1
4th stage
جراحة بولية
Lec-1
د.احمد
5/10/2015
Symptomatology & Investigations
URINARY SYSTEM
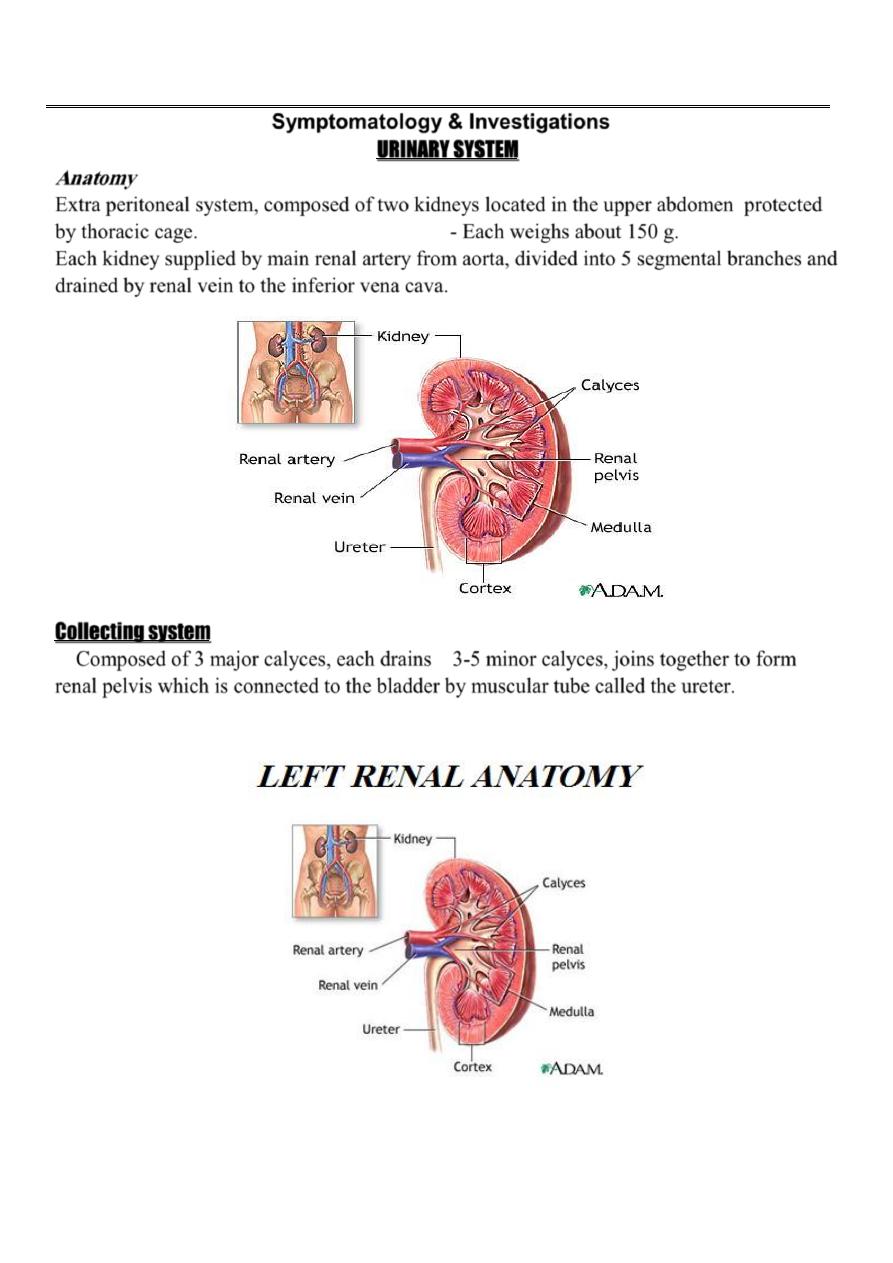
Anatomy
Extra peritoneal system, composed of two kidneys located in the upper abdomen protected
by thoracic cage. - Each weighs about 150 g.
Each kidney supplied by main renal artery from aorta, divided into 5 segmental branches and
drained by renal vein to the inferior vena cava.
Collecting system
Composed of 3 major calyces, each drains 3-5 minor calyces, joins together to form
renal pelvis which is connected to the bladder by muscular tube called the ureter.
2
3
FUNCTIONS
1- Excretion of metabolic end products.
2- Control body fluid constituents concentration.
3- Control acid base balance.
4- Hormone and enzyme
Symptomatology
The basic approach to the patient in urology is still dependent on taking a complete
History, executing a thorough Physical Examination, and performing a Urinalysis.
HISTORY
A complete history can be divided into three major components:
- The chief complaint - History of the present illness
- Past history.
Pain
Renal Pain:
Pain is usually caused by acute distention of the renal capsule, generally from
inflammation, or obstruction of minor calyx or PUJ by a stone.
-
Pain due to inflammation is usually steady Dull aching at the renal angle radiate
to the relevant hypochondrium usually associated with fever and general ill health.
Eg.: Pyelonephritis, pyonephrosis, and renal abscess.
- Pain due to obstruction is colicky &fluctuates in intensity.
Pain of renal origin may be associated with gastrointestinal symptoms like nausea
& vomiting.
