
Injuries of upper arm and elbow
Dr. AMMAR TALIB AL-YASSIRI
COLLEGE OF MEDICINE/ BAGHDAD
UNIVERSITY

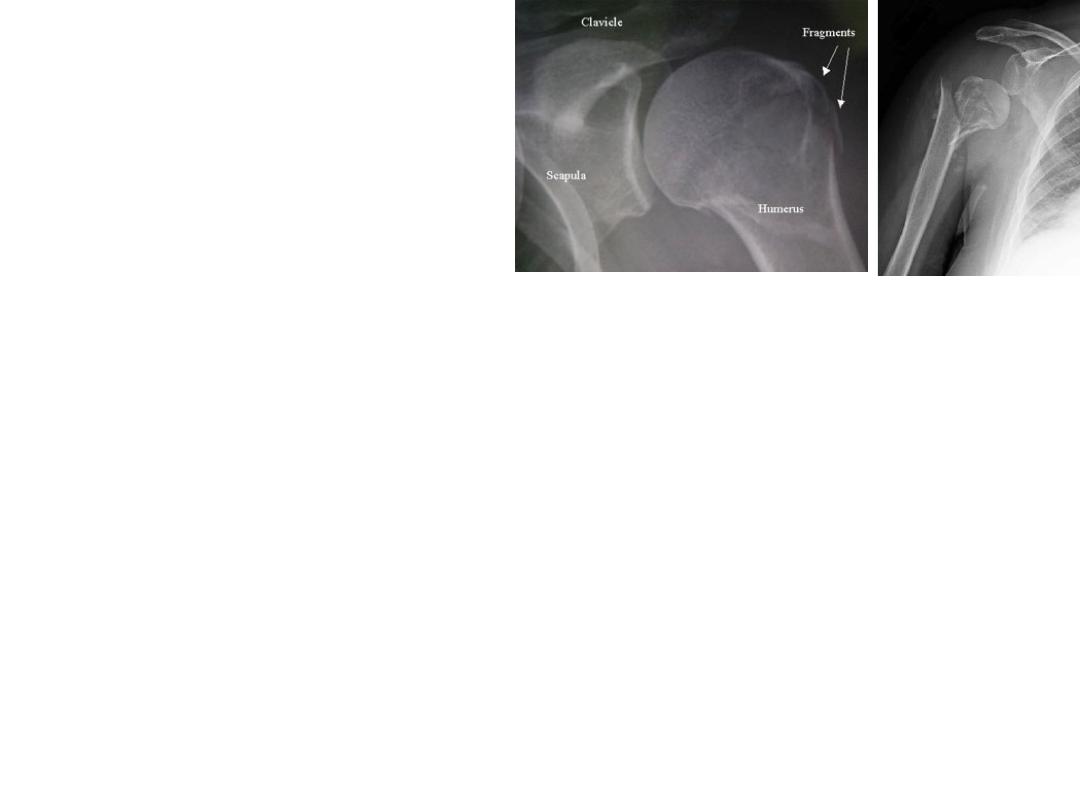
FRACTURES OF THE PROXIMAL
HUMERUS
•
occur after middle age
•
most of the patients are osteoporotic,
postmenopausal women
•
Mechanism of injury: fall on the out-stretched
arm
•
Classification and pathological anatomy
–
Neer
–
four major segments
–
distinguishes between the number of displaced
fragments, with displacement defined as greater than
45 degrees of angulation or 1 cm of separation.

