TRUMA OF THE LOWER LIMB
Fracture of the femoral neck in adults
*The femoral neck is the commonest site of
fractures in the elderly.
*The femoral neck fracture occurs more in
Caucasian elderly women [postmenopausal].
*Other risk factors = bone weakening disorders
e.g. osteomalacia , diabetes, stroke [disuse]
and alcoholism.
*The femoral neck fracture occurs less in
negroid populations and in patients with
osteoarthritis of the hip joint.

Mechanism of injury
In elderly
= fall directly onto the greater
trochanter.
In very osteoporotic people
= less force is required
, perhaps no more than catching a toe in the
carpet and twisting the hip into external
rotation.
In younger individuals
= fall from a height or a
blow sustained in aroad accident , these
patients have multiple injuries and in 20 % there
is an associated fracture of the femoral shaft.

Pathological anatomy and classification
The femoral head obtains its blood supply from 3
sources =
1
‐Intramedullary vessels in the femoral neck.
2
‐Ascending cervical branches of the medial and
lateral circumflex anastomosis , which run within
the capsular retinaculum before entering the
bone at the egde of the femoral head.
3
‐The vessels of the ligamentum teres.
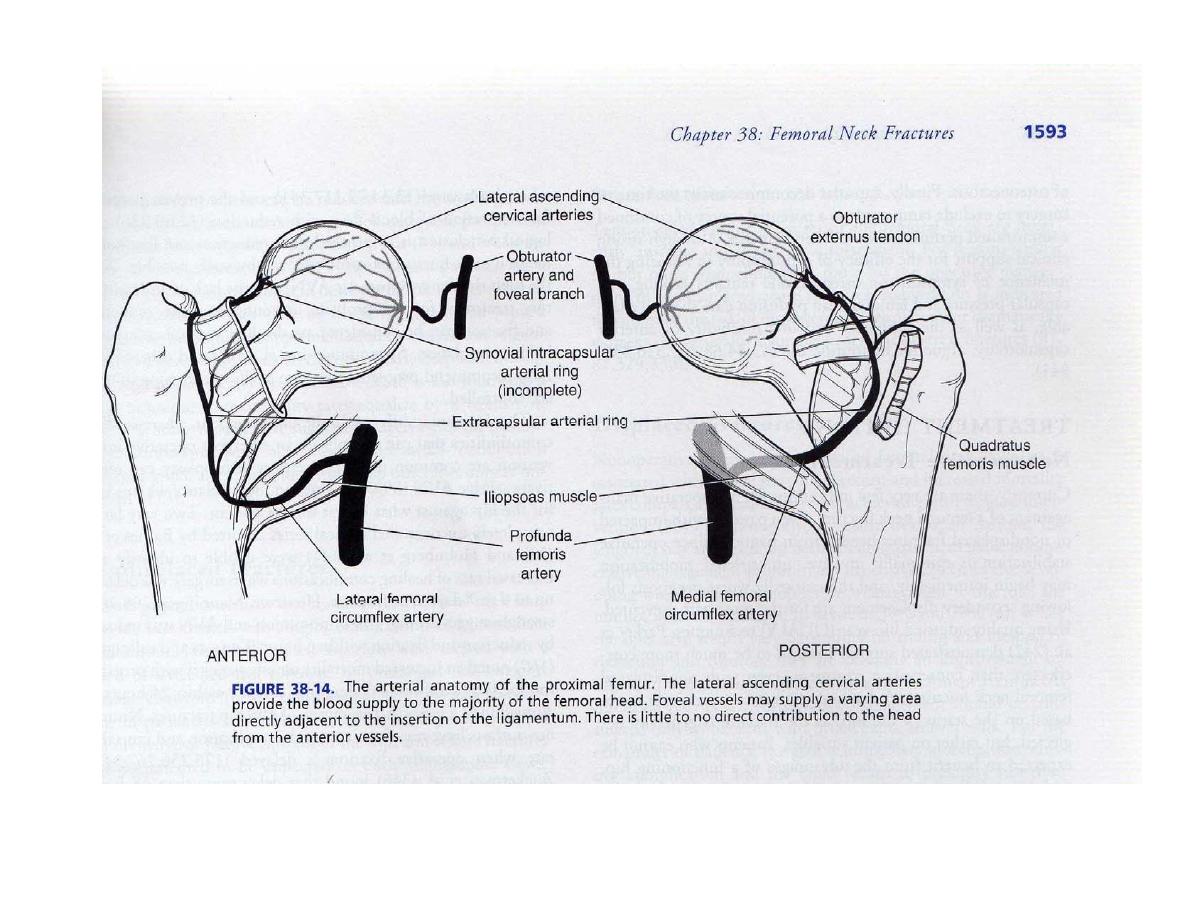

*The intramedullary supply is always
interrupted by the fracture.
*The retinacular vessels also may be kinked or
torn if the fracture is displaced.
*In elderly people , the remaining supply in the
ligamentum teres is at best fairly meagre and
in 20 % of cases non‐existent.

