
1
Lectures In community
Medicine
(LEC1,2,3)
4th Stage
BY:
DR Zaid
October 2015
2
4th stage
طب مجتمع
Lec-1
د.زيد
26/10/2015
Food born diseases
Terms applied to illnesses acquired by consumption of contaminated
food.
( food born intoxicant &food born infections )
1.Illness caused by toxicants elaborated by bacterial growth before
consumption :
(Staphylococcus aureus & bacillus cereus)
2. toxins elaborated in intestine
(Clostridium perfringens)
3.Illness caused by bacterial infection with short incubation period
( salmonelosis )
Food born disease outbreak :
Occurrence of illness within usually short but variable period of time
among individuals who have consumed certain foods in common.
Staphylococcus food intoxication
An intoxication not infection
Abrupt onset
Severe nausea , vomiting , cramps , often accompanied by
diarrhea
Some time subnormal blood pressure & temp.
Self limiting disease ,death are rare
Most people are susceptible
3
Dx :
1. Clinical features ,history &incubation period
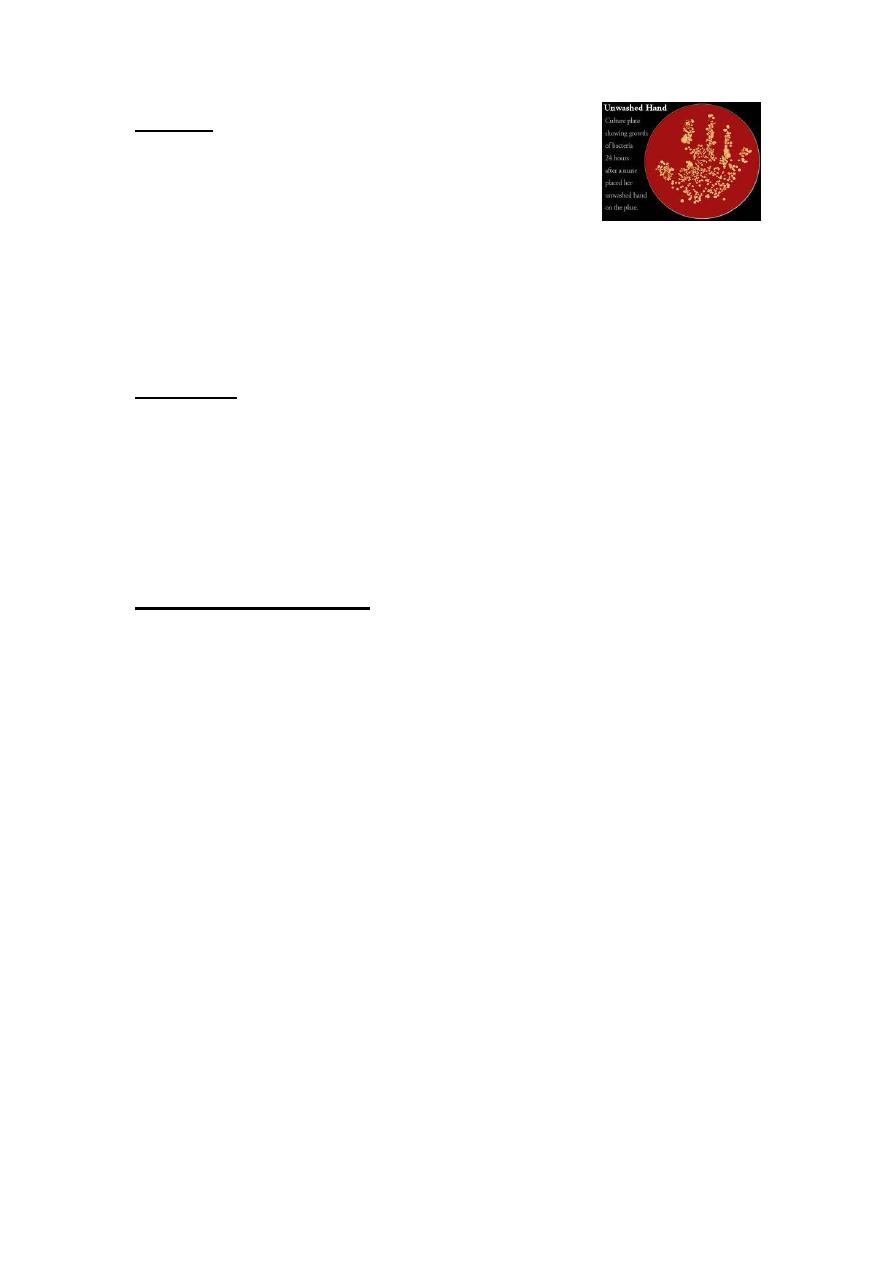
2. In an outbreak recovery of large no. Of staphylococcus on routine
culture media or detection of enterotoxin from an
epidemiologically implicated food confirms the DX
*Absence of staph. On culture of heated food does not rule out the DX
Incubation period:
½ - 8 hours , usually 2-4 hours
Toxic agent: several enterotoxins of staph aureus
Coagulase +ve stable at boiling temp
Reservoir : humans in most instances occasionally cows as well as dogs
.