4
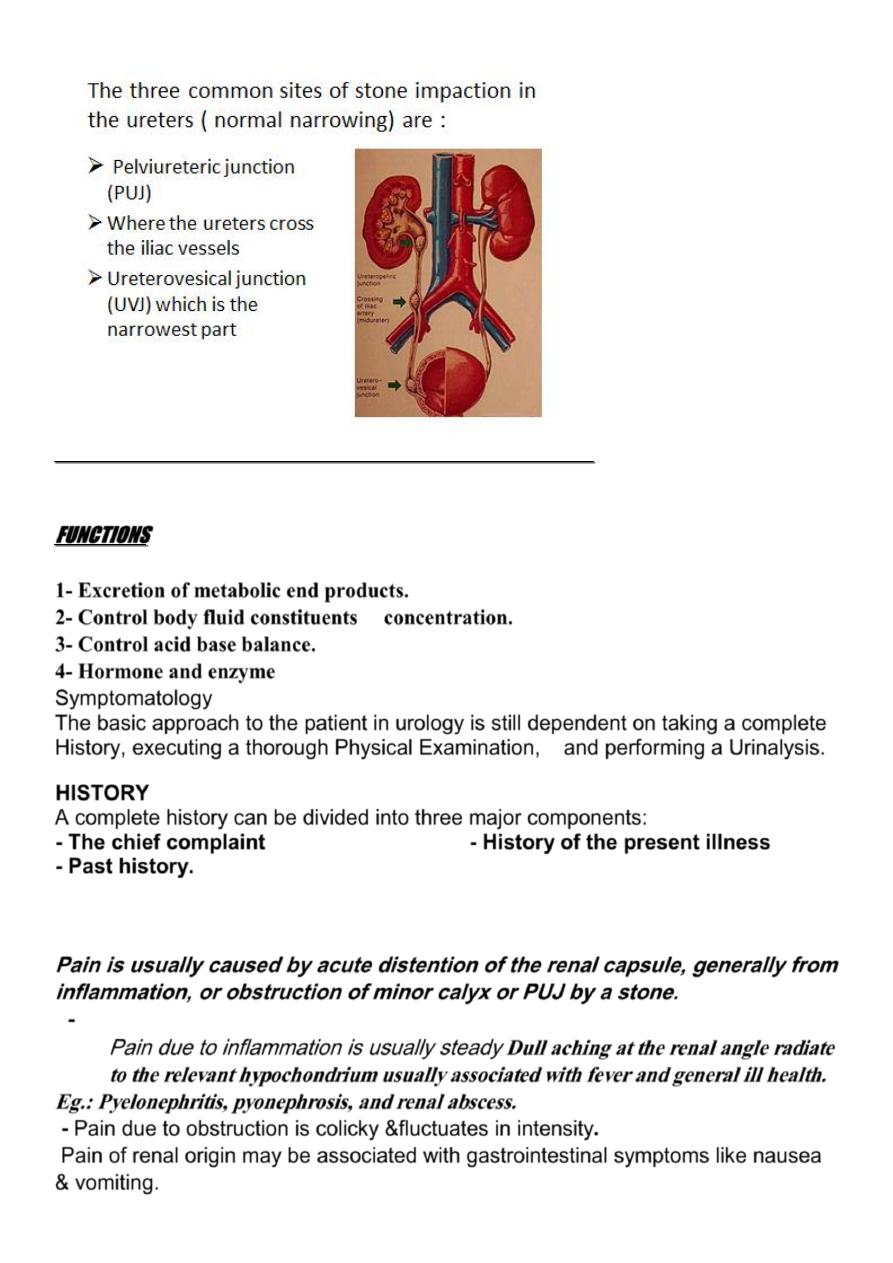
Ureteral Pain (
Ureteric Colic):
Sudden severe agonizing pain, started at the loin, radiates to the ipsilateral iliac fossa,
suprapubic region, and genitalia
Associated with nausea, vomiting, and urinary symptoms like hematuria or dysuria.
The patient is rolling around. (
Contrast this with the
patient suffering from peritoneal pain, who lies still to avoid exacerbating the pain by
movement.
)
It is ischemic pain
Usually due to acute ureteral obstruction either by stone, clot, crystals, sloughed tissue
or papillae.
The site of ureteral obstruction can often be determined by the location of the
referred pain. If the cause in the lower ureter the pain radiates to the testicle, labia or
inner aspect of the thigh.
Vesical Pain:
Suprapubic pain aggravated by vesical filling, relieved by urination.
Produced either by
overdistention of the bladder as a result of acute urinary retention
or by Bladder inflammation (cystitis)
Prostatic pain :
Usually secondary to inflammation (
Prostatitis)
with secondary edema and
distention of the prostatic capsule.
Usually felt deep in the rectum, penis, pelvis perineum, suprapubic, low backache, & both
iliac fossae.
5
Urethral pain:
Scalding in nature usually at the tip of the penis but sometimes at its base, usually due to
urethritis, cystitis or vesical or urethral calculus.
N.B.: Tumors in the GU tract usually do not cause pain unless they produce
obstruction or extend beyond the primary organ to involve adjacent nerves.
Testicular Pain
:
Primary pain arises from within the scrotum and most commonly secondary
to acute epididymo orchitis or torsion of the testicle or testicular appendices
or trauma.
Because the testicles arise embryologically in close proximity to the kidneys,
pain arising in the kidneys or retroperitoneum may be referred to the testicles.
Similarly, the dull pain associated with an inguinal hernia may be referred to the
scrotum.
Also testicular pain may by referred to the epigastric region.
