Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 1 of 13
BENIGN TUMORS OF UTERUS
(Uterine fibroids)
Definition
o A uterine fibroid (also uterine leiomyoma,
myoma, fibromyoma,
leiofibromyoma, fibroleiomyoma, and fibroma) (plural of ... myoma
is ...myomas or ...myomata) is a benign (non-cancerous) tumor that
originates from the smooth muscle layer (myometrium) and the
accompanying connective tissue of the uterus.
o Fibroids are the most common benign tumors in females and
typically found during the middle and later reproductive years. While
most fibroids are asymptomatic, they can grow and cause heavy and
painful menstruation, painful sexual intercourse, and urinary
frequency and urgency. Some fibroids may interfere with pregnancy
although this appears to be very rare.
Prevalence
o Uterine fibroids Present in up to 25% of women of reproductive age.
o Fibroids are most common in women aged 30-40, but they can occur
at any age.
o Fibroids occur more often in black women than in white women.
o They associated with nulliparity and more common in women with
family history of fibroids and obesity.
o The incidence is decreased with:
1. Prolonged use of the oral contraceptive pill.
2. Prolonged use of Depo-provera.
3. increasing numbers of term pregnancies.
4. smoking.
5. Fibroids regress in size and undergo degeneration after the
menopause.
:العدد
7
2/3/2014
Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 2 of 13
Aetiology and pathogenesis
o The exact causes of fibroid are not well understood but research and
clinical experience point to several factors:
o Genetic alterations. Many fibroids contain alterations in genes that
code for uterine muscle cells.
o Hormones. Estrogen and progesterone, two hormones that stimulate
development of the uterine lining in preparation for pregnancy,
appear to promote the growth of fibroids. Fibroids contain more
estrogen and estrogen receptors than do normal uterine muscle cells.
o Other chemicals. Substances that help the body maintain tissues, such
as insulin-like growth factor, may affect fibroid growth.
Fibroid location
o Intramural Fibroids are located within the wall of the uterus and are
the most common type; unless large, they may be asymptomatic.
Intramural fibroids begin as small nodules in the muscular wall of the
uterus. With time, intramural fibroids may expand inwards, causing
distortion and elongation of the uterine cavity.
o Subserosal fibroids are located underneath the mucosal (peritoneal)
surface of the uterus and can become very large. They can also grow
out in a papillary manner to become pedunculated fibroids. These
pedunculated growths can actually detach from the uterus to become
a parasitic leiomyoma.
o Submucosal fibroids are located in the muscle beneath the
endometrium of the uterus and distort the uterine cavity; even small
lesion in this location may lead to bleeding and infertility. A
pedunculated lesion within the cavity is termed an intracavitary
fibroid and can be passed through the cervix.
o Cervical fibroids are located in the wall of the cervix (neck of the
uterus). Rarely fibroids are found in the supporting structures (round
ligament, broad ligament, or uterosacral ligament) of the uterus that

Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 3 of 13
also contain smooth muscle tissue.
o Tumors in subserosal and intramural locations comprise the majority
(95%) of all fibroids while submucous fibroid comprise 5%.
Pathology
o Leiomyomas grossly appear as round, well circumscribed (but not
encapsulated), solid nodules that are white or tan, and show whorled
appearance on histological section. The size varies, from microscopic
to lesions of considerable size. Typically lesions the size of a
grapefruit or bigger are felt by the patient herself through the
abdominal wall.
o Microscopically, tumor cells resemble normal cells (elongated,
spindle-shaped, with a cigar-shaped nucleus) and form bundles with
different directions (whorled). These cells are uniform in size and
shape, with scarce mitoses. There are three benign variants: bizarre
(atypical); cellular; and mitotically active.
Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 4 of 13
Clinical features
It depened on the size, location, and number of tumors.
A. Asymptomatic:
Most fibroids (50%) not cause any symptoms& accidentally
discovered on abdominal or pelvic examination or during
ultrasound examination.
B. Symptomatic:
About 20–50% of women with fibroids present with symptoms.