Mode of transmission:
foods involved are particularly those that come in contact with food
handlers hands either without subsequent cooking or with inadequate
heating or refrigeration:
Source :
(human)…Purulent discharges of an infected finger ,eye ,abscesses,
naso-pharyngeal secretions or apparently normal skin
(bovine)…contaminated milk or milk products

4
Prevention:
1.Education of food handlers in
Strict food hygiene
Sanitation &cleanliness of kitchens
Proper temp. control
Hand washing
2. Reduction of food handling time (initial preparation to service) to an
absolute minimum
3. Temporarily exclude people with boils, abscesses or other purulent
lesions of hands, face or nose from food handling
Salmonellosis:
It is bacterial disease commonly manifested by an acute
enterocolitis
Sudden onset of headache , abdominal pain ,diarrhea ,nausea &
some times vomiting
Dehydration may be severe especially among infants &elderly
Fever is almost always present
Anorexia &diarrhea often persist for several days
Septicemia or focal infection may develop
Deaths are uncommon except in every young ,very old ,debilitated
&immunosuperessed
5
Infectious agent:
About 2000 serotype :
salmonella typhimuruim & S. enteriditis are the most commonly
reported
Occurrence :
World wide
Incidence of infection is highest in infants &young children
It may occur is small outbreaks
About 60-80% of all cases are sporadic
Reservoir :
1.Wide range of domestic &wild animals:
Poultry, ,cattle ,rodents, dogs, cats
2.Human i.e patient ,convalescent carriers & mild unrecognized cases
3.Chronic carriers are rare in humans but prevalent in animals &birds
Mode of transmission :
By ingestion of organisms in the food derived from infected
animals or contaminated by stool of infected animal or
person
Raw or undercooked eggs &egg products
Raw milk &milk products
Contaminated water
Meat &meat products
Poultry &poultry products
6
Incubation period
From 6-72 hrs , usually about 12-36hrs
Period of communicability
Throughout the course of illness
From several days to several weeks
Prevention
1.Education of food handlers the :
a. hand washing
b. Refrigeration
c. Thoroughly cooking of food of animal origin
d. Maintain sanitary kitchen
2.Educate the public to avoid consuming raw or incompletely cooked
eggs
3.Exclude individuals with diarrhea from food handling
4.Educate the known carriers on the need for very careful hygiene
&hand washing after defecation &prior to food handling
5.Adequately cook or heat-treat animal derived food prepared for
consumption to eliminate pathogens
7
Control:
1.Reporting
2.Isolation
a. Wearing gloves and gowns during handling of feces &contaminated
bed linen in hospitalized patients
b. Exclude patients from food handling
c. Release to return to work requires 2 consecutive negative stool
culture for salmonella collated not less than 24 hours apart
Note: if antibiotic have been given the initial culture should be taken at
least 48 hrs after the last dose
3. Disinfection
4. Investigation of contacts
5. Specific Rx :uncomplicated :none except rehydration
Antibiotics of choice:
(Ciprofloxacine, Ampicillin, Amoxicillin, TMP-SMX, Chloramphenicol )
Botulism
:
There are 3 types of botulism
1.Food born (the classic type)
2.Wound
3.Infant
The site of the production of the toxin is different for each type ,but all
shares in common the flaccid paralysis that results from botulism
neurotoxin
8
DX:
Demonstration of botulinum toxin in:
Serum , stool, gastric levage , and incriminated food
Culture of C. botulinum from:
gastric aspirate , stool, of clinical case
Infectious agent:
Food born…… toxin (heat labile) produced by C. botulinum
Toxin is produced in:
Improperly processed ,canned, low acid or alkaline food
Unpasteurized foods held without refrigeration especially in
airtight packaging
(Toxin is destroyed by boiling)
Reservoir
Spores are present in soil world wide
Incubation period:
Food born… 12-36 hrs .
