1
Fifth stage
E.N.T
Lec-1
د.باسل
4/10/2015
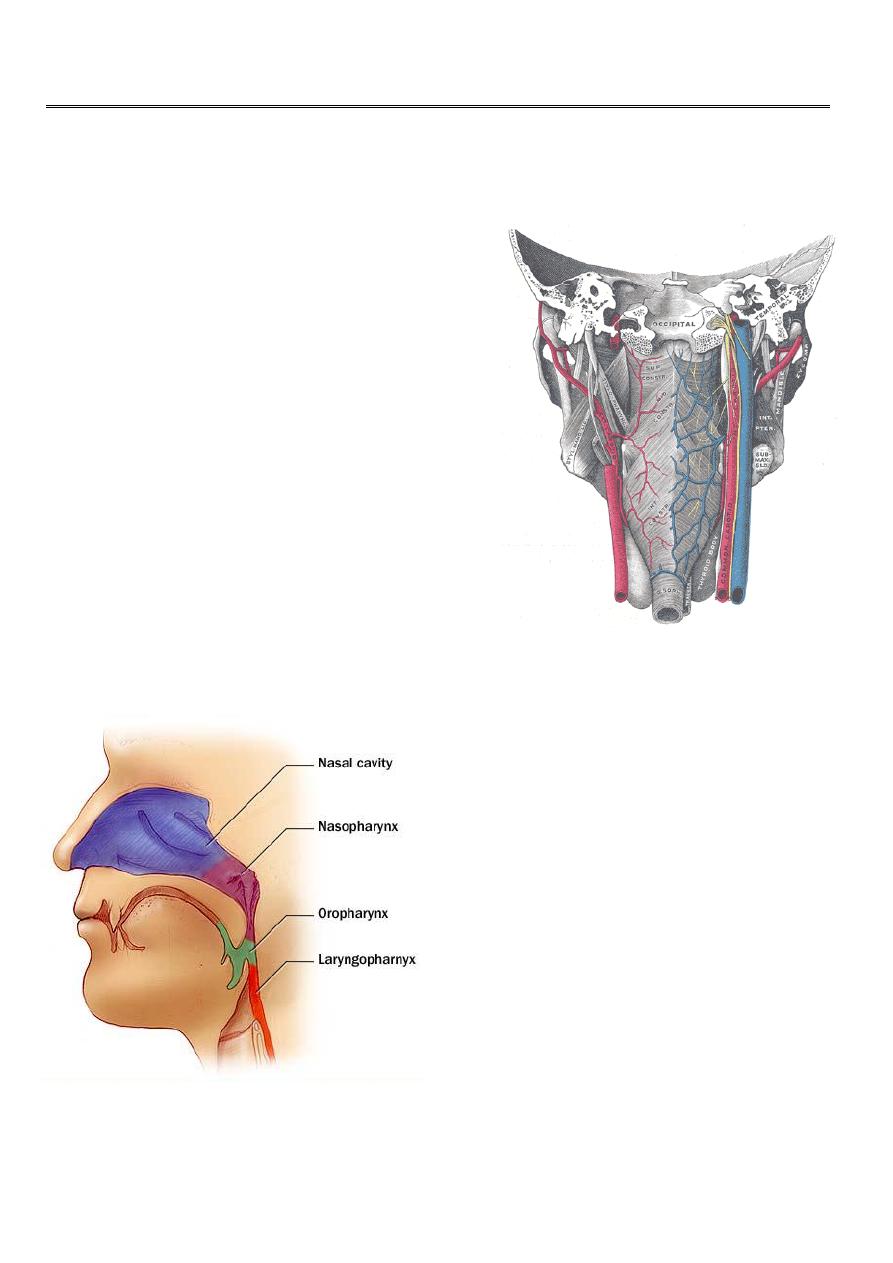
PHARYNX
Pharynx :
Is a funnel-shaped fibromuscular tube,
10-12 cm in length in adults.
Extends from the base of the skull to the level of
C6.
The pharynx is divided
anatomically into 3 parts;
Nasopharynx
Oropharynx
Laryngopharynx
(( Hypopharynx))
Behind :
The Nose
The Mouth
The larynx
2
Nasopharynx
Oropharynx
Laryngopharynx
(Hypopharynx)
Nasopharynx(( Postnasal Space))
This extends from the base of the skull to the hard palate.
At the junction of the roof and posterior wall lies a small mass of lymphoid tissue
called adenoids (nasopharyngeal tonsil).
On the lateral wall, there are the openings
of the Eustachian tubes.
Behind which are hollows called the fossa
of Rosenmuller, which is the site of
nasopharyngeal malignancy
Communicates inferiorly with the
oropharynx through the velo-pharyngeal
sphincter
Oropharynx
Extends from the level of hard palate to the level of hyoid bone and opens anteriorly
into the oral cavity. Behind the oral cavity (in front of 2
nd
&3
rd
Cervical vertebra)
The palatine tonsils are situated in it's lateral wall
Between the ant. and post tonsillar pillars.
