Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 1 of 15
1.cervical disease
2.Cervical intraepithelial neoplasia
(Cervical dysplasia)
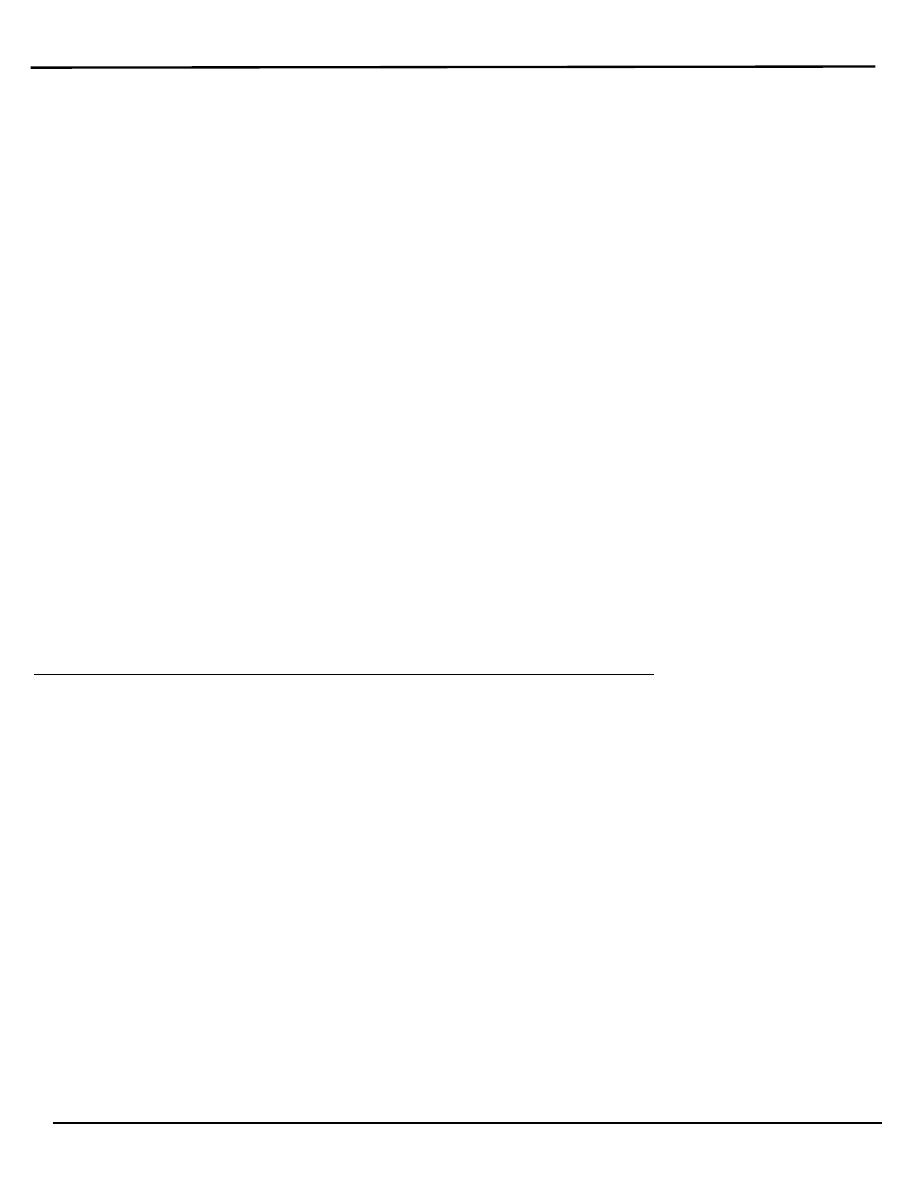
o Cervical cancer is the common cancer affecting women after breast cancer.
o Cervical cancer is a preventable disease because of:
1. There is usually a phase of premalignancy intraepitheilial
neoplasia and has relatively long natural history.
2. The cervix is a relatively accessible organ to examine.
3. The availability of a simple test for the presence of pre-
malignancy.
4. Treatment for pre-invasive disease is highly effective.
Aetiology
1. Human papillomavirus (HPV) infection
HPV infection is extremely common and in majority of cases will
not lead to development of cancer. Progression or regression
depends on several factors that interfere with the host's ability to
clear the virus such as in.
2. Transplant patient.
3. HIV-Positive women.
4. Smoking.
Screening for cervical intraepithelial neoplasia (CIN)
(Very
Important)
o Medical screening method
Detect premalignant and malignant processes of cervix.
Prevent progression of abnormal cells to cancer.
This is NOT a diagnostic test!
o Cervical cancer screening with cytology provides the opportunity for
:العدد
8
22/2/2014

Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 2 of 15
early effective intervention and has reduced morbidity and mortality
o Papanicolaou
o Cervicoscopey
o Visual inspection with acetic acid (VIA)
o Visual inspection with acetic acid and magnification (VIAM):
Gynescope or Aviscope
o Colposcopy
o Cervicography
o Automated pap smears
o Molecular (HPV/DNA) tests.
o Co-testing using the combination of cytology plus HPV DNA testing is
an appropriate screening test for women older than 30 years (applied in
some places).
Papanicolaou (Pap) smear test
What is a pap smear
o Screening test for Asymptomatic Women
o To detect treatable pre-invasive squamous Abnormalities of the Cervix
o Small number of women will develop invasive Cancer
o Not diagnostic-rather screening test to detect early changes on the
cervix.
o Exfolative cervical cytology was a technique to collect the cells that had
been shed from the cervix.
o It is a simple and painless test that may cause minor discomfort.
o Cervical Smear aims to prevent cancer, not to detect cancer.
o Cervical cancer screening should begin at age 21 years and not before
age 21 because it may lead to unnecessary and harmful evaluation and
treatment in women at very low risk of cancer.
o Women who have been immunized against HPV-16 and HPV-18 should
be screened by the same regimen as non-immunized women.
Frequency of cervical cytology screening
o Cervical cytology screening is recommended every 2 years for women
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 3 of 15
aged 21–29 years.
o Women aged 30 years and older who have had three consecutive
cervical cytology
o Test results that are negative for intraepithelial lesions and malignancy
may be screened every 3 years.
o Women with any of the following risk factors may require more
frequent cervical cytology screening:
1. Women who are infected with human immunodeficiency virus (HIV)
2. Women who are immunosuppressed (such as those who have received
renal transplants).
3. Women who were exposed to diethylstilbestrol in utero.
4. Women previously treated for CIN 2, CIN 3, or cancer (continue to
have annual screening for at least 20 years).
o Pap smear is not necessary in women in these categories:
1. Virginal patients.
2. Total Hysterectomy for benign disease.
3. Recent result of pap smear.
4. Age over 65 and over 10 benign Pap Smears.
o To prepare for the Pap test, for two days before the test, women should
avoid:
Vaginal Douching.