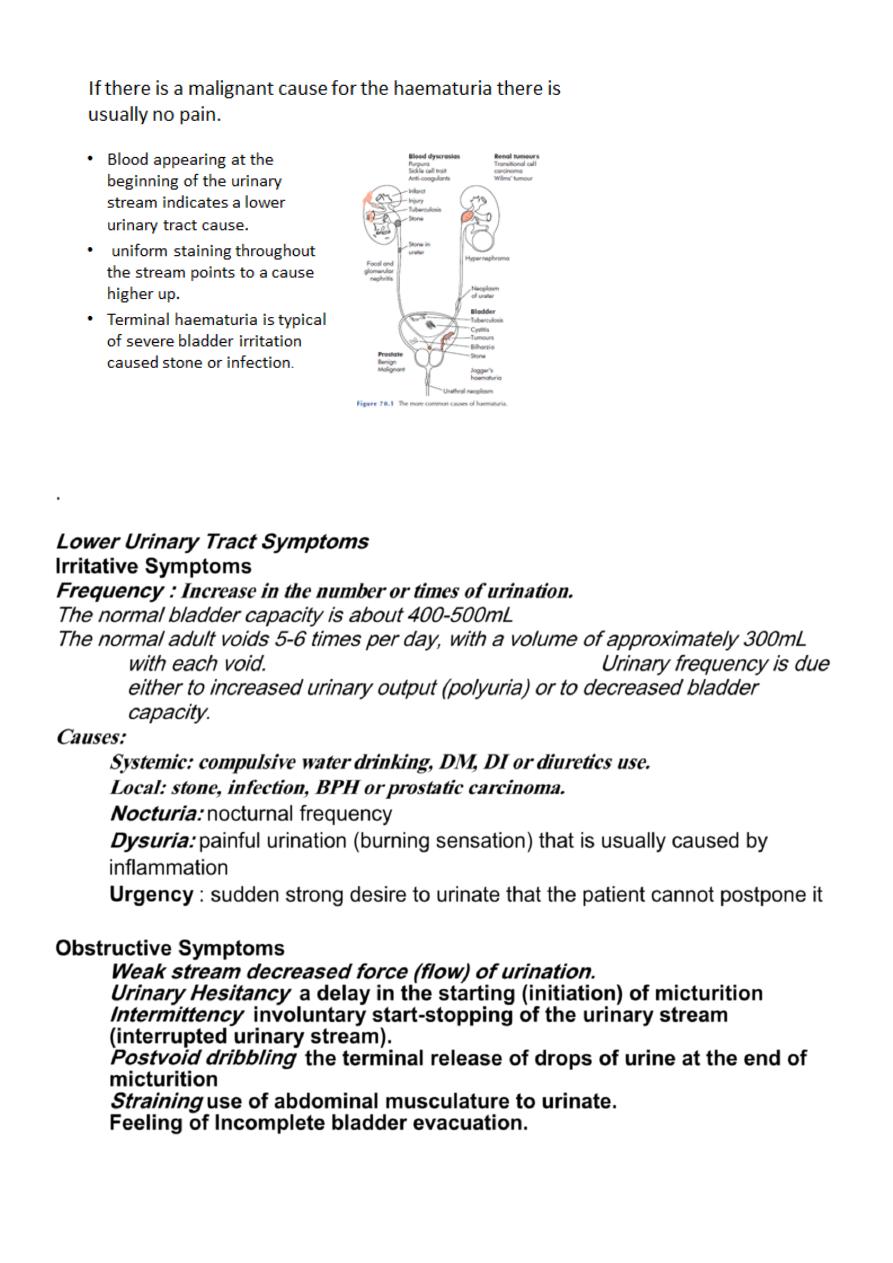
Hematuria
The presence of blood in the urine. > 3 RBC /HPF is significant.
Hematuria of any degree should never be ignored and, in adults, should be
regarded as a feature of urologic malignancy until proved otherwise.
The most common cause of gross hematuria in a patient older than age 50 years is
bladder cancer.
Important points about hematuria
-
Macroscopical or microscopical
?
-
Initial, terminal or total
?
-
Painless or painful.
?
-
Intermittent or persistent?
- If the patient is passing clots, do the clots have a specific shape ( thread like +
ureteric or renal origion)?
Causes:
- Local cause like stone, UTI, trauma, or malignancy.
- Systemic cause like bleeding tendency
6
.
Lower Urinary Tract Symptoms
Irritative Symptoms
Frequency :
Increase in the number or times of urination.
The normal bladder capacity is about 400-500mL
The normal adult voids 5-6 times per day, with a volume of approximately 300mL
with each void. Urinary frequency is due
either to increased urinary output (polyuria) or to decreased bladder
capacity.
Causes:
Systemic: compulsive water drinking, DM, DI or diuretics use.
Local: stone, infection, BPH or prostatic carcinoma.
Nocturia:
nocturnal frequency
Dysuria:
painful urination (burning sensation) that is usually caused by
inflammation
Urgency
: sudden strong desire to urinate that the patient cannot postpone it
Obstructive Symptoms
Weak stream decreased force (flow) of urination.
Urinary Hesitancy
a delay in the starting (initiation) of micturition
Intermittency
involuntary start-stopping of the urinary stream
(interrupted urinary stream).
Postvoid dribbling
the terminal release of drops of urine at the end of
micturition
Straining
use of abdominal musculature to urinate.
Feeling of Incomplete bladder evacuation.
7
Retention of urine: Inability to pass urine in spite of a full bladder ( due to outlet
obstruction).
Acute & chronic
N.B.:
Anuria: complete absence of urine production.
Oliguria is present when less than 300 ml of urine is excreted in a day
Incontinence
Involuntary loss of urine or
Inability to control urination.
1.
Continuous incontinence
.
2.
Stress incontinence
.
3.
Urgency incontinence
.
4.
Overflow urinary incontinence
Nocturnal Enuresis : Bed wetting (urinary incontinence that occurs during sleep )
Physiological during first 2-3 yr of age
Urethral Discharge
Pyuria:
presence of pus in the urine.
Chyluria:
presence of lymph in the urine.
Phosphaturia:
presence of phosphate crystals
in the urine.
Necroturia:
presence of necrotic tissue in the urine as in malignancy.
Pneumaturia:
presence of air in the urine.
Past History
Past Medical History
Past
Surgical
History
Family History
Smoking and Alcohol Use
Allergies
PHYSICAL EXAMINATION
With the exception of:
•
renal and scrotal masses or tenderness.
•
palpable bladder
•
abnormal prostate on digital rectal examination.
urological conditions are most likely to be diagnosed from the history or by
investigations.
8
Scrotal examination
A firm or hard painless mass within the testis should be considered a malignant
tumor until proved otherwise.
Transillumination is helpful in diagnosing hydrocele.
Prostate Examination:
Digital rectal examination (DRE) should be performed in every male after age 40
years and in men of any age who present for urologic evaluation.
Normally, the prostate is about the size of a chestnut and has a firm consistency
similar to that of the contracted thenar eminence of the thumb.
Pelvic Examination in the Female
Investigations
I-
URINALYSIS (
General urine examination: GUE)
complete urinalysis includes physical, chemical, and microscopic analyses.
Physical: color, pH, & Specific Gravity
Color
: yellowish
Turbidity
:phosphaturia , Pyuria
Specific Gravity and Osmolality :
Specific Gravity
usually varies from 1.003 to 1.030.
Osmolality is a measure of the amount of material dissolved in the urine and
usually varies between 50 and 1200 mOsm/L.
pH
the average pH varies between 5.5 and 6.5
Biochemical Examination of Urine
The abnormal substances commonly tested for with a dipstick include (1)
Hemoglobin, (2) protein, (3) glucose, (4) ketones, (5) Electrolytes, (6) myoglobin
, and (7) urobilinogen and bilirubin.