SO
there is high incidence of a vascular necrosis
of the femoral head in displaced femoral neck
fractures.
Femoral neck fractures are
INTRACAPSULAR
,they
have a poor capacity for healing because =
1
‐By tearing the capsular vessels , the injury
deprives the head of its main blood supply.
2
‐Intra‐articular bone has only a flimsy periosteum
and no contact with soft tissue which could
promote callus formation.
3
‐
Synovial fluid prevents clotting of the fracture
haematoma.

SO
there is high incidence of non‐union in
fracture neck of femur.
*For both prognostic and therapeutic purposes
, the femoral neck fracture can be classified
as =
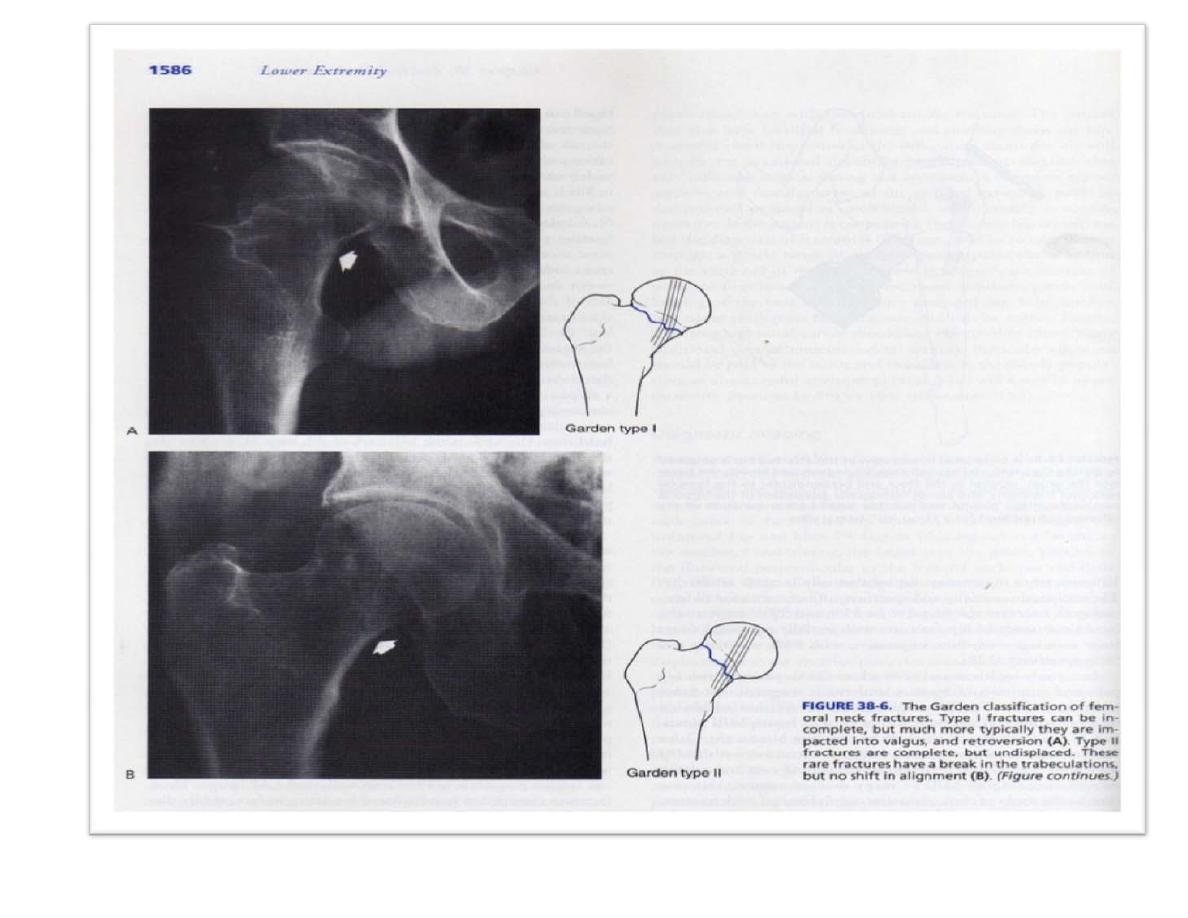
*Garden classification
It is most useful classification , which is based
on the amount of displacement apparent in
the pre‐reduction x – ray.