Using tampons.
Sexual intercourse.
Using birth control foams, creams, or jellies or vaginal medications
or creams.
o The ideal time for a woman to have a Pap Smear is five days after her
menstrual period has ended.
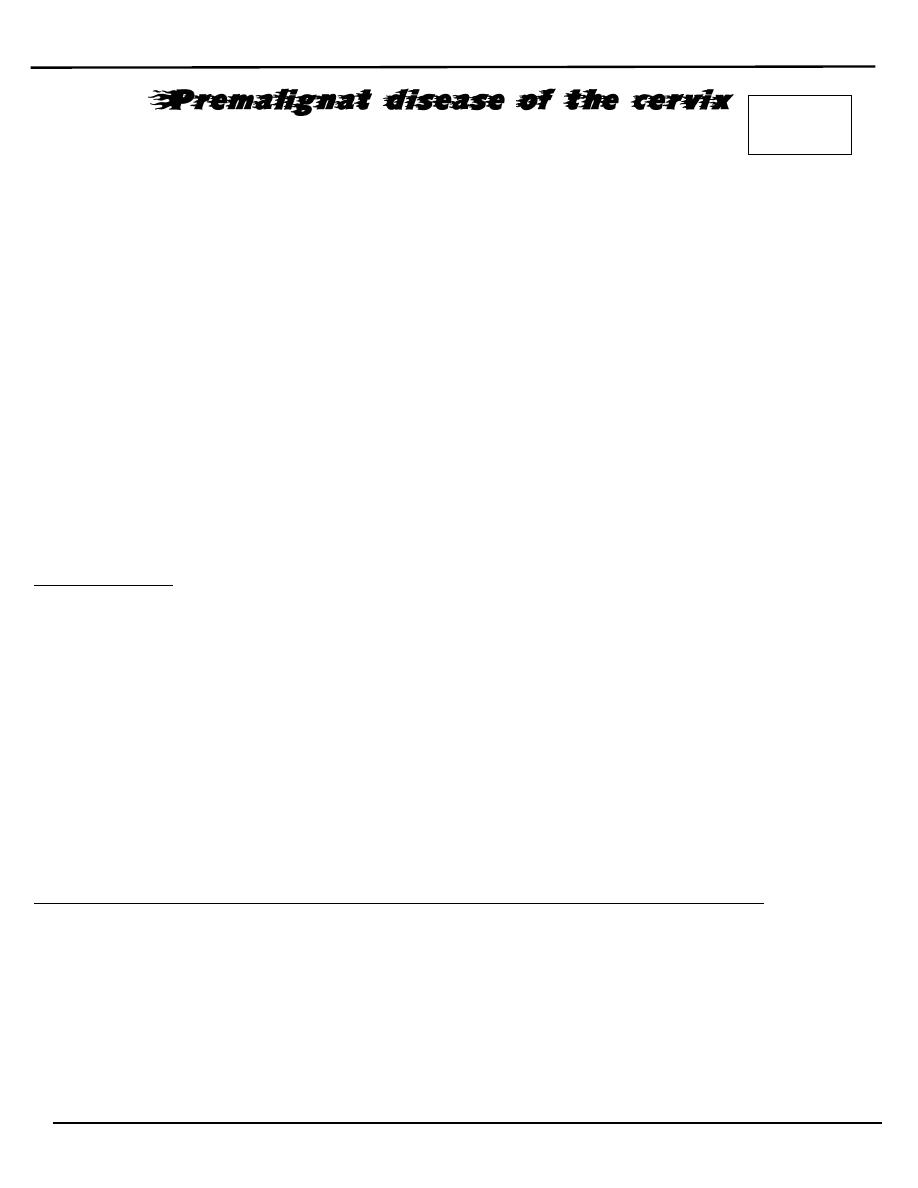