From the soft palate superiorly to tip of epiglottis inferiorly Communicates:
Anteriorly with the oral cavity Superiorly with the nasopharynx
Inferiorly with the hypopharynx
3
Hypopharynx
Behind the Larynx (in front of 3
rd
to 6th Cervical
vertebra) From the tip of epiglottis
superiorly to the lower border
of cricoid cartilage inferiorly
Communicates:
-
Anteriorly with the Larynx
-
Superiorly with the oropharynx
-
Inferiorly with the esophagus
The hypopharynx does not only
lie behind the larynx BUT also
Projects laterally on each side of the larynx and is formed of :
-
Postcricoid region
( behind the larynx)
-
Two pyriform fossae
(on each side of the larynx
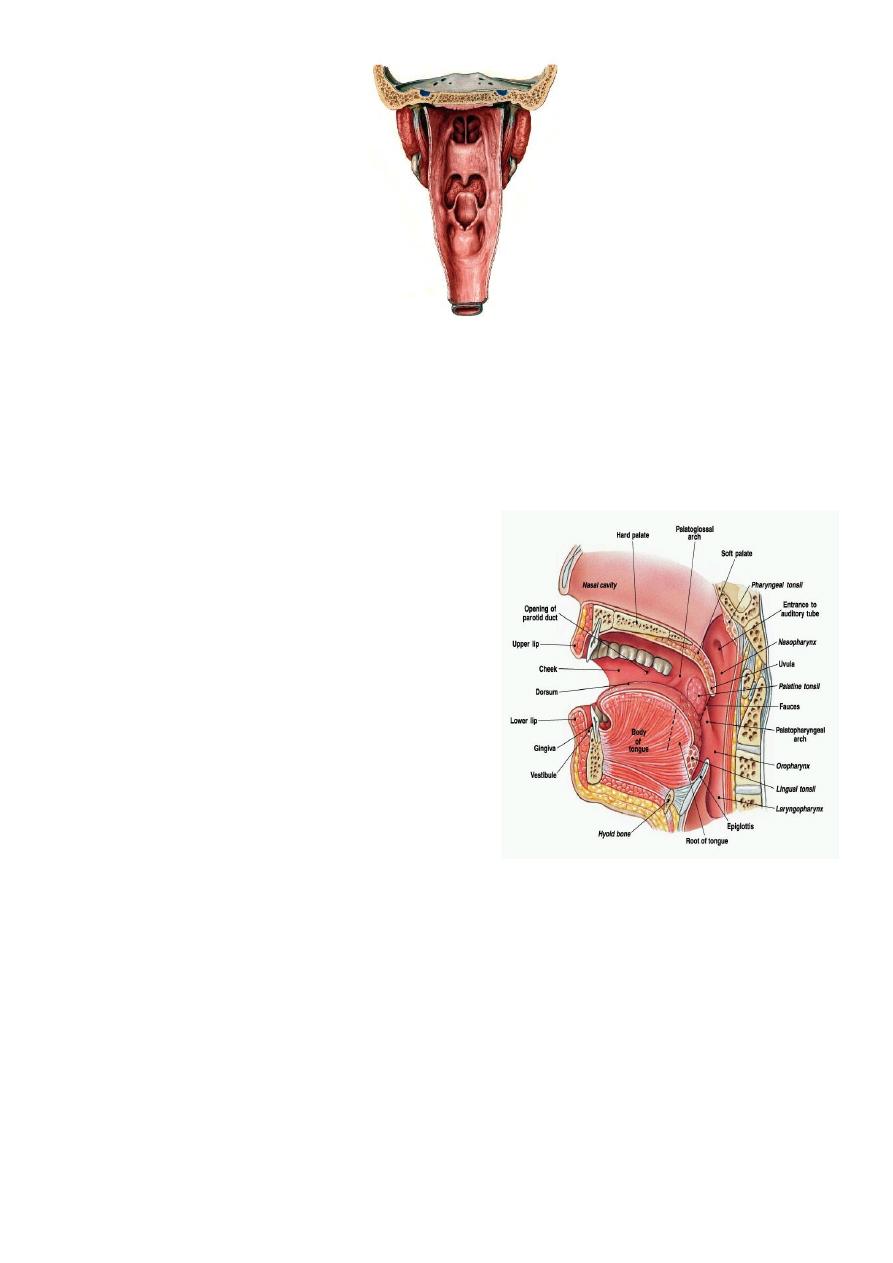
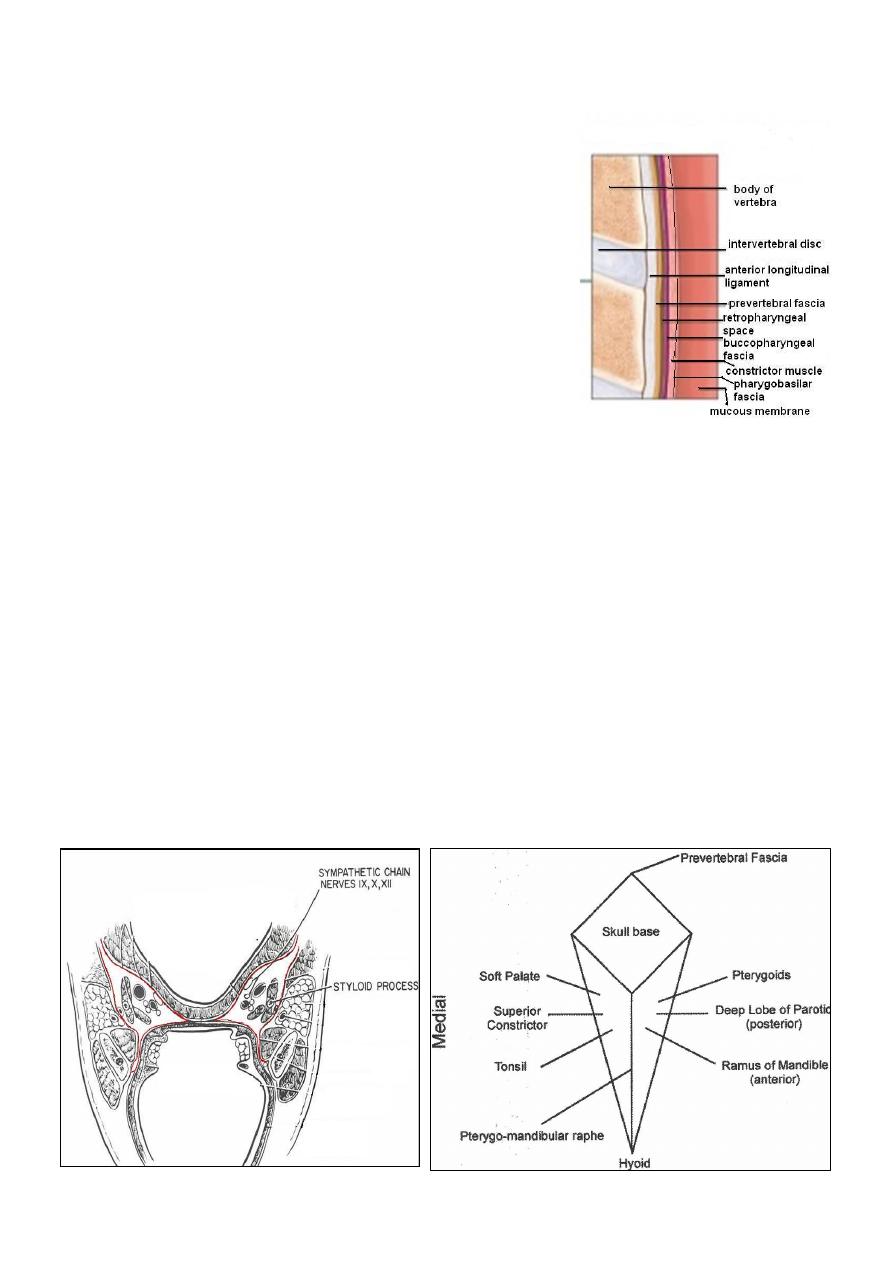
Pharyngeal Wall Histology
4
Wall Histology
The pharyngeal wall consists of 4 layers:
1. Mucous membrane.
2. Pharyngobasilar fascia.
3. Muscle layer.
4. Buccopharyngeal fascia.
1- Mucus Membrane
The lining epithelium is stratified squamous except in the nasopharynx, where
columnar epithelium is found.
2- Pharyngobasilar fascia
This fascia is strengthened posteriorly by a strong band called the median raphae.