•
Clinical features:
–
pain may not be severe.
–
large bruise on the upper part of the arm is suspicious.
–
Signs of axillary nerve or brachial plexus injury should be
sought.
•
X-ray:
•
In elderly
•
In younger patients,
•
Axillary and scapular-lateral views should always be
obtained, to exclude dislocation of the shoulder.
•
The advent of three-dimensional CT reconstruction

•
Treatment
–
MINIMALLY DISPLACED FRACTURES
•
a week or two period of rest with the arm in a sling until the pain
subsides,
•
gentle passive movements of the shoulder.
•
Once the fracture has united(usually after 6 weeks) active exercises
–
TWO-PART FRACTURES
•
Surgical neck fractures
•
Greater tuberosity fractures
•
Anatomical neck fractures
–
THREE-PART FRACTURES
–
FOUR-PART FRACTURES
–
FRACTURE-DISLOCATION

•
Complications
–
Vascular injuries and nerve injuries:
–
Avascular necrosis:
–
Stiffness of the shoulder:
–
Malunion:

FRACTURES OF THE PROXIMAL
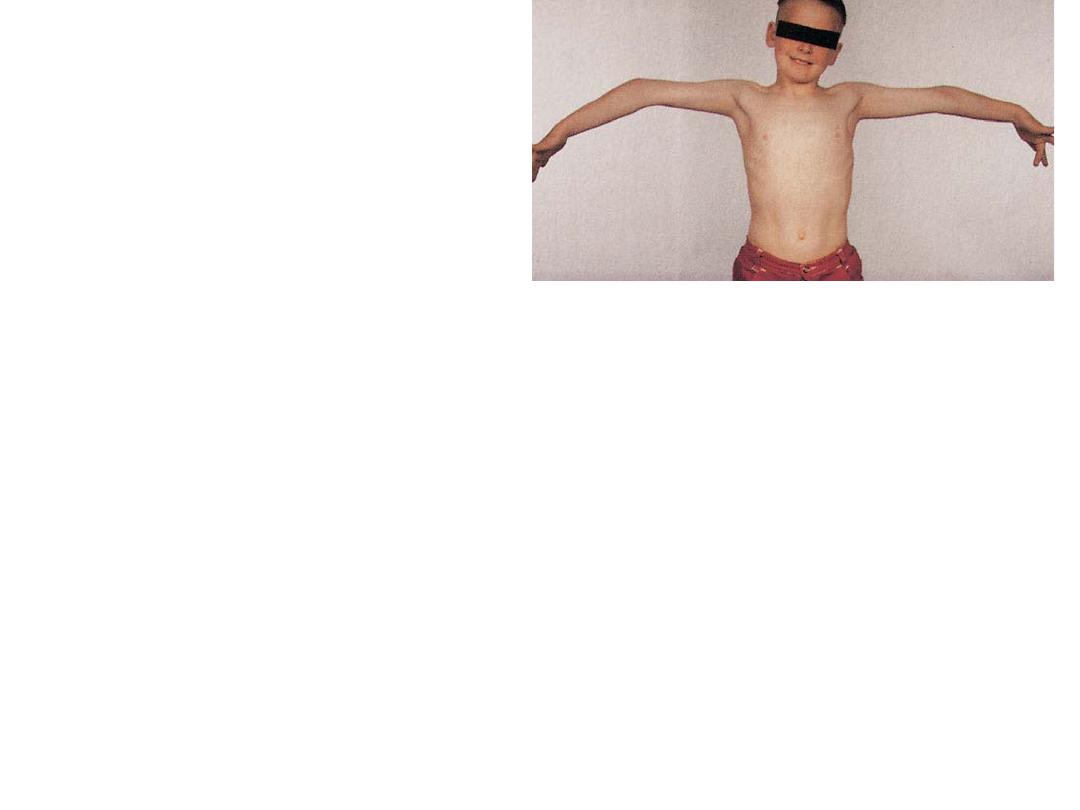
HUMERUS IN CHILDREN
•
At birth, the shoulder is sometimes dislocated or
the proximal humerus fractured. Diagnosis is
difficult and a clavicular fracture or brachial
plexus injury should also be considered.
•
In infancy, the physis can separate (Salter–Harris
I); reduction does not have to be perfect and a
good outcome is usual.
•
In older children,
–
metaphyseal fractures or Type II physeal fractures
occur.
–
Pathological fractures are not unusual,

