Cutaneous Drug
Reactions
Dr. Ammar AL-Faisal
Overview
• The skin is one of the most common targets for
adverse drug reactions
• Most cases are mild, causing pruritus, resolving upon
drug withdrawal.
• Others are life threatening ex: toxic epidermal
necrolysis (TEN).
• The most commonly offending drugs are: penicillins,
sulfonamides, and NSAIDs
• But any drug, potentially can cause adverse
cutaneous reaction.
Pathogenesis
1. Immunologic mechanism:
•
Type I (IgE-dependent)
– Urticaria, Angioedema.ex: penicillin.
•
Type II (Cytotoxic)
– Petechiae (2
o
to drug-induced thrombocytopenia),ex:sulfonamide.
•
Type III (Immune complex)
– Vasculitis, Serum sickness, Ex: Infliximab.
•
Type IV (Delayed cell-mediated)
– SJS/TEN, Ex : anticonvalescents.
Pathogenesis
2- Non-immunological:
3- Idiosyncratic: SJS/TEN.
4-
May involve a combination of immunologic
interactions and genetic predisposition.
Diagnosis
• Most immunologically mediated drug reactions occur within
7-21 days after initiation of a new medication.
• Exclude other causes of such reaction especially infections.
• Clinical characteristics
• Chronological factors
– Time between drug introduction and rash.
– Response to removal of suspected agent.
– Previous history of such reaction due to the same medication.
– Challenge test ( reaction on re-administration, not practical).
Exanthematous reaction
• Perhaps the most common adverse effects of
medications.
• Morbilliform (measles-like).
• The most common cause is antibiotics ex: penicillin.
• Generalized symmetical distribution of confluent
erythematous macules
• usually accompanied by pruritus (important feature to differentiate
from viral exanthema which is typically not itchy).
Exanthematous
• Rash disappears spontaneously after 1 to 2 weeks
without sequelae
• Ddx: viral exanthems
• Tx: supportive
– Topical steroids and antihistamines.
– Discontinue the offending agent .

Exanthematous
Urticaria and Angioedema
• IgE-mediated immediate hypersensitivity
reaction
• Antigen binds to IgE on the surface of mast
cells
– Induces degranulation and histamine release
Urticaria
• Transient erythematous, edematous papules
and plaques (wheals).
• Associated with severe pruritus.
• Lesions can occur anywhere on the body
Urticaria
• Most common agents: Antibiotics; penicillins,
cephalosporins, sulfonamides, tetracyclines
• Tx:
– Withdrawal of causative agent
– H1 antihistamines.
– Sometimes short course of systemic steroid.

Urticaria
Angioedema
• Edema of the deep dermis, subcutis, and
submucosal tissues.
• Presents as swelling (usually not itchy)
– Usually involves the mucocutaneous junctions
( face:lips and eyelids, genetilia), sometimes
causing dangerous laryngeal edema.
• Most commonly due to ACE inhibitors
– Can also be caused by penicillins, and
radiographic contrast media

Angioedema
Phototoxicity
• Direct interaction of UV radiations with the drug
• ( topical or systemic) in the skin.
• Limited to sun-exposed areas
– Appears as exaggerated sunburn
• Most commonly due to tetracyclines.

Phototoxicity
Fixed drug eruption
• Presents as one or a few round, sharply
demarcated, erythematous to dusky plaques.
• Usually recurrent, occur at the same sites which
previously affected (fixed).
• Typical causative example is sulfonamides.
• Common locations: genitalia, face, hands/feet,
Resolves with postinflamatory hyperpigmentation
• Upon rechallenge, lesions recur at the same sites

Fixed drug eruption
• Caused by: sulfonamides, NSAIDs, tetracyclines
Drug-induced diseases
• Bullous pemphigoid :
furosemide
• Pemphigus :
penicillamine.
• Acneform eruption : topical or systemic steroids
• Lupus erythematosus. Ex:hydralazine
• Psoriasis ex:antimalarial.
• Lichenoid (lichen planus like):chloroquine
Erythema Multiforme
• Hypersensitivity reaction to drugs (ex:
sulfonamides) or herpes simplex infection.
• Iris (target) lesions is characteristic feature
• Usually on palms and sole.
• May be mild (EM minor):classic target,
recurrent, no mucosal involvement.
• EM major: severe with systemic
symptoms(fever),marked mucosal
involvement, symptomatic treatment.