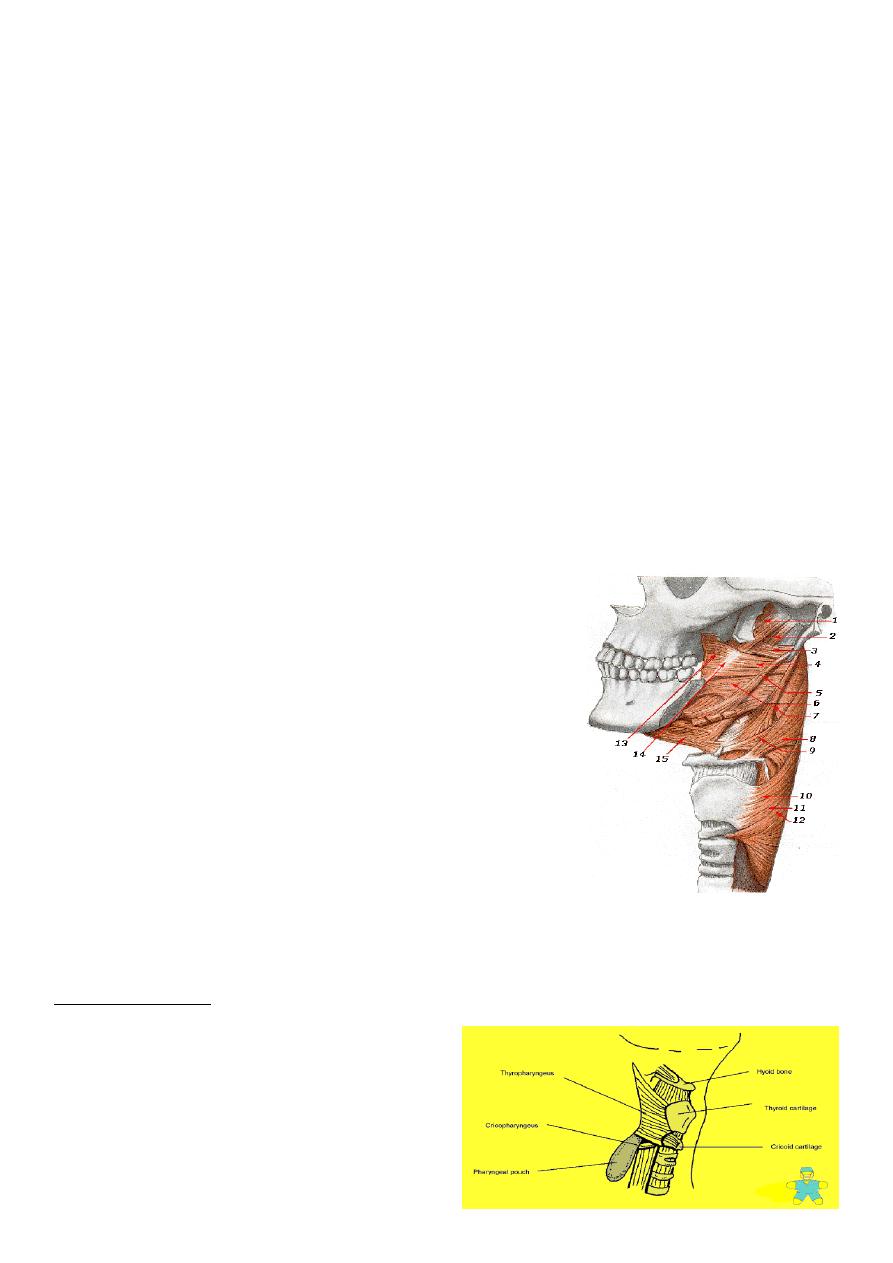
3- Muscular Layer
I- Circular (outer): which consist of 3 constrictor muscles overlapping one another
from below upwards.
1. Superior constrictor.
2. Middle constrictor.
3. Inferior constrictor.
The inferior constrictor muscle is composed of 2
parts:
a. Thyropharyngeus (oblique): arises from the
thyroid cartilage.
b. Cricopharyngeus (transverse): arises from the
cricoid cartilage and passes transversely
backwards forming the upper oesophageal sphincter.
All the constrictor muscles are inserted posteriorly
into the median pharyngeal raphae.
Functions
The constrictor muscles propel the bolus of food down into the esophagus
The Cricopharygeus (lower fibers of the inferior constrictor) act as a sphincter, preventing
the entry of air into the esophagus between the acts of swallowing
Killian dehiscence:this is a potential gap between the fibers of the thyropharyngeus and
cricopharyngeus. The mucous membrane may
bulge between these two muscles when
there is incoordination of the pharyngeal
peristaltic waves.
Pharyngael Pouch
5
II- Longitudinal (internal):
these muscles elevate the larynx and shorten the pharynx
during deglutition:
1. Stylopharyngeus.
2. Salpingopharyngeus.
3. Palatopharyngeus
Buccopharyngeal Fascia
This fascia is loosely attached posteriorly to the prevertebral fascia and laterally connected
to the styloid process and to the carotid sheath
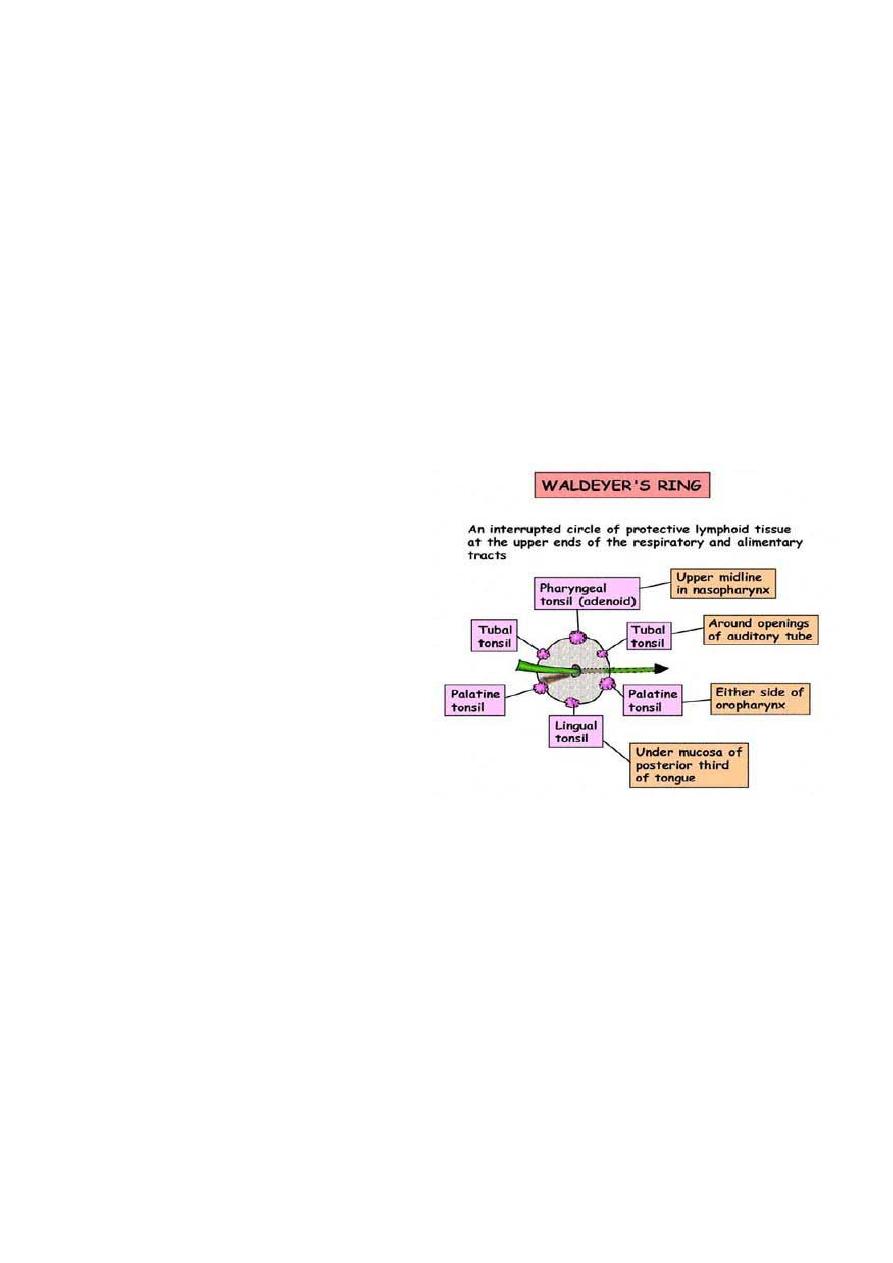
Waldeyer's ring
Subepithelial lymphoid tissue of the pharynx (Waldeyer's ring)
Is a collection of sub-epithelial lymphoid tissue around the entrance of the respiratory and
alimentary tracts.
Waldeyer's ring is formed by
1. Nasopharyngeal tonsil (adenoid).
2. Tubal tonsils: lie behind the openings of
the Eustachian tubes.
