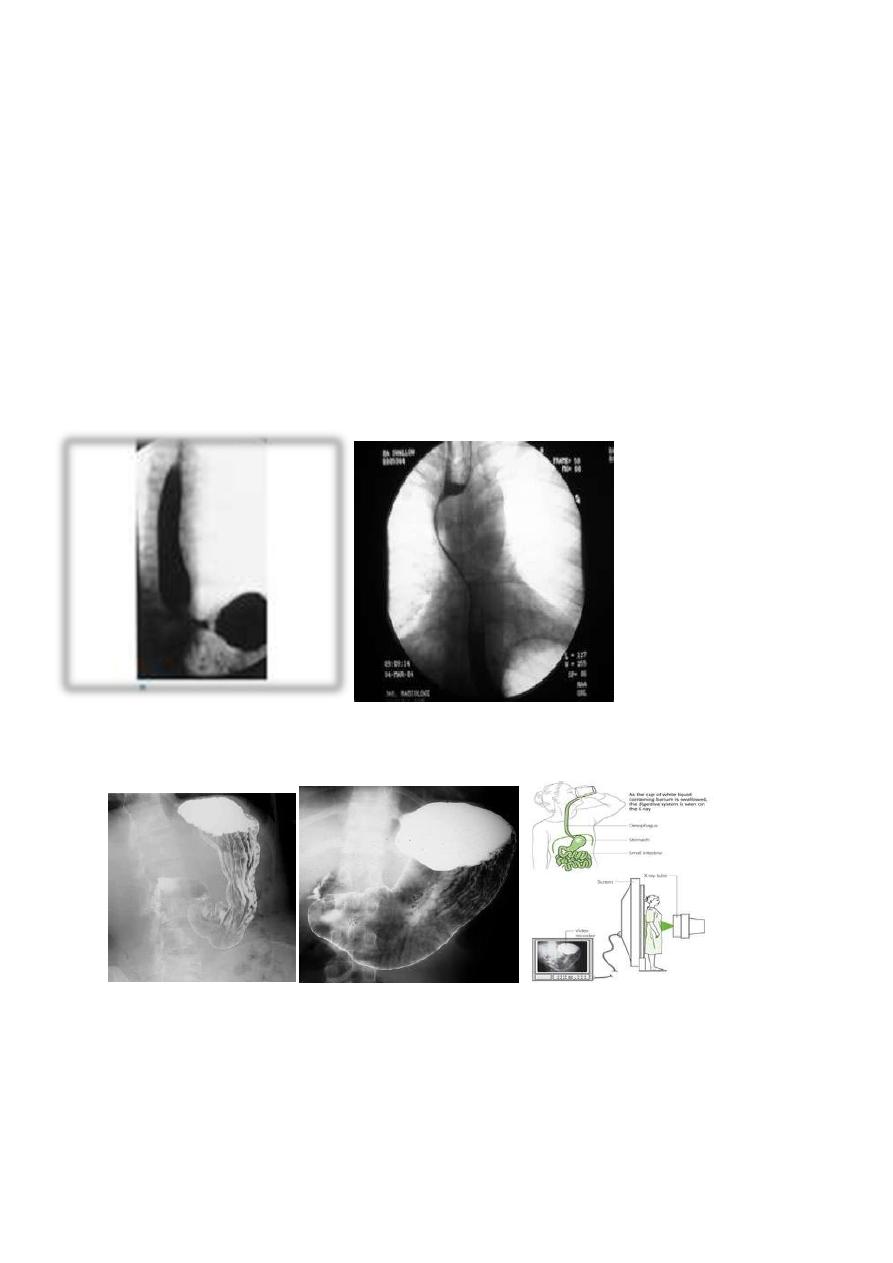
Barium Swallow
1. Conventional
2. Double contrast (DC)
3. Flouroscopy + spot films

2
Technique:
1. Patient will need to be NPO after midnight before the exam
2. The patient will have to swallow a contrast agent: Barium or Gastrograffin
3. May also swallow sodium bicarbonate for double contrast barium swallow
4. X-ray tech will have the patient perform various maneuvers so that the barium can
coat the GI tract
Indications:
1. Odynaphagia
2. Dysphagia
3. Hematemesis
4. Abdominal pain
5. Unexplained weight loss
The Normal Anatomy:
Long tubular structure
Length 25-30 cm
Start at level of C5 ( Crico-pharengeal)
End – Cardiac sphincter
Three portions
a) Cervical
b) Thoracic
c) Abdominal
Normal Mucosal pattern (DC)
a) thin
b) regular
c) longitudinal
d) Parallel
e) Numbers of lines ( 4-5 ) >>>>>>MCQ
Areas of normal Narrowings
1. body of the cervical vertebra
2. AA
3. LT atrium
4. diaphragmatic hiatus
3
On the Hypo pharyngeal part Common structures that we can visualize are:
1. Epiglottis
2. Post cricoid impression
3. lateral pharyngeal pouches
4. Crico pharyngeal muscle impression
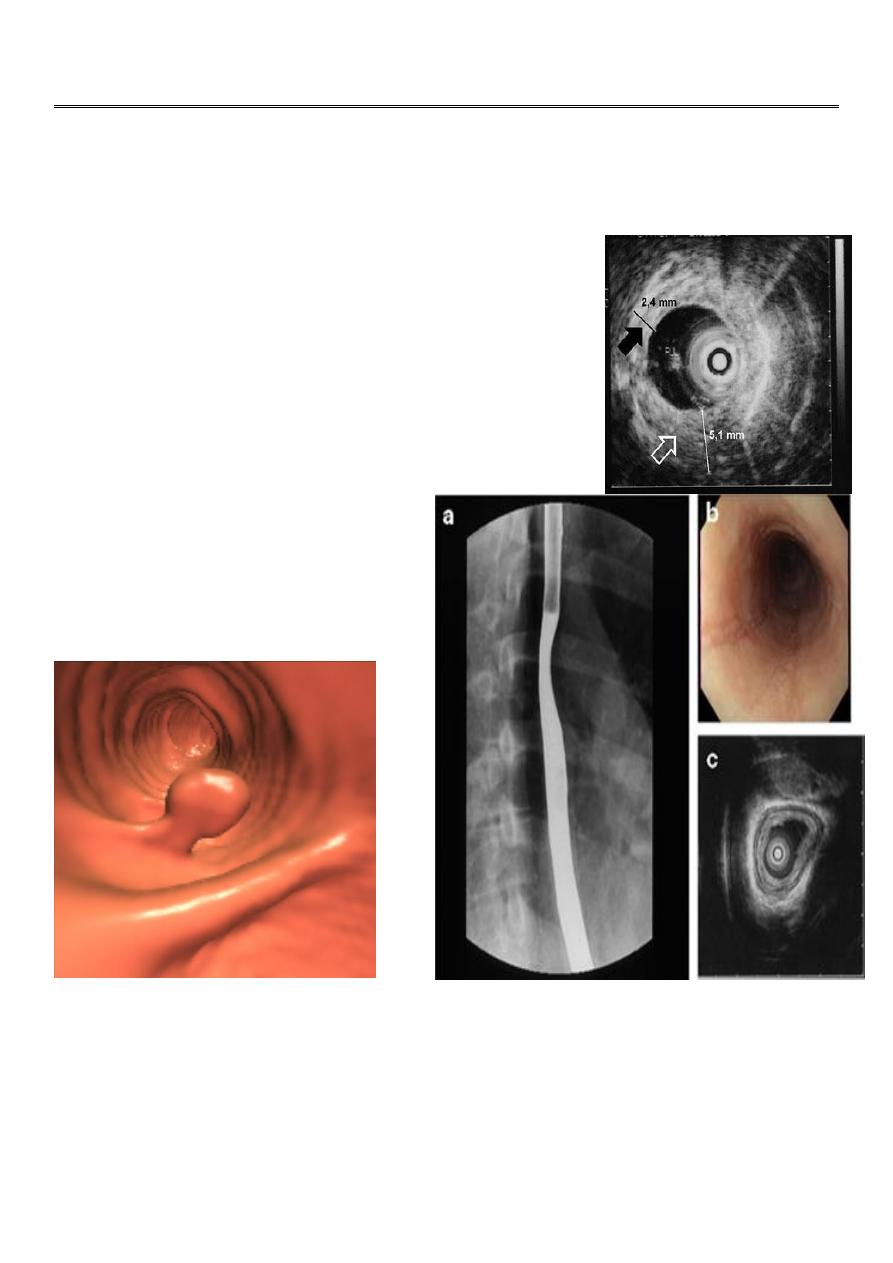
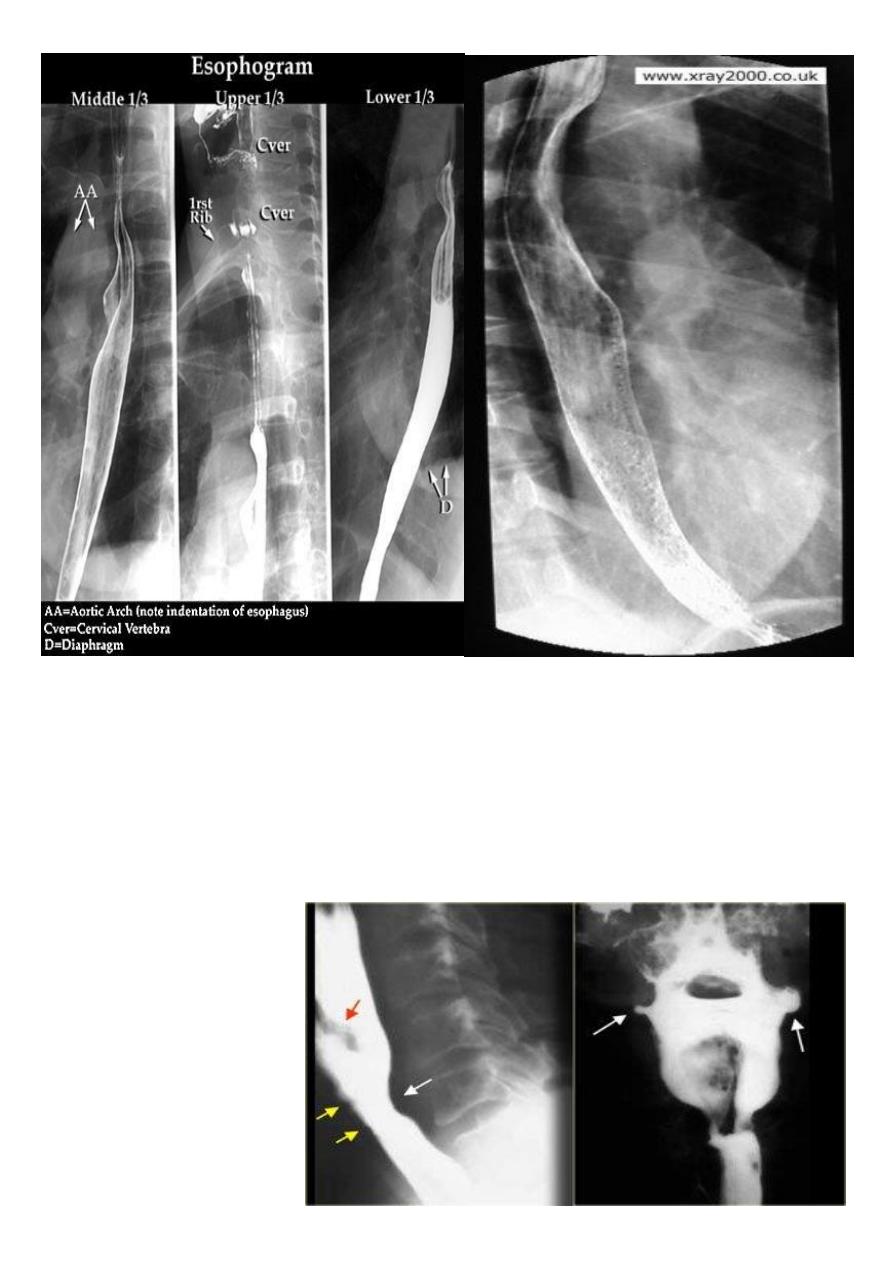
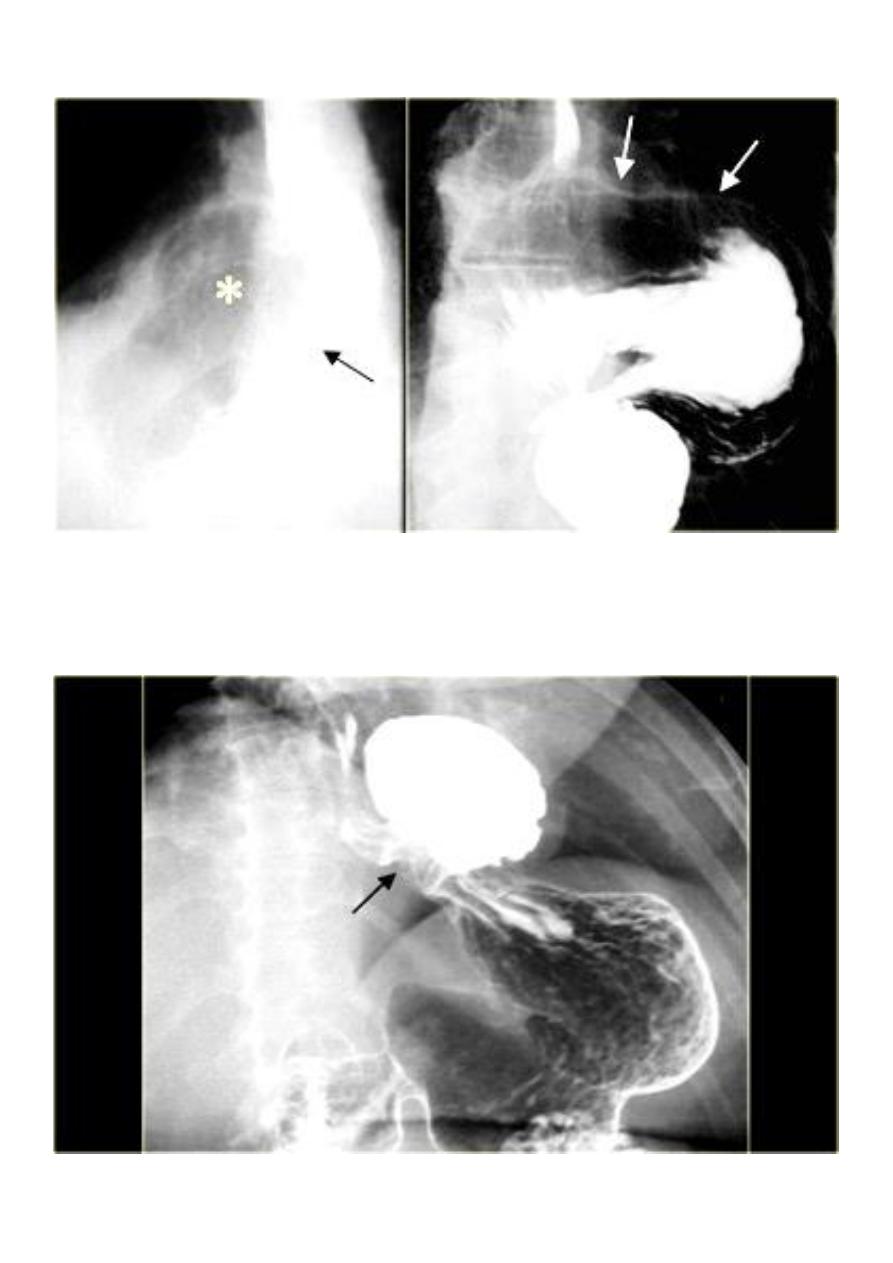
LEFT: Lateral view:
Epiglottis (red arrow).