Stage 1
= is an incomplete impacted fracture ,
including the so called abduction fracture in
which the femoral head is tilted into valgus in
relation to the neck.
Stage 2
= is a complete but
undisplaced
fracture
.
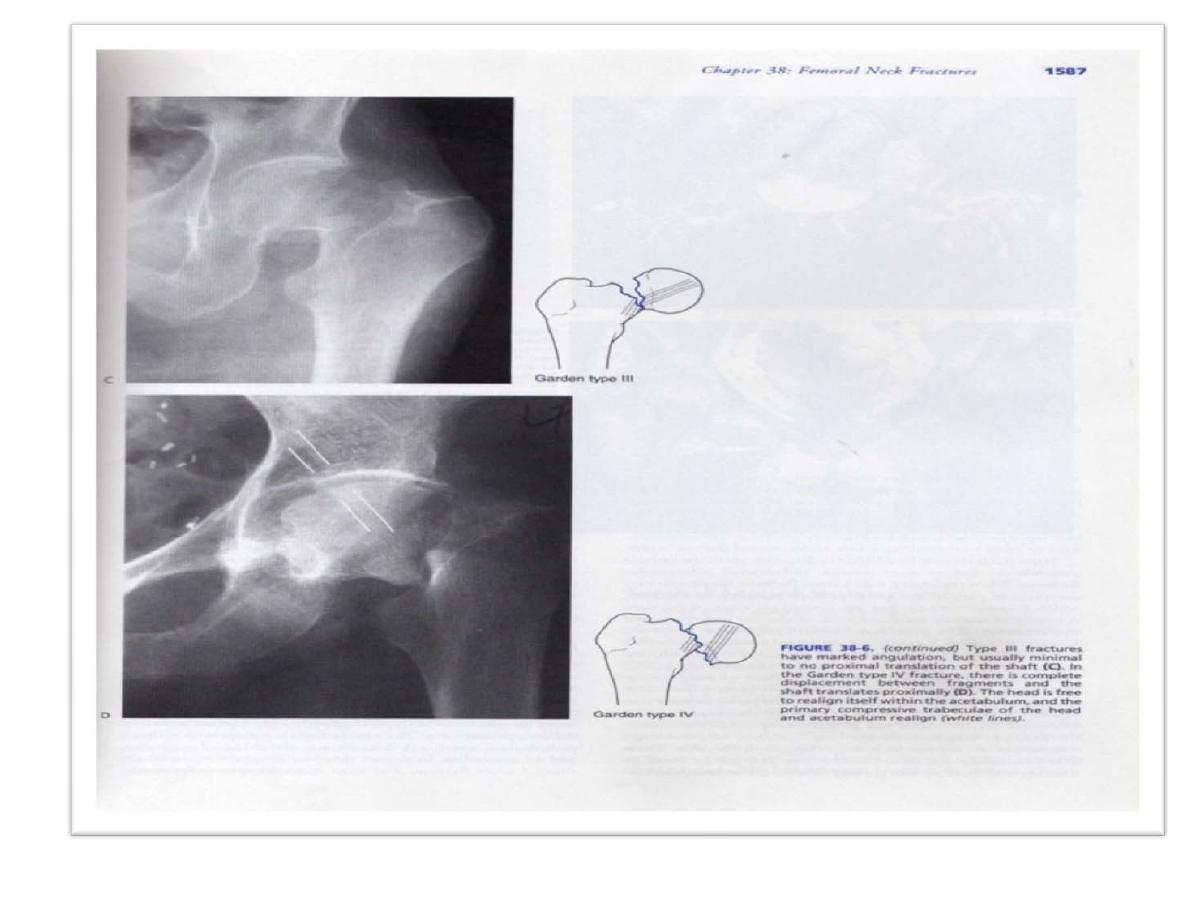
Stage 3
= is a complete fracture with moderate
displacement.
Stage 4
= is a severely displaced fracture
.

*Garden
1
and
2
are only slightly displaced
and have a much better prognosis for
union and for viability of the femoral head
than the more severely displaced Garden
3
and
4
fractures.
*
Stage 1
fracture may rapidly progress to
stage 4
fracture.

*
Pauwel classification
Pauwel classified the fracture according to the
increasing verticality of the fracture line from the
horizontal.
1
‐Less than 30 degree.
2‐
Between 30 and 50 degree.
3
‐
More than 50 degree
.
*
Anatomically
the fracture of the femoral neck can
be
1‐
subcapital.
2
‐
Transcervical
.
3
‐
basal
.

Diagnosis
*
Clinical features
*There is usually a history of a fall , followed by
pain in the hip.
*If the fracture is displaced , the patient lies
with the limb in lateral rotation and the leg
looks short.
BEWARE
=* Not all hip fractures are so obvious.
*With impacted fracture the patient
‐ may still be able to walk.
*In young adults , we should always
examine for an associated fractures.

* X‐RAY
= 2 QUESTIONS must be answered
1
‐
is there a fracture
.
2
‐
is it displaced.[ look for any
degree of mismatch of the Trabecular
lines in femoral head, neck and
supraacetabular Part of the pelvis].

The femoral neck fracture can be missed in
=
1‐Stress fracture
=*usually elderly patient with
unexplained pain in the hip.
*x‐ray may be normal or hairline
fracture.
*bone scan will show the hot lesion
.
2‐ Undisplaced fracture
[impacted fracture], can be
shown on MRI or bone Scan after few days.
3‐Painless fracture
[ silent fracture ] in elderly or bed‐
ridden people.
4‐Pathological fracture
= secondary metastasis , or
multiple myeloma.
5‐Multiple fractures
= patient with femoral shaft fracture
may have femoral neck fracture as well.