3. Palatine tonsils.
4. Lingual tonsils: which is embedded in
the posterior 1/3 of the tongue.
5. Lateral pharyngeal bands behind the
posterior tonsillar pillar.
6. Lymphoid nodules scattered on the
posterior pharyngeal wall
Hypertrophy of the lymphoid tissue of Waldeyer's ring occurs in the earlier years of
childhood. Maximum bulk is obtained at the age of 3- 6 years, and in old age it atrophies
Waldeyer's ring is characterized by:
1. Sub-epithelial lymphoid tissue.
2. Lack a definite capsule.
3. They have efferent lymph vessels, but no afferent vessels.
4. Function as one unit: when a member of it is removed, the others parts undergo
compensatory hypertrophy.
6
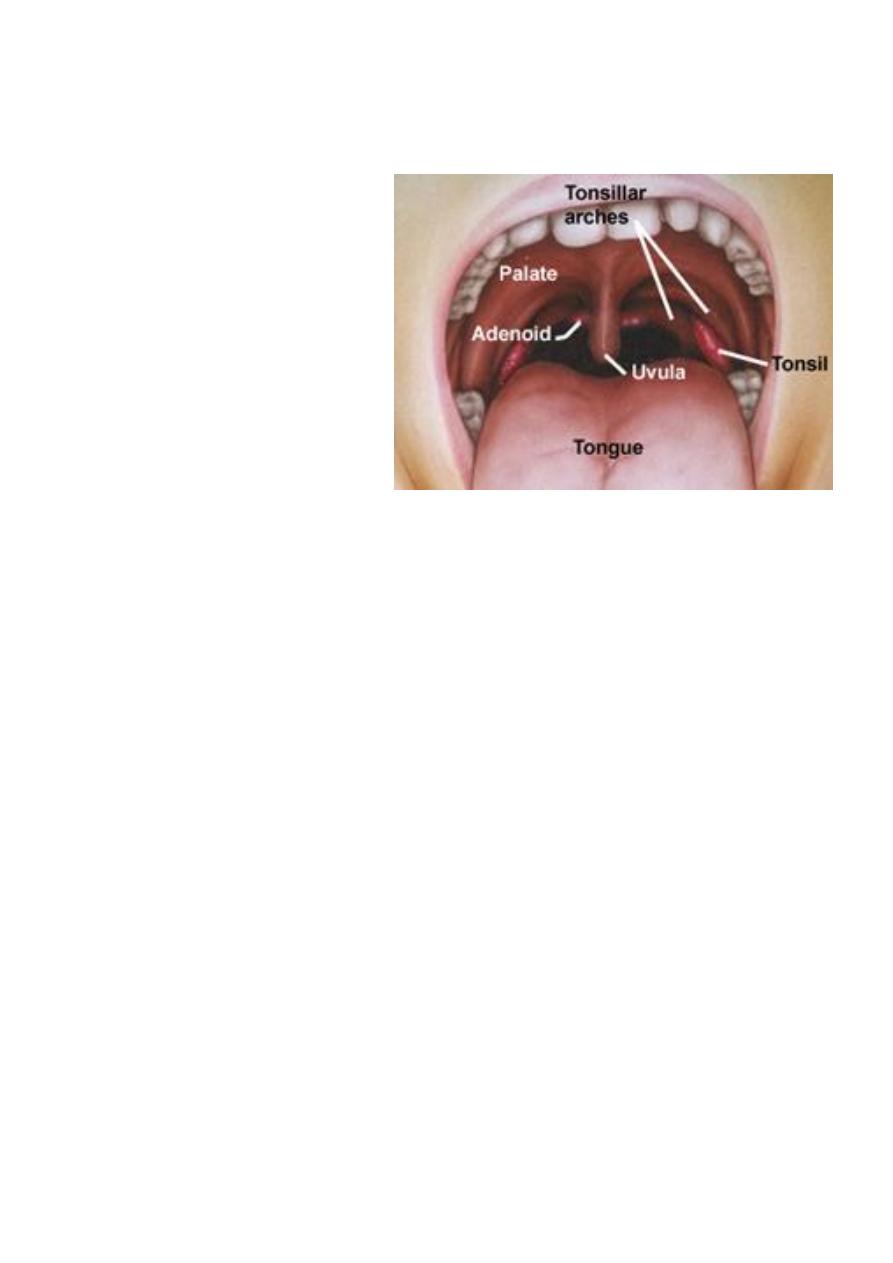
Palatine Tonsils
Two masses of lymphoid tissue situated on each side of the oropharynx.
The medial surface is exposed in the pharynx and is pitted by a number of crypts.
The tonsil is related anteriorly and posteriorly to the palatoglossus and
palatopharyngeus muscles.
Laterally the tonsil is enclosed
by a dense fibrous capsule
separating the tonsil from the
superior constrictor muscle
(tonsillar
bed).This
capsule
provide a convenient plane of
separation of the tonsil during
tonsillectomy
Blood Supply of the Tonsil
The main supply is the tonsillar branch of the facial artery, and decsending
palatine artery.The venous drainage is to the paratonsillar vein which drains to the
pharyngeal plexus, and the internal jugular vein.
Lymphatic Drainage
Deep cervical chain of lymph nodes.
Nerve Supply of the Pharynx
Sensory Nerve Supply
Nasopharynx: Maxillary nerve, trigeminal
Oropharynx: Glossopharyngeal nerve, trigeminal
Laryngopharynx: vagus nerve, and glossopharyngeal.
Motor supply
All the muscles of pharynx, except the stylopharyngeus, are supplied by the
pharyngeal plexus.
Pharyngeal branches of the IX and X nerves, and sympathetic fibers from the superior
cervical ganglion.