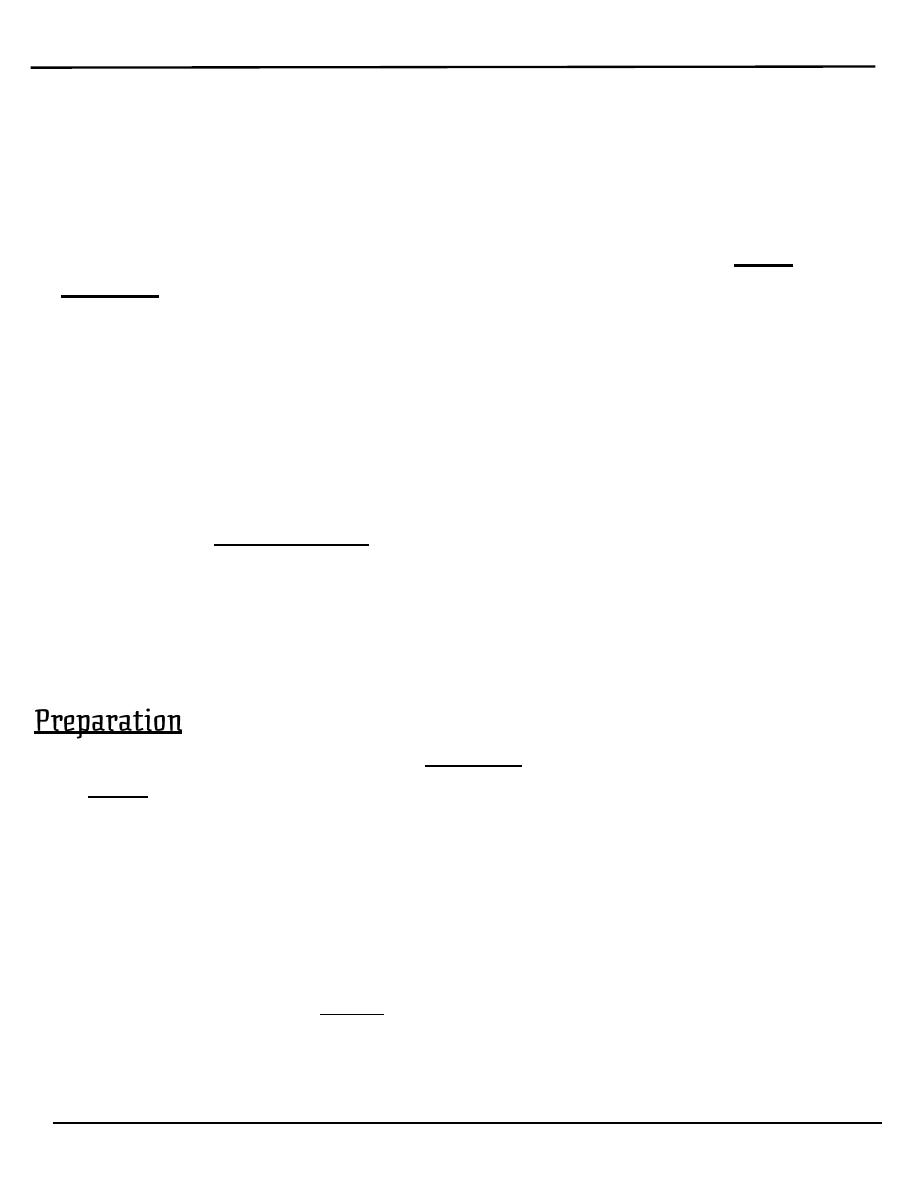
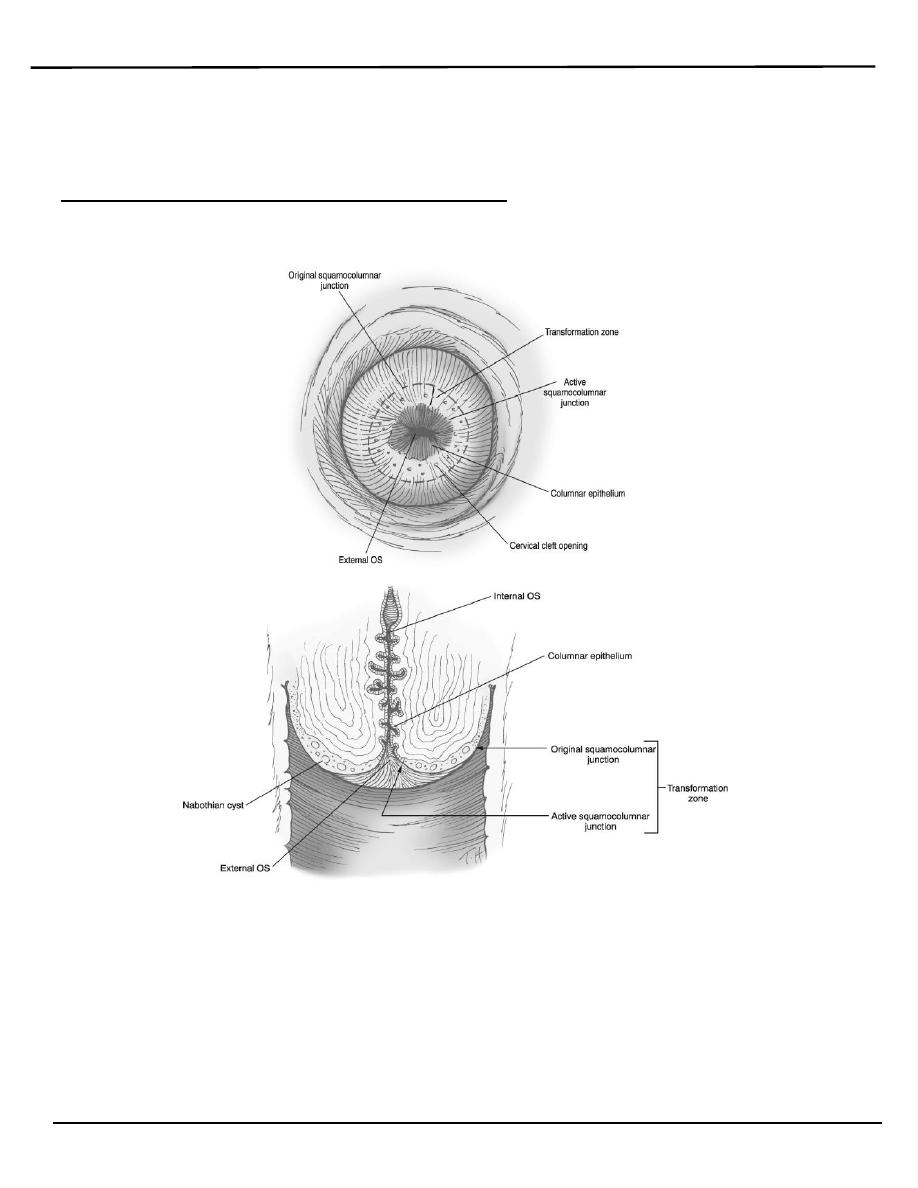
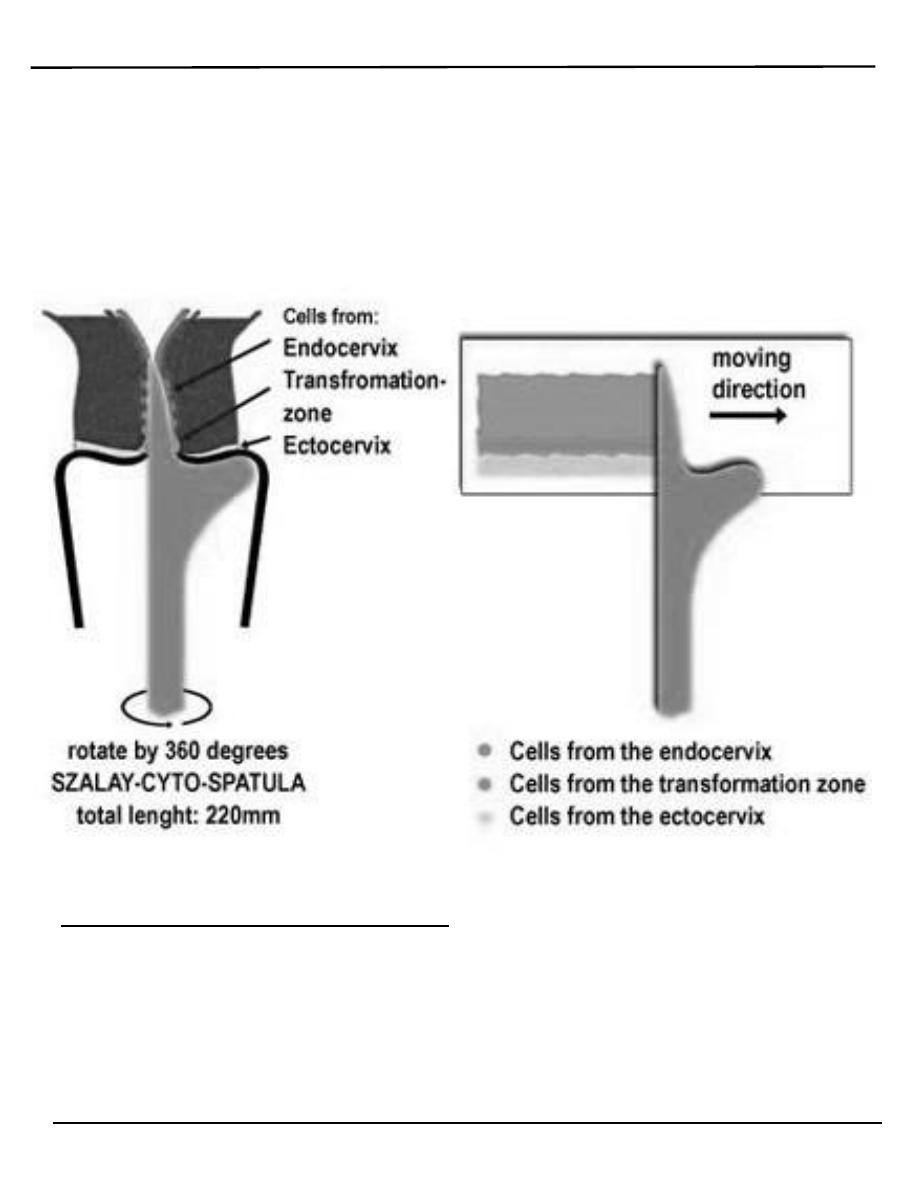
o Exfoliated cells are collected from the transformation zone of the cervix
by Use spatula of different size or brush.