Post cricoid impression
(yellow arrows).
Crico pharyngeous
impression (white arrow).
RIGHT: AP-view: Small
lateral pharyngeal pouches
(arrows)
4
The esophageal wall is composed of:
1. Mucosa
2. Musculature
a) Inner circular layer
b) Outer longitudinal layer:
i) Upper 1/3 striated muscle
ii) Middle 1/3 striated and smooth muscle
iii) Lower 1/3 smooth muscle
3. No serosa >>>>>>MCQ
Esophagus mucosa: normal thin, parallel, uniform mucosal folds 3-4 in no.in double
contrast examination
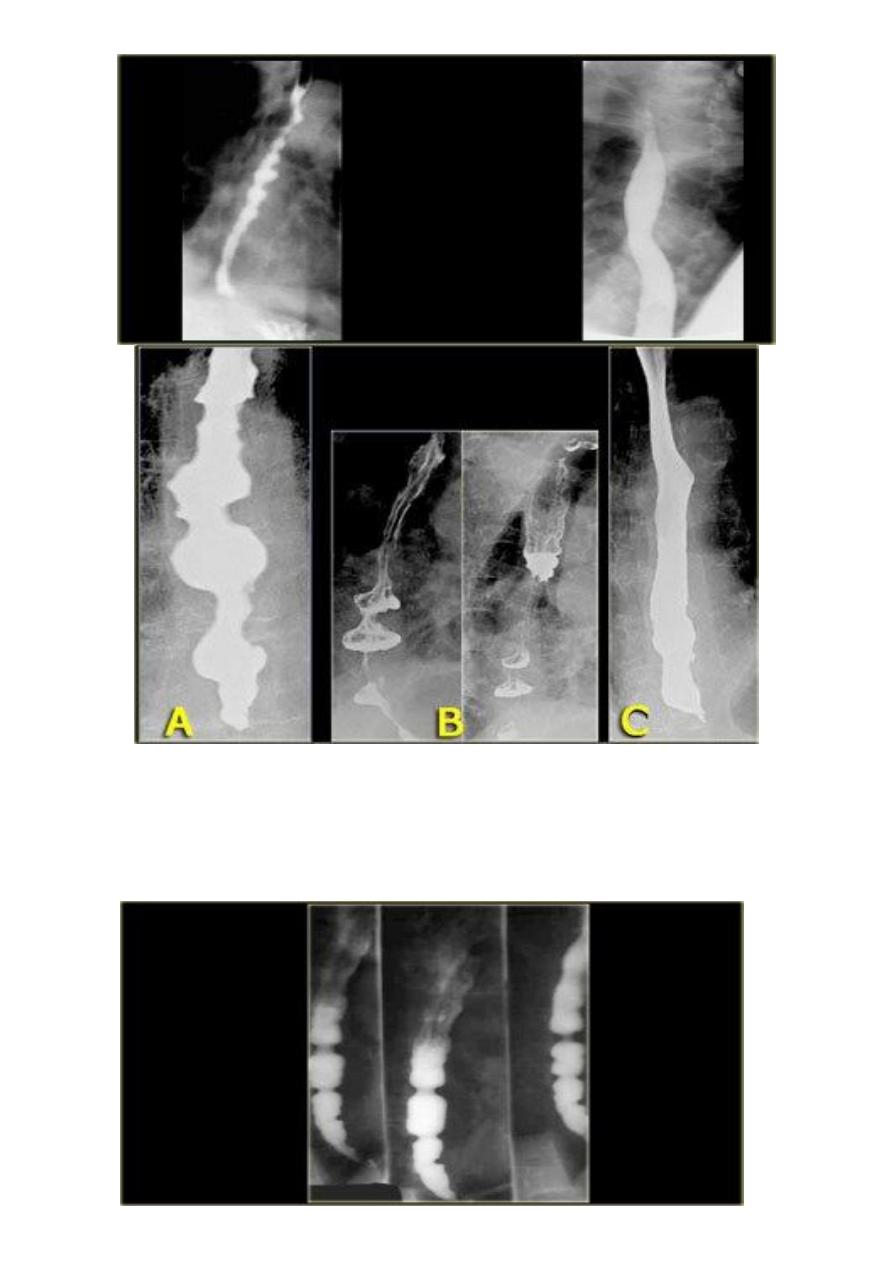
Esophageal peristalsis
1. Normal:
a) Primary contraction: Propels bolus through the esophagus
b) Secondary contraction: Follows primary contraction and propels any remaining
bolus from thoracic esophagus
2. Abnormal contraction :
Tertiary contractions as in :
i.
Diffuse esophageal spasm
ii.
Nutcracker esophagus( crock screw o.)
iii.
Decreased peristalsis
resulting from achalasia, scleroderma, dermatomyositis, polymyositis, esophagitis,
and secondary to many other diseases
5
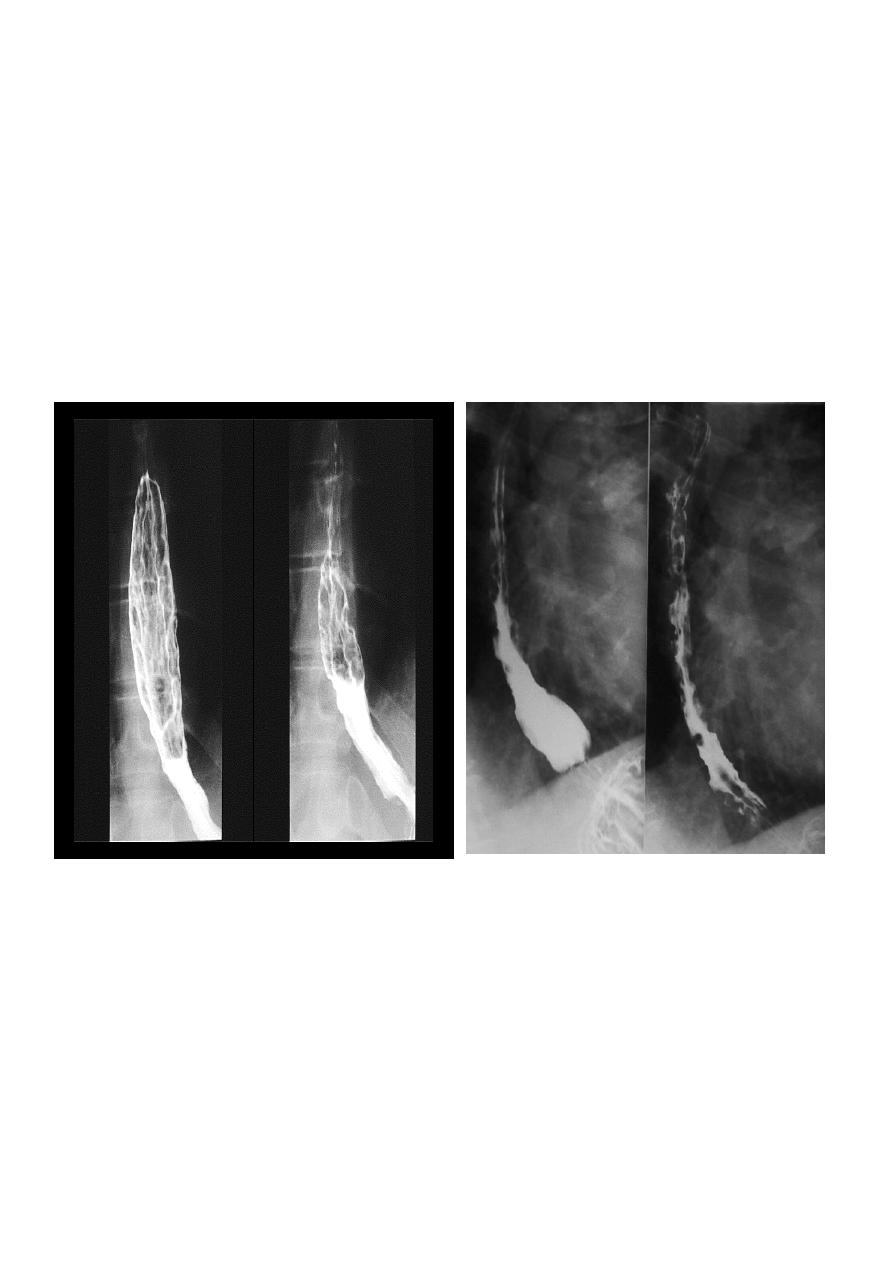
Diffuse esophageal spasm
Diffuse esophageal spasm produces intermittent contractions of the mid and distal
esophageal smooth muscle, associated with chest symptoms
6
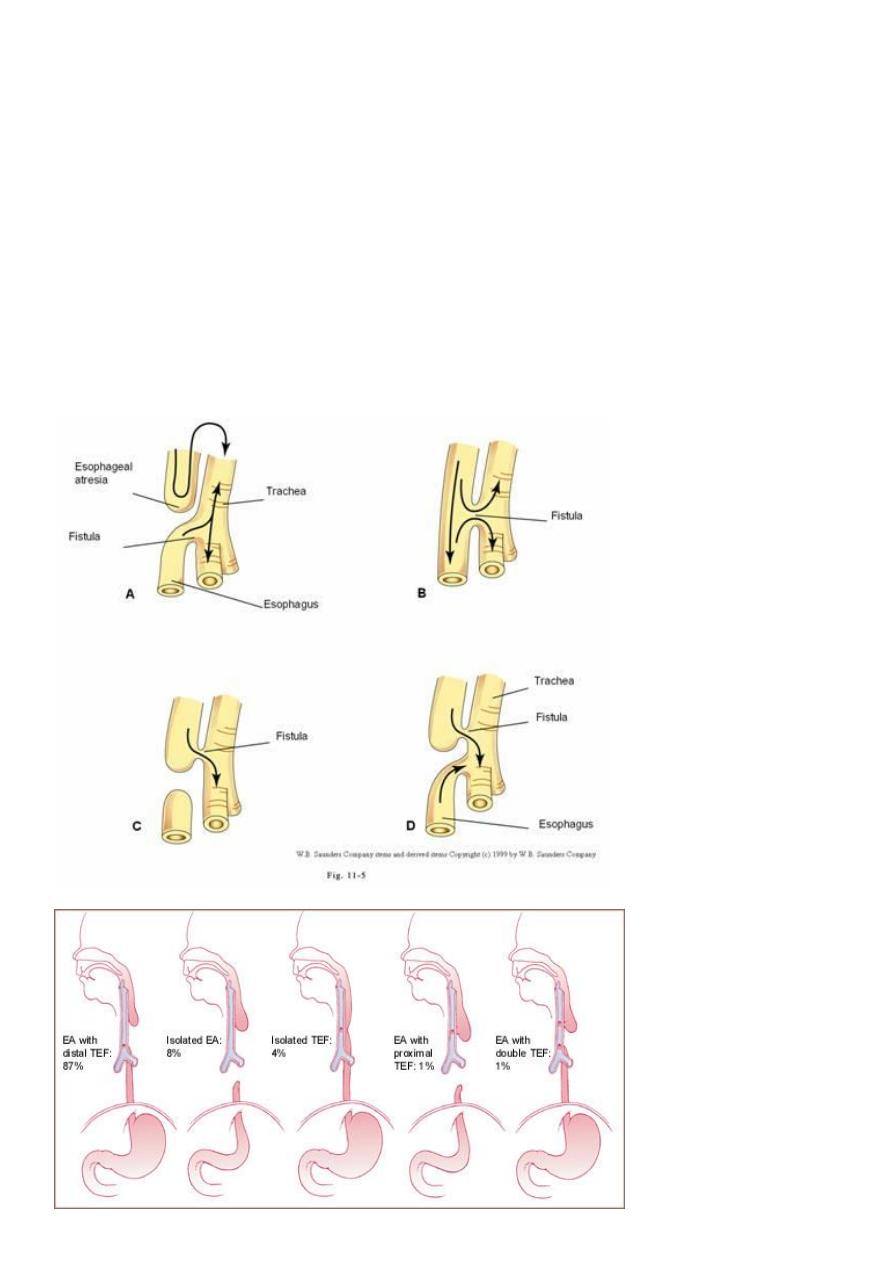
Congenital Anomalies
1- Artesia with or with out tracheo-oesophageal fistula (TEF).
2- Congenital Short oesophagus.
3- Congenital Duplication ( Neuro-enteric cyst ).
ATRESIA:
1. Complete blockage of the lumen .
2. The diagnosis is suggested after birth by inability of infant to feed or by choking
during swallowing .