The stylopharyngeus is supplied by the glossopharyngeal nerve
7
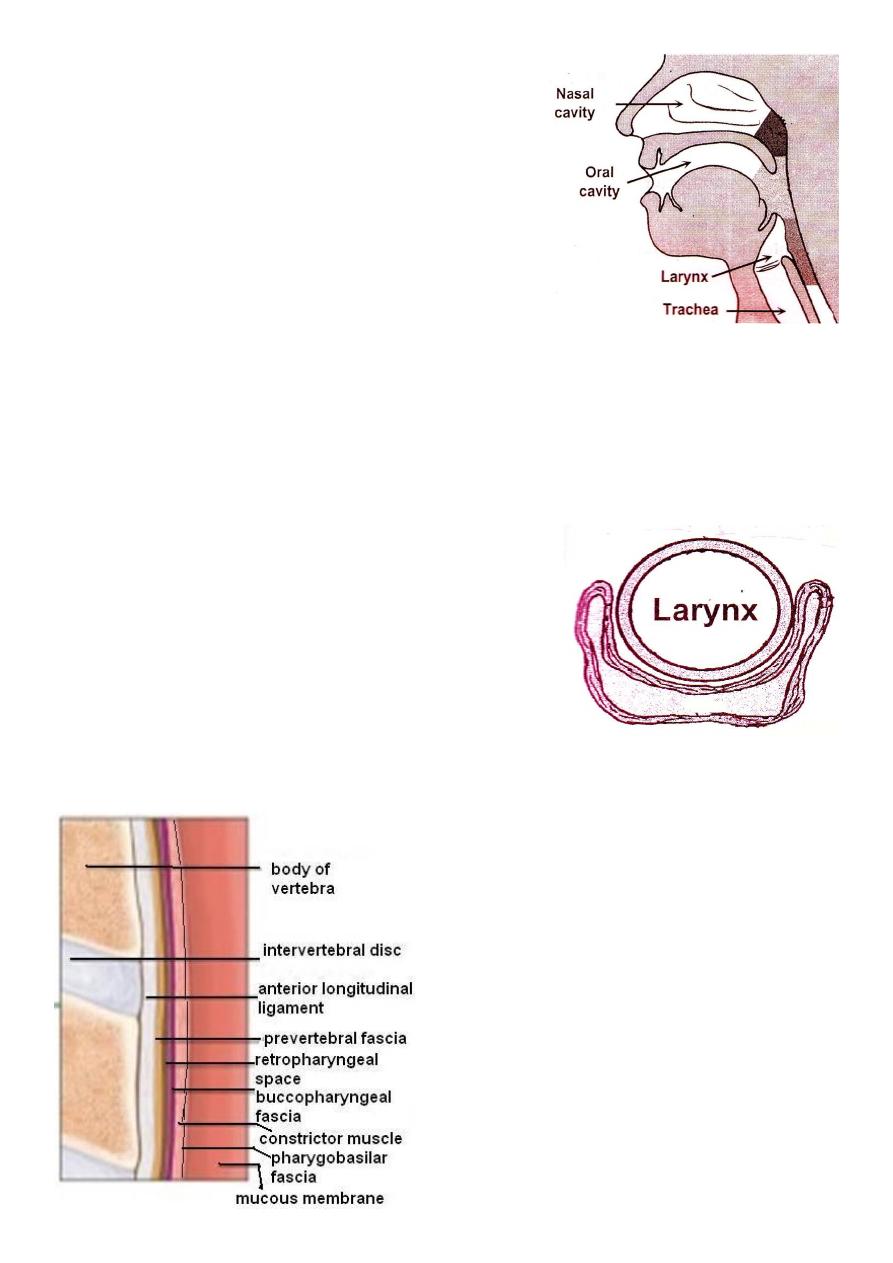
Retropharyngeal Space (Space of Gillette)
This space lies behind the pharynx and extends from
the base of the skull to the superior mediastinum.
The anterior wall is formed by the posterior
pharyngeal wall and it's covering buccopharyngeal
fascia.
The posterior wall is formed by the cervical vertebrae
and their covering muscles and fascia.
Contents:
Retropharyngeal lymph nodes of Rouviere.
Usually disappear spontaneously during the
3rd or 4th year of life.
Parapharyngeal Space
This potential space lies lateral to the pharynx and connects posteriorly with the
retropharyngeal space.
It extends from the base of the skull to the hyoid bone.
It's bounded medially by the superior constrictor muscle.
Laterally lies the medial pterygoid muscle, the mandible and the parotid gland.
It's posterior wall is the prevertebral muscles and fascia.
Contents
1. Deep cervical lymphnodes.
2. The last 4 cranial nerves and the cervical sympathetic trunk.
3. Great vessels of the neck: carotid and internal jugular vein.

8
Physiology of the Pharynx
1. Food and air inlet.
2. Play an important role in speech through vocal resonance and articulation.
3.The protective function of Waldeyer's ring.
4. Deglutition: it's divided into 3 stages:
a. Oral stage (voluntary).
b. Pharyngeal stage (involuntary).
c. Oesophageal stage (involuntary).
Symptoms of Pharyngeal Diseases
1- Sore throat (pain)
a. Inflammatory.
b. Neoplastic.
c. Neurological: IX neuralgia.
d. Blood dyscrasia: agranulocytosis and leukaemia.
2- Dysphagia: is difficulty in swallowing whereas odynophagia is painful
swallowing.
Dysphagia: Intraluminal, Luminal , Extraluminal
3- Difficulty in breathing like stridor in Ludwig's angina.
4- Difficulty in speech: Paralysis of the soft palate(hypernasalily).
5- Neck mass Cervical lymphadenopathy
Examination
Nasopharynx: This can be done with postnasal mirror and tongue depressor
(posterior rhinoscopy), and it can be thoroughly examined by rigid and
flexible endoscopes.
Oropharynx: It is simple with tongue depressor; palpation may be needed
for the tongue.
Hypopharynx: It can be done with the use of laryngeal mirror to examine
the larynx too. It can be done thoroughly with the use of endoscope.
Neck examination: for cervical lymphadenopathy.
Other areas : ears are examined for secretory otitis media in cases of
nasopharyngeal tumours.
Investigations of pharyngeal diseases
Radiography:
Plain films like lateral X-Ray of the skull, is needed in nasopharyngeal mass like
adenoids, and can demonstrate bone erosion in cases of nasopharyngeal
cancer.
Contrast films: barium swallow is needed in the diagnosis of pharyngeal pouch,
esophageal web and hypopharyngeal mass.
9
CT scan
MRI scan.
Laboratory investigations:
CBC, ESR, serum iron and iron binding capacity, monospot test, serology for
toxoplasma, brucella, CMV and HIV.
Biopsy for suspected lesions in the pharynx may be needed
.
Stomatitis
Is an inflammation of the whole lining of the oral cavity.
It could be:
-Viral infection: Herpes simplex
-Bacterial: Gingivitis.
-Fungal: candidiasis (thrush).
-Spirochaetes: Vincent's angina.
-Miscellaneous: Aphthus, Behcets syndrome, pemphigus and pemphigoid.
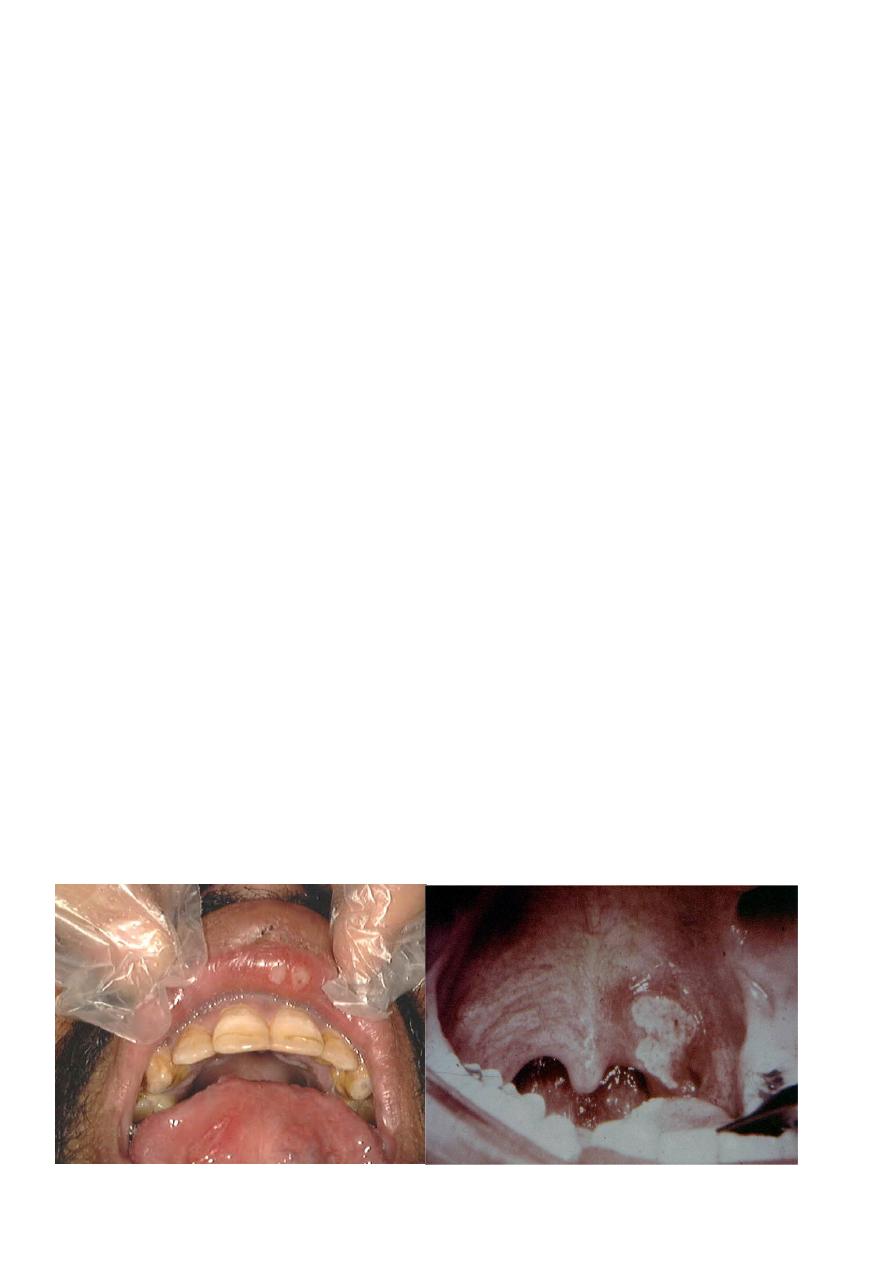
Aphthus Ulcer
Recurrent oral ulceration of unknown aetiology:
viral, psychogenic, endocrinal and autoimmune.