(1). Abnormal uterine bleeding ;include
o Menorrhagia (Heavy menstrual bleeding) is usually caused by
intramural fibroids or submucosal fibroids.
o Intermenstrual bleeding, mainly in pedunculated submucosal fibroid
o Postcoital bleeding, mainly in pedunculated submucosal fibroid
(2). Pressure symptoms: pressure on surrounding structures.
1. Urinary bladder:
Urinary frequency.
Incontinence.
Urine retention (rarely)
hydroureter or hydronephrosis
2. Venous system; varicosities, lower extremity edema,
hemorrhoids.
3. Nerves that supply the pelvis and the legs, causing pain in
the back, flank, or legs.
(3). Pain:
Pain occurs in approximately 30% of women with uterine fibroids.
Feeling of pelvic heaviness that can radiate to the back or lower
extremities.
Congestive Dysmenorrhea

Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 5 of 13
Dyspareunia.
Causes of pain in fibroid
a. Torsion of a pedunculated fibroids.
b. Prolapse of pedunculated submucosal fibroids.
c. Red degeneration.
d. Infection.
e. Sarcomatous changes (Malignant changes).
f. Adhesion
(4).infertility; (less than 3% of cases).
It Compromise of the patency of the fallopian tube.
A. Large intramural tumors located in the cornual regions may
obstruct the tubes.
B. intraligamentous fibroids may cause tubal obstruction.
C. Distortion of the endometrial cavity and Continuous bleeding in
patients with submucous fibroids may impede implantation.
(5) A palpable abdominal-pelvic mass and abdominal swelling.
(6) Malignant changing Transformation to uterine leiomyosarcomas
is extremely rare (0.1% ).
It must always be suspected when the following signs are
present:
A. Enlargement of the uterus in postmenopausal patients.
B. Rapid changes in size and consistency of the tumor.
C. Ascites and recurrence after surgery.
o The signs depends on type, size, number, any changes of fibroids.
o By Abdominal examination:
o Very large fibroids can cause abdominal distension and can be
palpated abdominally as irregular nodular tumor firm mass arising
Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 6 of 13
from pelvis.
o Those smaller than 13 weeks gestational size are usually confined to
the pelvis (abdominally not palpable).
o By speculum examination, Polyp coming out cervical os can be seen.
o Bimanual examination show uterine enlargement. The mass felt to be
part of the uterus usually with some mobility.
o Uterine enlargement:
o Symmetrically enlarged uterus (submucosal fibroid).
o Asymmetrically enlarged uterus (subserous fibroid).
Degeneration
1. Hyaline degeneration
2. Cystic degeneration
3. Red degeneration
4. Sarcomatous change
5. The others:
a. Fat degeneration
b. Calcification
c. The secondary infection
Red Degeneration
o Occasionally seen as a complication of pregnancy(during pregnancy
or immediate postpartum period)
o The pathogenesis is unknown,may be the result of the accumulation of
blood in the tumour because of venous obstruction.
o The cut surface resembles raw meat.
