University of Al Qadisiyah / College of Pharmacy
Pharmacology – 4
th
Stage
By Dr. Bassim I. Mohammad, MBChB, MSc, Ph.D
Renal Pharmacology
• Diuretics
• Renal Vasodilators
• Urine PH manipulation
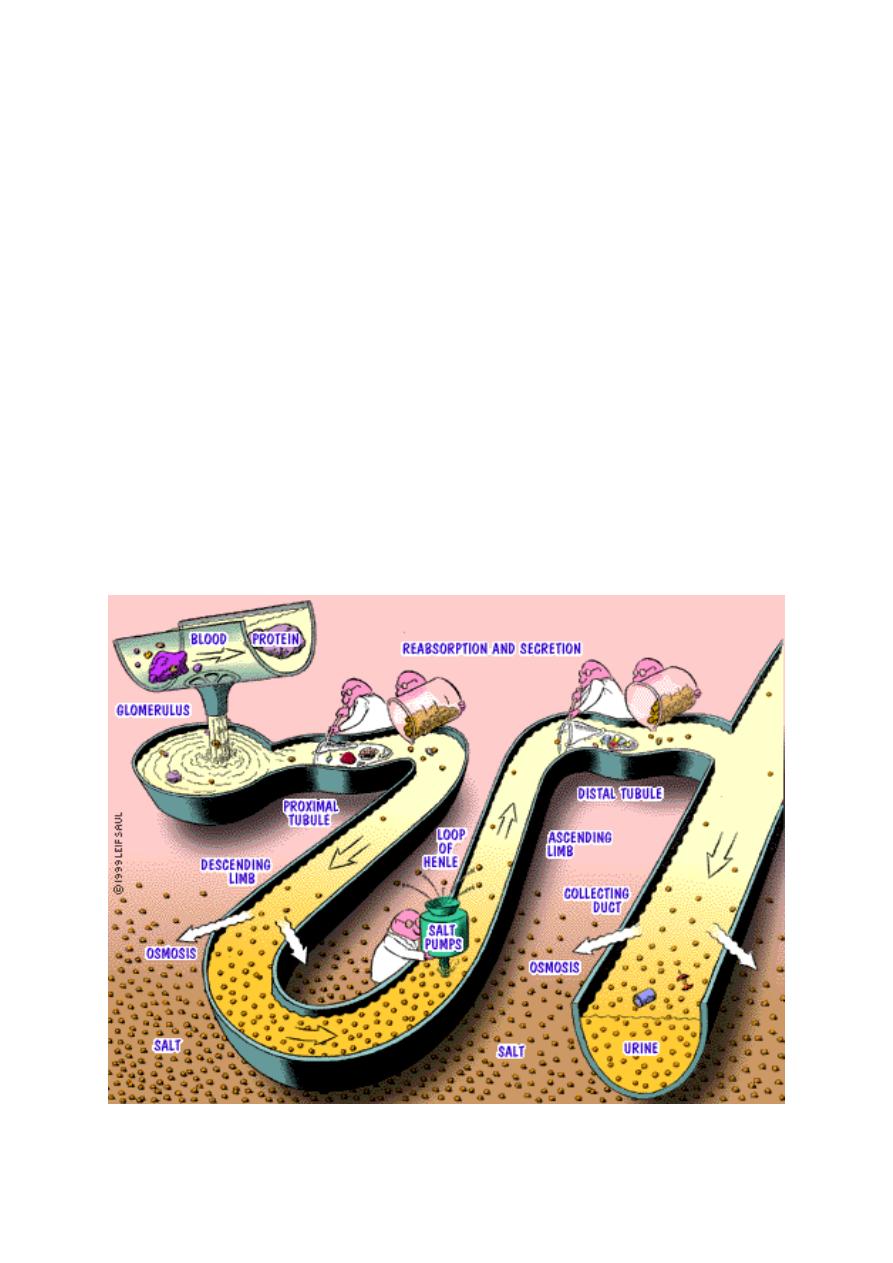
Renal Physiology:
• GFR is usually 200 L/day while urine output is approximately 1 L/day, so
99% of GFR is reabsorbed and 1% is excreted.
• Water follows Na
+
• NaCl is reabsorbed by active process while H2O absorbed passively.