3. The blocked segment is mostly seen at level of thoracic inlet
Types of Fistula
The most common
esophageal atresia is
(distal trachea
esophageal
fistula)>>>>MCQ
7
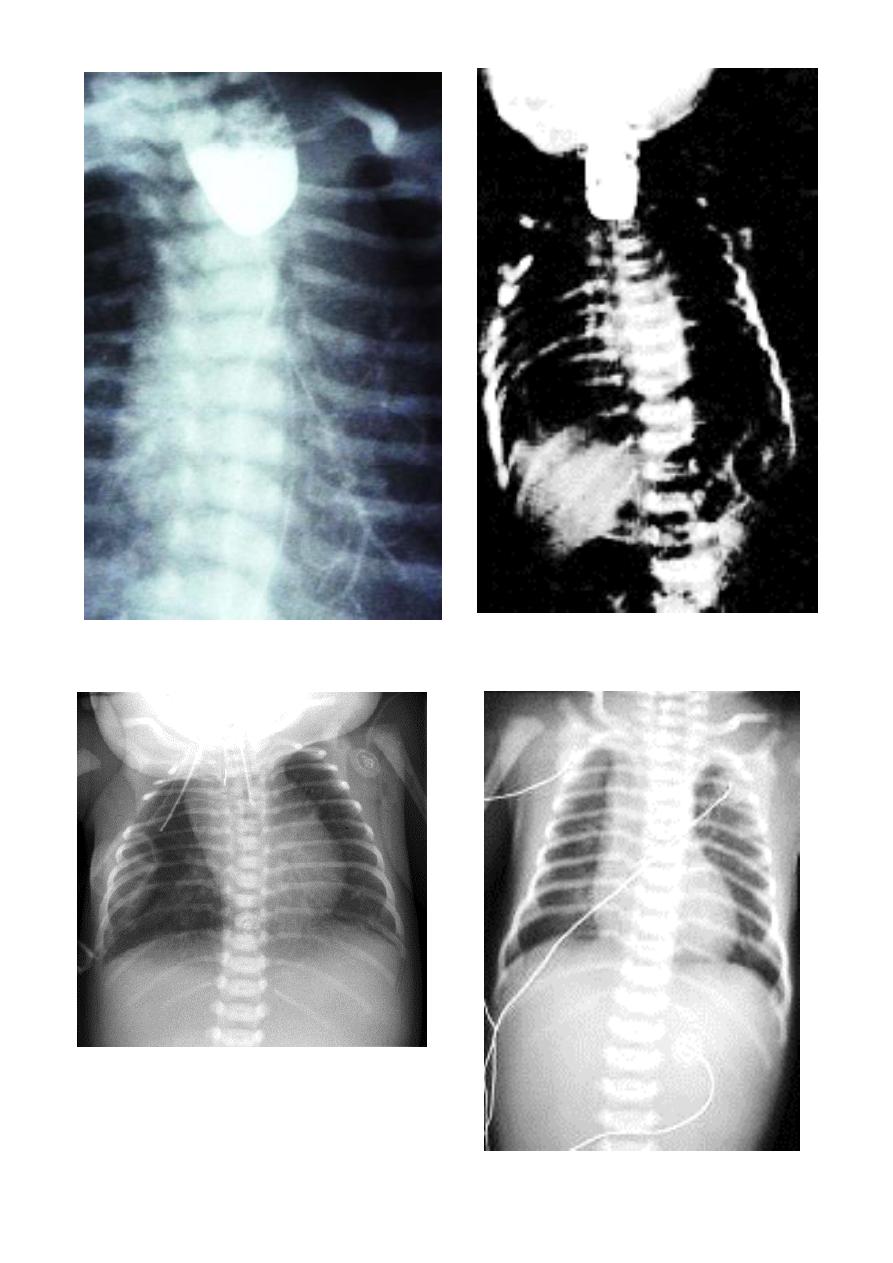
8
Acquired Lesions
DYSPHAGIA
difficulty in swallowing causes :
1. Carcinoma ( Malignant stricture).
2. Benign Stricture (Corrosive ).
3. Achalasia Cardia.
4. forgien body
5. osophagitis .
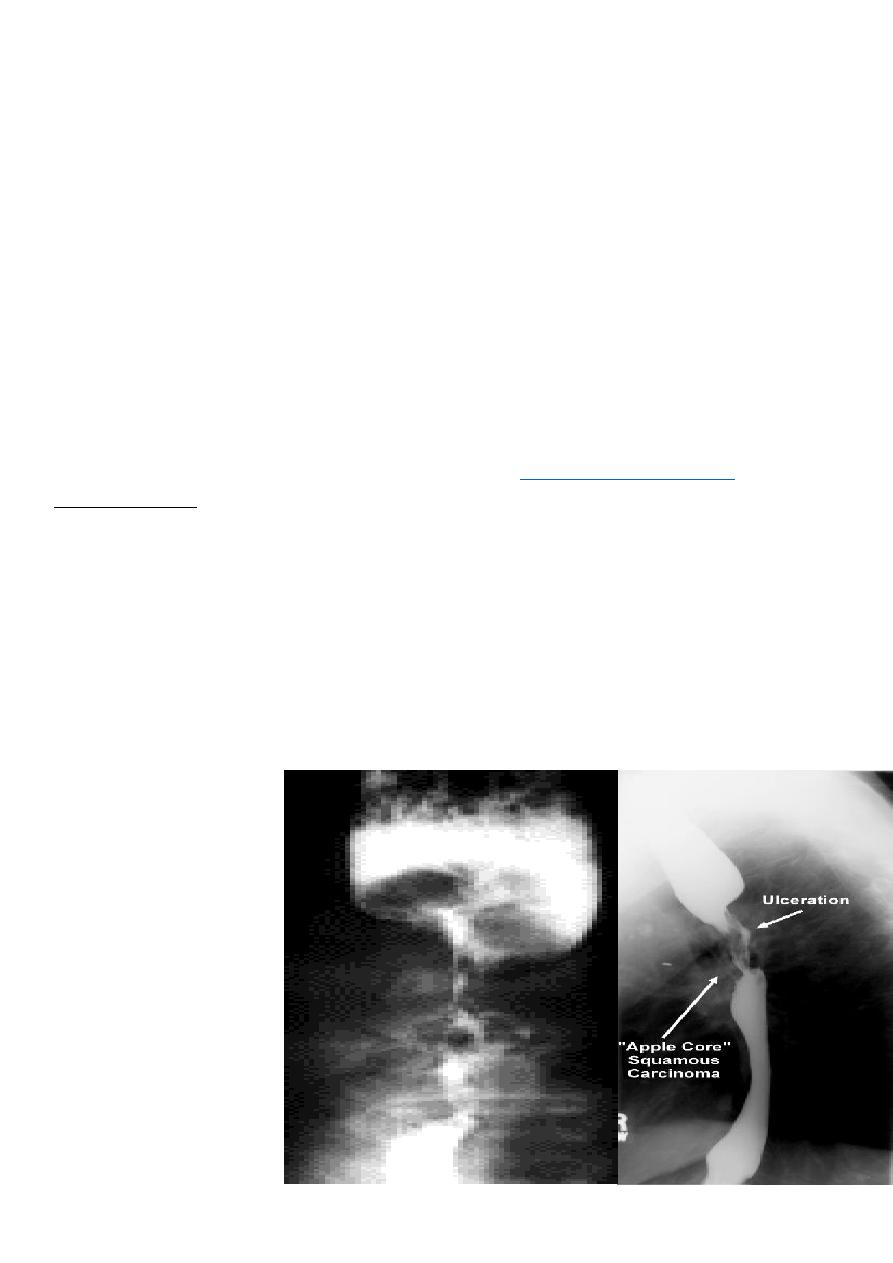
Malignant stricture
CA esophagus is the cause for the malignant stricture
The most common types of esophageal carcinoma are
adenocarcinoma .
esophagography is unique among esophageal studies for assessing both morphology and
motility.
Barium esophagography remains the study of choice for characterization of esophageal
strictures. Esophageal carcinoma may demonstrate a variety of appearances on barium
esophagrams.
Annular Carcinoma
Narrowing :
1. Constant.
2. Irrigular .
3. Variable length.
4. Shouldering sign.
5. Fistula (double
tract).
6. Soft tissue
shadow of the
mass
9
Computed Tomography
Contrast-enhanced CT plays an important role in the
staging of esophageal carcinoma. To :
1. determining the extent of the local tumor.
2. invasion of mediastinal structures.
3. involvement of supra clavicular, mediastinal, or upper abdominal lymph nodes.
4. Assessment of the distant metastases.
examination should extend from the thoracic inlet through the liver
Routine oral contrast material such as (gastrographine) or a negative intra luminal
contrast medium, such as water.
+/ - IV contrast injection
CT essential in the Dx & staging of the CA
CT finding of esophageal malignancy
1. Eccentric or circumferential wall thickening is greater than 5 mm.
2. Peri-esophageal soft tissue and fat stranding may be demonstrated.
3. A dilated fluid- and debris-filled esophageal lumen is proximal to an obstructing
lesion.
4. Aortic invasion .
11
5. Osophageal CA is often metastatic at the time of presentation ( look for the LN &
distal metastasis ) .
الصور المتعلقة بهذا الموضوع غير مطلوبة. لالطالع عليها يرجى زيارة موقع محاضراتي
Barrett's esophagus
is a metaplastic disorder in which specialized columnar epithelium replaces healthy
squamous epithelium.
Barrett's metaplasia is the most common cause or precursor of esophageal
carcinoma. The rate of esophageal adenocarcinoma is increasing in the Western
world, and it is associated with a poor prognosis, mainly because individuals present
with late-stage disease..
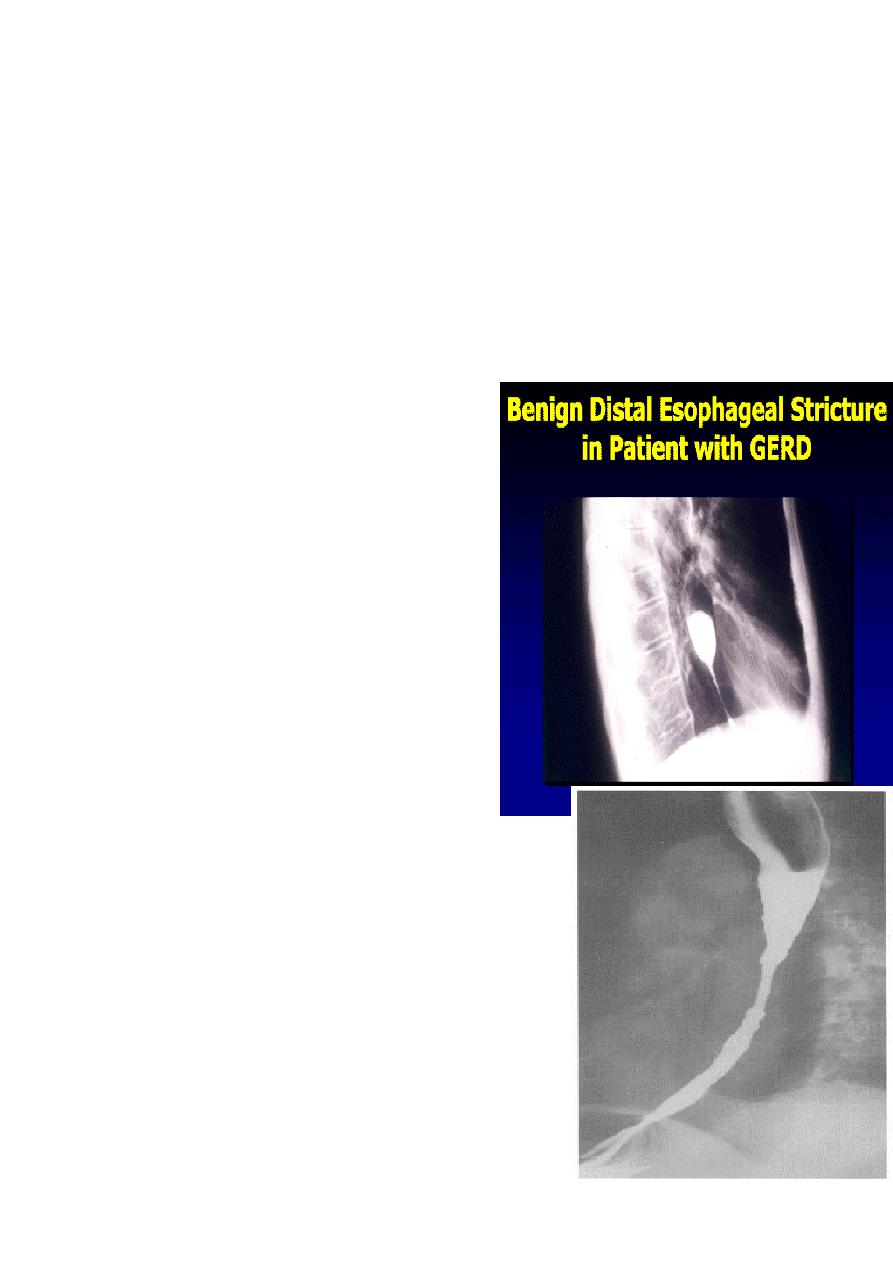
Benign Stricture
1. Causes :
a) Peptic esophagitis
b) Corrosive
c) Traumatic
2. Ba. swallow :
a) Constant narrowing.
b) Long length (lower third).
c) Smooth and regular.
d) Mild proximal dilatation.
e) No shouldering sign.
f) Smooth tapering
( funnel shape).