1. a cause of pain(acute)
Result from the diminished
vascularity of the
connective-tissue element
Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 7 of 13
2. Fever
3.Rapid growth,
4. tender
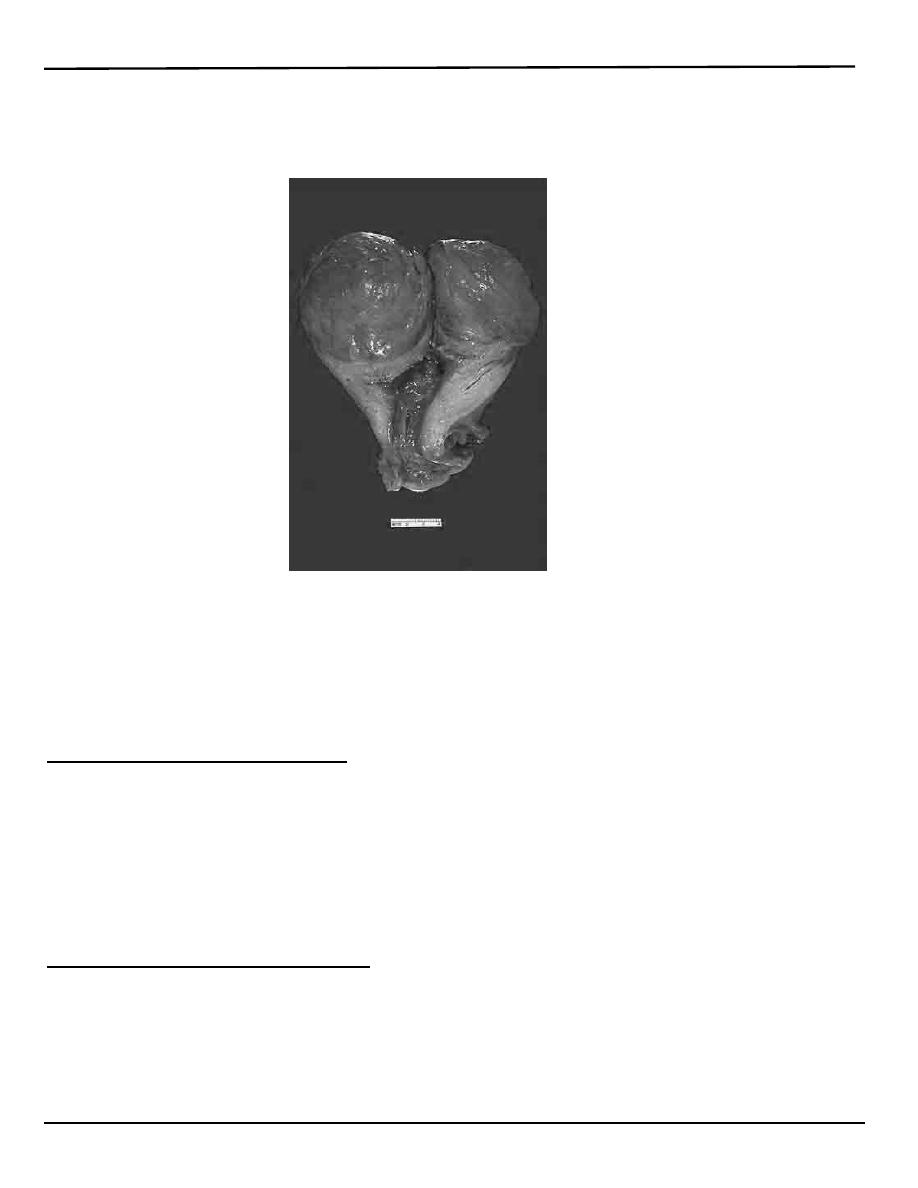
Here is a very large leiomyoma of the uterus that has undergone
degenerative change and is red (so-called "red degeneration"). Such an
appearance might make you think that it could be malignant.
Rmember that malignant tumors do not generally arise from benign
tumors.
Sarcomatous Change
o Rare:0.4%~ 0.8%
o More common at 40~ 50 years old
o Usually occur in intramural fiboids
o grow quickly
o vaginal bleeding
Differential Diagnosis
1. Pregnancy.
2. Ovarian tumors
3. Adenomyosis.
4. Tubo-ovarian abscesses.
Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 8 of 13
5. Endometrial cancer.
6. Liomyosarcoma .
7. Congenital anomalies of the uterus.
Investigations
1. Gynecologic ultrasonography
I. transabominal and/or transvaginal ultrasound
A..identify uterine fibroid or any mass.
B.Assess uterine dimension
C.Location of fibroid.
II. Sonohysterography (saline infusion sonography):
Inject a small amount of saline into the uterine cavity so
that the lining of the uterus can be seen, Tumors sitting
inside of the cavity can be readily seen.