TREATMENT
Aim of the treatment
1
‐Accurate reduction of the fracture.
2
‐
Adequate and rigid fixation
.
3
‐
Rehabilitation
=early
mobilization
to
prevent
complication of prolong bed rest.
A
‐
If patient
less than 60
years old.
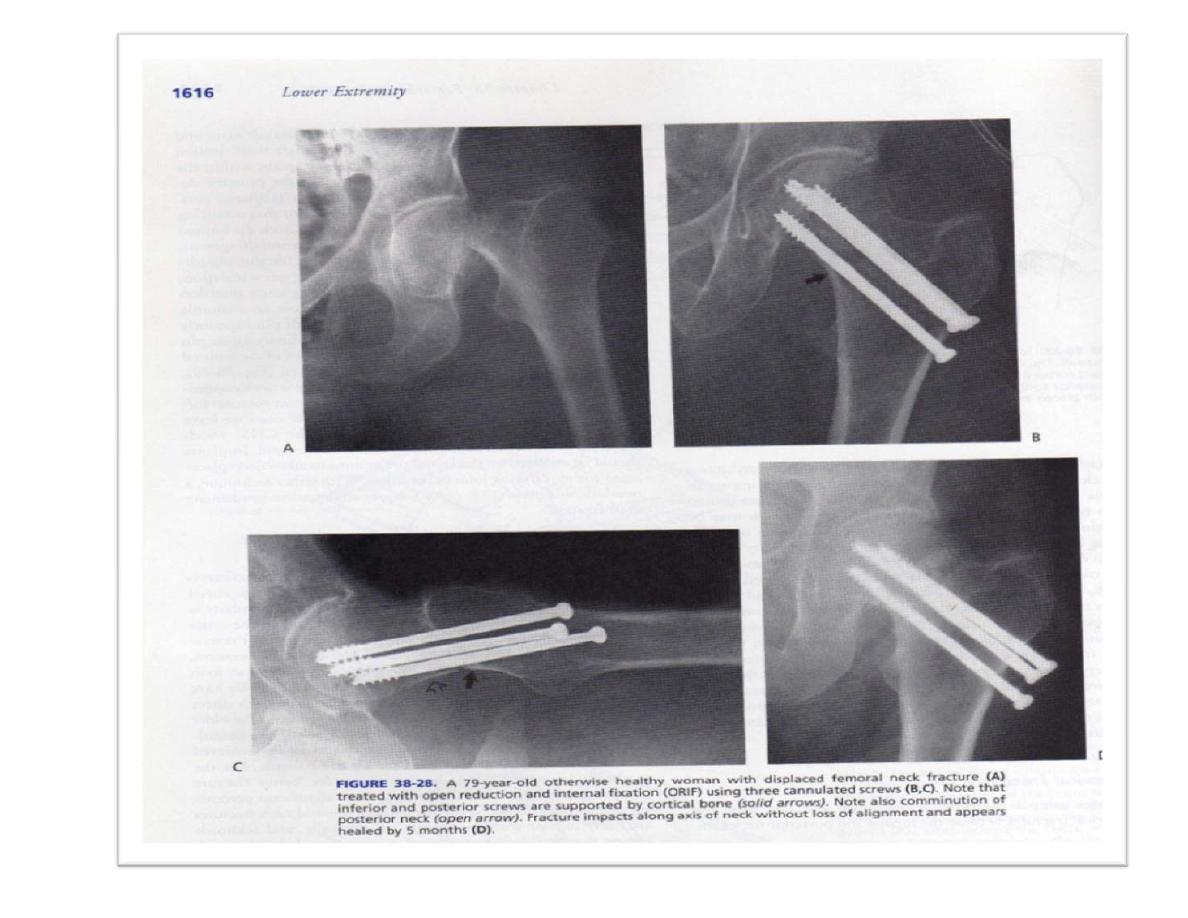
*accurate reduction by either [ MUA ] under x‐ray control
[ closed reduction ] or if failed by open reduction.
*then rigid fixation [ 3 canulated screws or dynamic hip
screw ].
*postoperatively , the patient kept un bed for 2 weeks
then walks with 2 crutches and non ‐weight bearing
for 4‐6 weeks, until healing then gradual weight
bearing.