11
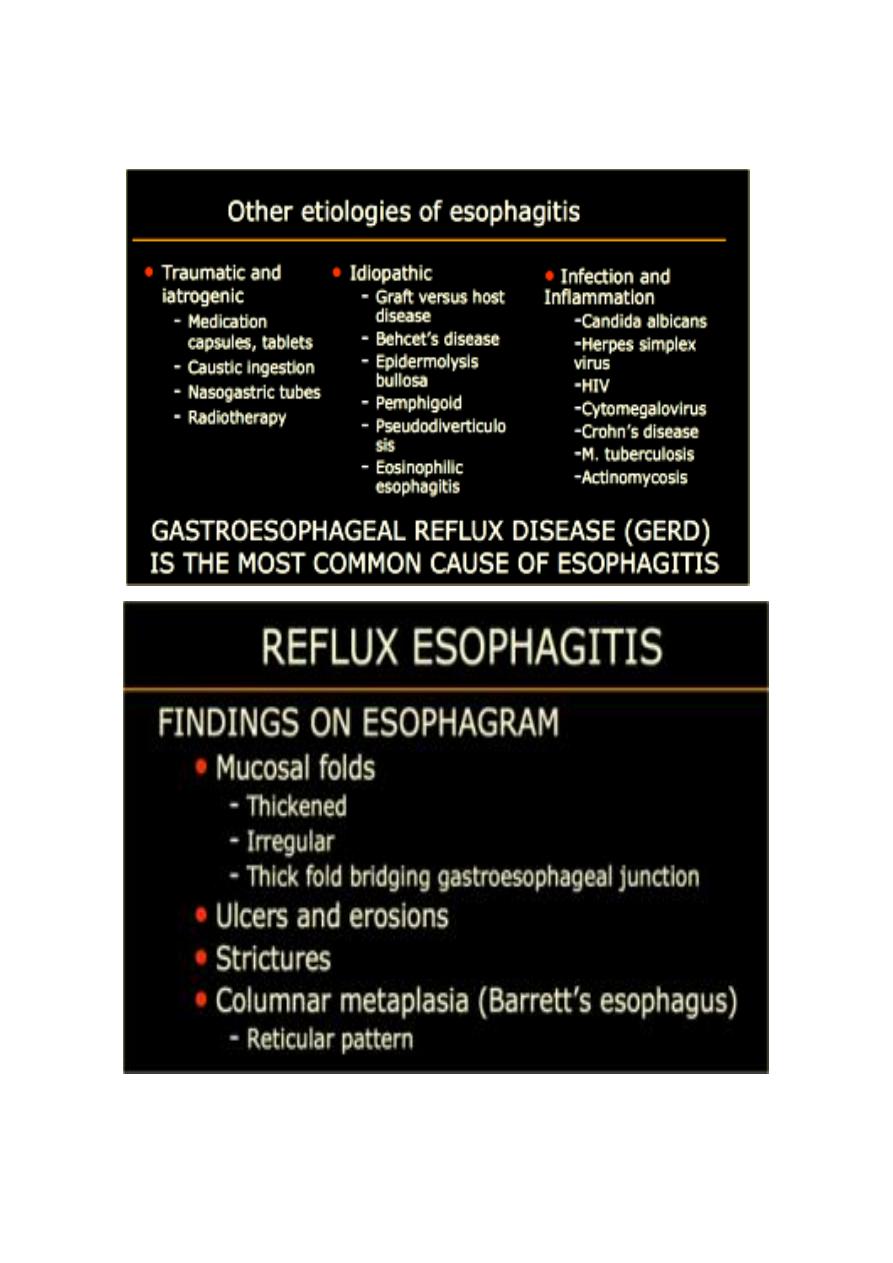
Inflammation and Infection
Gastroesophageal reflux (GERD) is the most common cause of esophagitis

12
Infectious esophagitis
Candida esophagitis
in patient with an infectious esophagitis due to candida , the barium shows numerous fine
erosions & plaques causing shaggy outline of the osophagus due to Candida albicans in
immunocompromised patient.
middle year old female with a past medical
history significant for HIV/AIDS comes in with
complaint of loosing their weight over the
past 2 weeks with pain & difficulty on
swallowing …. Also feels like food is getting
stuck in her throat
What is your diagnosis ??????????
A chalasia Cardia
Presentation:
1. Equal M:F incidence, most common in middle-age
2. Slow progression of dysphasia to start with to solid material then to solid & water
3. Increased incidence of carcinoma
Etiology:
1. Unknown ??? absent or reduced esophageal ganglion cells at their distal lower
sphincter
2. Incomplete or absent relaxation of LES with swallowing
3. Absent primary peristaltic waves
A : Absence
Chalasia : Relaxation
Narrowing :
1. the narrowing is Constant Short length (confined to cardia).
2. Regular and smooth.
3. No shouldering sign.
4. Tapering (Tip of pencil , cigar shape) Under left dome of diaphragm.