9
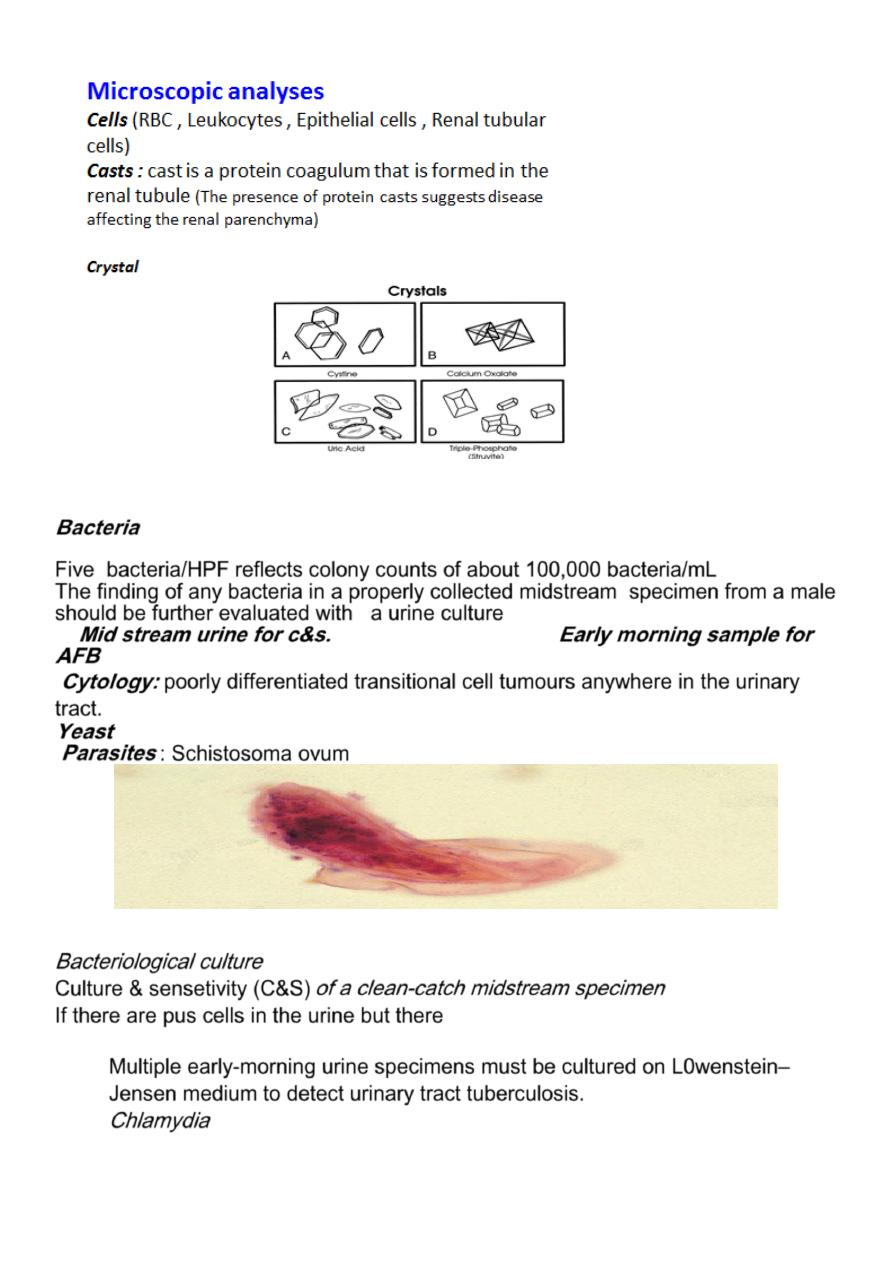
Bacteria
Five bacteria/HPF reflects colony counts of about 100,000 bacteria/mL
The finding of any bacteria in a properly collected midstream specimen from a male
should be further evaluated with a urine culture
Mid stream urine for c&s. Early morning sample for
AFB
Cytology:
poorly differentiated transitional cell tumours anywhere in the urinary
tract.
Yeast
Parasites
: Schistosoma ovum
Bacteriological culture
Culture & sensetivity (C&S)
of a clean-catch midstream specimen
is no growth on the routine culture media
If there are pus cells in the urine but there
(sterile pyuria), it is worth testing for more fastidious organisms.
- Multiple early-morning urine specimens must be cultured on L0wenstein–
Jensen medium to detect urinary tract tuberculosis.
-
Chlamydia
11
Analysis of a 24-hour specimen of urine
Quantify the rate of loss, and is especially useful in the investigation of calculus
disease caused by abnormal excretion of calcium, oxalate, uric acid and other
products of metabolism
II- Renal function tests:
More than 70% of kidney function must be lost before renal failure becomes evident
(
Because of large renal reserve, considerable structural damage can occur before
functional damage become apparent).
1- Blood urea (Blood Urea Nitrogen)normally (15-
40 mg/dl) (2.5-6.5 mmol/l)
It increases in dehydration, fasting, fever & after protein meal. Also in renal
failure
2- Serum creatinine: (0.6-1.2 mg/dl)
( 62-124
µ
mol/l)
More accurate than urea and less affected by dehydration.
3- Creatinine clearance: (85-120 ml/min)
Creatinine clearance test will give an approximate value for glomerular filtration rate
Needs 24h urine collection and a sample of blood. Cr. CL.=UV/P
U : Cr. in urine (mg/dl)
V: ml of urine excreted (per minute or 24hour)
P: Cr. in plasma (mg/dl)
III- Tubular function tests:
1- Specific gravity: (1.003-1.030).