Clinical picture
This ulcer is typically quite sensitive and painful, has a central necrotic base with a
surrounding red circumference.
Two types:
The minor form, more common, 3-6 mm in size and multiple and heal within 7-10
days without leaving a scar.
The major form, 1-2 cm in size, less common, long lasting and heal with a scar.
11
Treatment
Is symptomatic:
-Oral antiseptic: like chlorhexidine gurgle.
-Topical application of local analgesic like xylocaine.
-Topical steroids e.g. Kenalog in orabase.
Acute necrotizing gingivitis (Vincent's angina)
It is a gingivitis producing ulceration and necrotic membrane.
It is called "Trench Mouth"
Aetiology
Infection : Spirochaete, Borrelia vincenti & an Anaerobic organism , Bacillus
fusiformis.
Occurs in debilitated patients who have poor dental hygiene.
Fever, sore throat , tender LN.
On examination
The lesions originate around the interdental papillae and gums and may spread to
involve the tonsil and oropharyx. The ulcers are painful, associated with foeter (fishy
odor), and covered by a slough.
Diagnosis
Swab for gram stain and culture.
Treatment
-Oral hygiene by mouth wash.
- Antibiotics like benzyl penicillin + metronidazole.
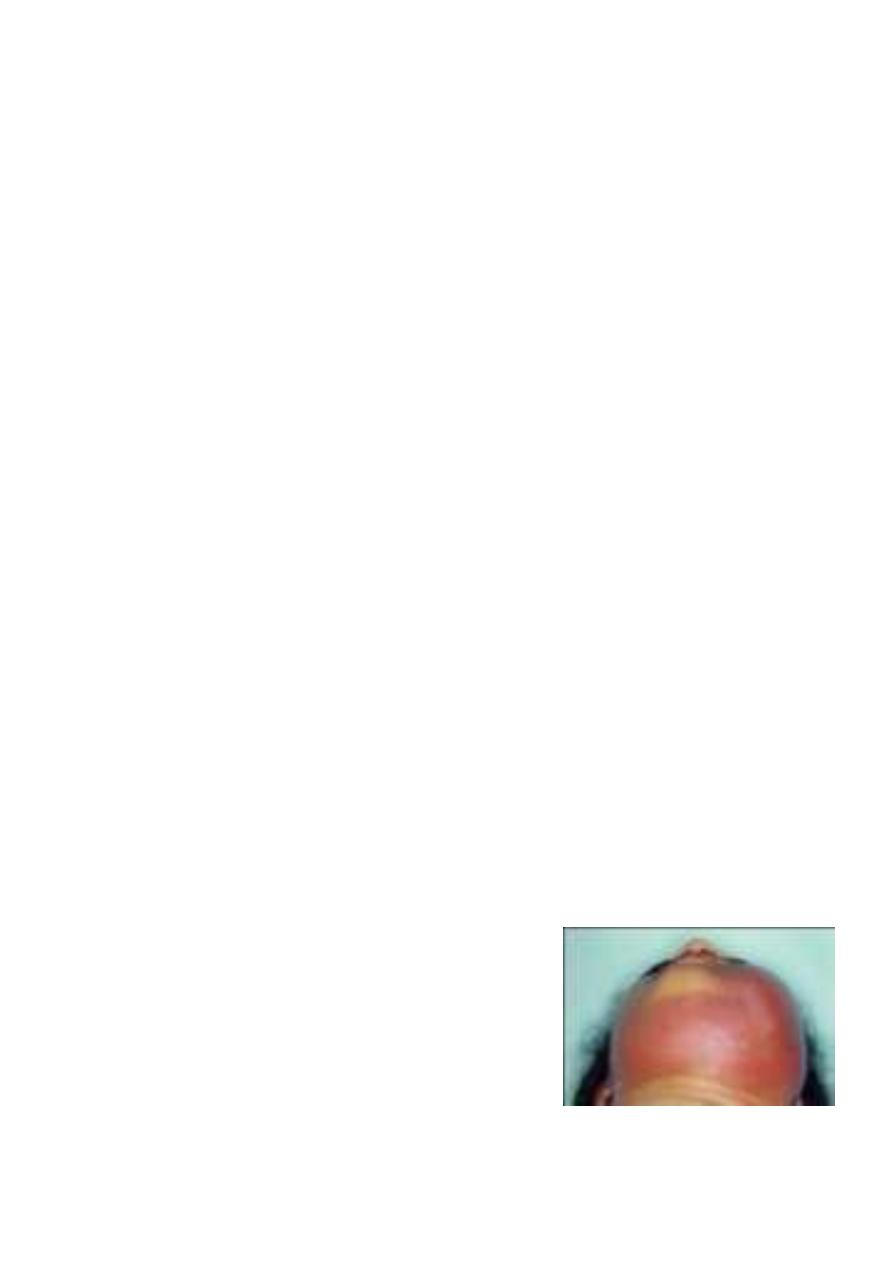
Ludwig's Angina
Acute cellulitis of the floor of the mouth and submandibular space secondary to soft
tissue infection.
Infection within a closed fascial space, tension rises rapidly and laryngeal oedema
may occur.
Aetiology
Root abscess of the lower premolar and molar
teeth (80%).The most usual organisms are strepto.
viridans and E. coli.
-Tonsillar infection.
-Submandibular sialadenitis
Clinical picture
The patient is ill, toxic > 38 oC with odynophagia and salivation.
11
On examination
Indurated and usually non-fluctuant swelling below the angle of the jaw.
The floor of the mouth becomes very oedematous with the tongue pushed upwards.
Potential complications
-Airway compromise due to laryngeal oedema.
-Spread into the parapharyngeal and retropharyngeal spaces.
-Septicaemia.
-Aspiration pneumonia.
Treatment
-Early stages (early cellulitis): heavy antibiotics covering aerobes and anaerobes.
-Drainage: If the state progress and the swelling
increases.
Curved incision 2 cm below the angle of the jaw.
-Endotracheal intubation and
tracheostomy may be required
if laryngeal oedema
supervenes.