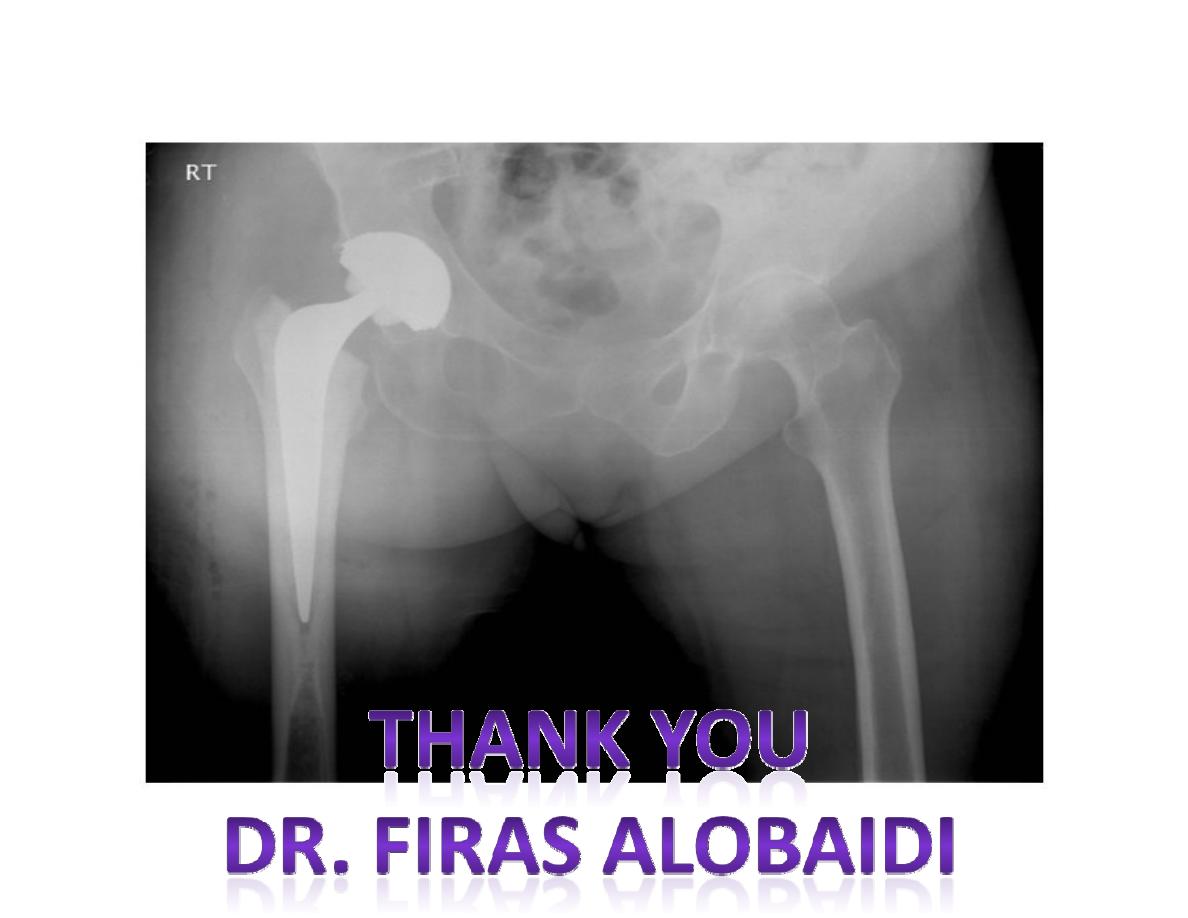
B‐
If patient
more than 60
years old.
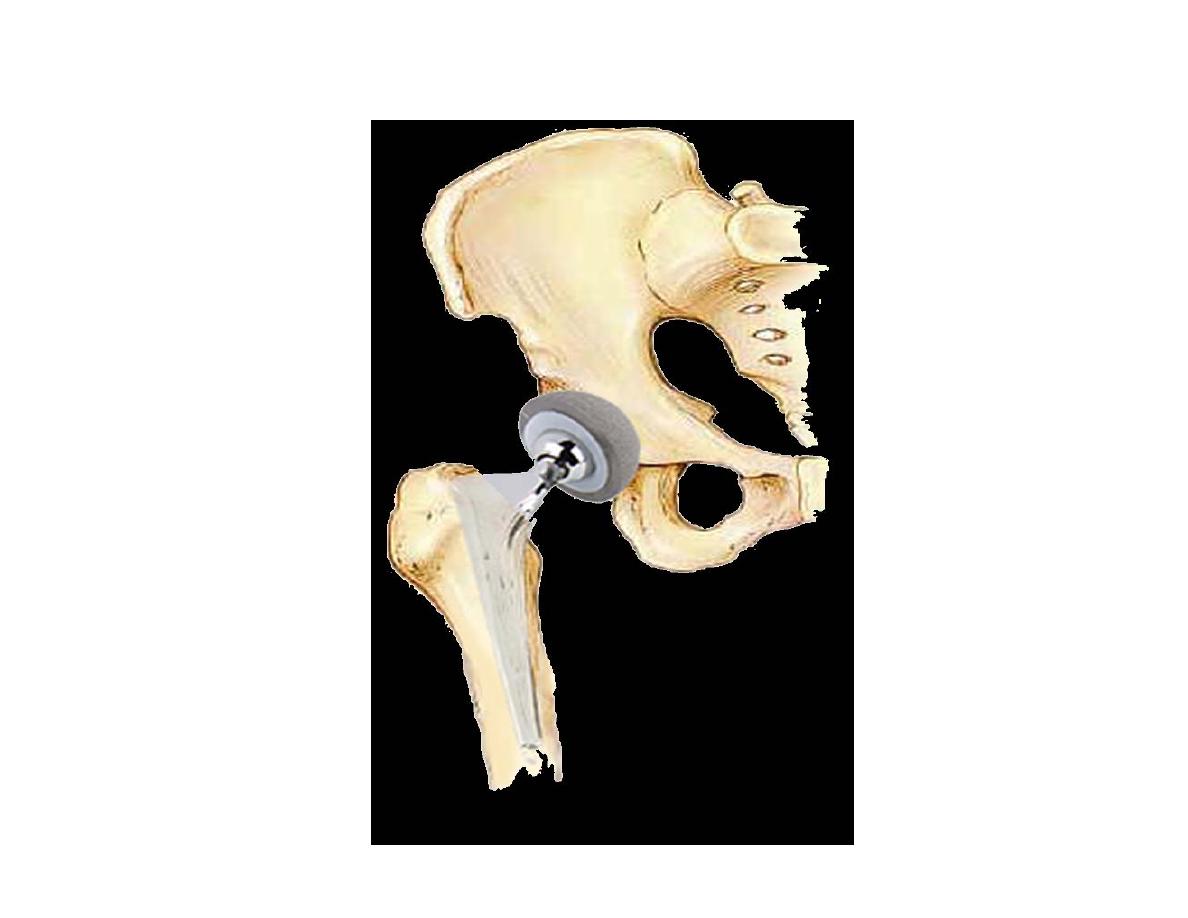
*Because of high incidence of a vascular necrosis of
the femoral head, non –union of the fracture and
serious possible complications of prolonged bed
rest, we prefer to do either partial replacement
arthroplasty [Austin Moore] from the start, or in
cases of failed internal fixation or delayed
fracture with acetabular changes, we can do total
hip replacement arthroplasty.
Post operatively, patient can walk after 1 week with
aids, until patient can walk unaided