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 4 of 15
There are two methods of preparing and processing cervical smear
slides.
These methods are:
1. conventional cervical (Pap) smear test.
collecting the cells smears on a microscope slide and applies a
fixative. The slide is sent to a laboratory for evaluation.
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 5 of 15
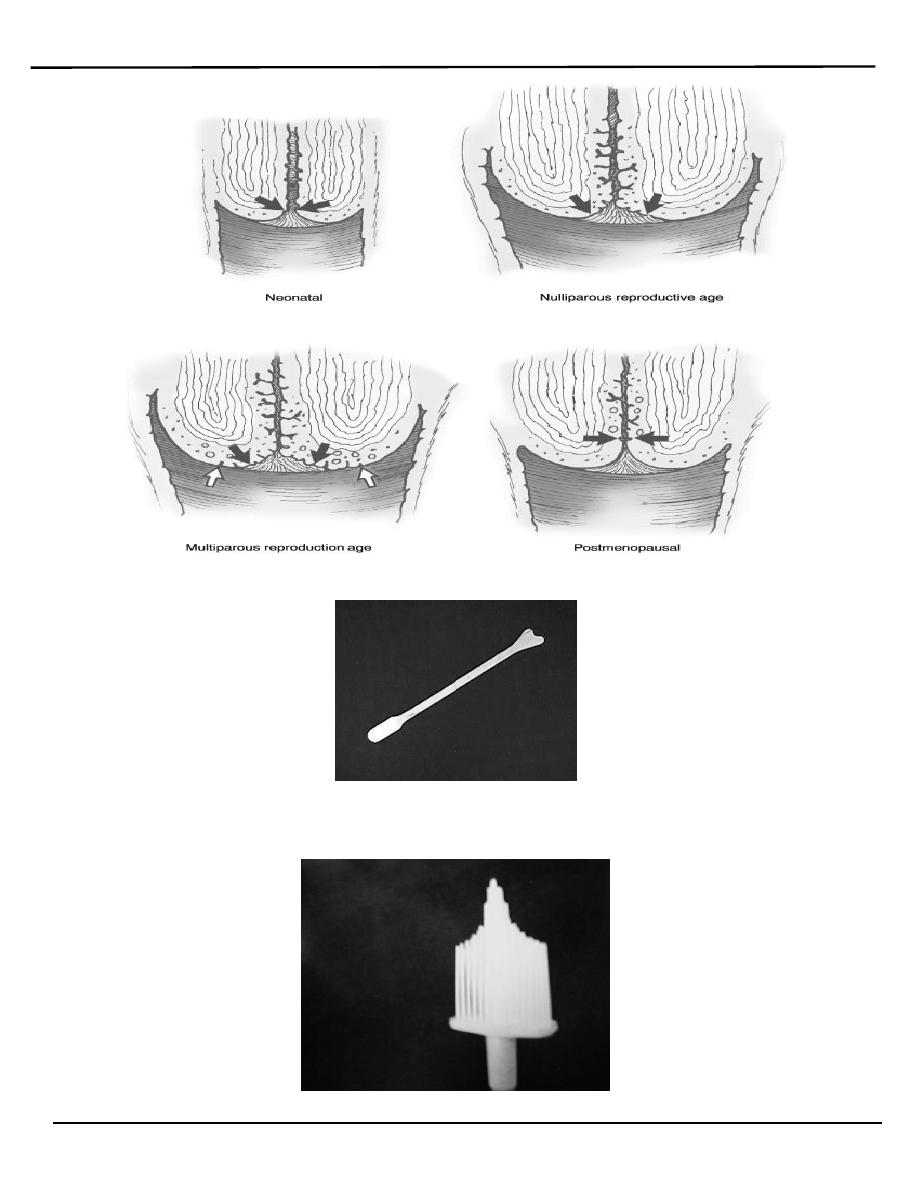
Broom type sampler
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 6 of 15
The 'tongue' of the spatula is introduced into the canal, whilst its
'shoulder' is positioned on the 3 o'clock position of the ectocervix at
the beginning of the procedure.With gentle pressure the spatula is
rotated in a clockwise direction.