Renal Pharmacology:
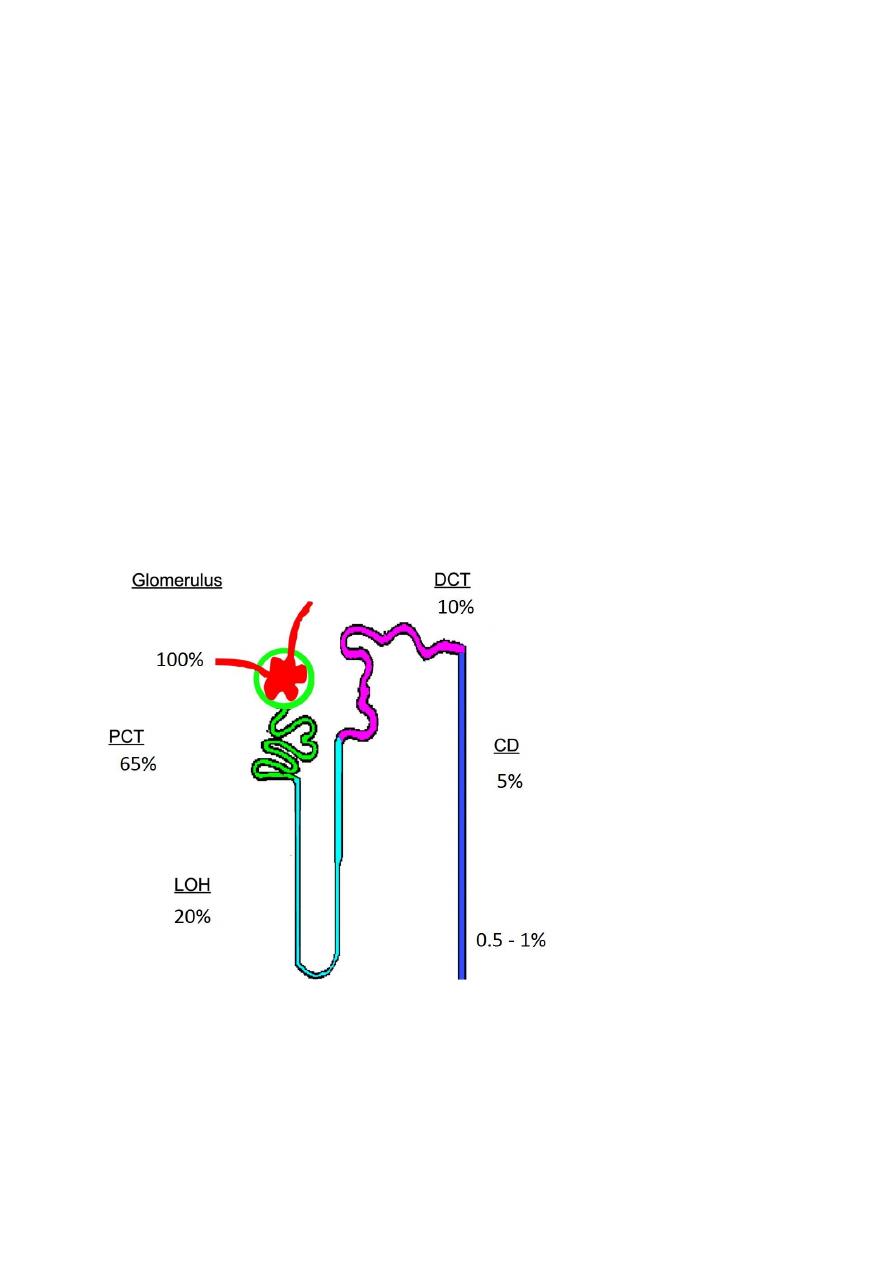
Normally sodium is reabsorbed:
• 65 % in PCT
• 20 % in Loop of Henle
• 10 % in DCT
• 5 % in CD
Diuretics:
Diuretics: are drug that increase urine flow/volume by causing sodium and
water excretion , by inhibiting sodium reabsorption in different sit in renal
tubules.