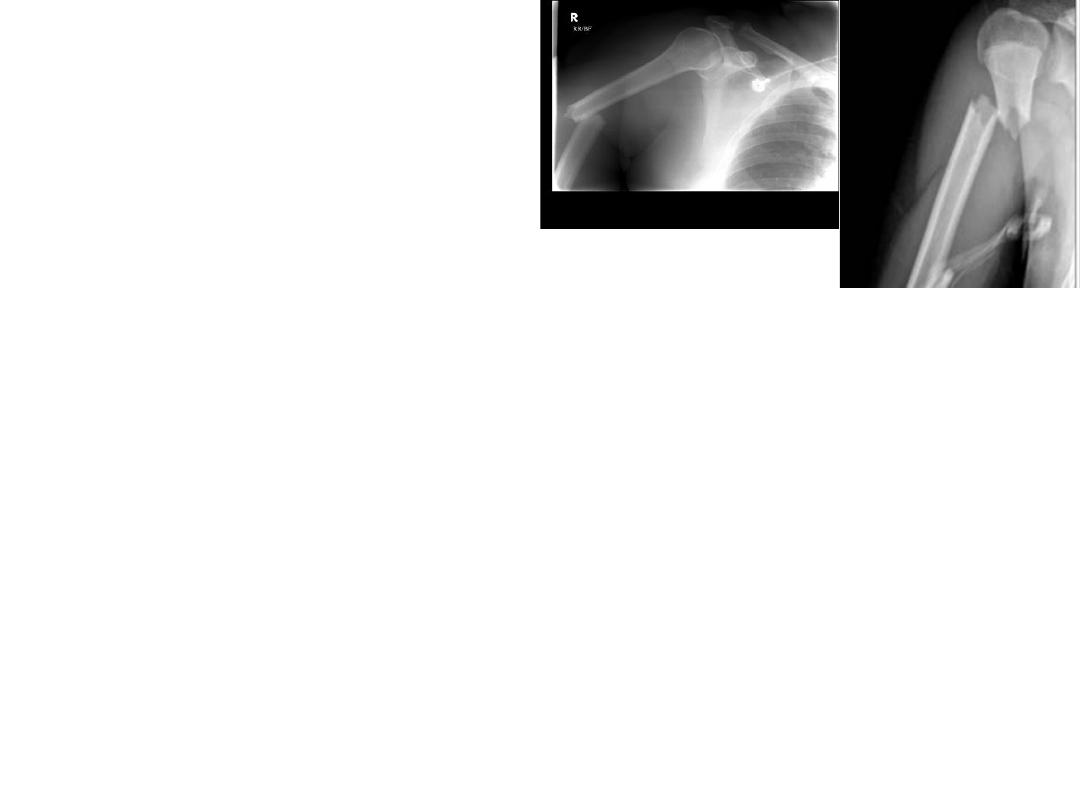
FRACTURED SHAFT OF HUMERUS
•
Mechanism of injury:
–
A fall on the hand may twist the humerus, causing
a spiral fracture.
–
A fall on the elbow with the arm abducted exerts a
bending force, resulting in an oblique or
transverse fracture.
–
A direct blow to the arm causes a fracture which is
either transverse or comminuted.
–
Fracture of the shaft in an elderly patient may be
due to a metastasis.
•
Pathological anatomy:
–
With fractures above the deltoid insertion
–
With fractures lower down,
–
Injury to the radial nerve is common, though fortunately recovery is
usual.
•
Clinical features:
–
painful,
–
bruised
–
swollen.
–