some times several days
the shorter the incubation period the more severe the disease
&the higher the CFR

9
Prevention:
1-Ensure effective control of processing of commercially canned and
preserved food
2-Education of those concerned with home canning regarding the:
• Proper time, pressure, &temp. required to destroy spores
• Effectiveness of boiling home canned vegetables for at least (10)
minutes to destroy the toxin
3- Bulging containers should not be opened &foods with off-odors
should not be eaten or even tested
4-Identified source such as honey ,should not be fed to infants
Control
1. Reporting
2. Isolation :not required
3. The implicated food should be detoxified by boiling before
discarding
4. Containers &utensils should be sterilized by boiling or chlorine
disinfectant
5. Sanitary disposal of stool of infants cases
11
4th stage
طب مجتمع
Lec-2
د.زيد
26/10/2015
Nosocomial infection
) Hospital acquired infections)
An infection occurring to a patient in hospital or other health care facility
in whom it was not present or incubating at the time of admission or the
residual of an infection acquired during a previous admission .
Descriptive epidemiology
Agent host
Environment
Diagnostic procedures , medical or surgical therapy ..it can
cause.. infection
Potent immunosuppressive ,chemotherapeutic agents
&antibiotics affect normal flora
Exposure to persons who are infected or carriers can transmit inf.
(health workers or patients)
Infection rate differ considerably among hospitals
• Referral hospitals generally have higher rate than community
hospitals:
(More complex patient mix &more aggressive modes of therapy used)
11
Prevention (general outbreaks):
• Investigation of reservoir &mode of transmission
• Appropriate use of diagnostic procedures ,invasive
devices &medical therapy particularly antibiotics
• Hospital environment may be modified
• Strategies to proper use of isolation materials hand washing
,&other effective approaches to prevent transmission .
Main categories of Nosocomial infection :
1.Urinary Tract Infection:
IT accounts 1/3 of NI
80% of NUTIs caused by urinary catheters
The typical UTIs prolongs hospital stay
The prevalence of bacteruria during a short term use of catheter
is: approximately 15% compared with a prevalence of 90% in
along term use
Risk factor for bacteruria:
Duration of catheterization
Micro bacterial colonization of the drainage bag
No antibiotic use
Female gender
Diabetes mellitus
Abnormal serum creatinine
Errors in catheter care
12
Prevention
a. Prevention of catheterization by the use of alternative approach
Patient training
Medication
Surgery
Use of special clothes &bags
Intermittent catheterization
Use of external collection &urinary diversion
b. Prevention of bacteruria once catheterized
recommended minimizing the duration
closed drainage system
Good hand washing after caring each patient is the
single measure most –likely to prevent cross-transmission of urinary
pathogens
2.Lower respiratory infection (LRI) &pneumonia
It accounts >13% of NIs
CFR 20-50%
N pneumonia associated with an excess length of stay of >/one
week
Most of NLRI occur in ICU &surgery recovery units
13
Predisposing factors
Endotracheal intubations
Tracheostomy
(lead to decrease LRT defense mechanisms ..drying and direct rout of
entry)
Ventilator
Contaminated aerosols
Other contaminated equipment
Chronic lung diseases
Advanced age
prior administration of antibiotics
Immunosuppression.
Prevention
• General hygienic measures
• Use of barrier isolation materials
• Routine decontamination of respiratory equipments
• Using gloves ,gowns &masks
• Annual influenza immunization of pts &hospital staff
3.Surgical wound infections (SWIs)
• sWIs are now the 2
nd
most common NI accounting for at least 17%
• Infection rate varies according to:
• operative site
• patient co morbidity
14
Sources :
Inoculation from pt’s residual flora
Contaminated host tissues
Surgical team members hands at the time of surgery
Airborne contamination at the time of surgery
Post operative drains or catheters
Prevention:
Disinfection of the skin at the incision site
Appropriate use of preoperative antibiotics when indicated
Perioperative antibiotics started immediately before surgery
&continued for up to 24 hrs after are effective
4.Nosocomial Diarrhea:
