Tumours of the Pharynx
Juvenile Nasopharyngeal AngiofibromaIs a vascular tumour of the nasopharynx occurring almost entirely in adolescent males (7-19 years with a mean of 14 years). The tumour has a tendency to regress after puberty. Although the tumour is benign, but it is locally invasive and behaves as malignant.
Aetiology
The exact aetiology is unknown but various theories have been postulated.
1. Hormonal theory based on that it is a tumour of males.
2. Remnants of embryonic tissue.
3. Hamartoma or paraganglioma.
Pathology
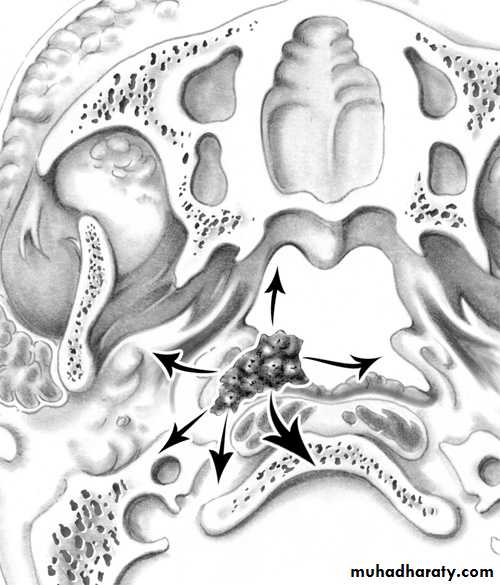
The tumour takes origin from the periosteum on the lateral wall of the nasopharynx close to the sphenopalatine foramen. Extension occurs:
1. Anteriorly to the nasal cavity and ethmoid.
2. Superiorly to the base of the skull.
3. Laterally to the pterygoid fossa, maxillary antrum and orbit.
Microscopically, the tumour consist of vascular spaces abounding in a stroma of fibrous tissue. The vascular spaces consist of thin-walled sinusoidal vessels unsupported by a muscular coat. This account for the severe bleeding as the vessels loose the ability to contract.
Clinical Picture
The patient is nearly always a young boy with a mean age of 14 years.
1. Repeated attacks of epistaxis which can be extremely profuse due to absence of muscular coat from the sinusoids.
2. Progressive nasal obstruction.
3. nasal speech (rhinolalia clausa).
4. Conductive deafness occurs from pressure on the Eustachian tubes.
Examination
1. Endoscopy and posterior rhinoscopy: smooth, rubbery lobulated mass in the nasopharynx.
2. Middle ear effusion.
3. Mass in the nasal cavity or on the cheek if the tumour has extended anteriorly or laterally.
4. Proptosis results from extension of the tumour to the orbit through the infraorbital fissure.
Investigation
1. Imaging: a. X-ray of the base of the skull and a lateral view of the skull.
b. CAT scan, MRI and MRA.
c. External carotid arteriography.
2. Biopsy is contraindicated because of fatal bleeding.
Differential Diagnosis
1. Antrochoanal polyp.2. Nasopharyngeal carcinoma.
Treatment
1. Surgical excision Haemorrhage is the main danger of operation, so adequate blood should be prepared before the operation.
2. Embolization is indicated preoperatively to control the vascularity of the tumour.
3. Radiotherapy should be reserved for patients with inoperable intracranial extension and recurrent tumours.
Nasopharyngeal Carcinoma
This tumour is common in south east Asia especially in China.
Aetiology
Is exactly unknown
Viral :Epestain-Barr virus has been suggested as a cause, but the exact role is unknown.
Genetics: Chinese have a high genetic susceptibility. Chinese population who move to western countries retain a high incidence suggesting a genetic predisposition.
Environmental factors: common in southern China.
a. Ingestion of salted fish.
b. Indoor cooking in homes without Chimneys.
Pathology
Most tumours arise from the fossa of Rosenmuller. Virtually all malignant tumours of nasopharynx are squamous cell carcinomas. In endemic areas undifferentiated carcinoma is the most common histological type.
Spread of Nasopharyngeal Carcinoma
Direct, lymphatic (cervical L.N.) and blood borne (rare)
Anteriorly into the nasal cavity and paranasal sinuses leading to nasal symptoms.
Posteriorly to the retropharyngeal space and lymphnodes of Rouviere.
Laterally into the parapharyngeal space involving the last 4 cranial nerves.
Superiorly through the the base of skull involving the optic nerve and the cavernous sinus.
Inferiorly to the oral cavity and retrotonsillar region.
Clinical Picture
Bi-modal age distribution with the first age peak at 2nd decade and the other peak at 5th – 7th decade of life. It affects males more than females.Cervical lymphadenopathy: is often the presenting feature which may be unilateral or bilateral.