test for radial nerve function before and after treatment.
•
X-ray: The site of the fracture, its line (transverse, spiral or
comminuted) and any displacement are readily seen. The possibility
that the fracture may be pathological
should be remembered.
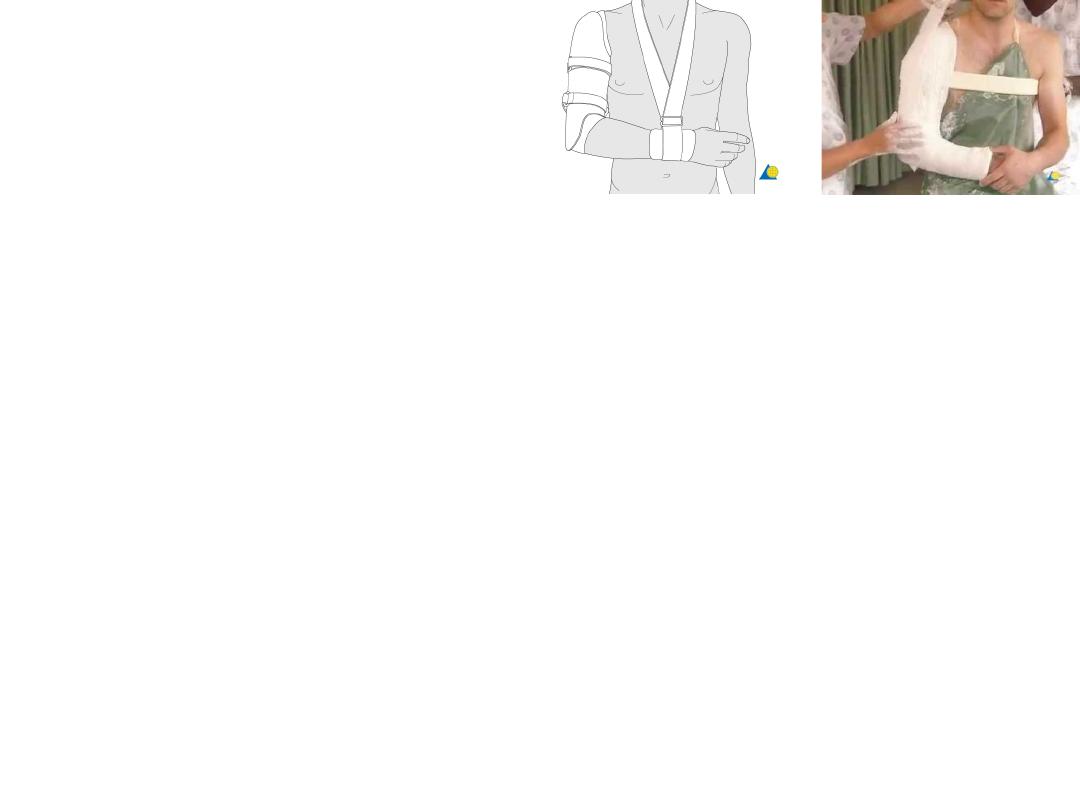
Treatment:
•
‘hanging cast’ replaced after 2–3 weeks by
•
a short (shoulder to elbow) cast or a functional
polypropylene brace (6 weeks).
•
The wrist and fingers are exercised from the start.
•
Pendulum exercises of the shoulder are begun
within a week
•
active abduction is postponed until the fracture
has united (about 6 weeks for spiral fractures but
often twice as long for other types)