2- Ion excretion test: Na
+
β2-microglobulin
URINARY TRACT IMAGING
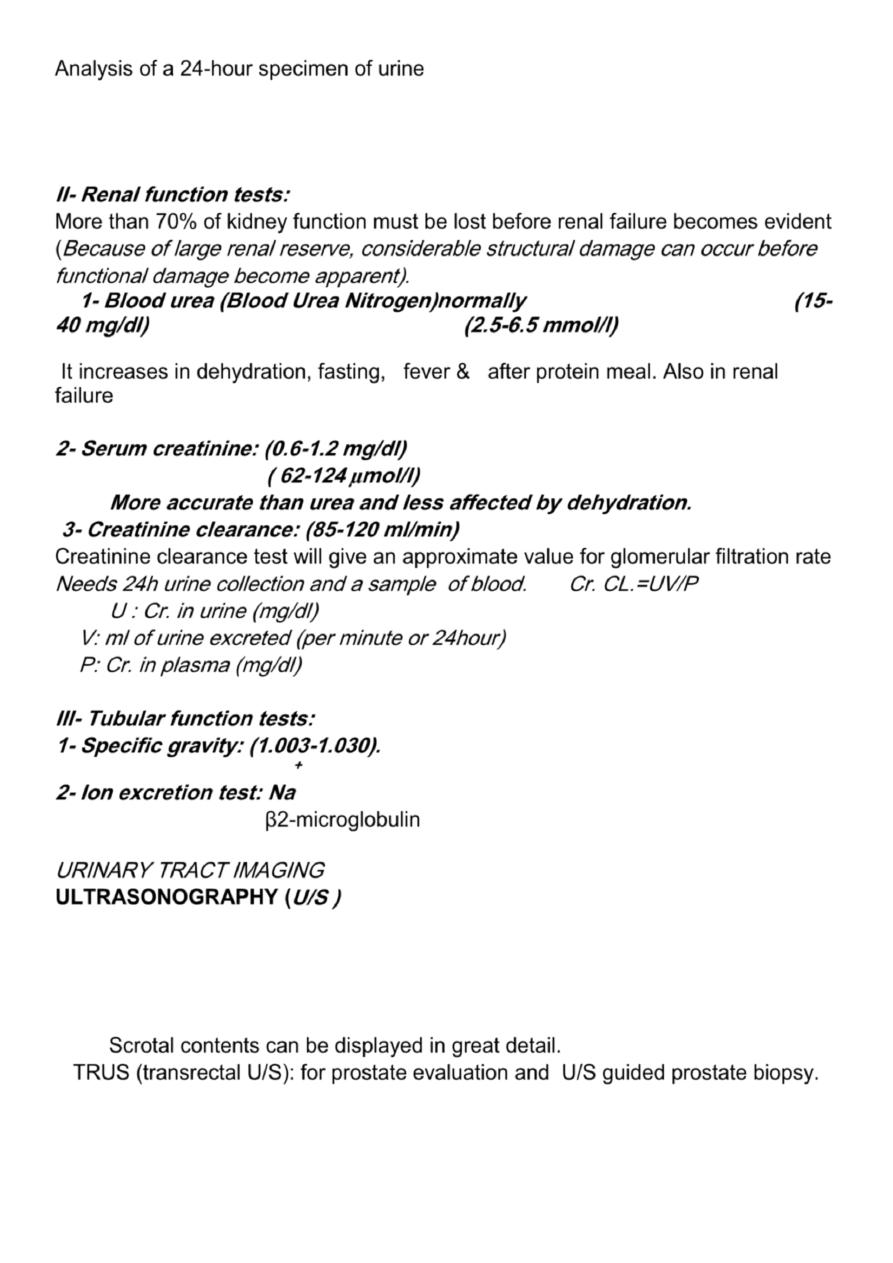
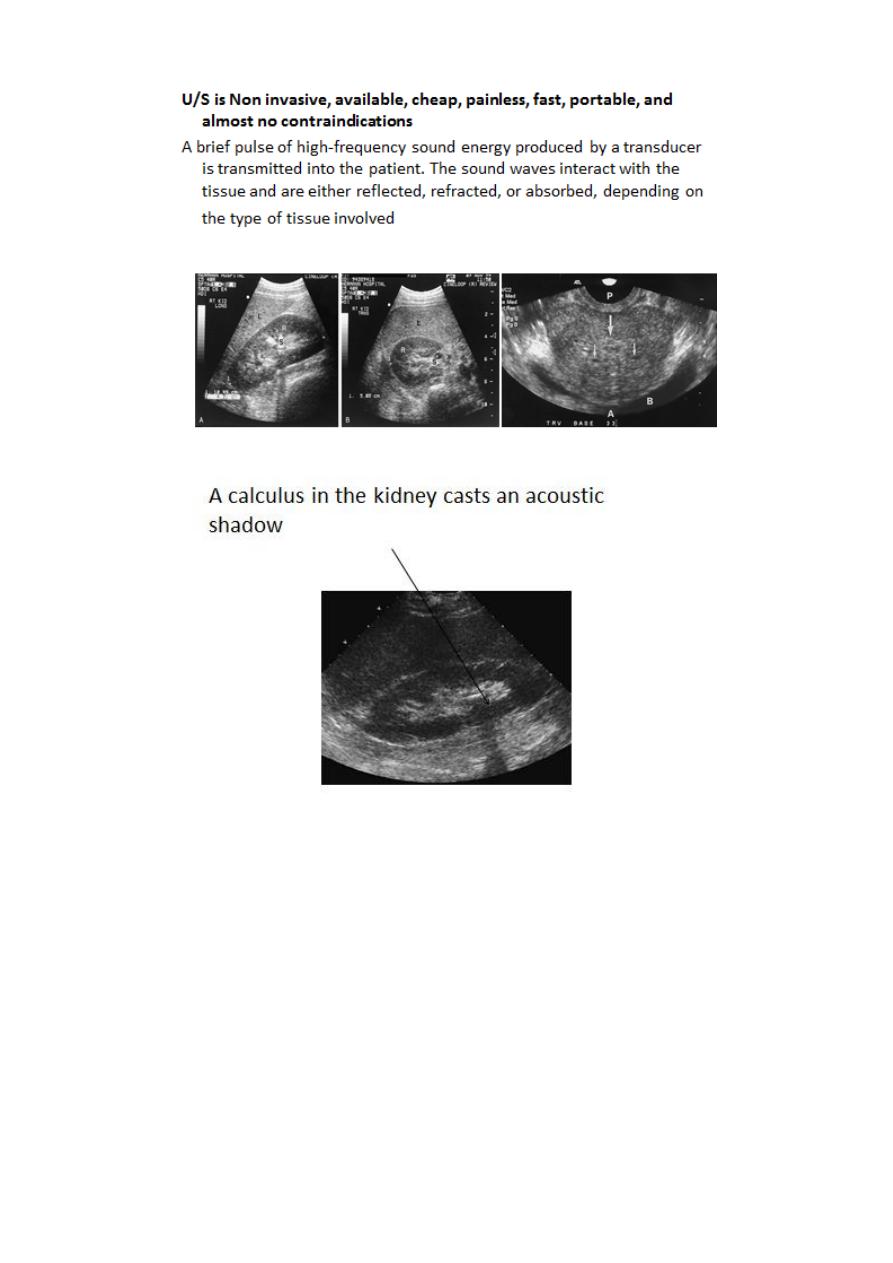
ULTRASONOGRAPHY (
U/S )
Structural study to differentiate cystic or solid masses, hydronephrosis,
renal size, renal cortical thickness, and stones.