Complications
A‐General complications
1
‐
DVT [deep venous thrombosis] with or without
pulmonary embolism.
In some centres, anticoagulants are used routinely
to avoid these fatal complications
.
2
‐
Bed sore =local skin ischemia and necrosis with
secondary infection due to prolonged bed rest.
Good physiotherapy by turning patient in bed every
2 hours ,skin care and pneumatic bed should be
practiced to avoid this complication.
3‐
Hydrostatic pneumonia =also due to prolonged
bed rest.
4
‐
Chronic resistant urinary tract infection.
Try to avoid folly's catheter for long period.

B‐Local complications
1‐Avascular necrosis of the femoral head
*
It occurs in 30 % of patients with displaced fractures and
in 10 % of those with undisplaced fractures
.
*
X‐ray changes occurs after several months or even
years, but bone scan or MRI may show diminished
vascularity and head collapse after few weeks.
*
The patient will complain of progressive pain and loss of
function.
Treatment in adult = total hip replacement arthroplasty.
In younger patients =
*
core decompression
*
Realignmen osteotomy
‐
for small Necrotic segment.

2‐Non‐union
Risk factors= * severe displaced fracture .
*poor blood supply.
*imperfect reduction.
*inadequate fixation.
*slow
healing
in
intracapsular
fracture.
∆ Patients have increased pain and shortening
∆ X‐ray show persistent fracture line.
TREATMENT depends on the age of the patients
and the cause of non –union

A‐In young patients
1
‐If fracture is vertical and the head is alive,
then do subtrochantric osteotomy with nail or
plate fixation.
2
‐
If the reduction or fixation was faulty and
there are no signs of necrosis= remove the
screws, reduce the fracture and insert fresh
screws correctly with bone graft.
3
‐
If the head is a vascular, then prosthetic
replacement and if the joint is damaged , then
total hip replacement arthroplasty.

B‐In elderly patient
If patient fit = total hip replacement
arthroplasty.[THR]
If not fit and pain is not unbearable, then
conservative treatment [ raised heel, elbow
crutches ..]
3‐Osteoarthritis of the hip joint
= both a
vascular necrosis and collapse after several
years may lead to secondary osteoarthritis.
and needs THR.

Fractures of the proximal femur in children
*These fractures rarely occur in children , but
when they do ,they are potentially very
serious.
*They can occur due to high velocity truma,
pathological e.g. bone cyst or tumor and
possibility of child abuse.
Classification [
Delbet
classification].
1
‐
Fracture‐seperation of epiphysis
.
2
‐
Transcervical fracture of the femoral neck [
commonest type].
3
‐
Basal [ cervico‐trochantric ] fracture.
4
‐
Intertrochantric fracture.