5. DILATATION (Sac like in proximal part )
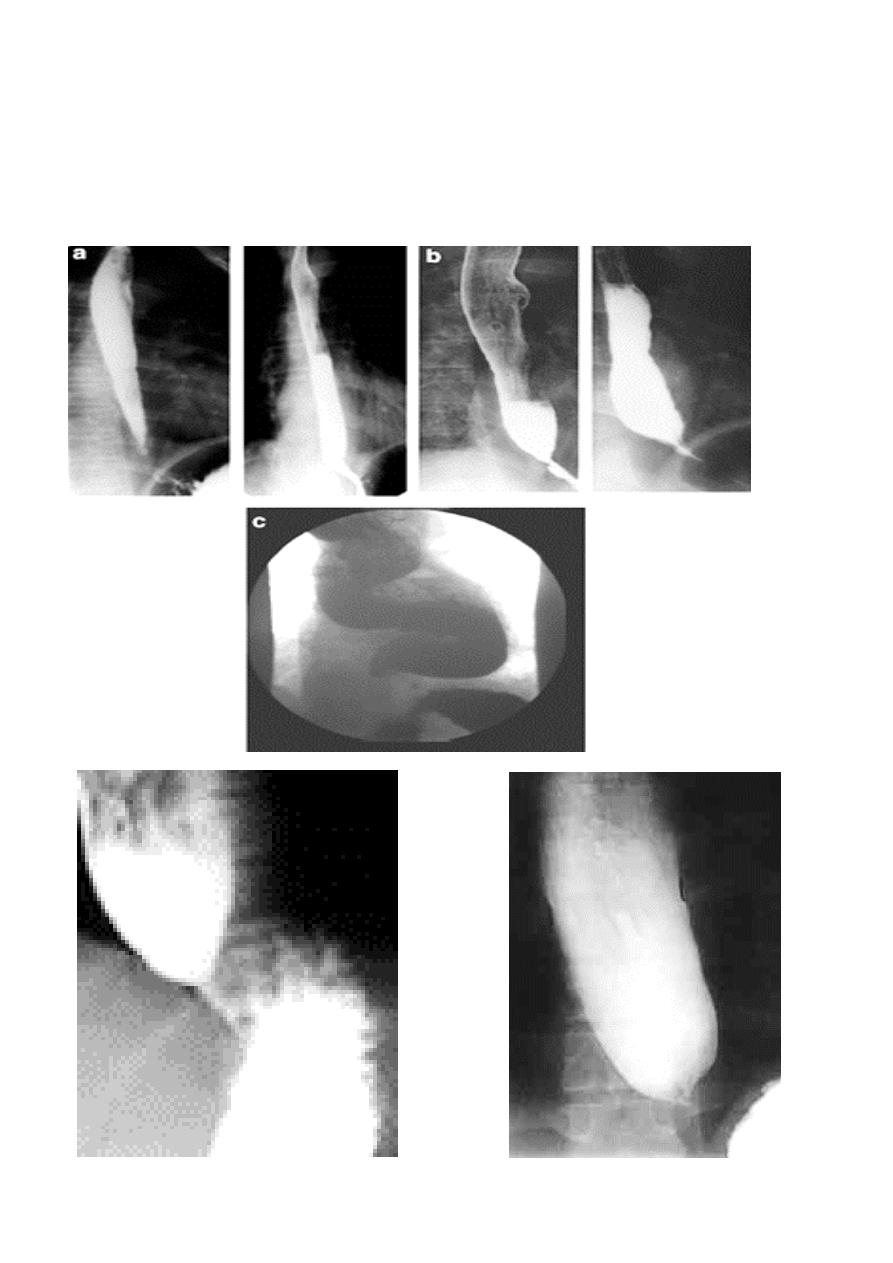
13
6. Undulating or spiky out line due to sluggish peristalsis.
7. Non- homogeneity of Barium due to food particles.
8. Air Barium level.
9. CXR shows widening of mediastinum.
10. Absence of fundal gas shadow.
11. Basal fibrosis in lungs due to repeated aspiration pneumonia .
14
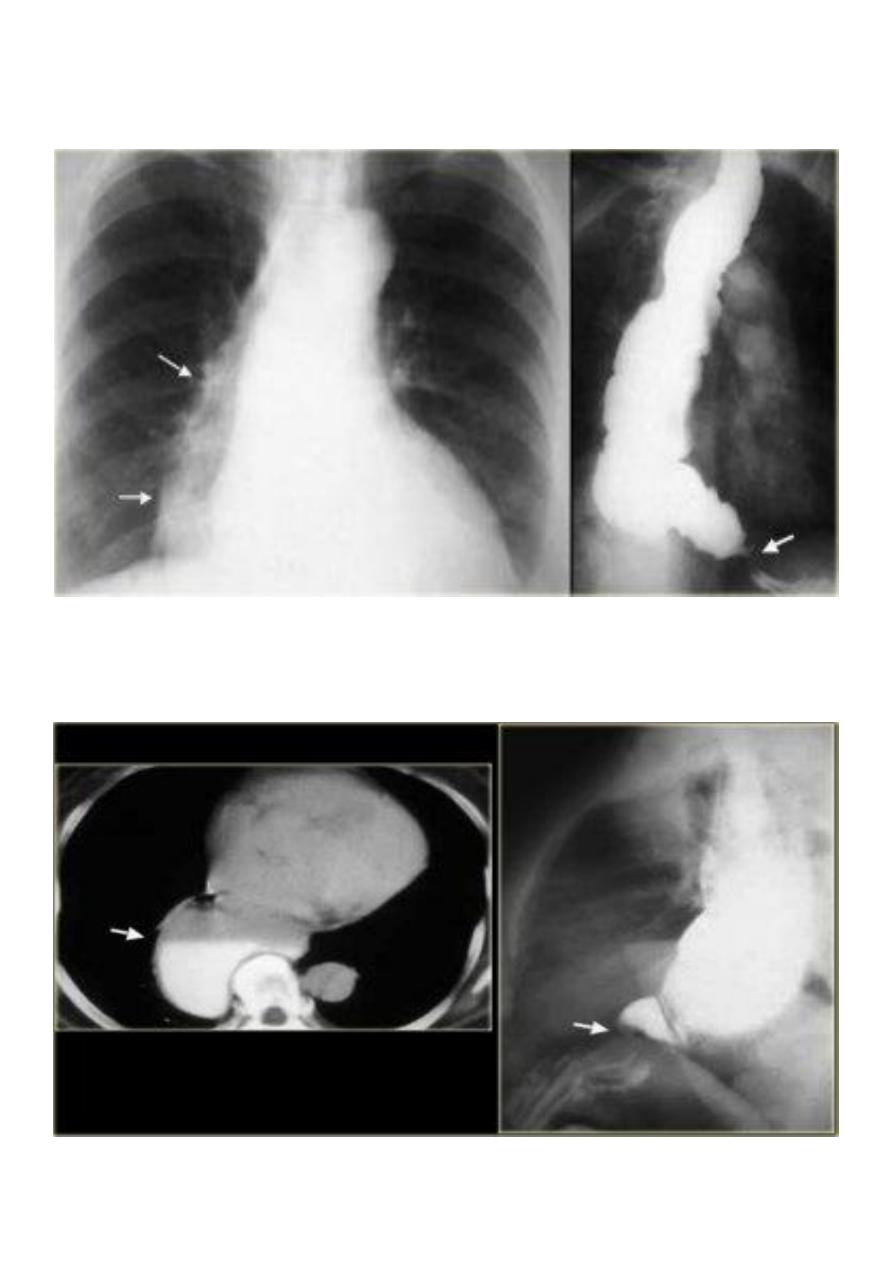
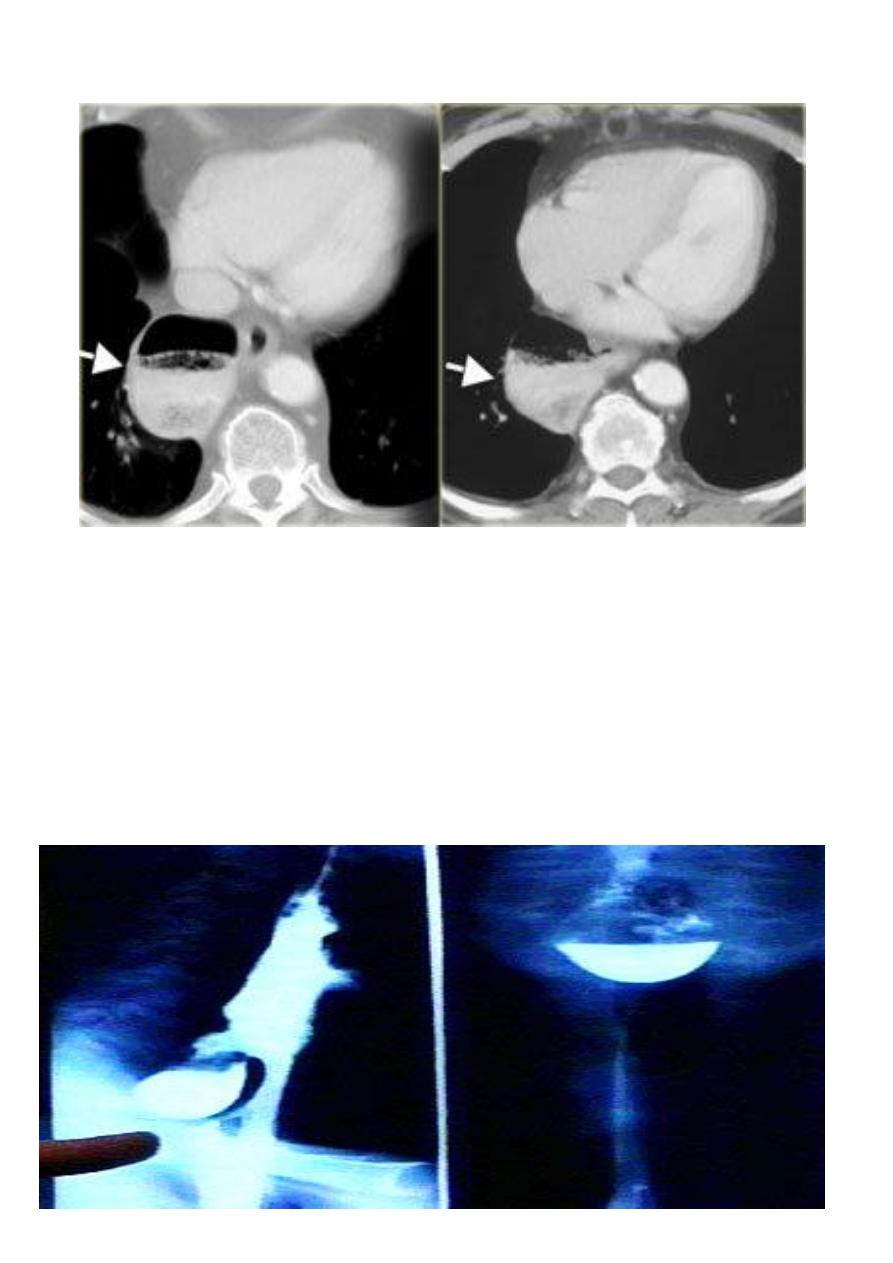
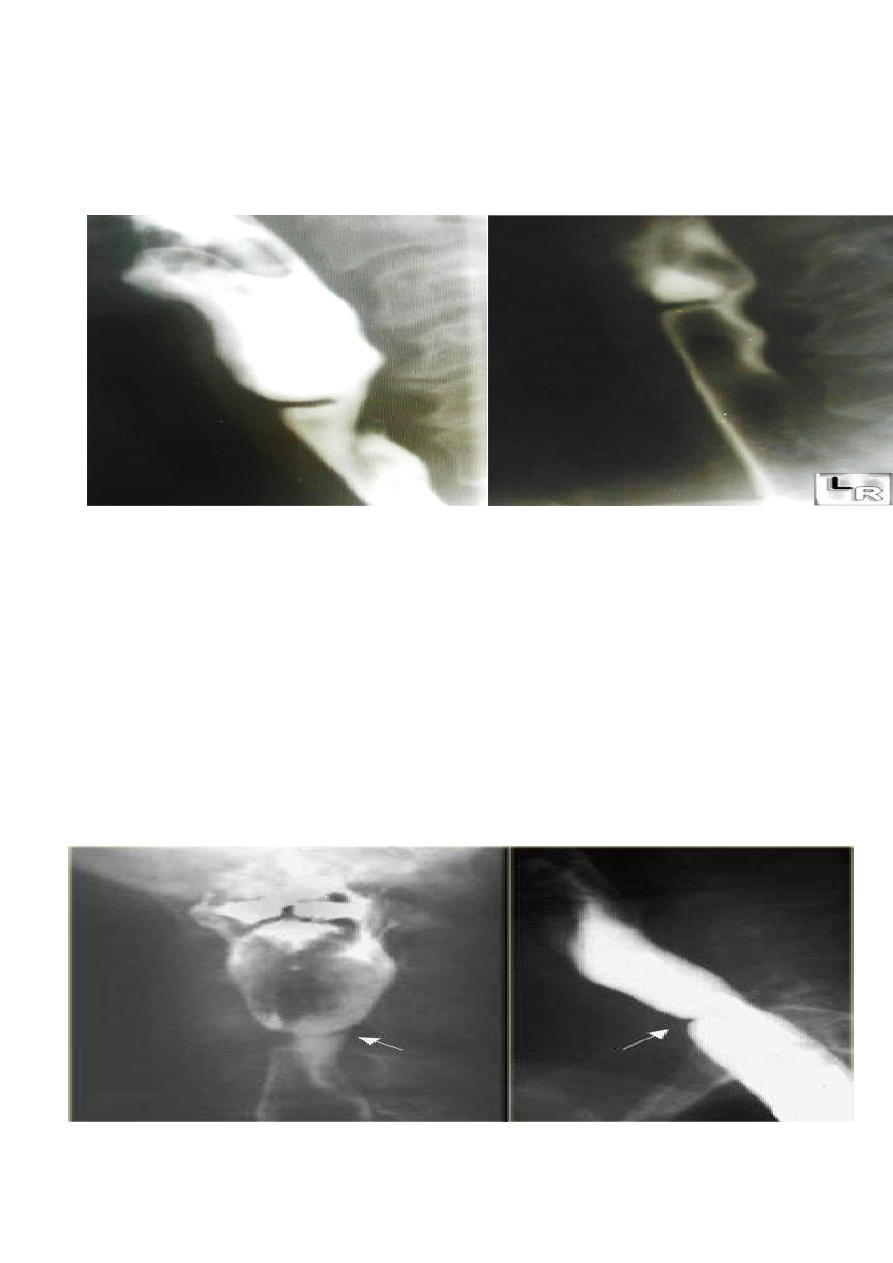
LEFT: Dilated esophagus (arrows) appears as long, well-defined structure paralleling heart
RIGHT: Dilated esophagus usually deviates to right. Narrowing (arrow) at hiatus.
LEFT: CT shows dilated esophagus (arrow) that led to esophagram.
RIGHT: Esophagram shows narrowing (arrow) at level of hiatus.
15
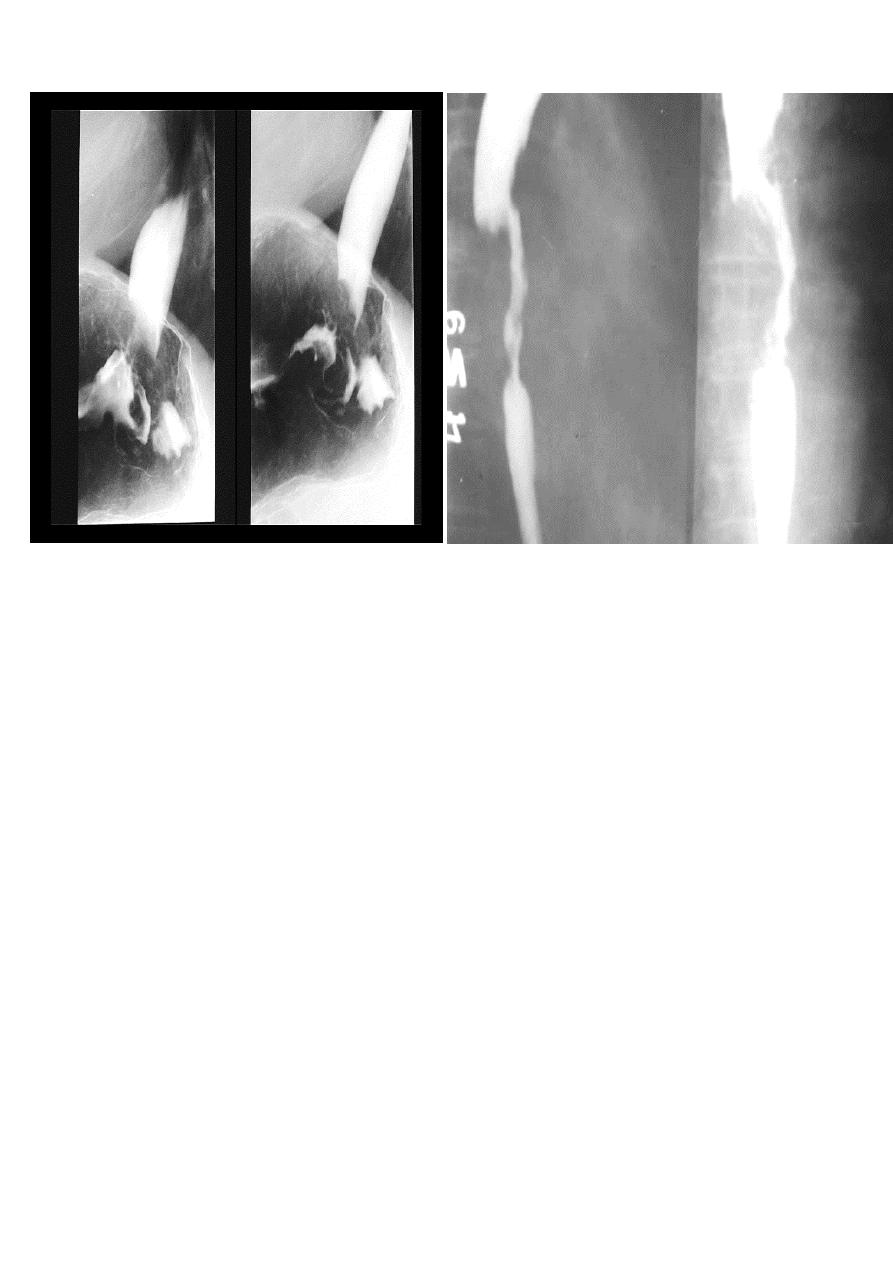
PULSION DIVERTICULUM
Due to:
1. raised intra-luminal tension
2. Chocking after meal .
3. In cervical portion at level of C5
4. Posteriorly (Killience dehiscent)
5. Lateral view show increased pre-vertebral space with air fluid level.
6. Confirmed by Ba. Swallow.
16
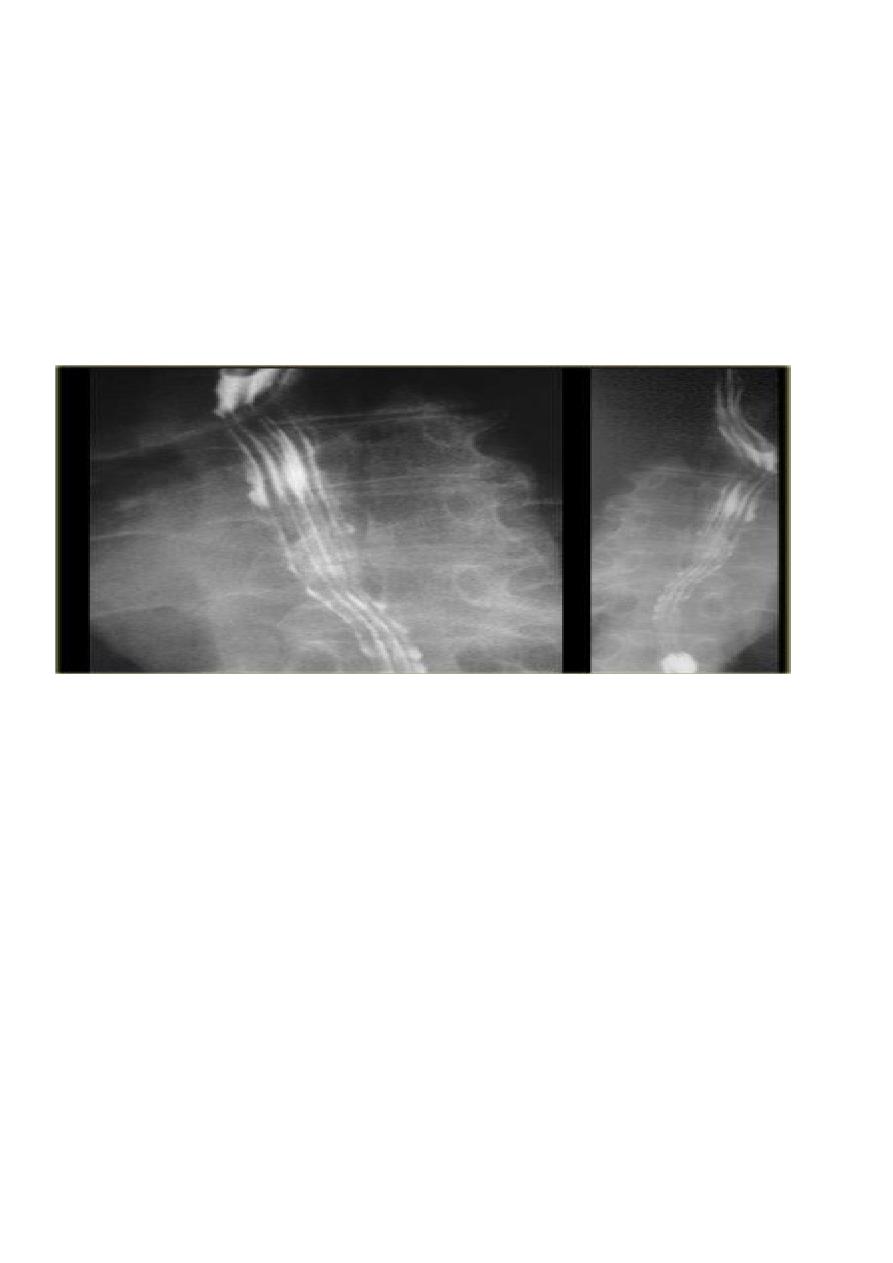
TRACTION DIVERTICULUM
1. Out pouching of lumen laterally due to fibrosis &
adhesions ( post-Tb.)