The volume of urine in the bladder before and after micturition can be
calculated, and even tiny filling defects within it detected.
The prostate
Scrotal contents can be displayed in great detail.
TRUS (transrectal U/S): for prostate evaluation and U/S guided prostate biopsy.
11
12
X-Ray: KUB
(kidneys, ureters, bladder)
A plain radiograph of the abdomen and pelvis includes the area above both adrenal
glands (lower chest) and extends to 2 cm below the symphysis pubis(includes the
external genitalia)
site, sex, stones, psoas shadow, skeleton, and soft tissue shadow.
Indications
1) as a primary study
2) as a scout film before contrast material injection

13
14
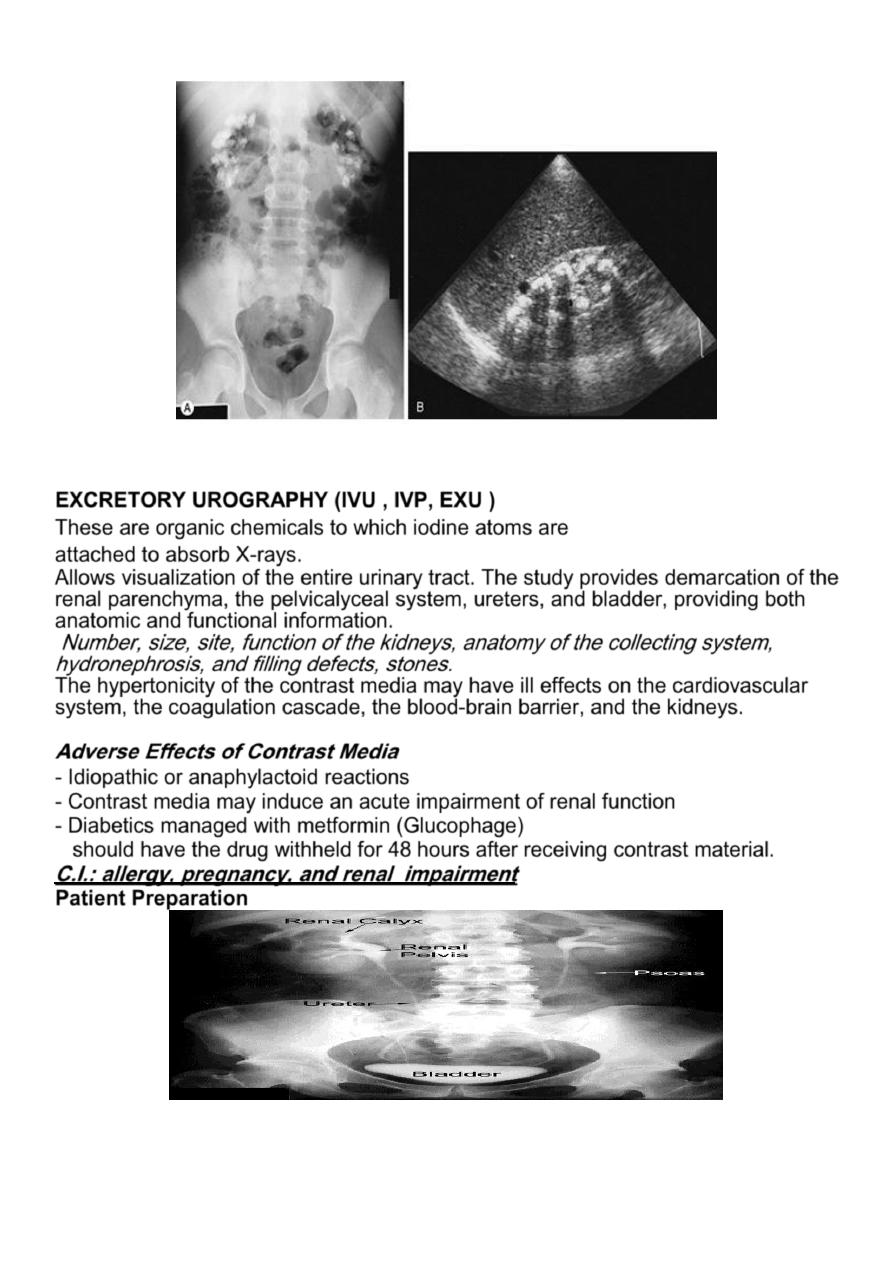
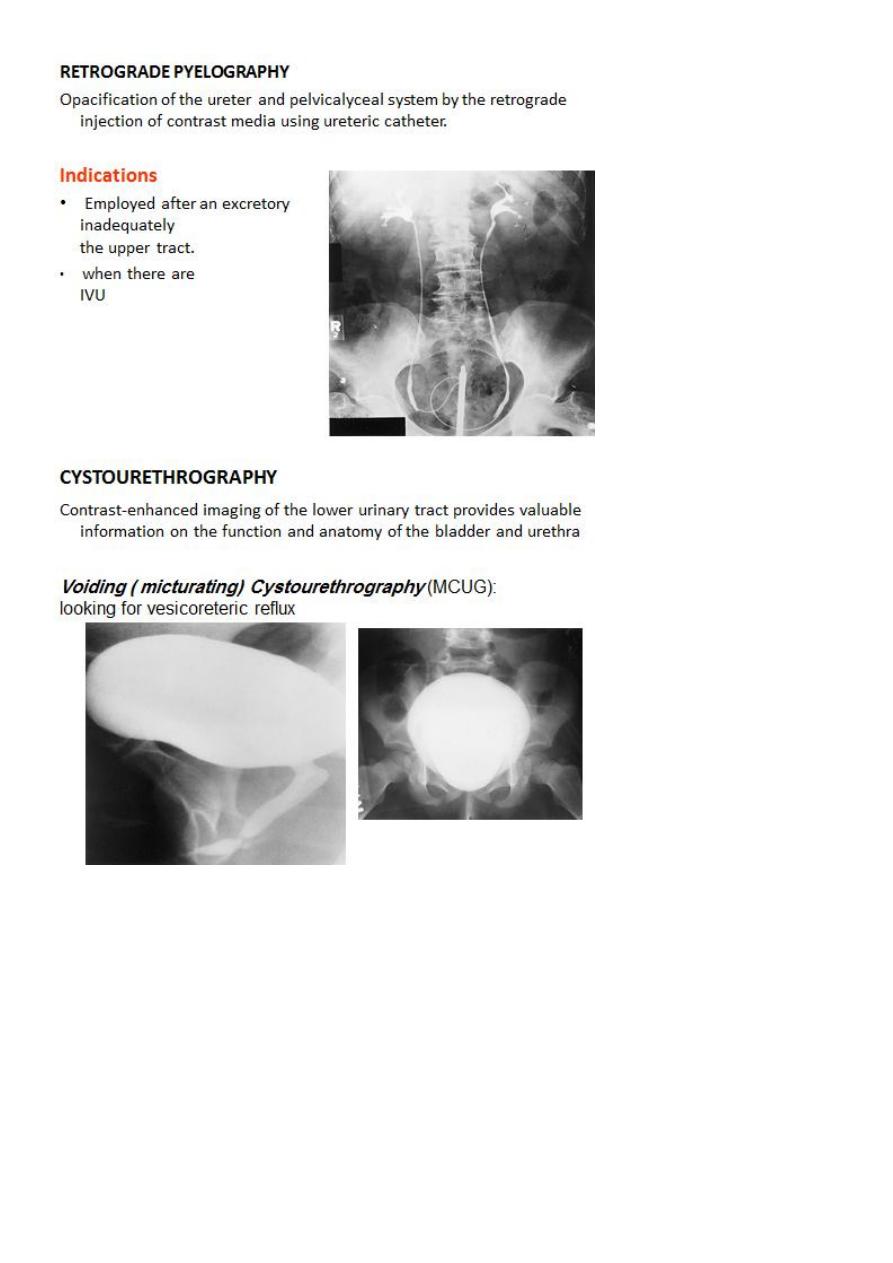
EXCRETORY UROGRAPHY (IVU , IVP, EXU )
These are organic chemicals to which iodine atoms are
attached to absorb X-rays.
Allows visualization of the entire urinary tract. The study provides demarcation of the