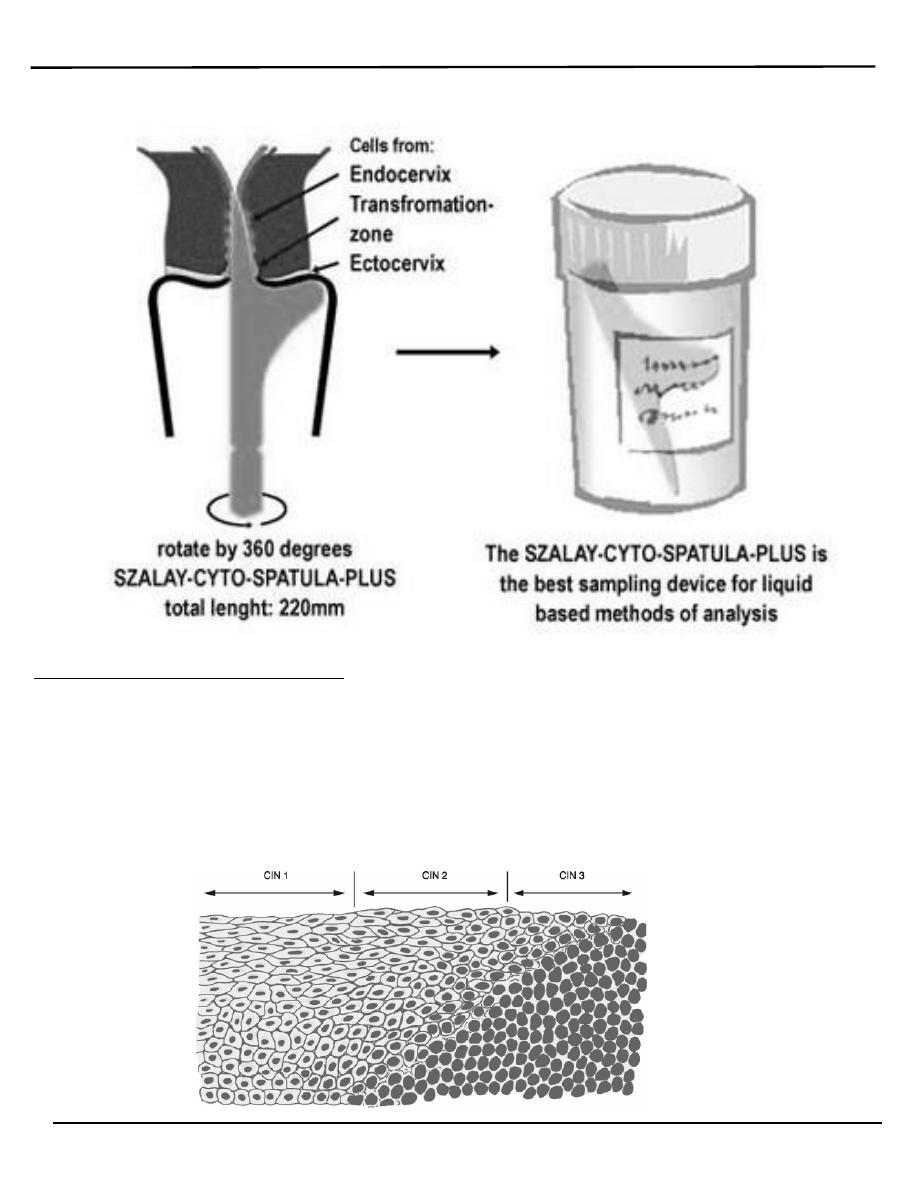
2. liquid based cytology (LBC) test.
Cell transferred to a vial of liquid preservative that is processed in
the laboratory to produce a slide for interpretation by light
microscopy.
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 7 of 15
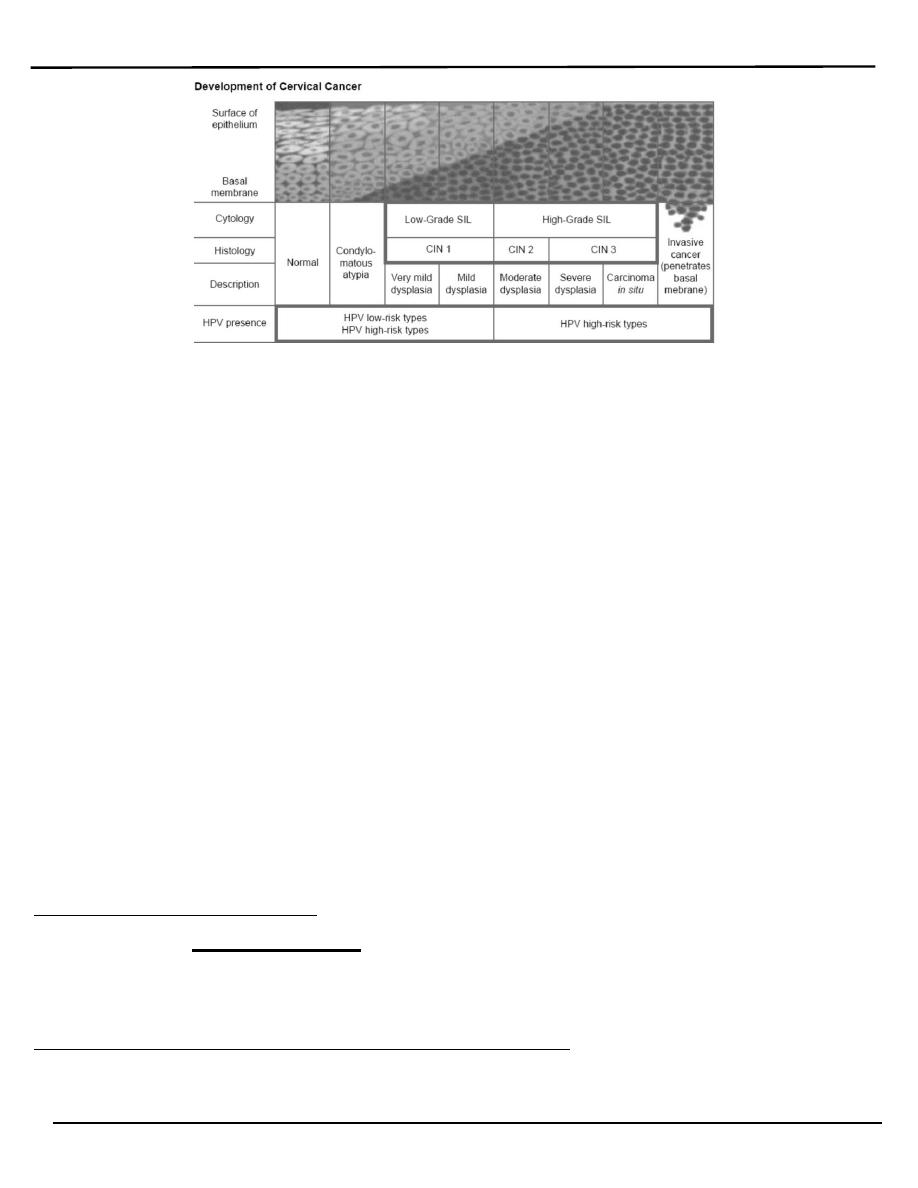
Classification of CIN
A. CIN classification
o CIN 1 (mild dysplasia) involvement of the inner one-third of the
epithelium.
o CIN 2 (moderate dysplasia) involvement of inner one-half to two-
third
o CIN 3 (severe dysplasia/carcinoma in situ) full thickness involvement.
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 8 of 15
B. Or can be classified as:
o Low grade lesions (CIN1 and HPV-associated changes) in which there
is a significant chance of regression and low progressive potential.
o High grade lesions (CIN 2 and CIN 3) are likely to behave as cancer
precursors.
A diagnosis of CIN is based primarily on the presence of nuclear atypia
and loss of normal squamous maturation (polarity).