OPERATIVE TREATMENT
•
indications for surgery:
–
severe multiple injuries
–
an open fracture
–
segmental fractures
–
displaced intra-articular extension of the fracture
–
a pathological fracture
–
a ‘floating elbow’ (simultaneous unstable humeral and
forearm fractures)
–
radial nerve palsy after manipulation
–
non-union
–
problems with nursing care in a dependent person.

Complications
•
EARLY:
–
Vascular injury:
–
Nerve injury:
•
LATE
–
Delayed union and non-union:
•
excessive traction has been used (a hanging cast must not be too
heavy).
•
Segmental high energy fractures and open fractures are more
prone to both delayed union and non-union.
•
Intramedullary nailing may contribute to delayed union.
•
The treatment of established non-union is operative.
–
Joint stiffness: Joint stiffness is common. It can be
minimized by early activity,
FRACTURES OF THE DISTAL HUMERUS
IN ADULTS
•
High-energy injuries which are associated with
vascular and nerve damage.
•
The AO ASIF Group have defined three types
of distal humeral fracture:
–
Type A – an extra-articular supracondylar fracture;
–
Type B – an intra-articular unicondylar fracture
(one condyle sheared off);
–
Type C – bicondylar fractures with varying degrees
of comminution.

•
TYPE A – SUPRACONDYLAR FRACTURES:
–
extra-articular fractures are rare in adults.
–
displaced and unstable
–
Treatment: Open reduction and internal fixation is the treatment of choice
•
TYPES B AND C – INTRA-ARTICULAR FRACTURES:
–
high-energy injuries with soft-tissue damage.
–
severe blow on the point of the elbow
–
Swelling is considerable
–
elbow is found to be distorted.
–
The patient should be carefully examined for evidence of vascular or nerve injury
–
X-Ray: T- or Y shaped break, or else there may be multiple fragments (comminution). CT scans can be helpful
in planning the surgical approach.
–
Treatment:
•
Undisplaced fractures
•
Displaced Type B and C fractures
–
Complications
•
EARLY:
–
Vascular injury
–
Nerve injury:
•
LATE
–
Stiffness:
–
Heterotopic ossification