Mechanism of Diuresis
Two basic mechanism for inducing diuresis:
1. Extra renal mechanism
2. Renal mechanism
Diuresis - Extra renal mechanism
A. Inhibition of ADH release:
• Hypotension
• Alcohol intake
• Water depletion
B. Enhancing COP (in case of HF) by Digoxin or dopamine
A. Mobilizing peripheral edema fluids (hypoprotenimia) by using albumin
Diuresis - Renal mechanism
In this setting, diuretics are agents that alter physiological renal mechanism
that form urine in such away that there is increase in the flow of urine with
greater excretion of Na (Natriuresis)
Principles important for understanding effects of diuretics
• Interference with Na
+
reabsorption at one nephron site leads to
increased Na
+
reabsorption at other sites
• Increased flow and Na
+
delivery to distal nephron stimulates K
+
(and H
+
)
secretion
• Diuretics act only if Na
+
reaches their site of action. The magnitude of
the diuretic effect depends on the amount of Na
+
reaching that site
• Diuretic actions at different nephron sites can produce synergism
(Sequential Nephron Block)
• All, except k-sparing, act from the lumenal side of the tubular cellular
membrane
Classification of Diuretics:
They are classified according to the percentage of loss of sodium in urine into:
1. High efficacy (loop or high celling) diuretics
2. Medium efficacy diuretics
3. Low efficacy (Weak or adjuvant) diuretics
Loop Diuretics
this type of diuretics leads to excretion of 15-25% of filtered Na:
• Frusemide or furosomide
• Bumetanide
• Toresmide
• Ethecrynic acid
•
• Frusemide and Bumetanide have same efficacy while ethecrynic acid is
less efficcious.
• Bumetanide is 40 times more potent than furosemide.
LD- Mechanism of action
• Major site of action on thick Ascending loop of Henle (Inhibitors of Na+
K+ 2Cl Co-transport)
• Minor action on PCT (weak carbonic anhydrase activity).
• The site of action is reached (intraluminal) after the drugs has been
excreted by PCT.
• They act by inhibiting the reabsorption and so increasing the loss of
H2O, Na, Cl, K, Mg and H in the urine.
• These drugs are effective even when GFR are is <20 ml/min and this
mean that these drug are effective even in renal failure.
•
Blood volume =
preload
• Loop diuretics by venodilation reducing venous return to the heart with
the resultant decrease in pulmonary congestion.
• This explain the effectiveness of these drugs at subdiuretic dose in
relieving pulmonary congestion (in APO) and reducing BP before diuresis
• Additional non-tubular effects
1. Renal Vasodilation
2. Increase in renin release
3. Increase in venous capacitance (I.V) decrease LV filling pressure.
• These effects mediated by release of PGs from the kidney.
sulphonamides
Non- sulphonamides
Loop Diuretics – Pharmacokinetics
• Rapid GI absorption. Also given i.m. and i.v.
• Extensively protein bound in plasma
• Diuresis started within 10-20 minutes (1V) and one hour (oral).
• Short half-lives in general
• Elimination: unchanged in kidney or by conjugation in the liver and
secretion in bile.
Loop Diuretics – Clinical Uses
• EDEMA due to CHF, nephrotic syndrome or cirrhosis
• Acute heart failure with PULMONARY EDEMA
• HYPERCALCEMIA
• Forced diuresis
• Not in widespread use for the treatment of hypertension (except in a
few special cases e.g. hypertension in renal disease and hypertensive
emergencies)
Loop Diuretics – Side Effects
1. Sulphonamide Hypersensitivity: Ethecrynic acid is only non-sulph
diuretics and used in patient allergic to other diuretics.
2. Electrolytes and acid-base:
• Hypokalemia (so combine with K-sparing, ACEIs, ARBs)
• Hyponatremia
• Hypocalcemia (in contrast to thiazides)
• Metabolic alkalosis
3. Metabolic:
• Hypercholesterolemia
• Hyperuricemia (decreasing renal excretion – interference with tubular
secretion and reabsorption)
• Hyperglycemia (secondary to hypokalemia).
4. Dehydration and postural hypotension
5. Ototoxicity: could be transient with frusemide or permanent with EA
• Rapid IV bolus
• Ototoxic drugs (aminoglycoside, amphotericin-B)
• Renal impairment),.
6. Interstitial nephritis.
7. GI disturbance especially with EA.
8. Urine retention (elderly and nursing mother).

LD – Drug/Drug interactions
• With ototoxic drugs (like certain aminoglycoside, amphotericine-B….)
• Pobencid may interfere with effect of LD or thiazides by blocking their
secretion to PCT.