Accurate grading of CIN lesions becomes important as we begin to
understand the rates of regression, persistence and progression of the low-
grade (CIN 1) and high-grade lesions (CIN 2 and 3), as their treatment and
clinical follow-up are quite different.
Cervical pre-cancer has along natural history.
36% of women with CIN3 would develop invasive cancer if left untreated.
More than 40% of women with minor cytological abnormalities will revert
to normal without treatment.
Clinical presentation
The disease is a symptomatic. The premalignant lesions cause no
symptoms and are not recognizable with the naked eye.
Results of the cervical smear test
The cytologist will classify the smear accordingly:
Normal results:
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 9 of 15
o Mean that no atypical, dysplastic, or cancer cells were detected, and the
cervix is normal. It is seen in About 9 in 10 routine cervical screening
tests.
o (Note: a normal result means a very low chance of developing cancer of
the cervix - not a 100% guarantee that it will not occur.)
Abnormal result:
o Some changes in the cells are found in about 1 in 10 tests. There is a range
of changes that may occur. In nearly all cases, these changes do not mean
cancer.
o Inflammatory –excessive leucocytes, candida or trichomonas.
o Borderline. (Cellular appearance that cannot be described as normal).
o Mild dysplasia
o Moderate dysplasia.
o Severe dysplasia.
o Possible invasive carcinoma. Rarely, a cancer of the cervix is diagnosed by
a cervical screening test.
Management of abnormal cervical smears
(Very Very Important, e.g Q\
A woman present to you with abnormal pap smear, discuss her management?)
o Inflammatory smears should be treated by antibiotics or antifungal
agents accordingly. And the smear repeated 3-6 months later.
o Border line smear advice to Repeat smear in 6-12 months and refer for
colposcopy if abnormalities persist.
o Ideally all women with abnormal cervical cytology(some mild ,moderate
,sever dysplasia) should have colposcopic assessment to exclude an
invasive process and to identify the extent of abnormality.
o Minor or borderline abnormal changes are quite common. These often
clear away on their own and most mild changes do not progress to
anything serious. However, any change needs to be monitored as some
may progress to become more serious in the future. A repeat test after 3-
12 months is commonly advised, depending on the type and degree of
change. Often the changes will have gone when the test is repeated. If
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 10 of 15
the changes do not go, or the changes are more marked, then a referral
to colposcopy is advised.
o Any patient with a grossly abnormal cervix should have a punch
biobsy regardless of the results of Papanicolaou smear.
Abnormal Pap Smears Treatment is based on the biopsy results.
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 11 of 15
Colposcopy:
o It is a binocular operating microscope with
o magnification of 5-20 times. Indicated for further investigation of smear
abnormalities.
o It has been used to examine the cervix in detail to:
o Identify dysplastic abnormalities on the ectocervix.
o Detect changes in the cellular pattern and vascularity of the covering
epithelium.
o Allow the accurate localization of the abnormal epithelium.
o Exclude an invasive process.
CIN has the potential to be an invasive malignancy but does not have
malignant properties.high grade lesions (CIN2 and CIN3) should be
treated, but there is some debate about CIN1 they allow CIN 1 lesions to be
treated or kept under close surveillance.
The treatment for cervical dysplasia must be individualized for each
woman, taking into account
1. the grade of the dysplasia (CIN1, CIN2, or CIN3).
2. the findings at colposcopy.
3. the woman's age.
4. reproductive status.
5. and other factors.
Treatments for CIN include:
o CIN has the potential to be an invasive malignancy but dose not have
malignant properties. high grade lesions (CIN2 and CIN3) should be
treated, but there is some debate about CIN1 as some allow CIN 1
lesions to be treated and others advice to be kept under close
surveillance..
o Treatment involves completely removing the abnormal epithelium.
o This can be done by:
1. Destroying the abnormal epithelium.( cryosurgery, laser
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 12 of 15
vaporization)
2. Excisional techniques:(This allows better
histopathological interpretation of the excised specimen).
These techniques include:
a. local excision
b. loop electrode excision procedure (LEEP).
c. cone biopsy.
d. trachelectomy (excision of cervix).
e. hysterectomy.
The success of treatment is usually defined as negative cytology 6 months
following intervention.
Therapeutic vaccination aims to boost host's cell-mediated immunity but
still experimental.
Follow up:
Follow up of patient treated for CIN is controversial between
colposcopy or cytology. other tests such as a HPV DNA test may be
advocated
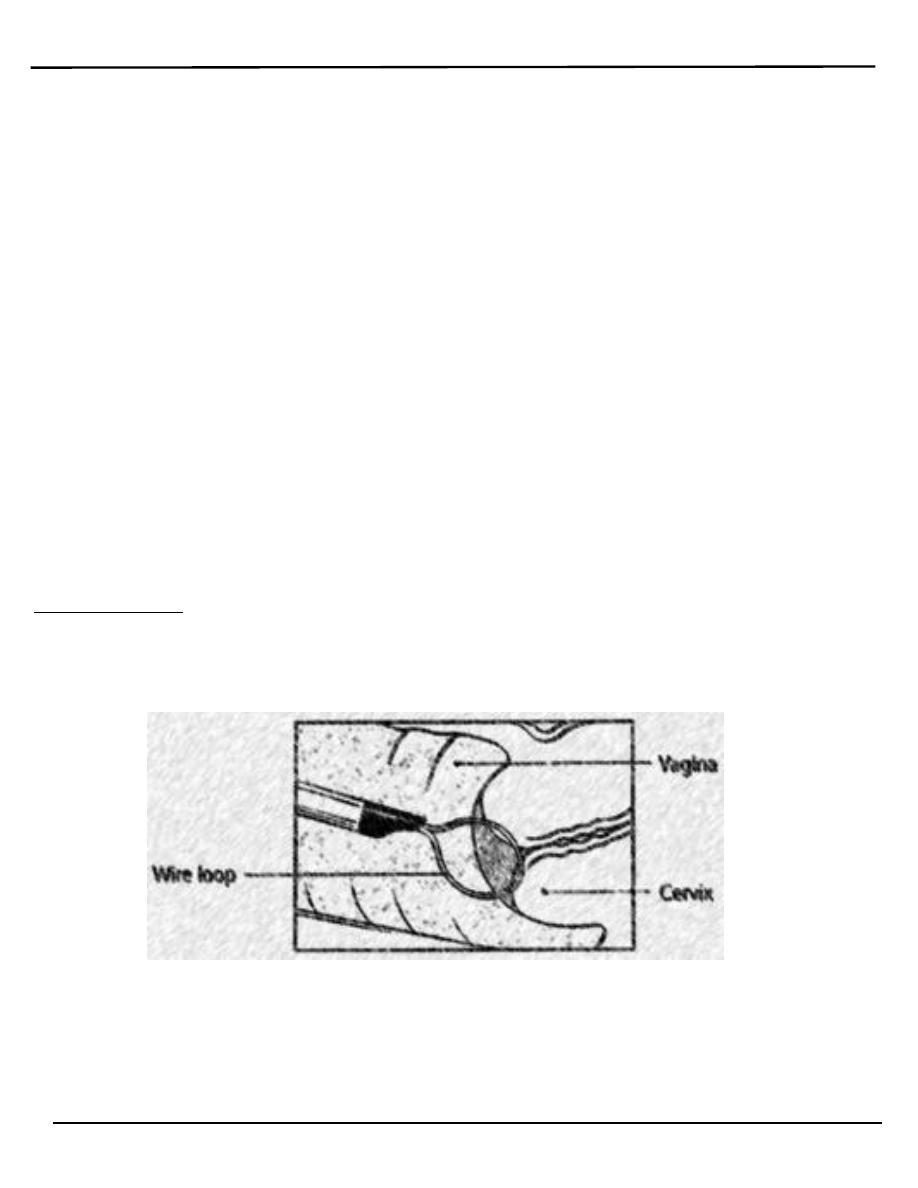
LEEP (loop electrosurgical excision procedure(. After freezing the area
with local anesthetic, an electrical wire loop is inserted into the vagina and
all the abnormal tissue is removed. This procedure is also done in the
physician's office.