*Diagnosis can be difficult, so ultrasonograghy,MRI,
and arthrograghy may be used.
Treatment
*Urgent treatment is required [within 24 hours ] of
injury.
*Hip is splinted and early aspiration of intracapsular
haematoma is advised to avoid epiphyseal
necrosis.
*Undisplaced fractures= plaster spica for 6‐8 weeks
*displaced type 4=closed reduction and spica, if
failed then operative fixation.
*Type 1,2,3 =treatment by closed reduction and
internal fixation, if failed then ORIF and then
spica for 6‐ 12 weeks.

Complications
1
‐Avascular necrosis of femoral head.
2
‐Coxa vara.
3
‐Diminished growth.
Intertrochantric fracture
*
It is an extracapsular fracture
.
Mechanism of injury =
*
Fall directly on greater
trochanter.
*
Indirect
twisting
injury
.
*
The crack runs up between the lesser and
greater
Trochanter
.
*
It can be stable or[ unstable if lesser
trochanteris is
Separated or medial cortex fragmented ]

Clinical features
= An elderly patient, with history of
truma,limb is short and externally rotated,
painful on movement and loss of function.
X‐ray =will show the fracture line.
Treatment
=This fracture has good blood supply
and can heal spontaneously by conservative way,
=traction in bed for 6‐8 weeks BUT because these
fractures usually occurs in elderly and due to
serious possible complications of prolonged bed
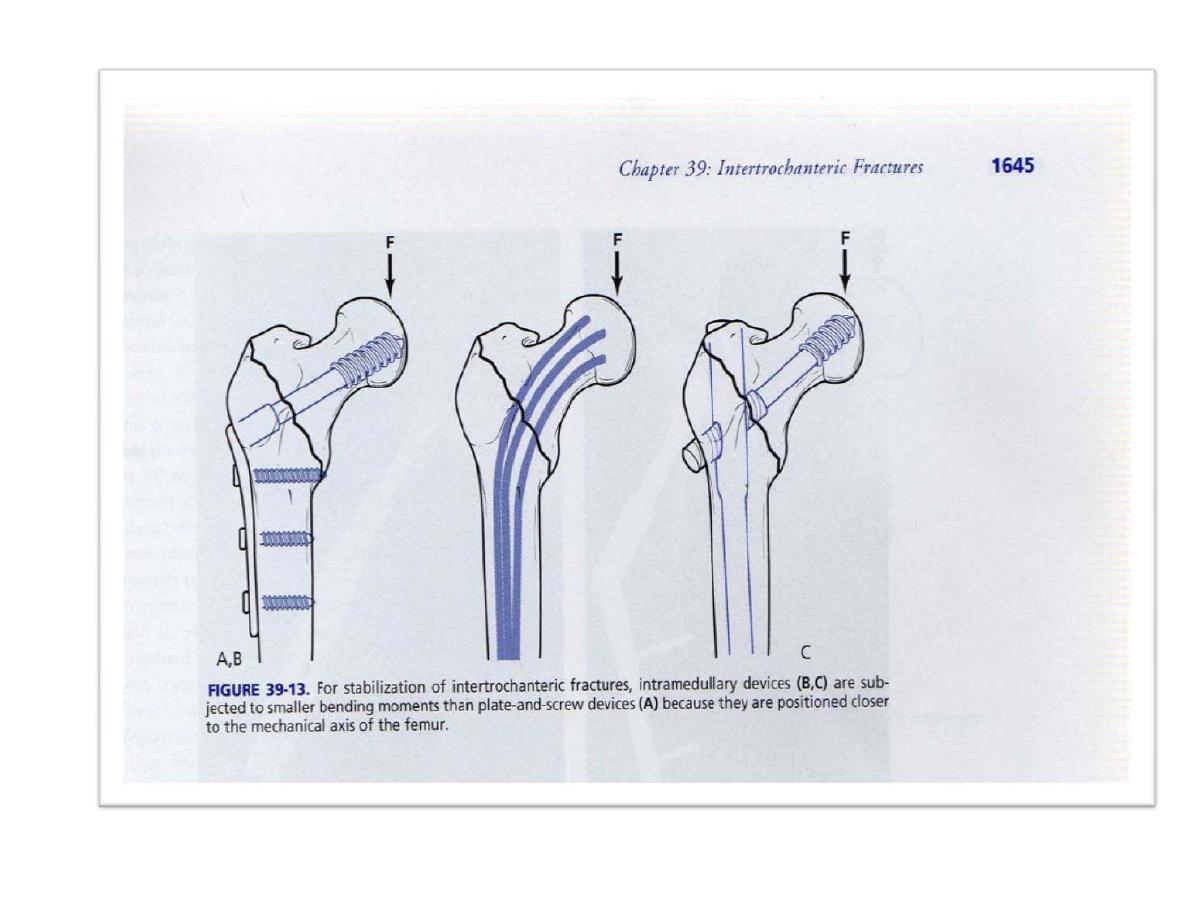
rest, these fractures usually treated surgically by
ORIF [dynamic hip screw or L –plate ].