renal parenchyma, the pelvicalyceal system, ureters, and bladder, providing both
anatomic and functional information.
Number, size, site, function of the kidneys, anatomy of the collecting system,
hydronephrosis, and filling defects, stones.
The hypertonicity of the contrast media may have ill effects on the cardiovascular
system, the coagulation cascade, the blood-brain barrier, and the kidneys.
Adverse Effects of Contrast Media
- Idiopathic or anaphylactoid reactions
- Contrast media may induce an acute impairment of renal function
- Diabetics managed with metformin (Glucophage)
should have the drug withheld for 48 hours after receiving contrast material.
C.I.: allergy, pregnancy, and renal impairment
Patient Preparation
15

16
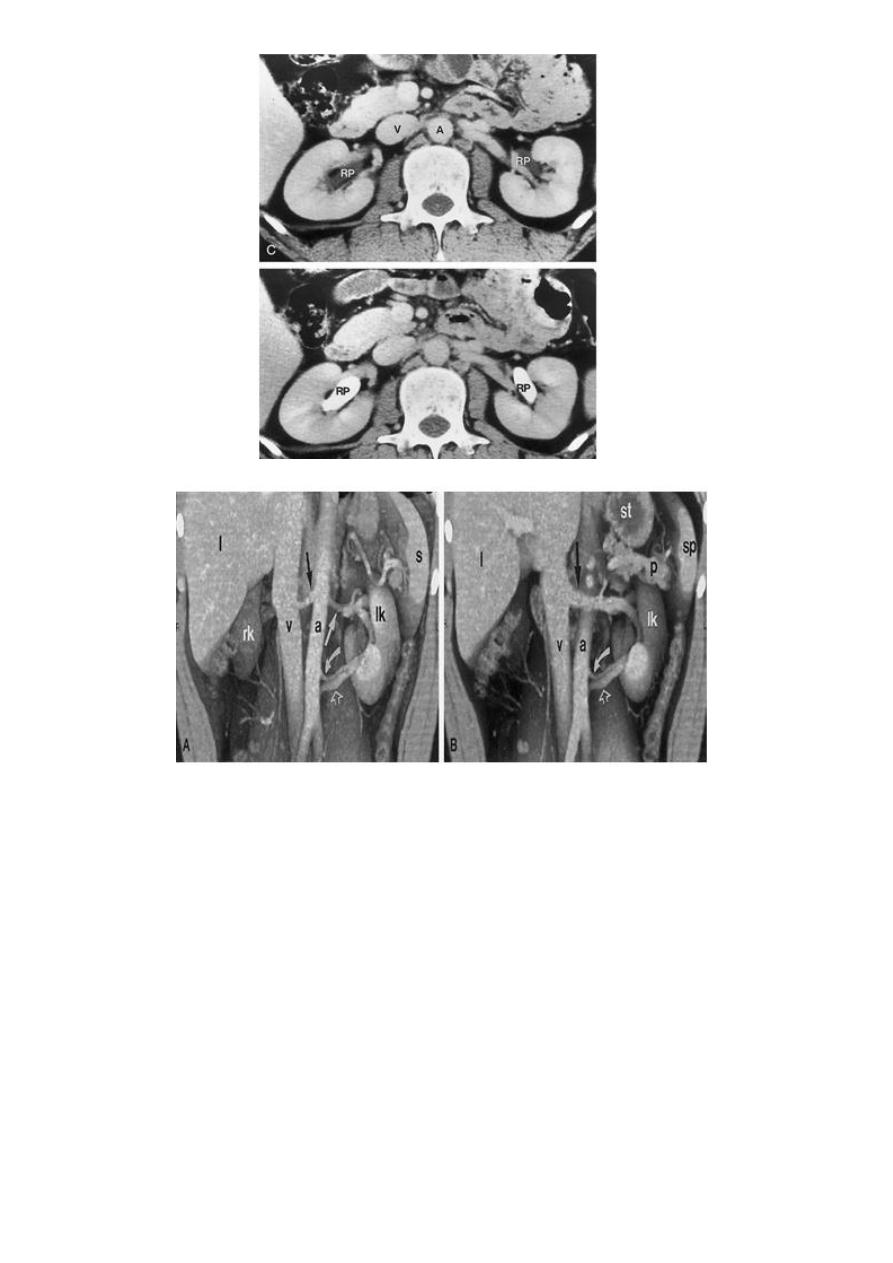
COMPUTED TOMOGRAPHY ( CT scan)
Non Contrasted (Native, non enhanced)
Contrasted: Oral Contrast Agents
Intravenous Contrast Agents
CT scan accurately characterize the nature of tissue in the lesion.