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 13 of 15
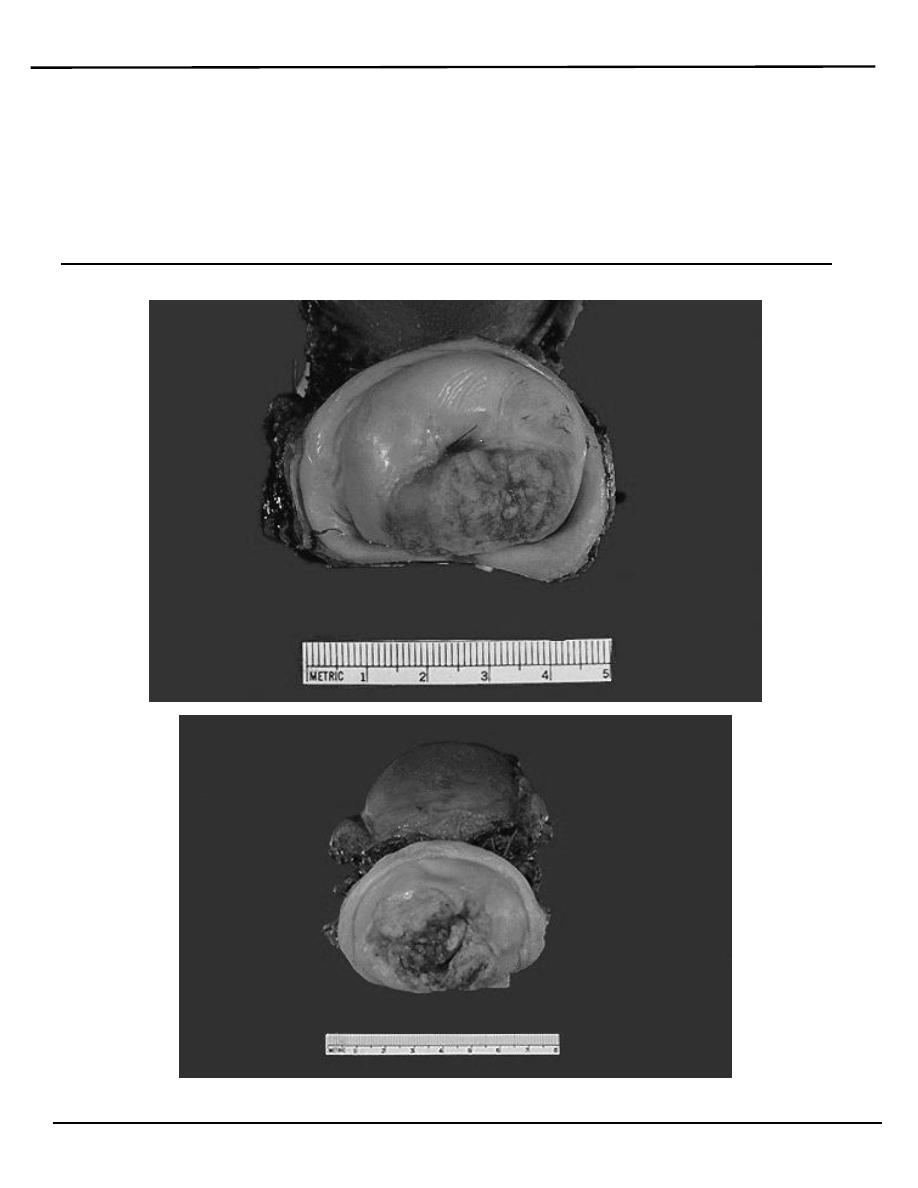
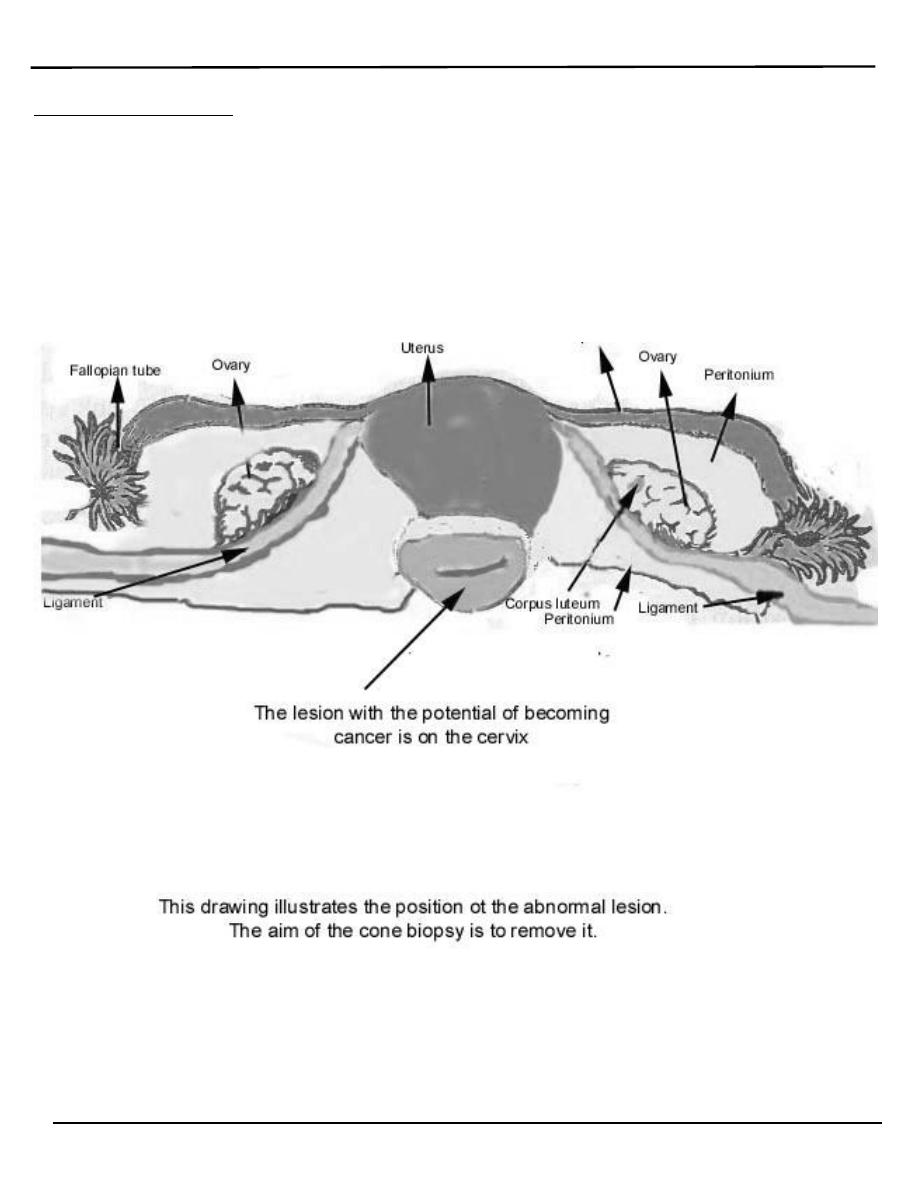
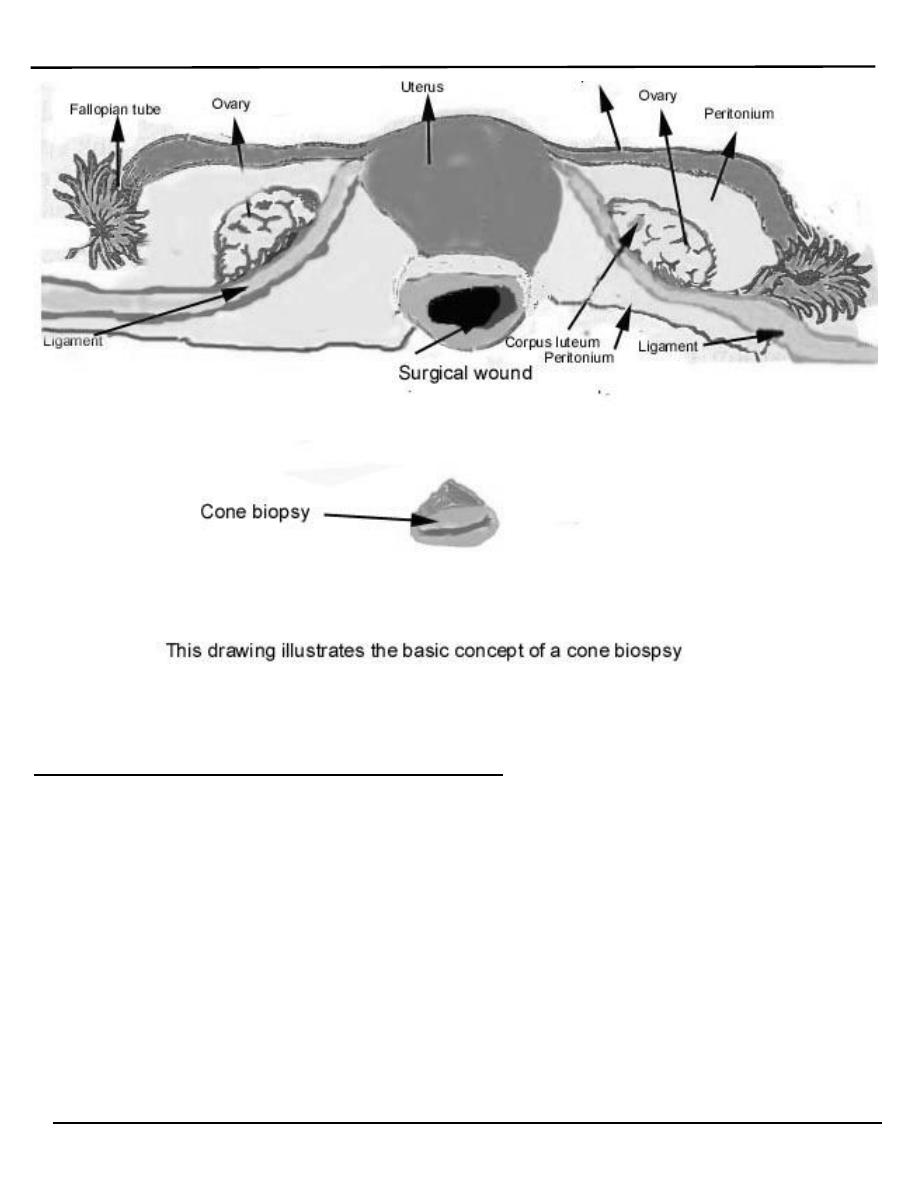
A cone biopsy
o Refers to removal of a cone-shaped piece of tissue. The tissue removed
provides a more extensive sample for diagnosis than a simple biopsy. A
cone biopsy is usually done in the operating room.
o The cold cone biopsy is a surgical procedure requiring general
anesthesia and is indicated by the presence of precancerous changes in
the cervix.
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 14 of 15
What happens after treatment?
o After treatment for dysplasia, patients are followed closely to make sure
all the dysplasia is gone, and that new dysplasia does not
occur. Typically, patients are followed with frequent Pap smears for two
years after treatment, e.g. Pap smears every 3 to 4 months for the first
year, and then every 6 months for the second year. If all the Pap smears
come back negative, the patient is be cured, and is then followed with
yearly Pap smears.
o A colposcopy-directed biopsy is a procedure in which the cervix is
examined with a colposcope for abnormalities and a tissue sample is
taken.
Lecture 3
النسائية
د. أحمد جاسم
Premalignat disease of the cervix
Page 15 of 15
Cost of Pap smear screening
1. office visit and cytopathology
2. colposcopy plus the pathology
3. cancer therapy
4. hidden costs of cancer care
5. unquantifiable cost of loss of life
Further research is needed to determine what role HPV testing should
play as part of a cervical cancer screening program.