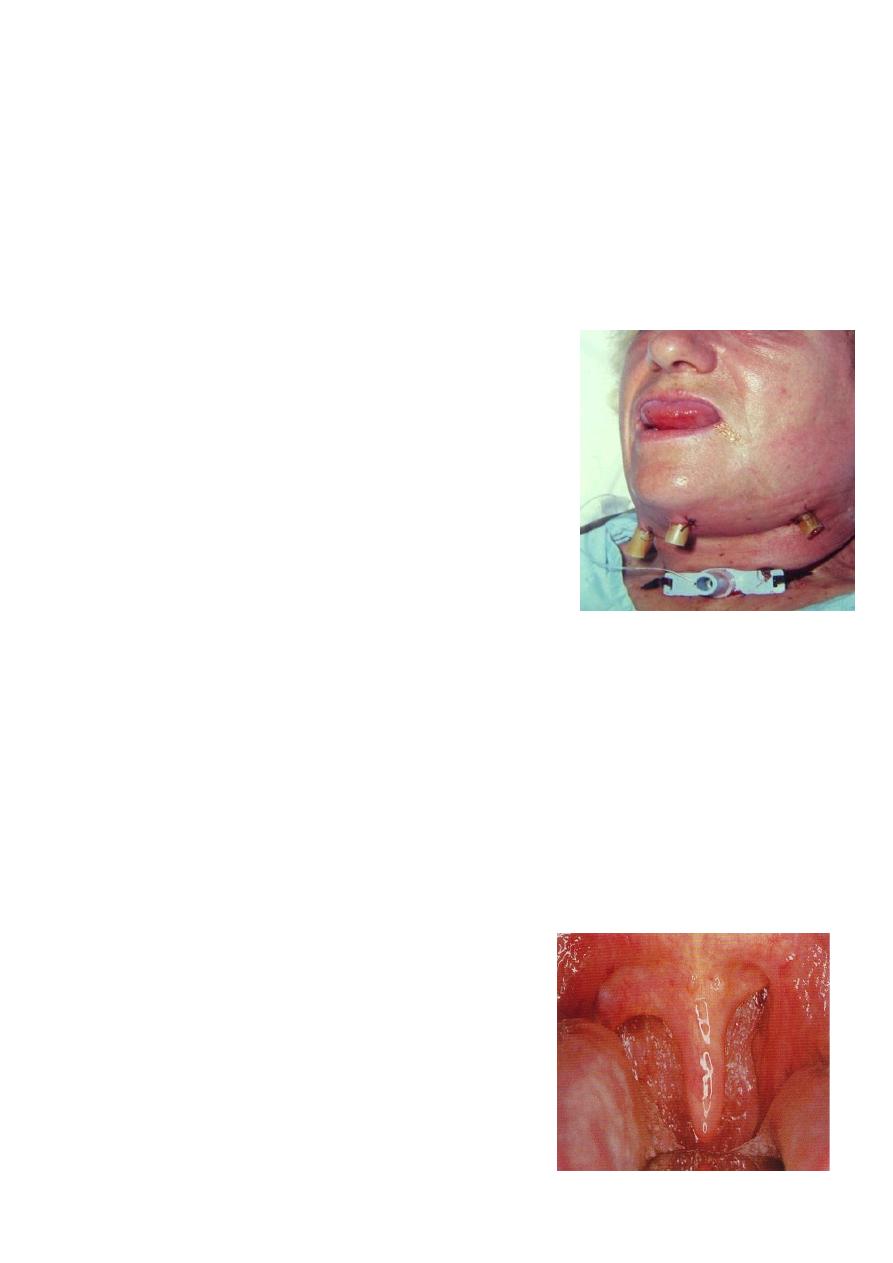
Pharyngitis
Acute pharyngitis
Acute inflammation of the mucous membrane of the pharynx occurring primarily in
winter months.
Aetiology
Viral in origin( mostly adenovirus and rhinovirus).
20 % are bacterial: mostly Pneumococci, Haemophilus influenza and group A beta-
hemolytic streptococci (S. Pyogens).
30 % No pathogen is isolated.
Pharyngitis may be part of the clinical picture of measles, scarlet fever, infectious
mononucleosis and typhoid fever.
Symptoms
-Sore throat, Chills, Pyrexia, Headache and Joint
pain.
Sings
-Redness and injection the mucous membrane of
the pharynx.
-Hypertrophic and proliferation of lymphoid tissue
on the posterior pharyngeal wall with particular
aggregates in the lateral pharyngeal bands.
- Oedema of uvula
-Tender and palpable cervical LN.
12
Treatment
-Symptomatic: bed rest, analgesics and fluid by mouth.
-Antibiotics: if bacterial infection is suspected.
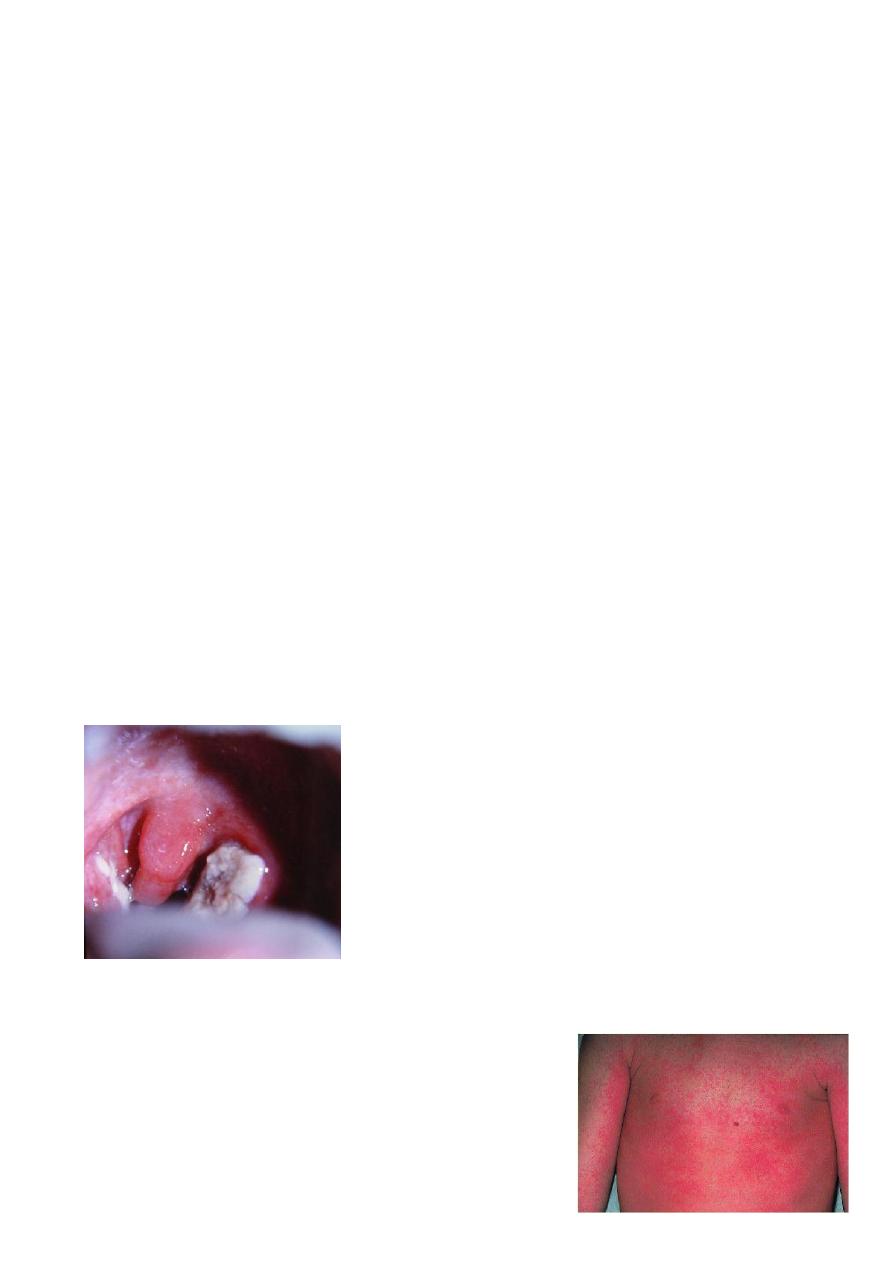
Acute Tonsillitis
Generalized inflammation of the mass of the tonsil, usually accompanied by a degree
of inflammation of the pharynx.