A common problem
Risk factors
1. Older age
2. sever underlying disease
3. Hospitalization of more than one week
4. Long stay in the ICU
5. Prior antibiotic treatment.
15
5.Blood stream infection (BSIs)
Account for 14% of NIs
Source:
1-IV catheters , intrinsic IV fluid contamination ,multi dose parenteral IV
medications
2-Contamination of antiseptics
3-Contamination of hands of health workers
4-External colonization of the catheter
16
4th stage
طب مجتمع
Lec-3
د.زيد
26/10/2015
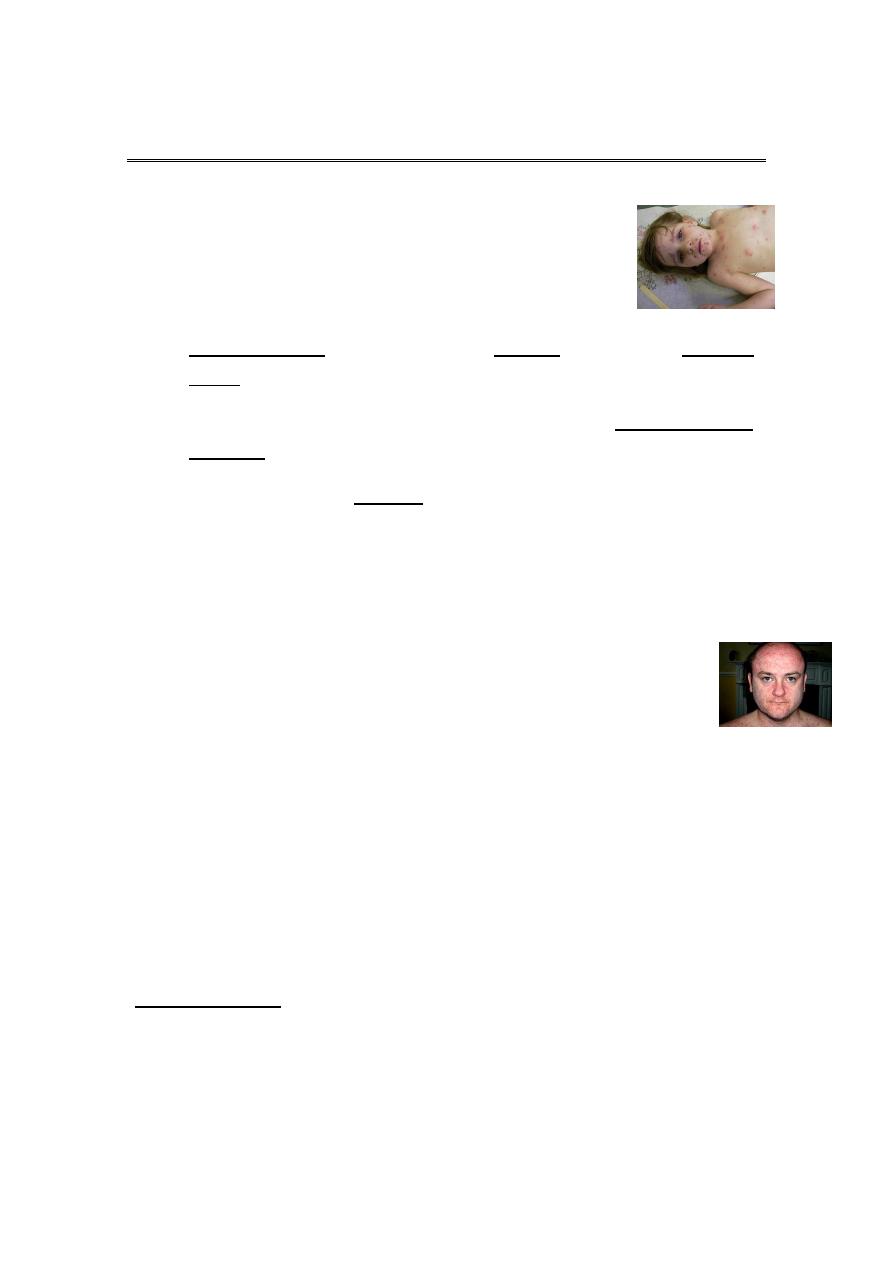
Chicken pox
• Acute generalized viral disease characterized by:
Sudden onset of fever, mild constitutional
symptoms, &skin rash
Maculo-papular rash.. few hours.. vesicles…. 3-4days.. granular
crusts
Lesion commonly occur in successive groups with several stage of
maturity present at the same time.