2. In the middle third at level of hilum
3. Up ward direction of diverticulum
4. Irregular base
17
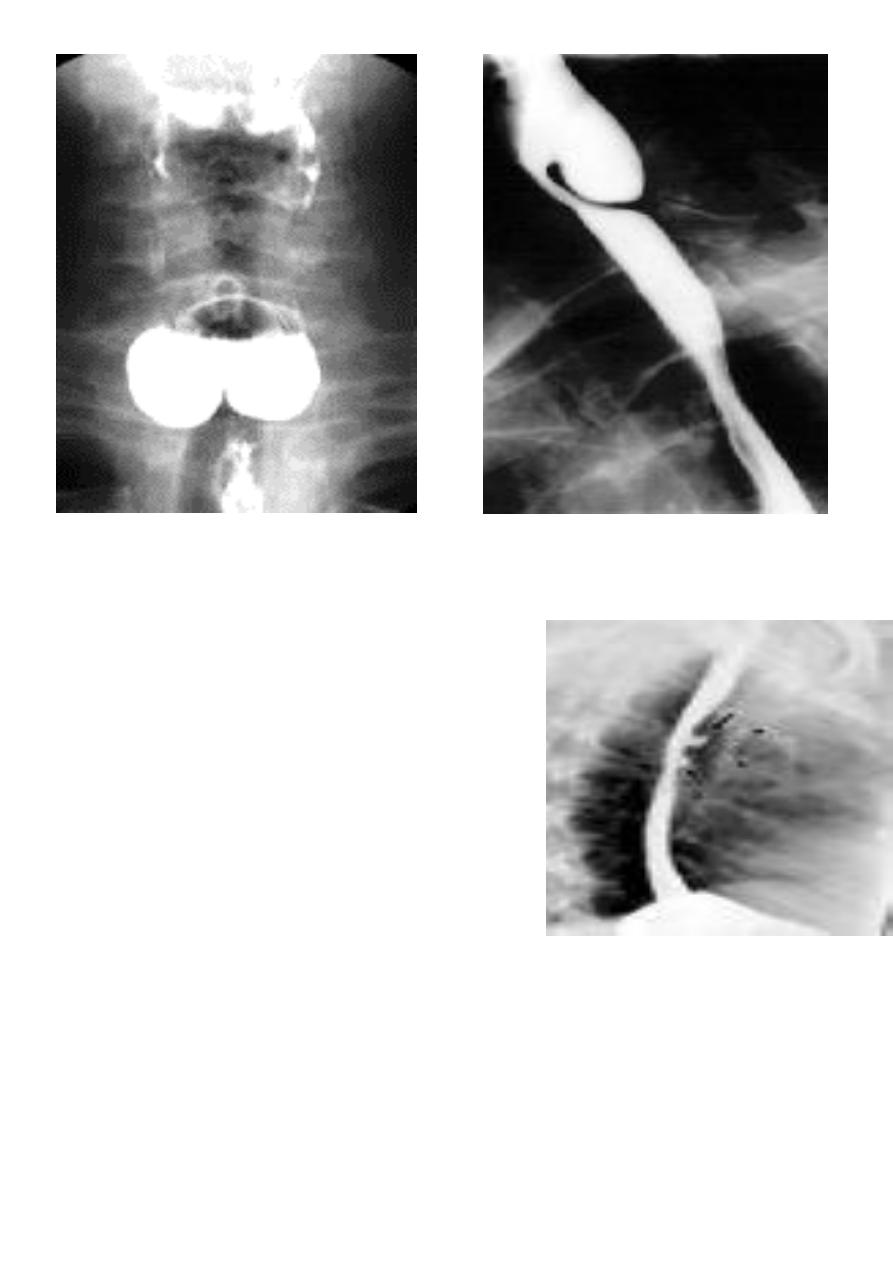
On the far left a traction diverticulum (arrow) due to hilar granulomatous disease.
Calcified adenopathy (asterisk).
In the middle a pulsion diverticulum (arrow) due to high intra luminal pressure.
On the right multiple pulsion diverticula (arrows)
CONGENITAL DIVERTICULUM
1. Asymtomatic unless complicated.
2. At lower part of esophagus above the diaphragm (Epi-phrenic)
3. Lateral or posterior in position.
18
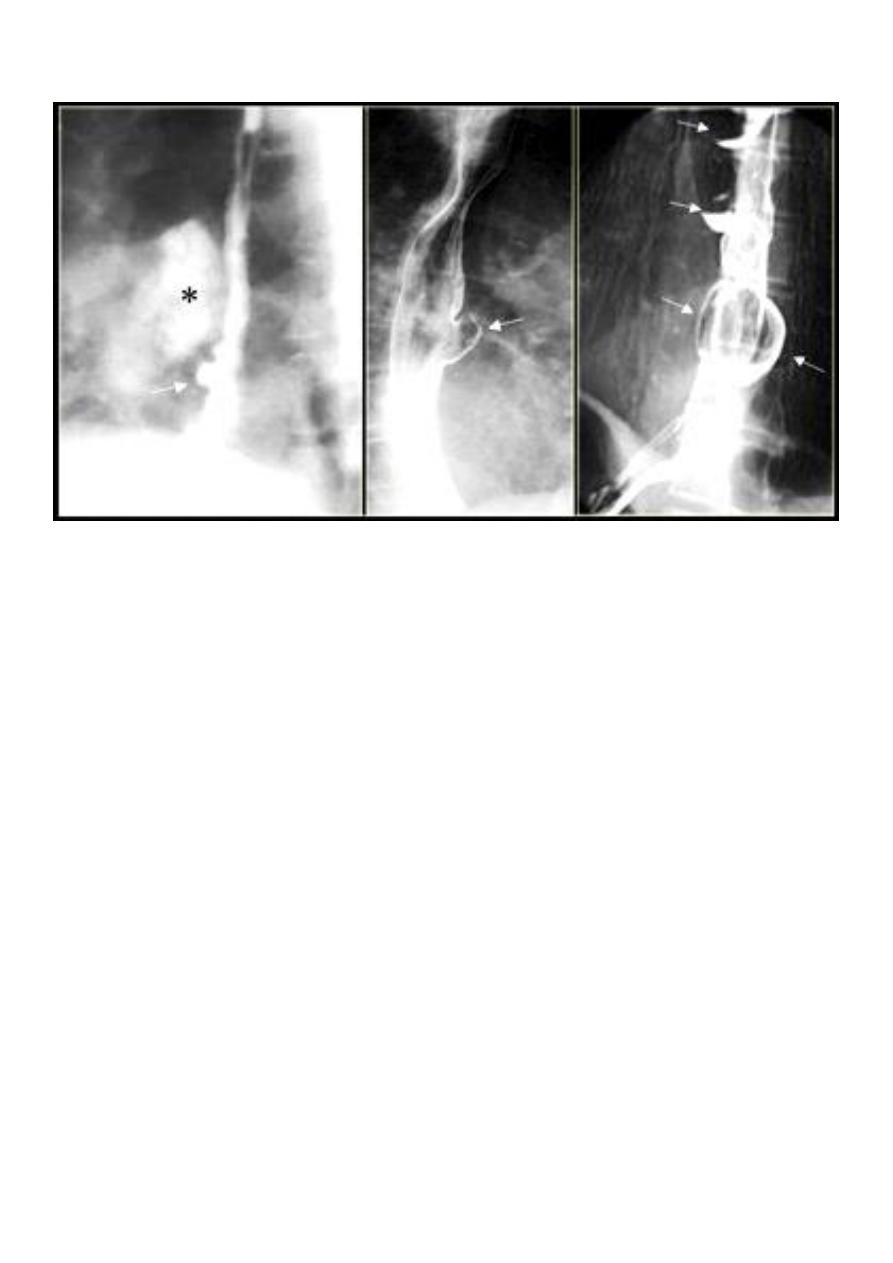
Sliding hernia
On the left initially, GE junction is below the esophageal hiatus.
Later, stomach protrudes through hiatus
19
Para esophageal hernia
On the far left gas filled gastric funds (asterisk) protrudes through hiatus but GE junction
(arrow) is below diaphragm
21
ESOPHAGEAL WEB
1. Thin mucosal fold (membrane)
2. Arise from anterior wall and extend Posteriorly .>>>MCQ
3. Lateral view Ba. Swallow show self like filling defect with proximal dilatation.
4. Single or multiple.
10% incidence at autopsy
Can be congenital or acquired
Most in hypopharynx and proximal esophagus
Majority protrude from anterior esophageal wall
Symptoms if lumen > 50% compromised
Sideropenic dysphagia (Plummer-Vinson syndrome) which is :
1. Iron deficiency anemia
2. Esophageal web with dysphagia
3. Increased incidence of carcinoma
4. Validity of syndrome debatable
21
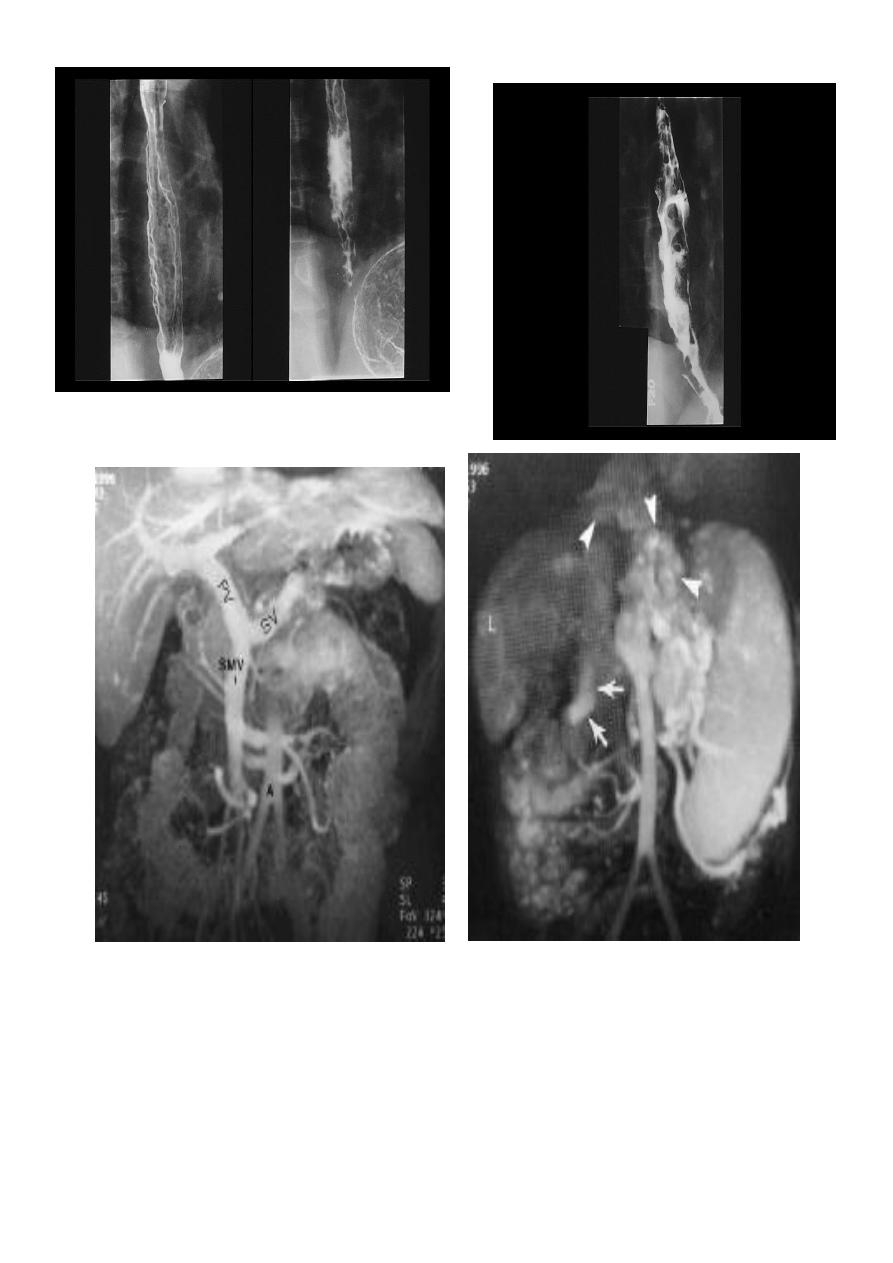
Esophageal Varieces
1. Dilatation of venous plexus in the wall of the esophagus due to increased pressure (
portal H.T.).
2. Important cause of Hematemesis .
3. Early changes seen in the mucosa (D.C.) loss of parallelism with thick and tortuous
folds.
4. Later multiple small filling defects (fine cobble stone).
5. In advanced stage large filling defects ( coarse cobble stone ) .
6. 7More advanced stage elongated and worm like filling defect .
7. The changes are seen at lower third and gastric fundus.
22
23
Stomach & duodenum
Barium meal
Barium meal is radiological study of esophagus,stomach&duodenum.
Done by oral administration of contrast media”Barium Sulphate”
Indications:-
1. Gastric or duodenal obstruction.
2. Malignancies of gastroesophageal junction,stomach &duodenum.
3. Upper Abdominal mass.
4. Motility disorders.
5. Systemic disease like Tb.
6. GIT hemorrhage.
Barium meal
Fluoroscopy + spot films Preparation
The Normal Anatomy of Stomach
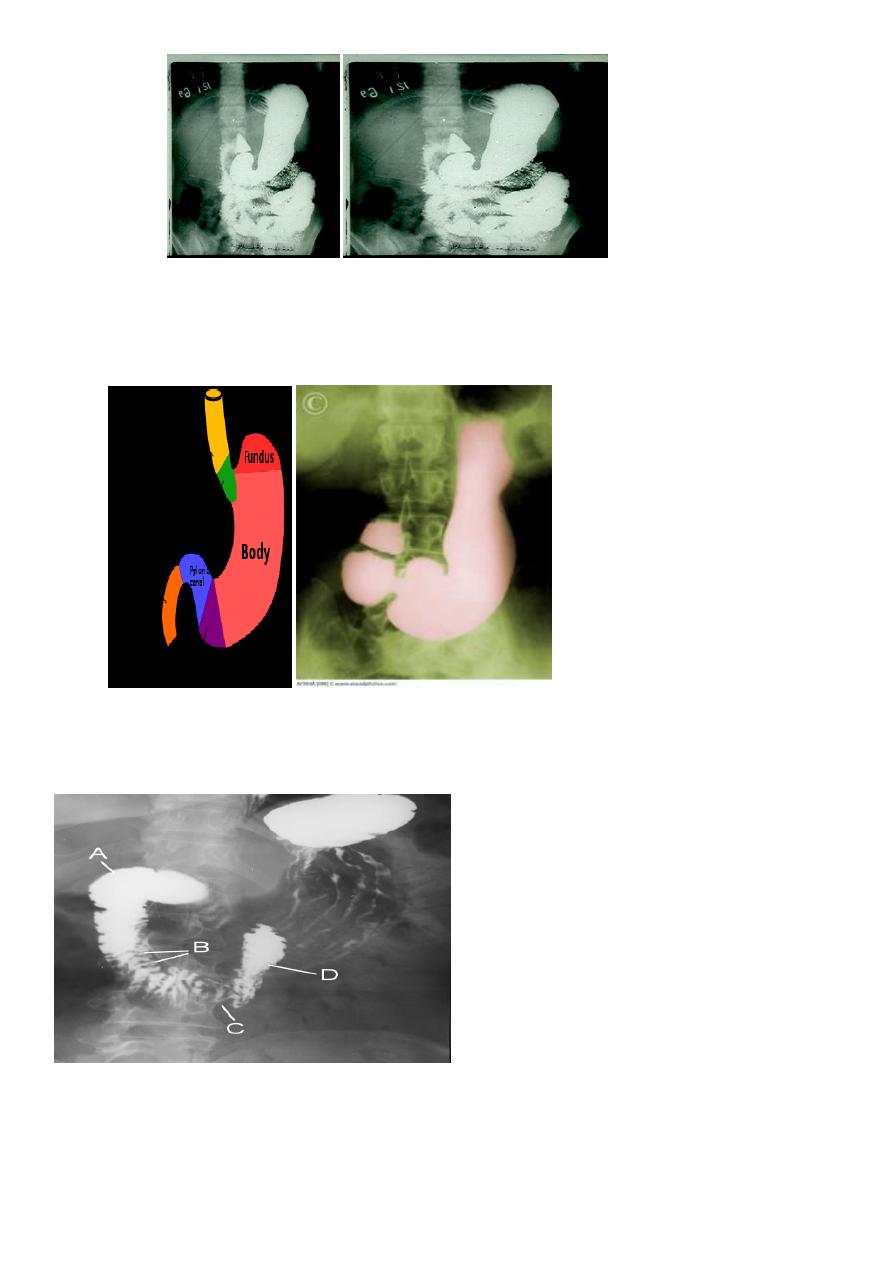
24
1- Shape.