Any age group, most frequently found in children.
Aetiology
Bacteria :group A B-haemolytic streptococcus, pneumococcus, staphylococcus&
Haemophilus influenzae.
Viruses: rhinovirus, adenovirus &
enterovirus
Symptoms
Onset: often sudden :
-Sore throat & odynophagia.
-Constitutional symptoms especially in children.
-Referred otalgia and abdominal pain due to mesenteric adenitis.
Examination
- Furred tongue & halitosis.
- Tonsils: enlarged red and swollen.
-The crypts become filled with pus (follicular tonsillitis).
- A patchy membrane on the surface of the tonsil (membranous tonsillitis).
-Cervical tender lymphadenopathy jugulodigastric node.
Acute follicular tonsillitis
Differential Diagnosis
-Scarlet fever: Streptococcal infection erythrogenic toxin.
Tongue has a strawberry appearance
Cutaneous punctate erythema.
-Glandular fever:
-Agranulocytosis and leukaemia.
-Acute diphtheria.
-Vincent's angina.
Acute
13
Complications
local
a. peritonsillar abscess(quinsy).
b. Retropharyngeal abscess.
c. Parapharyngeal abscess.
d. Acute otitis media.through the Eustachian tube.
General
a. Rheumatic fever and glomerulonephritis which follow B- haemolytic streptococcal
tonsillitis of Lancet group A.
b. Subacute bacterial endocarditis.
c. Septicaemia.
Treatment
1. Bed rest, good oral fluid intake.
2. Antipyretics and analgesics.
3. Antibiotics: Penicillin, Erythromycin in allergy to penicillin.
Lack of response may suggest the presence of B-lactamase producing organism or
even an anaerobic one, in which augmentin and/or metronidazole will be the
antibiotic of choice.
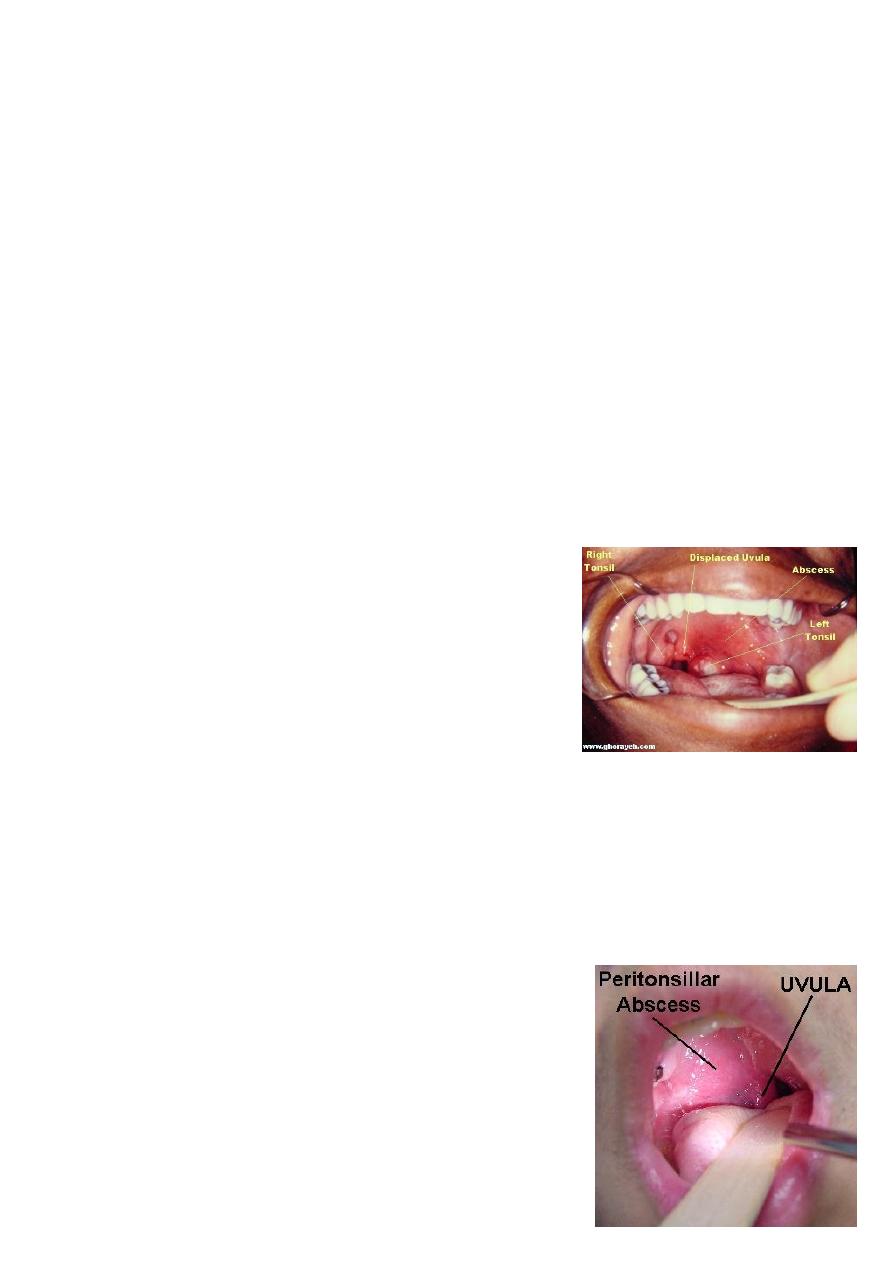
Peritonsillar Abscess( Quinsy)
Is a collection of pus between the fibrous capsule of
the tonsil and the superior constrictor.
Usually unilateral, Adult males.
Complication of acute tonsillitis.
Clinical Picture
1. The patient looks ill, feverish with rigor .
2. Acute sore throat & referred otalgia,
Odynophagia). This makes the saliva dribbles from
the month.
3. Trismus: irritation of the pterygoid muscles .
4. Thick and muffled voice often called “hot potato
voice”.
Examination
1. The tonsil is congested and pushed medially with the soft palate bulging
downward and forward.
The uvula may be pressed against the opposite tonsil.
2. Red and enlarged anterior tonsillar pillar.
3. Tender and enlarged cervical lymph nodes
Treatment
I. Medical : Effective in early peritonsillar cellulitis.
II. Surgical : when considerable swelling is present or
in case of failure to medical treatment.
1. Incision of the abscess: this is undertaken at the
point of maximum swelling of the soft palate. The

14
classical site is at a point where an imaginary
line through the base of the uvula is
intersected by a perpendicular line from the
junction of the anterior tonsillar pillar with the
tongue.
The tonsils might be removed 6-8 weeks
following quinsy.
2. Abscess tonsillectomy