More abundant on covered than exposed parts of the body
Lesions may appear high in the axilla &on the scalp ,MM of the
mouth and R.T., &on the conjunctivae
Sever form can occur in adults.
Children with acute leukemia are at high risk of severe
disseminated form with CFR of 5-10 %
Neonates (5-10days)have a CFR of up to 30%
Infection early in pregnancy may be associated with (CVS) in 0.7 %
&if infection occurs at 13-20 weeks in may be associated with CVS
in 2%
Herpes zoster is a local manifestation or reactivation of varicella
infection in dorsal root ganglia.
Infectious agent:
Human (alpha) herpes virus 3
(V-Z virus)
17
Occurrence:
World wide, in temperate climates at least 90% of the population
has had chicken pox by the age of 15 years &at least 95% by young
adulthood.
Reservoir : Human
Mode of transmission:
Direct contact person-to –person
* Droplet
* airborne spread
vesicle fluid or secretion of the URT of chicken pox case or vesicle fluid
of patient with HZ can transmit infection.
Indirect
* Soiled articles
Scabs are not infectious
Incubation period:
2-3 weeks , commonly 14-16 days
Period of communicability:1-2 days before the Rash and 5 days after.
Susceptibility &resistance:
general
More sever from occur among adults
Infection gives life long immunity
Second attacks are rare
18
Prevention:
1. Live attenuated Variclla vaccine (Varivax). A single dose of 0.5 ml
sc is recommended for children age 12m-12 yrs who have not had
chicken pox . This vaccine had cumulative efficacy at 70-90 % in
preventing varicella in children. It is protective if it is given within
3 days of exposure
2. Protect high risk individuals from exposure
3. VZIG is effective in preventing or modifying the disease .if given
within 96 hours of exposure
Control :
1. Reporting is not necessary
2. Isolation :Exclude children from school for 5 days after
appearance of rash
3. Disinfection of articles soiled by discharge from nose & throat
4. Protection of contacts
Acyclovir week of exposure 80mg/kg/day/qds
5. Specific Rx :
Antiviral drag
Zovirax( Acyclovir), Vidarabine
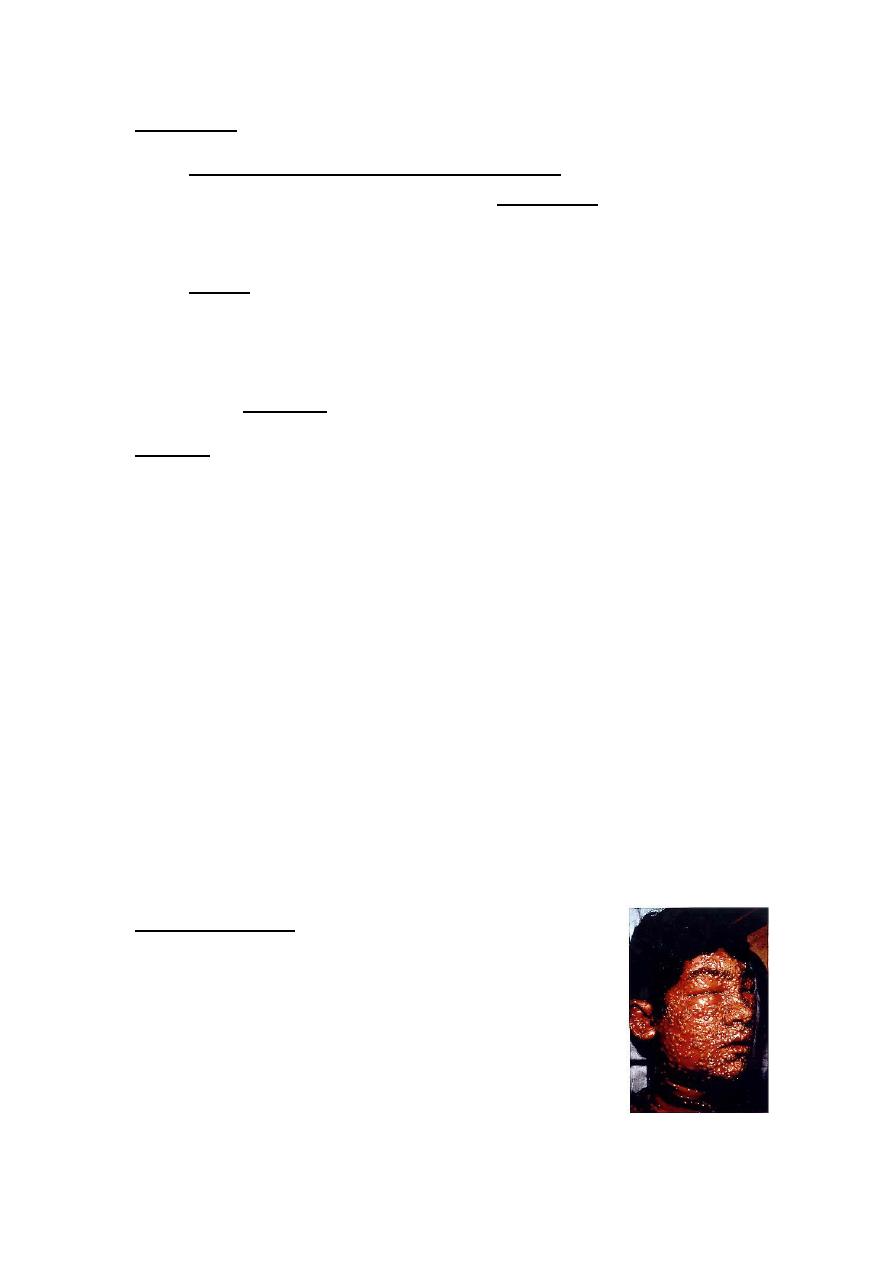
Smallpox (Variola)
Last naturally acquired case in word occur in
October 1977 in Somalai
Global eradication was certified two years later
by WHO
It is systemic viral disease
19
Then Fever began to fall deep seated rash developing in which
individual lesions containing infectious virus -
>
macules->
papules -> vesicles-> pustules -> crusted scrabs
Which fell off after 3-4 weeks
Appeared on the successive stages of maturity