Complications
General
=like those for fracture neck femur.
Local
=
1
‐malunion =in form of varus and
external rotation deformity of the limb.
Treated by subtrochantric corrective
osteotomy.
2
‐
delyed
union
and
non‐
union=uncommon and treated by ORIF
+bone graft.

Subtrochantric fracture of femur
*It occurs at or just below the level of the lesser
trochanter.
*It is associated with severe bleeding, and
sometimes hypovolemic shock.
Clinical features
=history of truma, painful,
tender, swollen limb with shortening and
external rotation and loss of function.
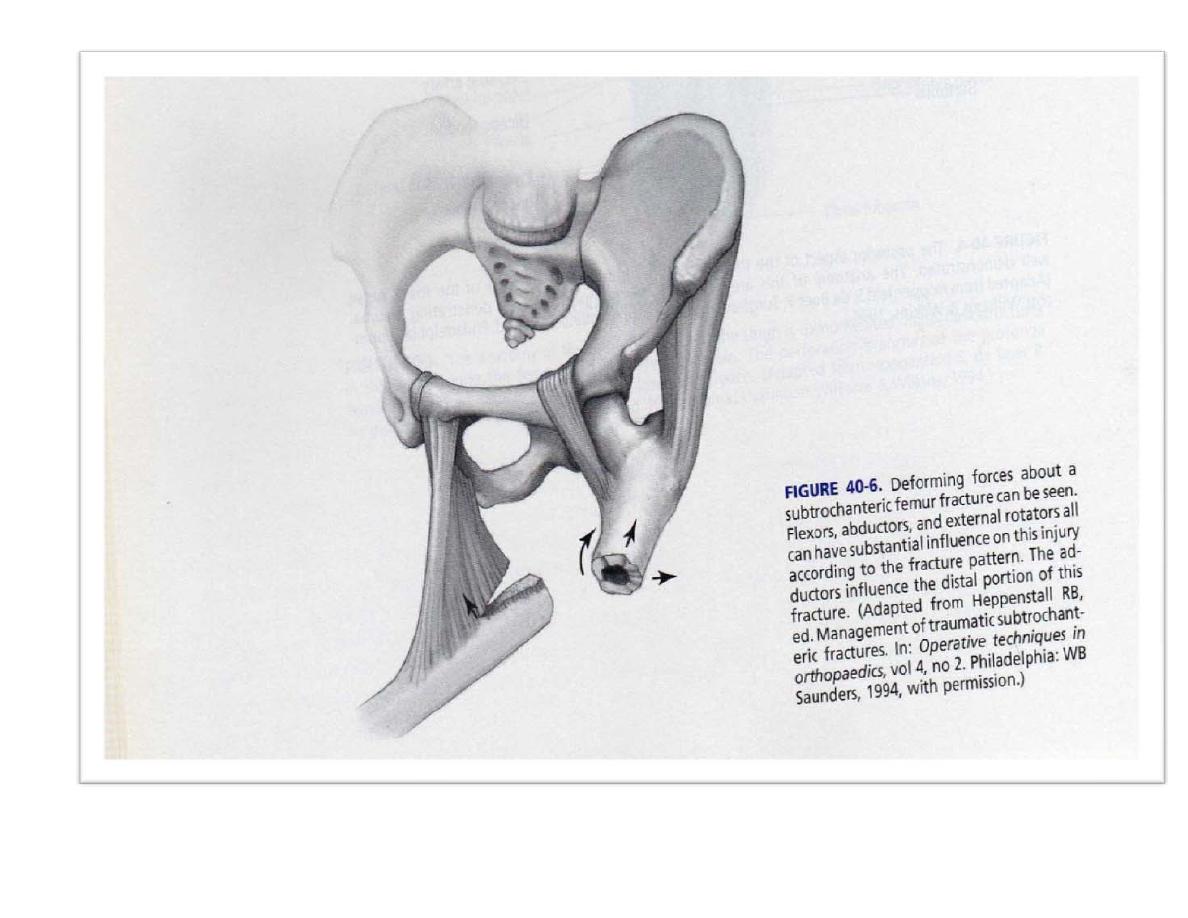
X‐ray
=the proximal fragment is flexed and
abducted by iliopsaos muscle,while distal
fragment is adducted and displaced upward by
adductors.

Treatment
= ORIF [ DHS or L –plate or locked
intramedullary nail ]
*If there is medial cortex loss, we should add
bone graft and gradually weight bearing.
*Conservative treatment may be used if severe
comminution or patient unfit.
Complications
=
General
=like those of fracture neck femur.
Local
= 1‐early= shock, fat embolism, associated
injuries to nerves and vessels.
2‐late= malunion, non‐union, delayed union.
THR
THR