2-Size.
3-Site.
4-Anatomical parts.
5-Mucosal pattern.
Normal Anatomy of Duodenum
A.Duodenal cap.
B.Duodenal loop
25
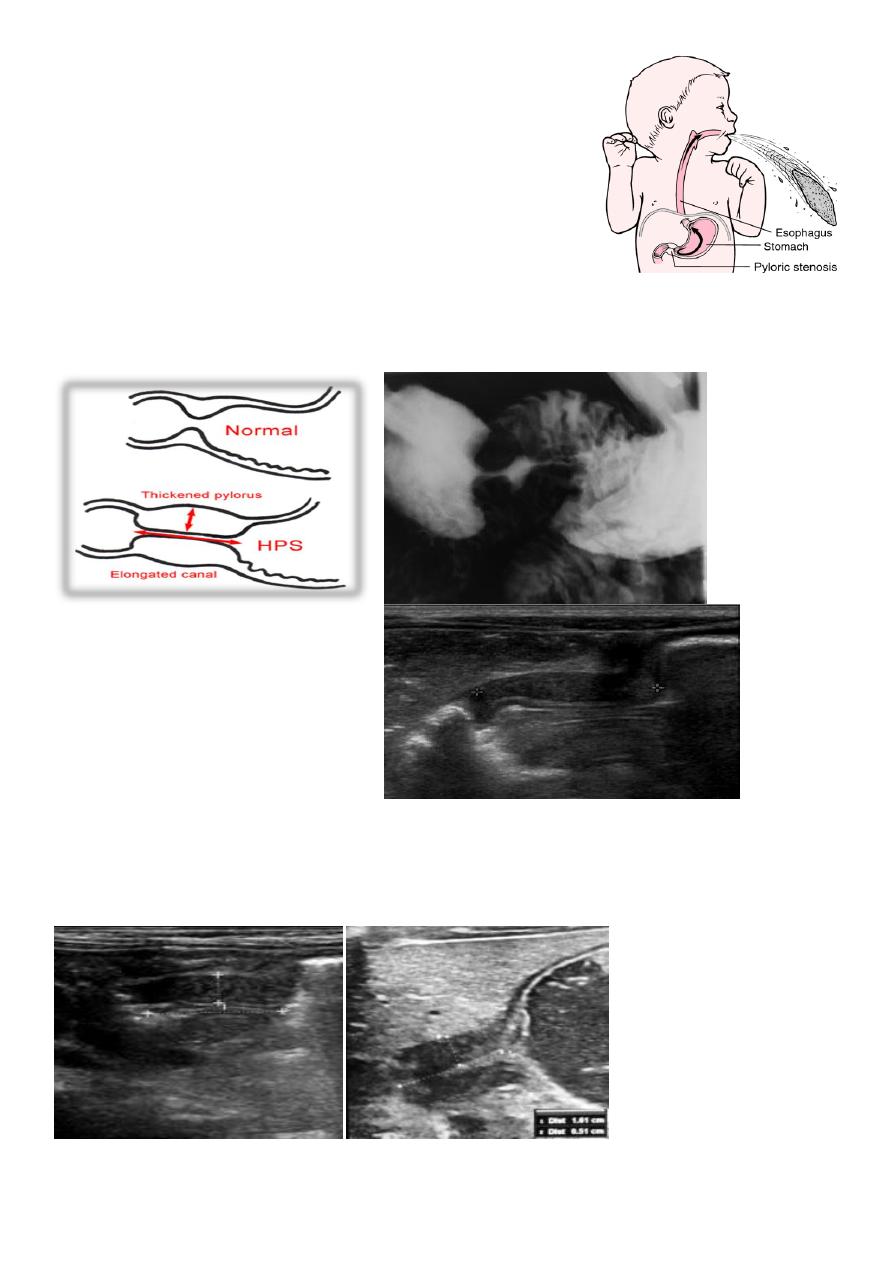
Hypertrophic pyloric stenosis
Cause:
A. Congenital type
B. Adult type
Epidemiology:-
Pyloric stenosis is relatively common and has a male
predilection (M:F ~ 4:1), and is more commonly seen in Caucasians
4
.
It typically occurs between the 4-8 weeks of life. There may be a positive family history.
Incidence of hypertrophic pyloric stenosis is approximately 2-5 per 1,000 births per year in
most white populations.
In a normal situation, the pyloric muscle thickness (diameter of a single muscular wall on a
transverse image) should normally be less than 3 mm (most accurate
3
) and the length
(longitudinal measurement) should not exceed 15 mm.
26
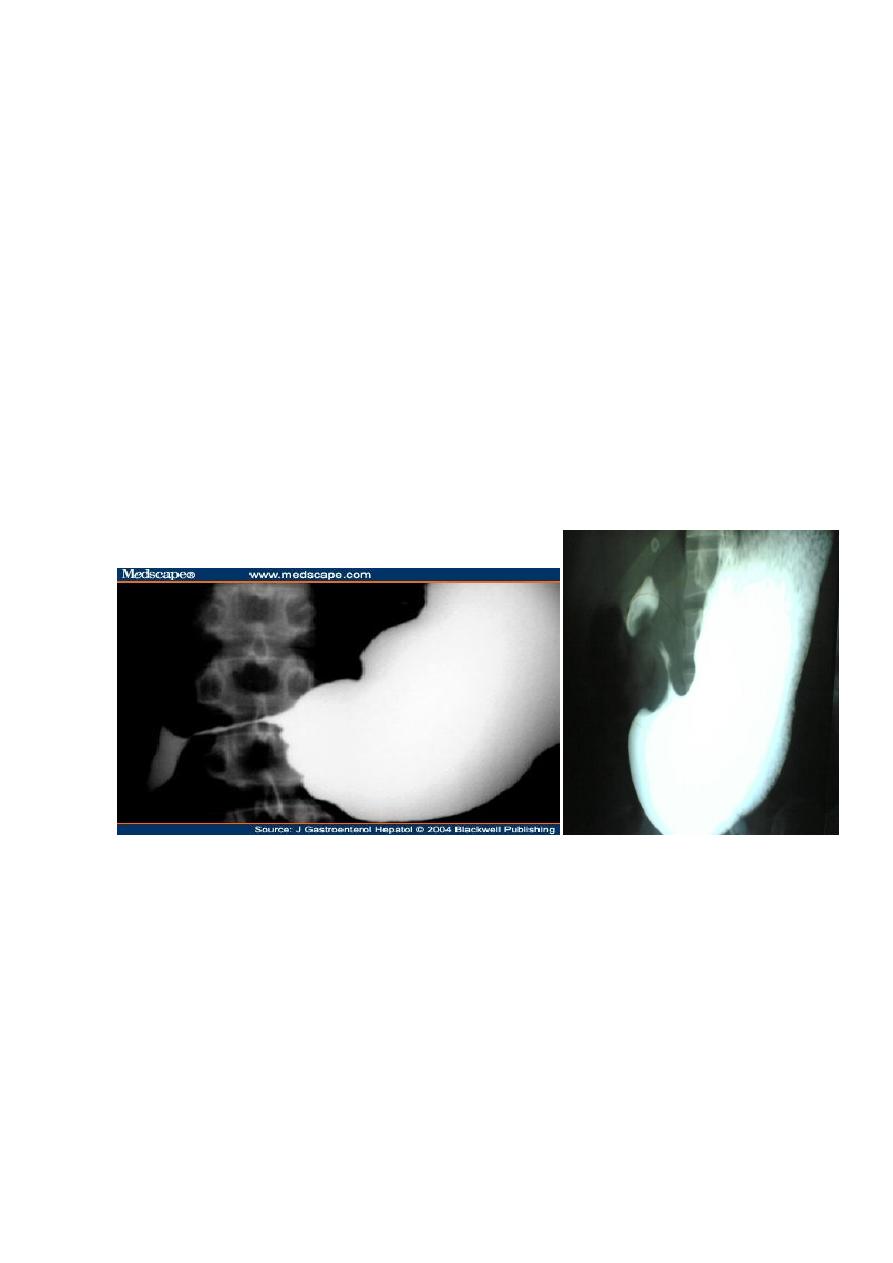
Gastric outlet obstruction (often abbreviated as GOO)
:-
is a medical condition where there is an obstruction at the level of the pylorus, which is
the outlet of the stomach.
Individuals with gastric outlet obstruction will often have recurrent vomiting of food that
has accumulated in the stomach, but which cannot pass into the small intestine due to the
obstruction.
The stomach often dilates to accommodate food intake and secretions.
Causes
:-
1-benign causes (such as peptic ulcer disease affecting the area around the pylorus.
2-malignant causes, such as gastric cancer.
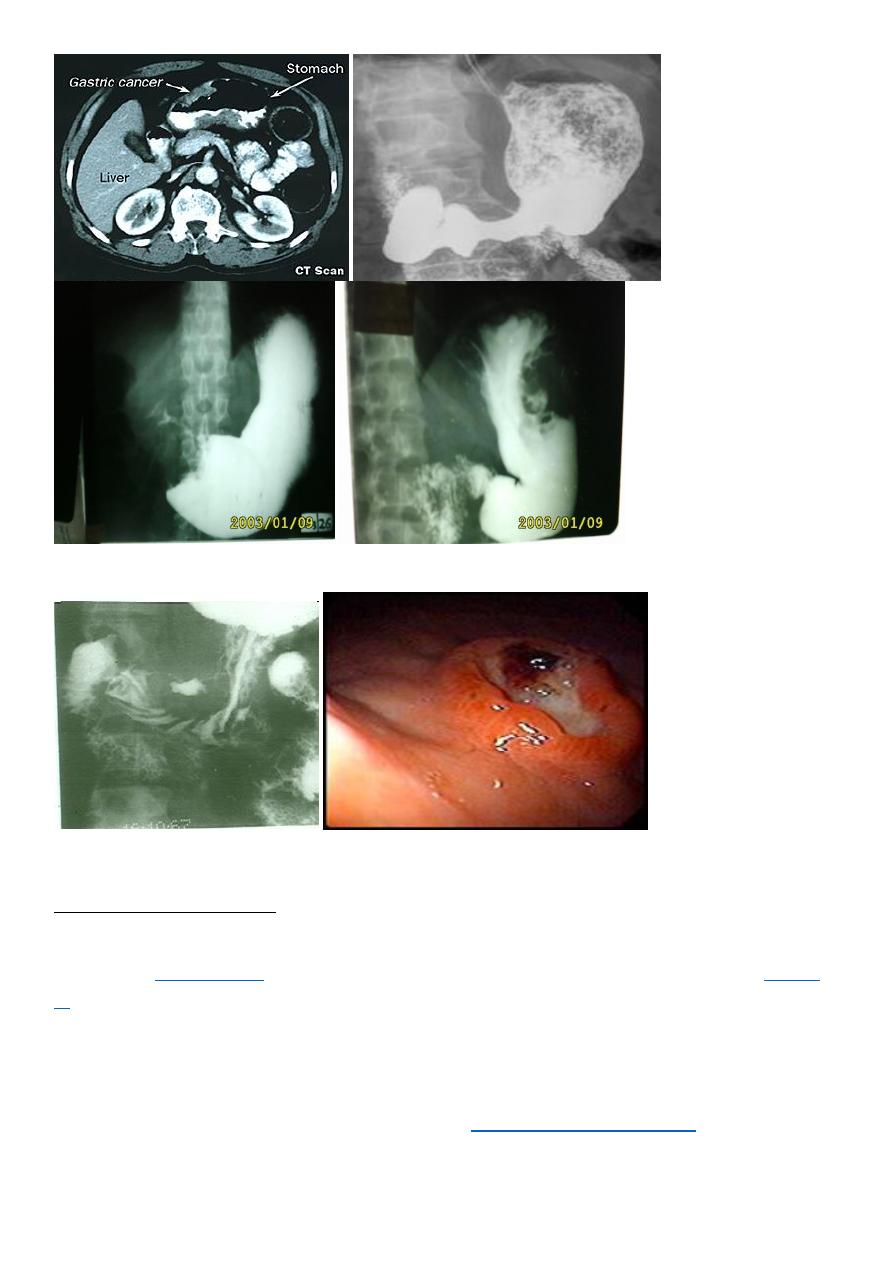
Radiographic Ba meal examination of the Pyloric stenosis:-
1. Marked dilatation of the stomach attends the pelvic cavity
2.Failure of passage of contrast into the duodenum.
3.Multiple filling defects are seen within the stomach due to retained food material .