Nasorespiratory symptoms: nasal obstruction, nasal speech and epistaxis.
Tinnitus and aural symptoms due to Eustachian tube obstruction. This may proceed to secretory otitis media.
Neurological symptoms: the most frequently involved nerves are V, VI, IX and X. The latter 2 nerves paralysis lead to immobility of the soft palate. Involvement of the sympathetic chain results in Horner,s syndrome.
5. Pain and headache due to intracranial extension or sphenoidal sinusitis.
Examination
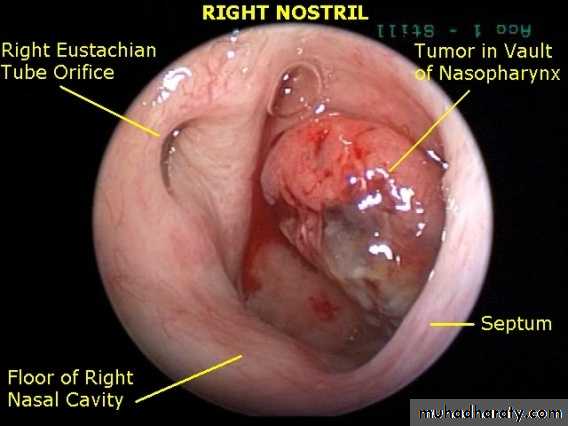
1. Endoscopy and posterior rhinoscopy. A large exophytic tumour may be seen.
2. The palate is pushed downward and paralyzed.
3. The neck should be palpated for metastatic lymphnodes.
4. Middle ear effusion.
5. Parapharyngeal spread can cause trismus.
Endoscopic view of NPC Extra-ocular muscle paralysis
Investigation
1. Imaging:
a. X-ray of the base of the skull---- bony destruction involving the petrous bone, foramen lacerum and carotid canal.
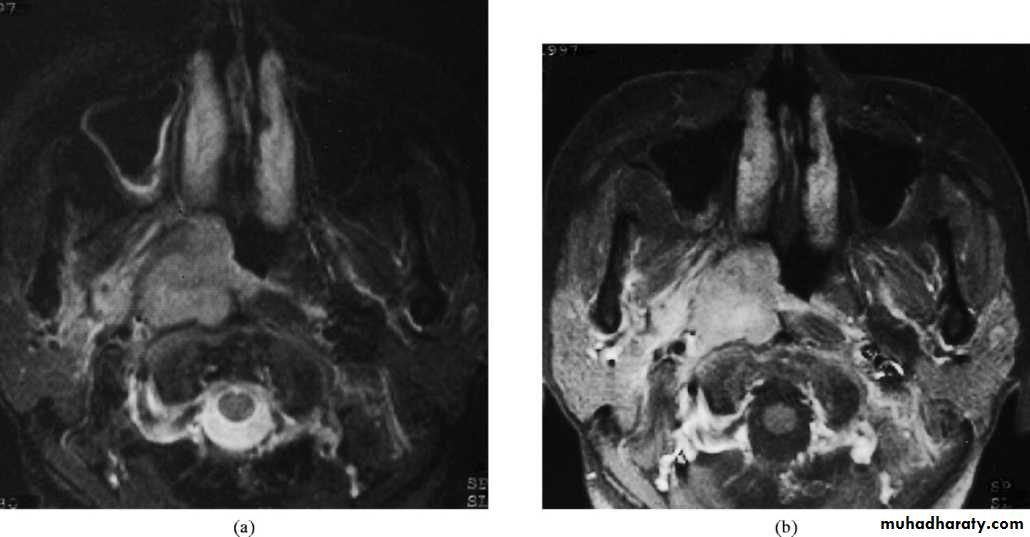
b. CT scan and MRI: MRI is superior to CT scan in finding soft tissue involvement.
2. Biopsy under G.A
Treatment
1. Radiotherapy is the treatment of choice because surgical removal of the primary growth is rarely possible.2. Chemotherapy as an adjuvant to radiotherapy is of contraverse.
3. Surgery in form of radical neck dissection is reserved for patients with persistent or recurrent neck disease following radiotherapy.
Nasopharynx
Benign: Angiofibroma (Most common)Papilloma
Haemangioma
Craniopharyngioma
Malignant: Nasopharyngeal carcinoma
Adenocarcinoma
Fibrosarcoma
Rabdomyosarcoma
Oropharynx
Benign: Papilloma
Malignant: Epithelial: squamous cell cacrcinoma
Lymphoma: Hodgkin's and non- Hodgkin's
Salivary gland: Adenocystic carcinoma
Hypopharynx
Benign: Fibrolipoma and leiomyoma
Malignant: Squamous cell carcinoma (pyriform fossa, postcricoid and
posterior pharyngeal wall).