Abundant on the exposed parts (centrifugal distribution).
In the previously vaccinated the rash stage was significantly
modified.
Infectious agent:
Variola virus a species of orthopox virus.
Occurrence :
Formerly a world wide disease. it is eradicated.
Reservoir :
Naturally human, officially, only in designated freezers.
Mode of transmission :
Air borne
Secondary attack rate among unvaccinated population was about 50%.
Incubation period:
7 to 19days
Communicability From the first day of the development of the earliest
lesion to the disappearance of all scabs (about 3 weeks).

21
Susceptibility & resistance:
Among unvaccinated is universal.
Method of control:
Immunization with vaccinia virus vaccine.
Mumps (Infectious parotistis):
• An acute viral disease characterized by: Fever, swelling
&tenderness of one or more salivary glands (usually the parotid
&some times the sublingual or sub maxillary glands).
Complications:
Orchitis, most commonly unilateral (20-30%) of post pubertal
males
OOpheritis and or mastitis can occur in females >15 years of age
Sterility is extremely rare
Sensoneural hearing loss in children(5:100.000 cases).
Encephalitis (1-2 :10,000 cases)
Pancereatitis usually mild (4% of cases )
Infectious agent:
Mumps virus: a member of the Paramyxoviradae

21
Occurrence:
Less regularly recognized than other common communicable
childhood diseases
1/3 of the exposed susceptible may have inapparent infection
By the use of effective vaccination program (MMR) the incidence
has dramatically decline &the greater risk of infection has shifted
toward older children, adolescence &young adults
Susceptibility &resistance:
Immunity is life long after clinical or inapparent infection
Inapparent infection is communicable
22
Prevention:
1. Public education
2. Vaccination (Jerky Lynn strain) live attenuated vaccine (MMR).
more than 95%develop long-lasting or probably life long
immunity. Administered at any time after 12 months .
3. Special efforts to vaccinate before puberty all persons with no
definite history of mumps or mumps immunization.
Contra-indication of the vaccine:
Immune suppression.
Pregnancy &planning of pregnancy in the next 3 months
Control:
1. Reporting: It is reportable disease.
2. Isolation: respiratory isolation &private room for
9 days from onset of swelling. Also school
exclusion for the same period
3. Disinfection of all articles soiled with throat secretion.
4. Protection of contact
* Active not effective
* Passive not effective
5. No specific Rx.