FRACTURED CAPITULUM
•
a rare articular fracture
•
occurs only in adults.
•
The patient falls on the hand, usually with the elbow straight. The anterior
part of the capitulum is sheared off and displaced proximally.
•
Clinical features:
–
Fullness in front of the elbow
–
The lateral side of the elbow is tender
–
flexion is grossly restricted.
•
X-Ray: In the lateral view the capitulum (or part of it) is seen in front of the
lower humerus, and the radial head no longer points directly towards it.
•
Treatment:
–
Undisplaced fractures can be treated by simple splintage for 2 weeks.
–
Displaced fractures should be reduced and held. Operative treatment is
therefore preferred.
FRACTURED HEAD OF RADIUS
•
common in adults but are hardly ever seen in children
•
Mechanism of injury: A fall on the outstretched hand with the
elbow extended and the forearm pronated
•
Clinical features: tenderness on pressure over the radial head and
pain on pronation and supination should suggest the diagnosis.
•
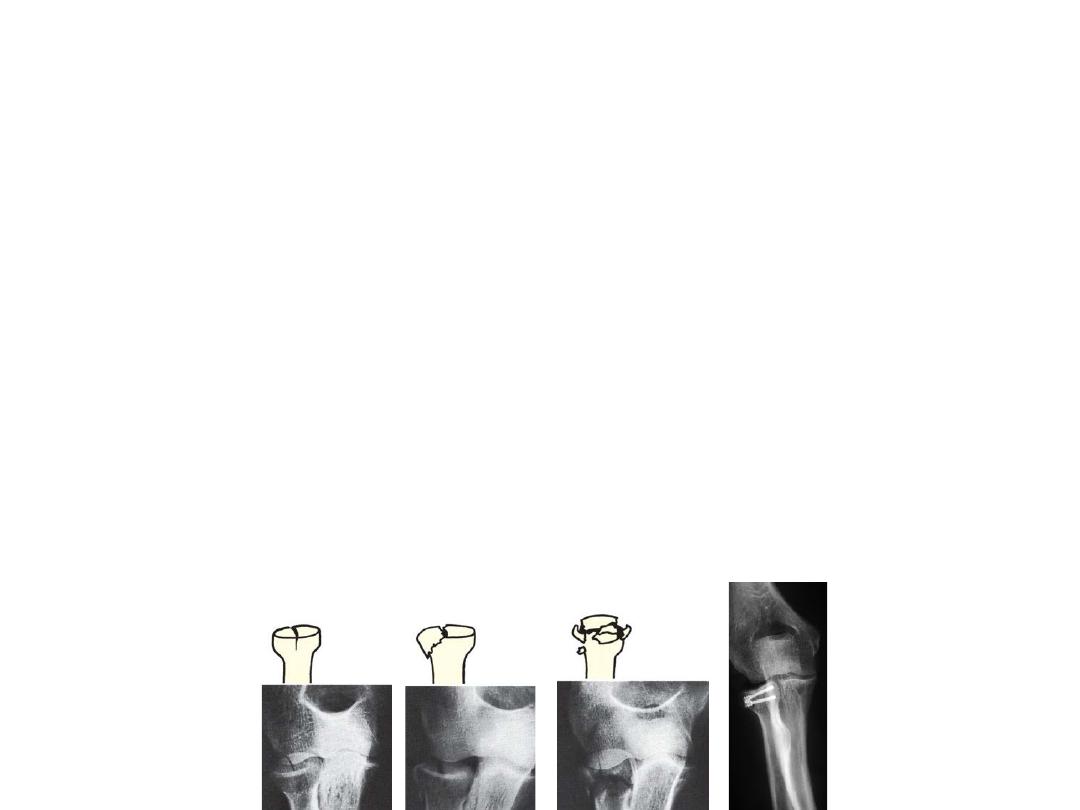
X-ray: Three types of fracture are identified and classified by Mason
as:
–
Type I An undisplaced vertical split in the radial head