2. Hysterosalpingography (HSG).
Helpful specifically in the evaluation of lesions that affect the
uterine cavity
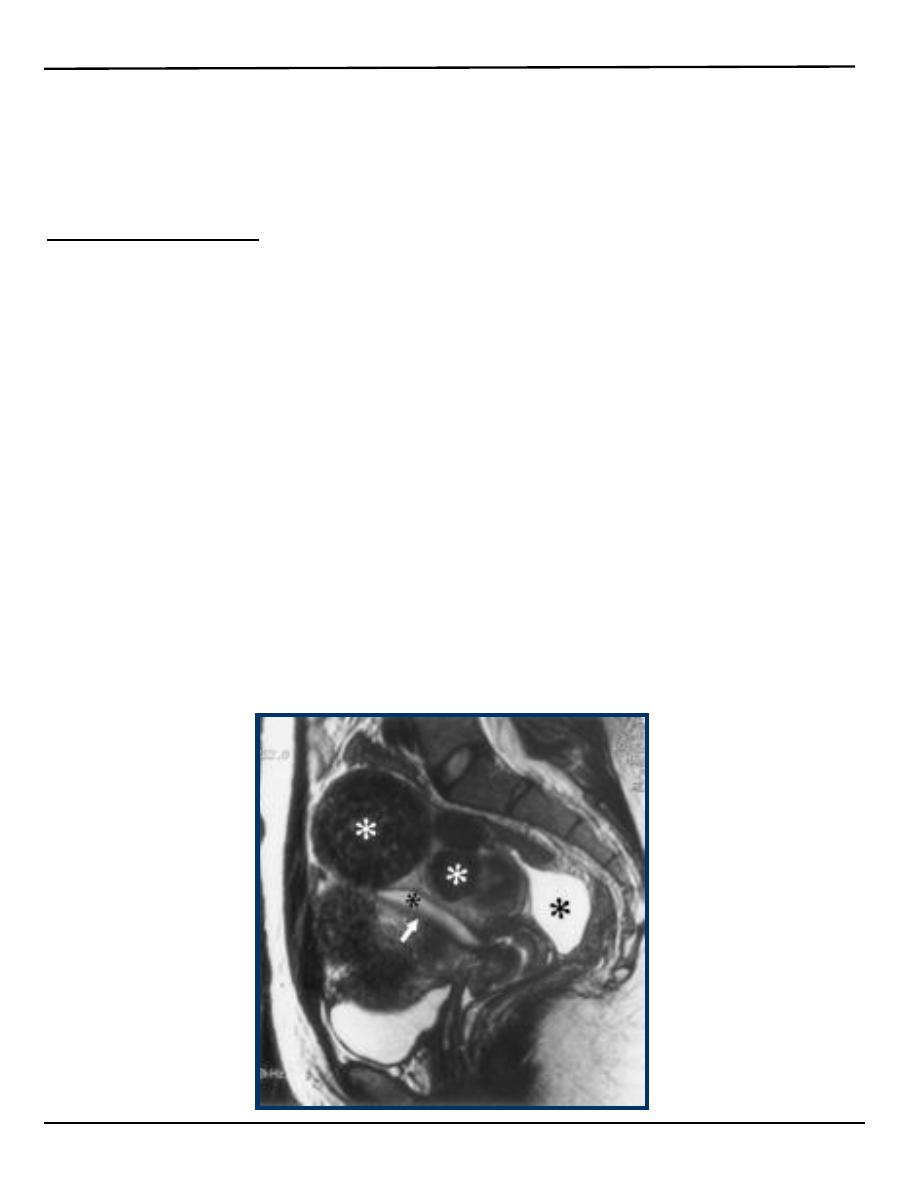
3. Magnetic resonance (MR) imaging
It is expensive and not used routinely. Only use if there is any
doubt about the nature of a fibroid mass.
Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 9 of 13
4. Hysteroscopy
5. Laparoscopy
6. Endometrial Sampling: Performed to evaluate abnormal Bleeding in
patients who are at risk for endometrial polyps, hyperplasia, or
carcinoma.