Barium meal image of a case of corrosive-induced
GASTRIC CA
gastric outlet benign narrowing
PEPTIC ULCER((GU, DU and IU))
The Ba. meal findings are :
1-Direct signs :
* Ulcer crater ( nitch):
Either in enface or in profile
* Associated signs:
I. Spasm
II. Radiated mucosal folds.
III. Edema (Hampton's line).
2- Indirect signs :
27
I. Hyper peristaltic waves.
II. Companion B sign.
III. Thick mucosal folds & hyper peristaltic stomach
(angry mucosa)
Radiographic Signs of a benign gastric ulcer
Ulcer crater-collection of barium on dependent surface which usually projects beyond
anticipated wall of stomach in profile (penetration)
Hampton’s line-1 mm thin straight line at neck of ulcer in profile view which represents the
thin rim of undermined gastric mucosa
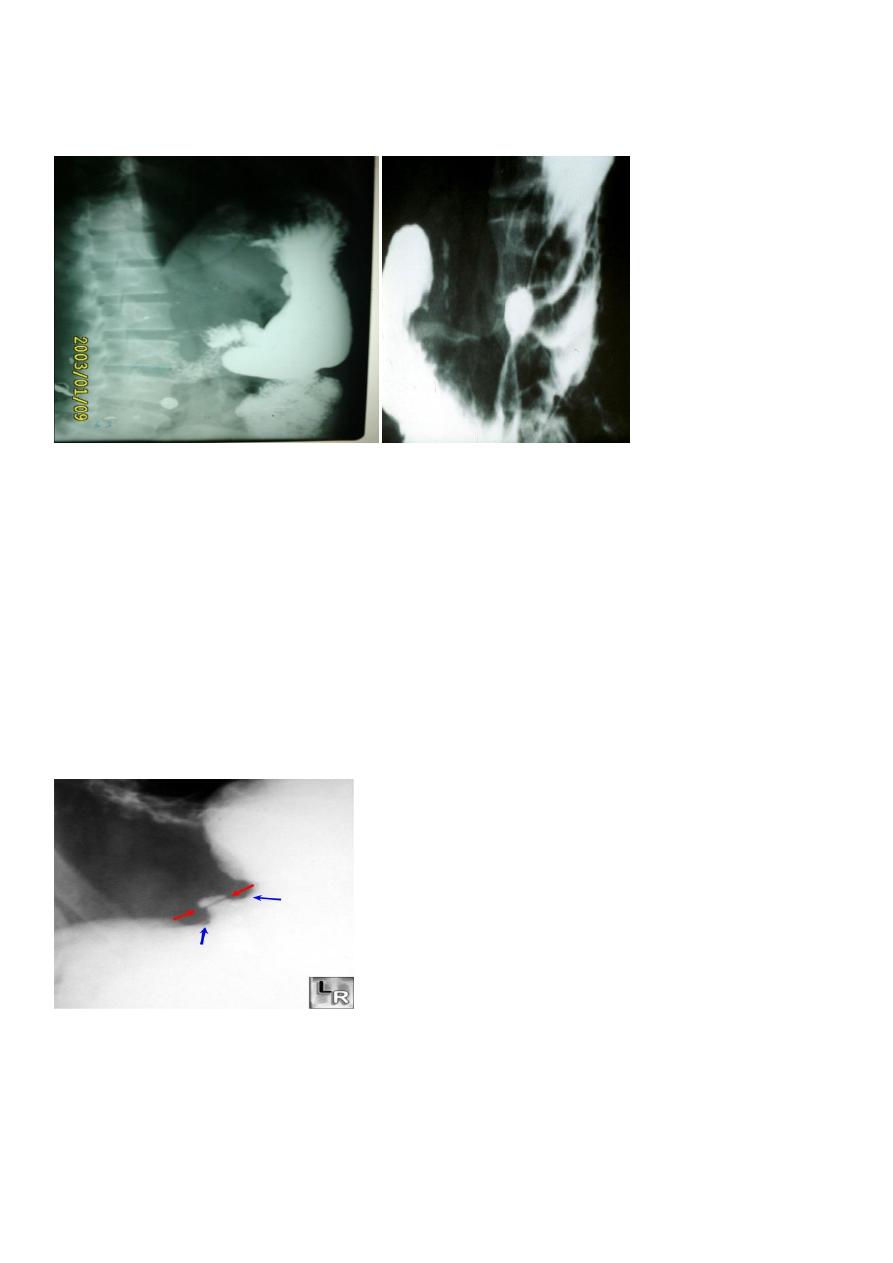
lesser curvature gastric ulcer. Red arrows point to Hampton's Line, a thin, straight line at
neck of ulcer in profile view which represents the thin rim of undermined gastric mucosa.
The blue arrows point to the
ulcer mound, a smooth, sharply delineated soft-tissue mass surrounding a benign ulcer.
Note how the ulcer projects beyond the confines of the expected wall of the stomach.
28
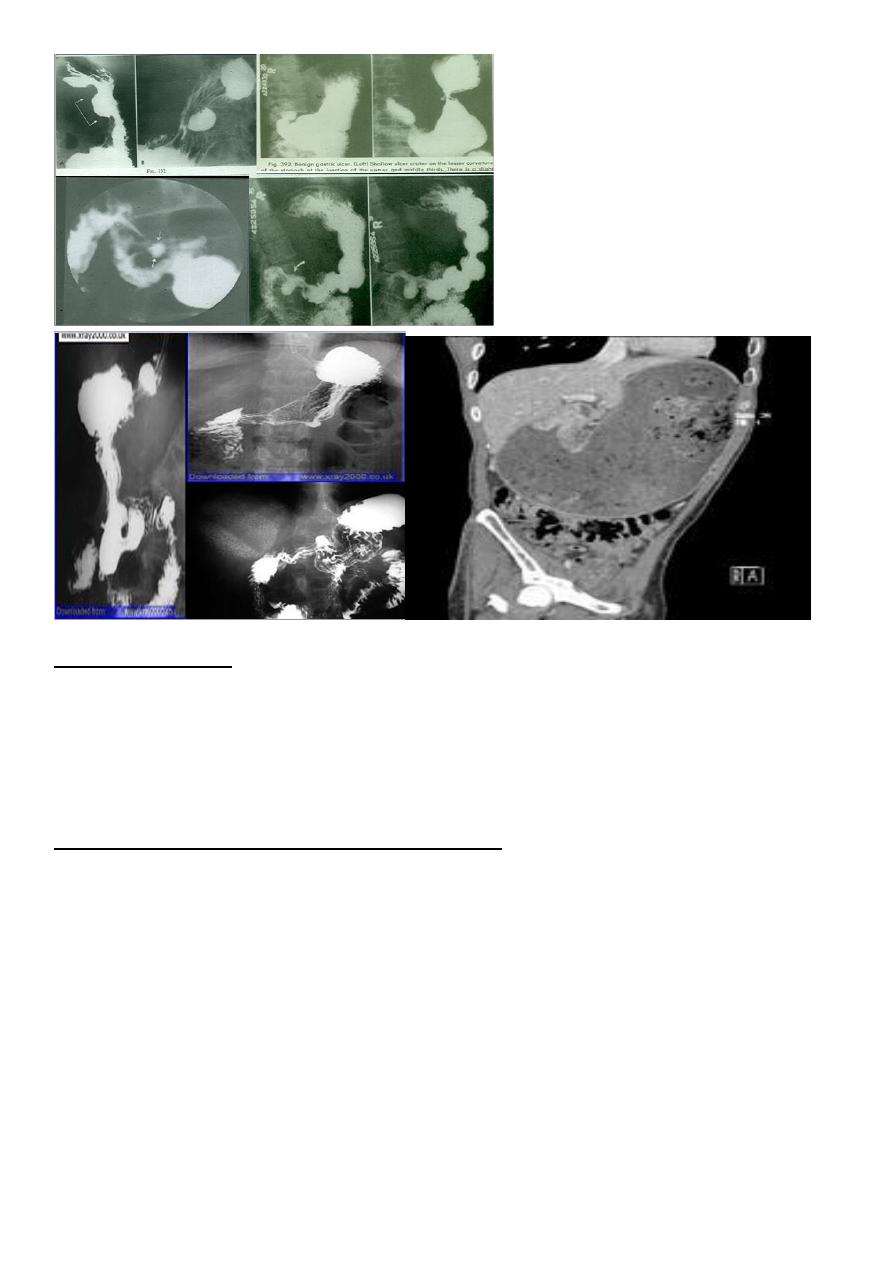
Gastric carcinoma
refers to a primary malignancy arising from the gastric epithelium.
3 presentation
1. Polypoidal
2. Infiltrative * localized * generalized
3. Ulcertaive type
barium meal presentation of the CA stomach
1.Carcinoma produce single or multiple irregular filling defect with alteration of near by
mucosal Pattern .
2.Localized or generalized narrowing of the stomach rigid in appearance with shoulding
sign on either sided aspect of the narrowing .
3- Ulcerative Ca Either :
I.Polypoidal tumour with ulceration or
II. Complicated benign gastric ulcer
on Ba. Meal :
* Filling defect with central ulcer crater
* No mucosal radiation , due to destruction .
* The ulcer crater is not projected out side the lumen ( meniscus sign )
* Hour glass deformity ( X ) of stomach
29
Duodenal ulcers (DUs)
affect nearly 10% of the adult population at some time,and these lesions account for two
thirds of all
, which are defined as mucosal breaks of 3 mm or greater;
cer accounts for the rest
Most duodenal ulcers are depicted as round or ovoid pools of barium; about 5% may be
linear, and most are smaller than 1 cm in diameter. Giant duodenal ulcers, defined as those
>2 cm in diameter, have an increased risk of perforation, obstruction, and bleeding.
Multiple ulcers occur in about 15% of patients
[1]
considered in these patients.
31
About 95% of duodenal ulcers occur in the duodenal bulb,
[1]
and the rest occur in the post
bulbar duodenum, bulber U which consists of the proximal 2 cm of the descending
duodenum above the ampulla of Vater. As many as half of all duodenal ulcers occur in the
anterior wall of the bulb.
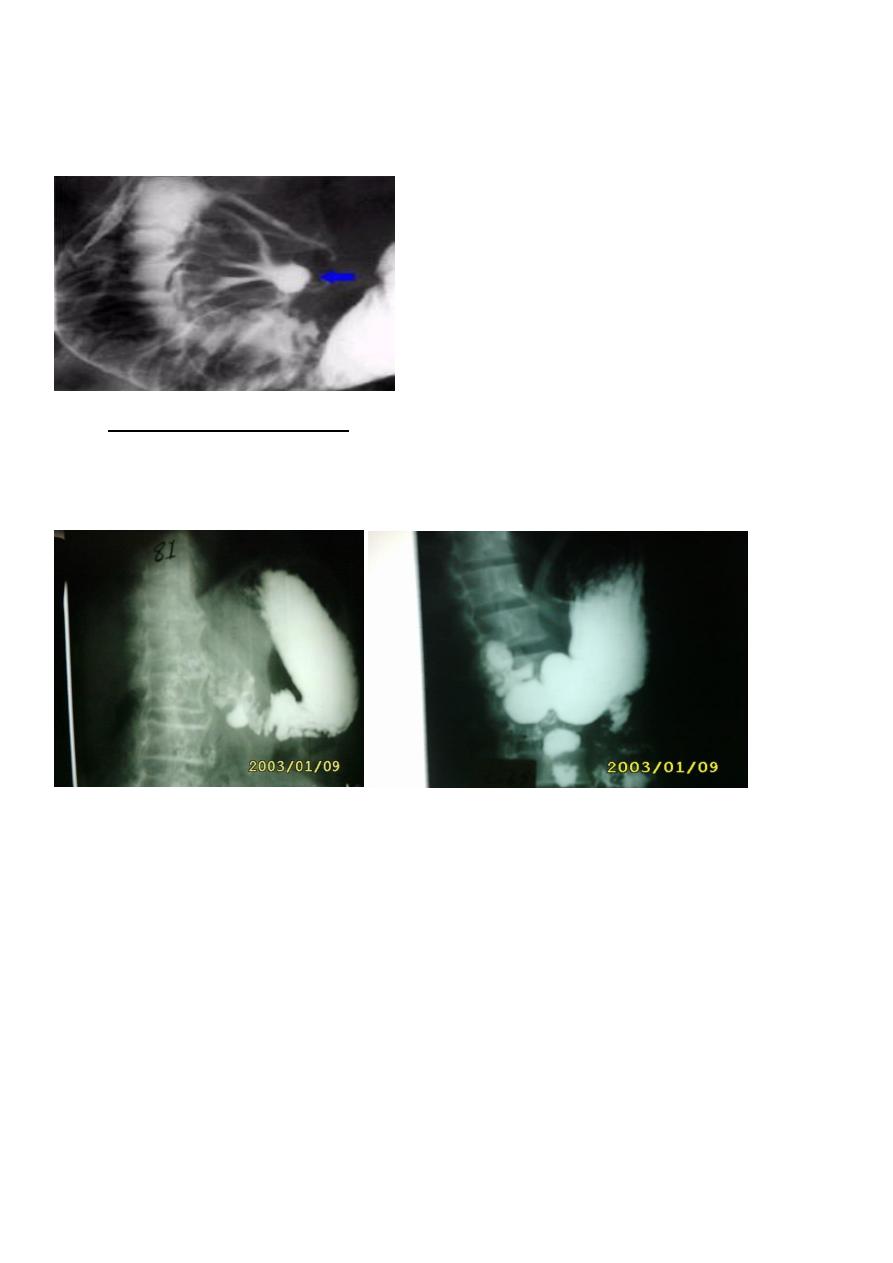
Complicated Chronic DU
1-Tri foil deformity ( tri foil tree )
2-Pseudo diverticulum (Akerland diverticulum)
3-Gastric outlet obstruction.( pyloric obstruction ).
During Ba examination
Bird's Beak deformity of lower oesophagus - Achalsia cardia (Barium Swallow)
Cork screw oesophagus-- Diffuse oesophageal spasm (Barium Swallow)
Commonest radiological appearance of gastric
Trifoliate duodenum - Chronic duodenal ulcer with scarring (Barium Meal)
Hour Glass stomach - Peptic ulcer
Single-bubble appearance - pyloric stenosis
Double-bubble sign--Duodenal atresia, duodenal stenosis.
Triple-bubble sign - Jejunal atresia
Coiled spring appearance -Intussusception