–
Type II A displaced single fragment of the head
–
Type III The head broken into several fragments (comminuted).
–
An additional Type IV has been proposed, for those fractures with an
associated elbow dislocation.
•
Treatment:
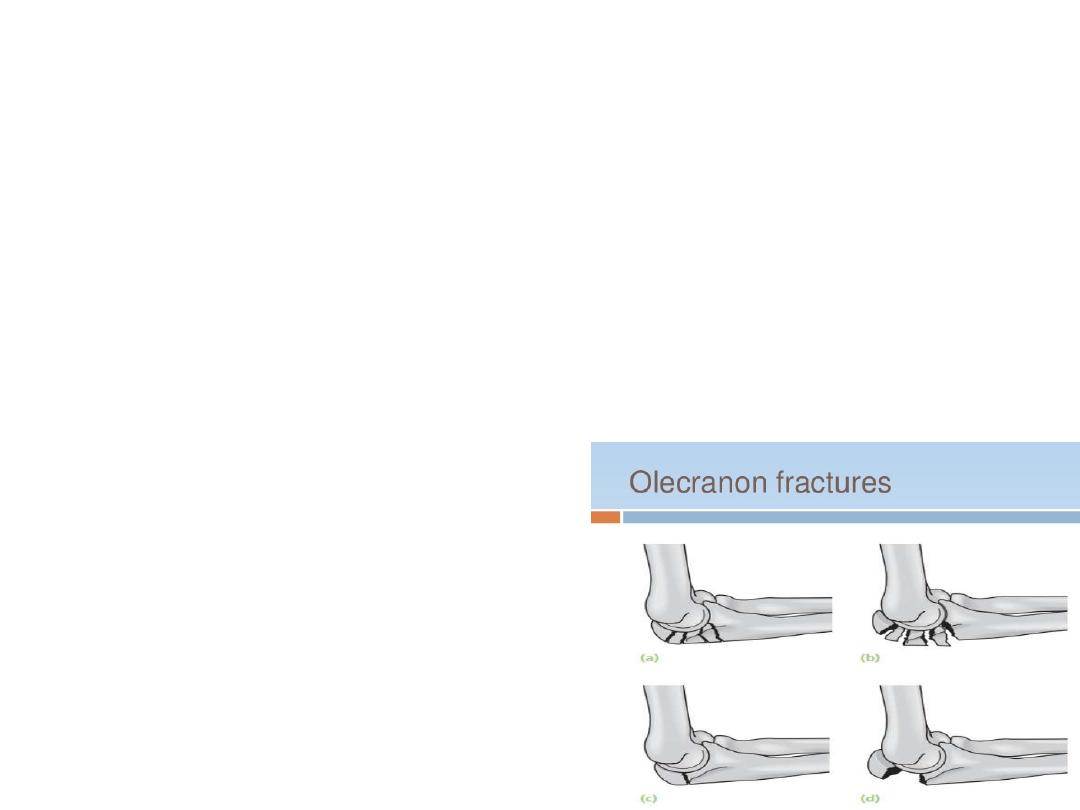
FRACTURES OF THE OLECRANON
•
Two broad types of injury are seen:
•
(1) a comminuted fracture which is due to a direct blow or a fall on
the elbow; and
•
(2) a transverse break, due to traction when the patient falls onto
the hand while the triceps muscle is contracted.
•
further sub-classified into (a) displaced and (b) undisplaced
fractures.
•
Clinical features:
•
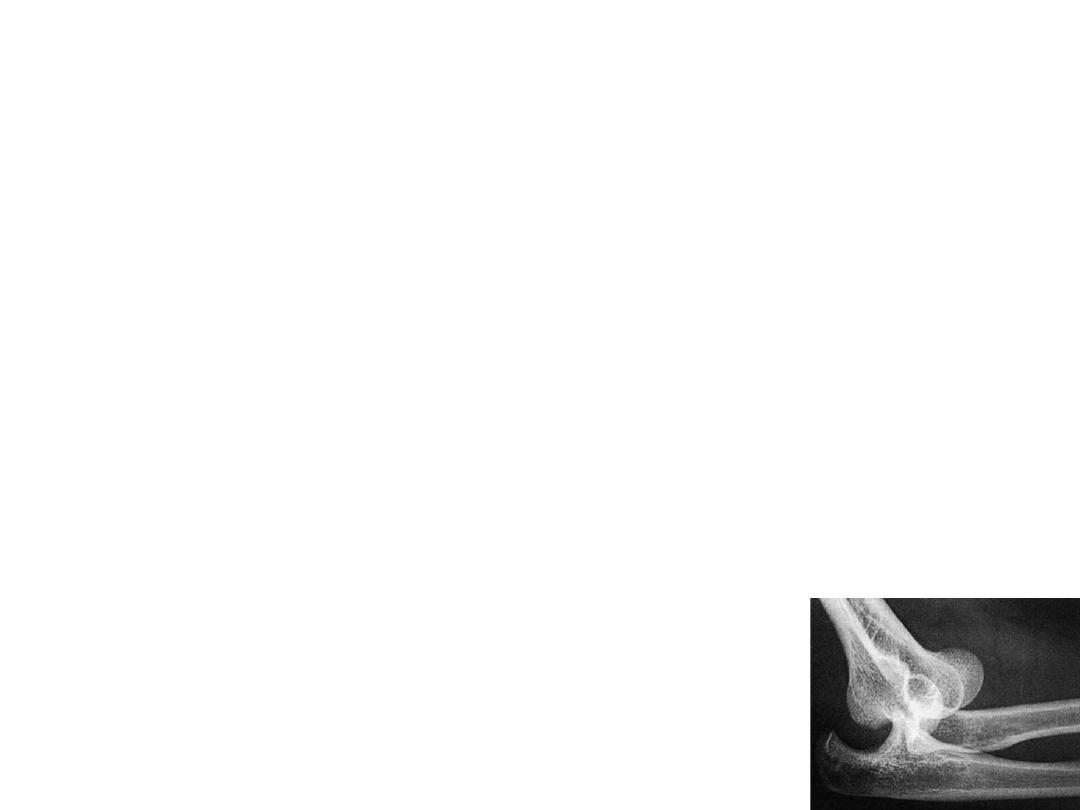
X-ray
•
Treatment
–
comminuted fracture
–
An undisplaced transverse fracture
–
displaced transverse
–
Displaced comminuted fractures
Dislocation of the elbow
•
most common joint dislocation second to the
shoulder
•
more in adults than in children
•
classified according to the direction of
displacement.
•
in 90% of cases the radioulnar complex is
displaced posteriorly or posterolaterally
•
Often together with fractures of the
restraining bony processes