7. Immaging of renal tract: may be helpful in patient with large fibroids
to excluded hydronephrosis
Treatment
o Most fibroids do not require treatment unless they are causing
symptoms. After menopause fibroids shrink and it is unusual for
fibroids to cause problems.
o Symptomatic uterine fibroids can be treated by:
1.medication to control symptoms
2.medication aimed at shrinking tumours
3.ultrasound fibroid destruction
4.various surgically aided methods to reduce blood
supply of fibroids
5.myomectomy or radio frequency ablation
6.hysterectomy
o Treatment must be individualized according to:
1. Patient (age-parity-symptoms).
2. Fibroid (number-size-type-rate of growth).
3. Complications associated with fibroids.
Approximately 80% of fibroids are asymptomatic and are smaller
in size than a twelve week gestation uterus do not need to be
removed and may be followed clinically. Observation with periodic
examination (every 3 to 6 months) is appropriate to rule out a
rapidly growing uterine sarcoma. After assurance of slow growth or
Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 10 of 13
stable uterine size, annual follow-up may be appropriate.
1. Medication to control symptoms
Treatment of symptom as menorrhagia
A. GnRH agonists;
It induce a hypoestrogenic pseudo-menopausal state and causes
shrinkage of the fibroids .
GnRH agonist treatment is not recommended for longer than 6
months because of the potential consequent development of
osteoporosis.
Side effect; hot flashes and osteoporosis.
Re-growth of fibroids is experienced within a few months, and for
this reason its use is recommended for short-term treatment in
selected cases which are:
1.Treatment of women approaching menopause in an
effort to avoid surgery.
2. Short-term therapy may be used preoperatively (at any
age) in the following situations:
A. pre-surgical treatment to decrease symptoms and
size which might make surgery easier or permit a
more conservative approach such as a vaginal or
laparoscopic surgical approach rather than
abdominal approach
B. control bleeding prior to surgery (so that anemia
might be corrected).
B. Levonorgestrel intrauterine devices
C. Danazol
2. Magnetic Resonance-Guided Focused Ultrasound
Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 11 of 13
There are two general types of surgery available for fibroids and its
choice depends on:
1. Patient’s wishes and parity
2. Fibroid size and number
3. Location of the fibroids.
A. Myomectomy
B. Polypectomy.
C. Hysterectomy.
A)
Myomectomy
o Involves the removal of single or multiple fibroids while preserving
the uterus.
o Myomectomy may be performed in a number of ways. The method
used depends on the location and size of the fibroids.
1. Laparotomy (Abdominal myomectomy)
2. Laparoscopic myomectomy.
3. Hysteroscopic myomectomy (submucosal fibroids).
1.Abdominal myomectomy has been associated with more
significant blood loss.
2.Abdominal myomectomy has been associated with higher
morbidity than hysterectomy.
3.The risk of recurrence after myomectomy has been
estimated to be 27% after 10 years.
4.With larger fibroids, attempted myomectomy frequently
results in hysterectomy due to uncontrollable bleeding in these
highly vascular tumors.
5.if the endometrial cavity is entered during myomectomy ,
future deliveries must be by caesarean section.
Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 12 of 13
B)
Hysterectomy
o It is a definitive therapy for uterine
o fibroids. (The only real "cure" for fibroids).
o Hysterectomy may be considered when:
(Important)