Erythema Multiforme -target lesions
SJS/TEN
• Stevens-Johnson Syndrome (SJS) and Toxic
Epidermal Necrolysis (TEN) are rare, life-
threatening mucocutaneous diseases
– Almost always drug-related
• Extensive erythema and exfoliation
– Due to keratinocyte cell death via apoptosis (separation of
skin at the dermo-epidermal junction
• High fever and skin pain and tenderness.
SJS/TEN
• Onset between 7-21 days after initiation of
drug therapy
• Mortality rate: 1-5% for SJS; 25-30% for TEN
SJS/TEN
• Most frequently implicated drugs:
sulfonamides, NSAIDs, anticonvulsants
(carbamazepine)
• Classified based on body surface area (BSA)
– SJS: <10% of BSA
– SJS-TEN overlap: 10-30% of BSA
– TEN: >30% of BSA
SJS/TEN
• Clinical features:
– symptoms due to mucosal involvement: pain of oral
cavity and the eyes, dysuria, dysphagia
– Skin lesions generalized,
erythematous to dusky red
macules and patches
• As epidermis detaches from dermis, blisters form
• Positive Nikolsky sign
• Atypical target lesion is common
– Skin is very painful
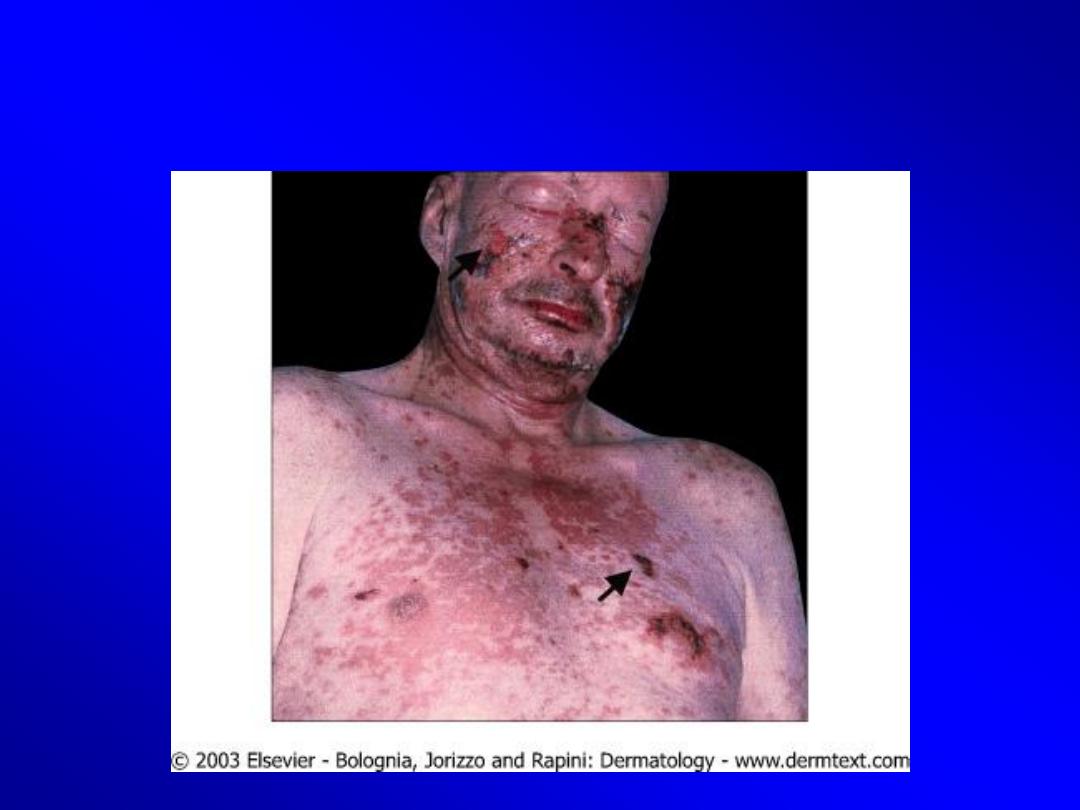
SJS/TEN

SJS/TEN

SJS/TEN
• Erythema and erosions of the buccal, ocular, and
genital mucosa
SJS/TEN
• Treatment:
• It is a dermatological emergency.
• Admission (ICU, or burn unit)
– Immediate discontinuation of the causative drug
– Supportive care
– Systemic corticosteroids or. IVIG (intravenous immunoglobulin)