• NDAIDs decrease renal response to LD by interfering with formation of
vasodilator PGs
• High dose may competitively inhibits the excretion of salicylate, thus
precipitate to SA poisoning
• Steroids or ACTH may predispose to hyperglycemia.
• LD do not alter digoxin level nor interact with warfarin
Moderate Efficacy Diuretics
1. Thiazides:
• Hydrochlorthiazide
• Bendrofluzide
• Chlorthiazide
2. Thiazide-Related agents:
• Metazolone
• Indapamide
• Clopamide
• Chlorthalidone
TD- Mechanism of action
• Secreted into the tubular lumen by the organic acid transport
mechanisms in the proximal tubule
• Act on the distal tubule to inhibit sodium and chloride transport and
result in a modest diuresis
• These drugs inhibit the reabsorption of 10% of filtered Na
• They are not effective in low GFR (20ml/minute) except metolazone
which is useful even when GFR is low (moderate RF).
• Main site of action is DCT (early part) (Inhibitors of Na/Cl Co-transport),
More of Na is reached to the distal nephron more of Na is exchanged
with K+ and H+, increased urinary K+ and H+ excretion
• Secondary action on PCT (weak inhibitor of carbonic anhydrase, the
more potent thiazide the less CA inhibitor).

Indapamide- Beyond diuresis
• Vasodilator
• Class I and III antiarrthymic effect
TDs – Pharmacokinetics
• Rapid GI absorption
• Distribution in extracellular space
• Elimination unchanged in kidney
• Variable elimination kinetics and therefore variable half-lives of
elimination ranging from hours to days
Thiazide Diuretics – Clinical Uses
1. HYPERTENSION:
• Usually first line therapy
• Diuresis and reduction in PVR (decrease in response of resistance blood
vessels to circulation catecho. and this explains the effect of Indapamide
(as antihypertensive) at subdiuretic dose
1. EDEMA (cardiac, liver and renal)
2. IDIOPATHIC HYPERCALCIURIA (recurrent renal stone formation due to
excess calcium excretion)
3. DIABETES INSIPIDUS (Nephrogenic)
Thiazide Diuretics – Side Effects
1. Electrolytes and acid-base
• HYPOKALEMIA (and risk of arrhythmias): Therapeutic strategy is to avoid
hypoK in high risk patients (IHDs, HF on digoxin, HT with LVH) by K-
sparing diuretics (unless contraindicated renal impairmant) or cotherapy
with ARBs or ACEIs.
• HHYPOMAGNESEMIA
• HYPRECALCEMIA (in hyperparathyroidism)
• HYPONATREMIA
• METABOLIC ALKALOSIS
2. Metabolic:
• Hyperglycemia (more diabetogenic potential than LDs), especially
when combine with B-blockers. The risk depends on dose of thiazide and
type of b-blocker, Patients with family history of DM and metabolic
syndrome are more prone for DM (so avoid TD or start low dose.
• Hyperlipidemia so frequent check up of lipid profile is required to
minimize the atherogenic potential.
• Hyperuricemia (precipitation of gout, so they should be avoided patients
with Hx of gout)
3. Impotence; it is a big challenge and frequently cause drug withdrawal
and failure of therapy. So changing the drug or using sildenafile (unless
contraindicated like in nitrate) may help.
4. Hypersensitivity reactions: may manifest as interstitial nephritis,
pancreatitis, rashes, blood dyscrasias (all very rare)
5. Dehydration and postural hypotension
Thiazide vs. Loop Diuretics
1. Less potency
2. Different site of action
3. Low ceiling diuretics (max. response reached at relatively low dose).
4. Longer duration
5. Ineffective in low GFR (except metalozone)
6. More diabetogenic potential
7. Reduce Ca excretion
Diuretic Resistance
1. Compensatory Mechanisms (RAAS, SNS)
2. Failure to reach tubular site of action
a - Decreased G.I. absorption
b - Decreased secretion into tubular lumen
(e.g. uremia, decreased kidney perfusion)
c - Decreased availability in tubular lumen
(e.g. nephrotic syndrome)
3. Interference by other drugs (e.g. NSAID’s)
4. Tubular adaptation (chronic Loop diuretic use)
Can Use Combination of Diuretics to Induce a Synergistic Effect (SNB)