1. Pain or abnormal bleeding persists.
2. Fibroids are very large.(uterus is large >12-14weeks)
3. Other treatments are not possible.
4. A woman no longer wants children.
5. A rapid growth of the uterus caused by fibroids
1. Abdominal hysterectomy
2. Vaginal hysterectomy.
3. Laparoscopically assisted vaginal hysterectomy.
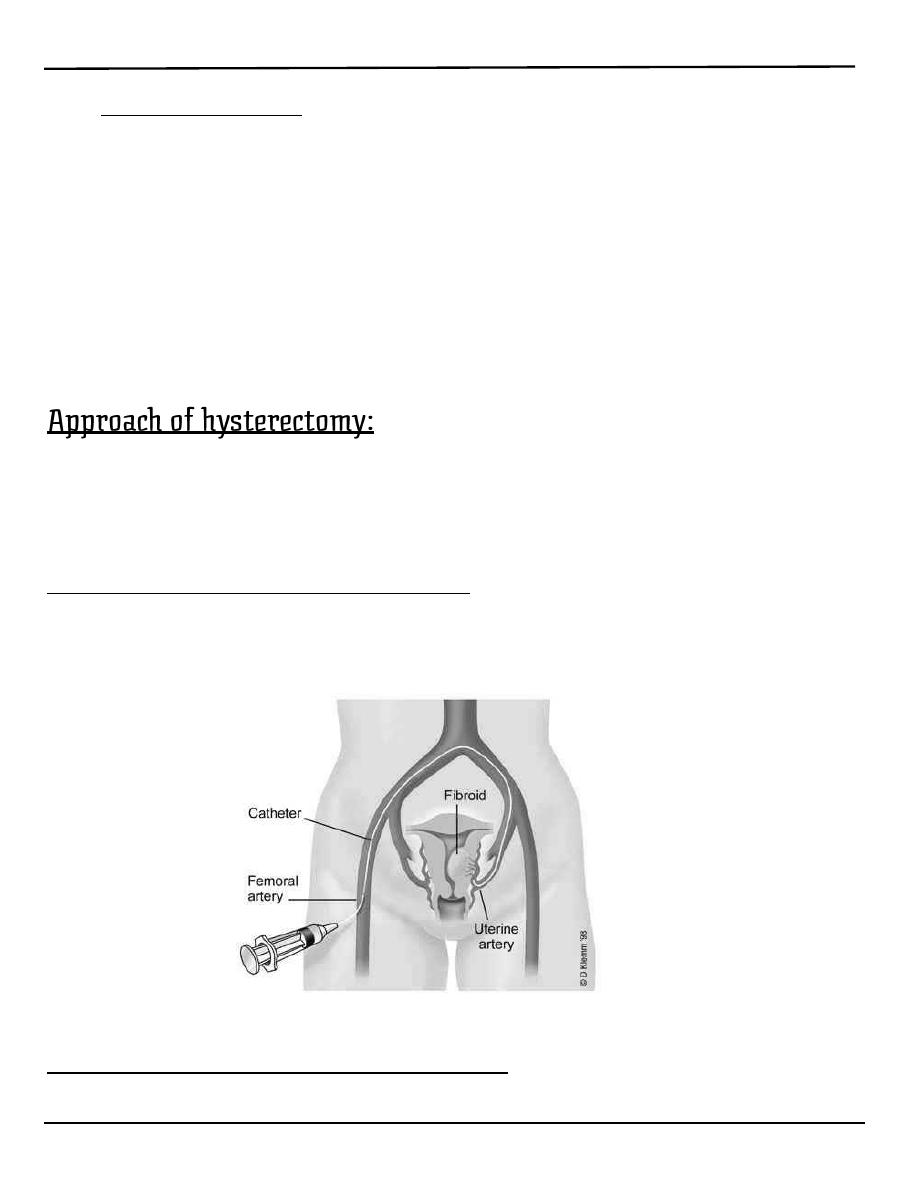
D) Uterine Artery Embolization:
Is a promising new method of treating symptomatic fibroids. In
this procedure, Embolization of the uterine arteries supplying
the fibroids.
Uterine Fibroids and Pregnancy
o A small number of pregnant women have uterine fibroids.
Lecture 5
النسائية
د. أحمد جاسم
BENIGN TUMORS OF UTERUS
Page 13 of 13
1. Enlarge .
2. Become softer ,flatten out and become indistinct.
3. May be mistaken for fetal parts.
4. Certain accident and degenerations are more common in fibroids
during pregnancy:
Red degeneration of fibroids. occur in 5-10% of women with
fibroids..
Torsion of pedunculated fibroids.( more in puerperium).
Infection in fibroids after delivery or abortion.
1. Fibroids can increase the risk of :
2. Large for date uterus
3. Abortion.
4. preterm labour
5. abruption placenta.
6. Fetal malpresentation.
7. Obstructed labour.
8. Increase incidence of caesarean section.
9. retained placental tissue.
10. Increase risk of post partum haemorrhage (PPH).
11. Delayed involuation of uterus
Usually no treatment of fibroids is needed during
pregnancy. Myomectomy should not be performed
in pregnant women because of the increased risk of
uncontrolled bleeding.
By: Mu’taz Fathi