CT is useful in the preoperative evaluation and staging of tumors.
CT has replaced IV urography as the primary modality for the assessment of
suspected renal injuries and their complications
For the evaluation of patients with acute flank pain, unenhanced spiral CT is more
sensitive in detecting calculi than EXU. (except indinaver no radiolucent stones).
Drawbacks: Expensive, more radiation, not always available, need experience,
contrast contraindications, pregnancy
17
18
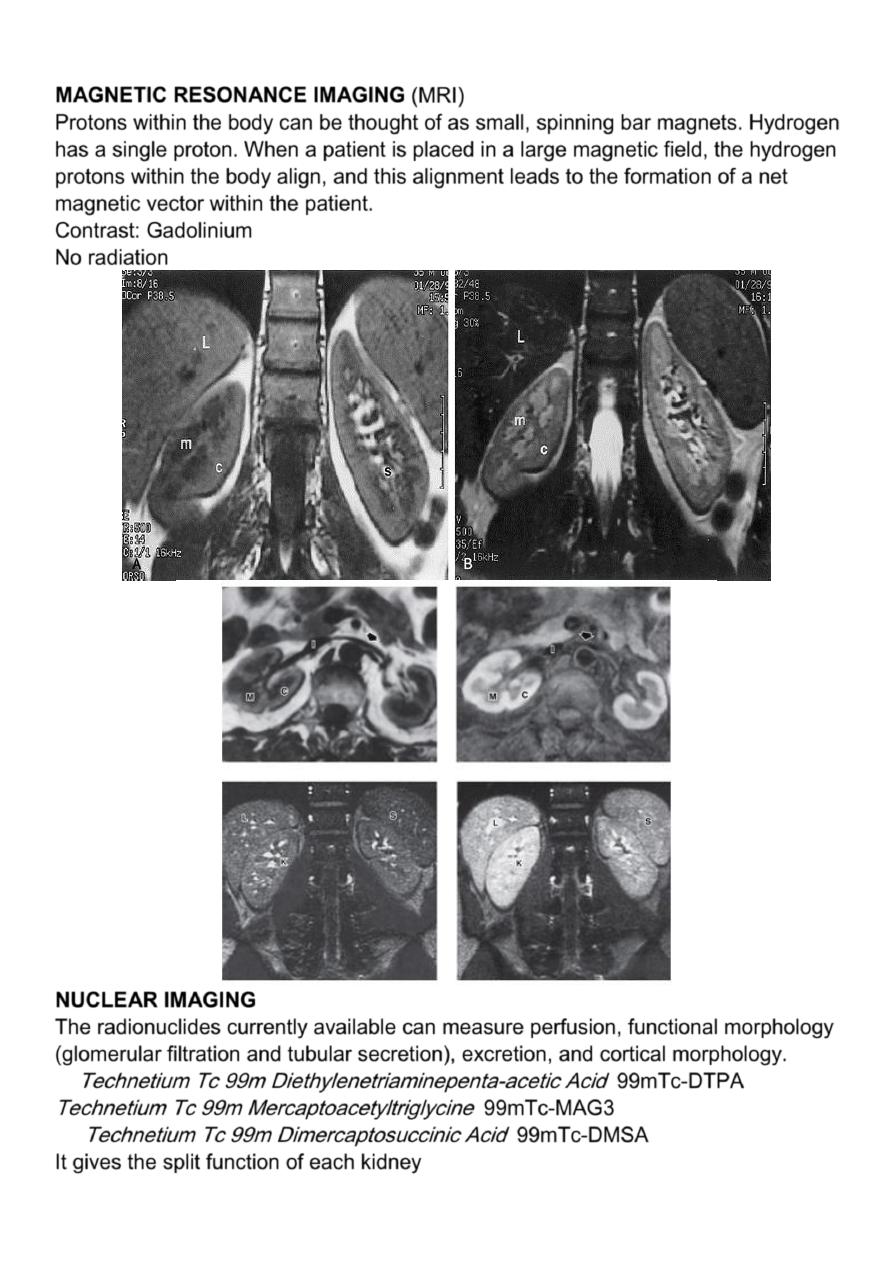
MAGNETIC RESONANCE IMAGING
(MRI)
Protons within the body can be thought of as small, spinning bar magnets. Hydrogen
has a single proton. When a patient is placed in a large magnetic field, the hydrogen
protons within the body align, and this alignment leads to the formation of a net
magnetic vector within the patient.
Contrast: Gadolinium
No radiation
NUCLEAR IMAGING
The radionuclides currently available can measure perfusion, functional morphology
(glomerular filtration and tubular secretion), excretion, and cortical morphology.
Technetium Tc 99m Diethylenetriaminepenta-acetic Acid
99mTc-DTPA
Technetium Tc 99m Mercaptoacetyltriglycine
99mTc-MAG3
Technetium Tc 99m Dimercaptosuccinic Acid
99mTc-DMSA
It gives the split function of each kidney
19
Endoscopy:
Direct visualization of the internal parts of the organ. Urethroscope, Cystoscope,
Ureteroscope and Renoscope.
Urodynamic studies:
To study the function of the lower urinary tract( vesico-urethral unit).
Include cystometry, flow rate, urethral pressure profile, video urodynamic studies,
and EMG of pelvic floor.