Mechanism of injury and pathology
•
fall on the outstretched hand with the elbow in
extension.
•
If there is no associated fracture, reduction will
usually be stable and recurrent dislocation
unlikely.
•
The combination of ligamentous disruption and
fracture of the radial head, coronoid process or
olecranon process (or, worse still, several
fractures) will render the joint more unstable
•
surrounding nerves and vessels may be damaged.

•
Side swipe injury occurs, typically, when a car-
driver‘s elbow, protruding through the
window is struck by another vehicle.
–
It’s a high energy injury
–
Forward dislocation with fractures of any or all of
the bones around the elbow; soft-tissue damage
(including neurovascular injury) is usually severe.

Clinical features
•
The patient supports his forearm with the elbow in
slight flexion.
•
Unless swelling is severe, the deformity is obvious.
•
The bony landmarks (olecranon and epicondyles) may
be palpable and abnormally placed.
•
the hand should be examined for signs of vascular or
nerve damage
•
X-ray:
–
confirm the presence of a dislocation
–
identify any associated fractures

treatment
•
UNCOMPLICATED DISLOCATION
–
under anaesthesia.
–
The surgeon pulls on the forearm while the elbow
is slightly flexed. With one band, sideways
displacement is corrected, then the elbow is
further flexed while the olecranon process is
pushed forward with the thumbs.
–
After reduction, the elbow should be put through
full range of movement to see whether it is stable

•
The distal nerves and circulation are checkcd
again.
•
an x-ray is obtained
•
The arm is held in a collar and cuff with the
elbow flexed above 90 degrees.
•
After 1 week the patient gently exercises his
elbow; at 3 weeks the collar and cuff is
discarded

•
DlSLOCATION WITH ASSOCIATED FRACTURES
–
Coronold process
•
A single or comminuted fracture involving more than 50
per cent and lf the elbow is unstable after reduction,
then fixation is usually needed.
–
Medial epicondyle
•
lf displaced, it must be reduced and fixed back in
position.
•
The arm and wrist are splinted with the elbow at 90
degrees;
•
after 3 weeks movements are begun under supervision

•
Head of radius
–
type ll or III unstable injury;
–
stability is restored repair of the ligaments and
restoration of the radial pillar (fracture fixation or
prosthetic replacement)
•
Olecranon process
–
Open reduction with internal fixation is the best
treatment.

Complications
•
EARLY
–
Vascular injury
•
The brachial artery may be damaged.
•
this should be treated as an emergency.
•
Splints must be removed and the elbow should be
straightened somewhat.
•
If there is no improvement, an arteriogram is performed; the
brachial artery may have to be explored.
–
Nerve injury
•
The median or ulnar nerve is sometimes injured.
Spontaneous recovery usually occurs after 6-8 weeks.

•
LATE
–
Stiffness
•
Loss of 20 to 30 degrees of extension is not uncommon after
elbow dislocation usually of little functional significance
•
Move as soon as possible
–
Hetrotopic ossification(myositis ossificans)
•
Occur in the damaged soft tissue in front of the joint
•
associated with forceful reduction
•
If the condition is suspected_ exercises are stopped and the elbow
is splinted in comfortable flexion until pain subsides; gentle active
movements and continuous passive motion are then resumed.
•
Anti-inflammtory drugs may help
•
A bone mass can be excised though not before the bone is fully
mature

–
Unreduced dislocation
•
A dislocation may not have been diagnosed; or only the
backward displacement corrected, leaving the
olecranon process still displaced sideway
•
Up to 3 weeks manipulative reduction .
•
Other than this there is no satisfactory treatment
•
Open reduction stiffness
•
Leave the condition in the hope to gain useful range of
movement

–
Recurrent dislocation
•
This is rare unless there is a large coronoid fracture or radial
head fracture.
•
If recurrent elbow instability occurs, the lateral ligament and
capsule can be repaired or reattached to the lateral condyle.
•
A cast with the elbow at 90 degrees is worn for 4 weeks.
–
Osteoarthritis
•
Quite common after severe fracture dislocations
•
In older patients, total elbow replacement can be considered

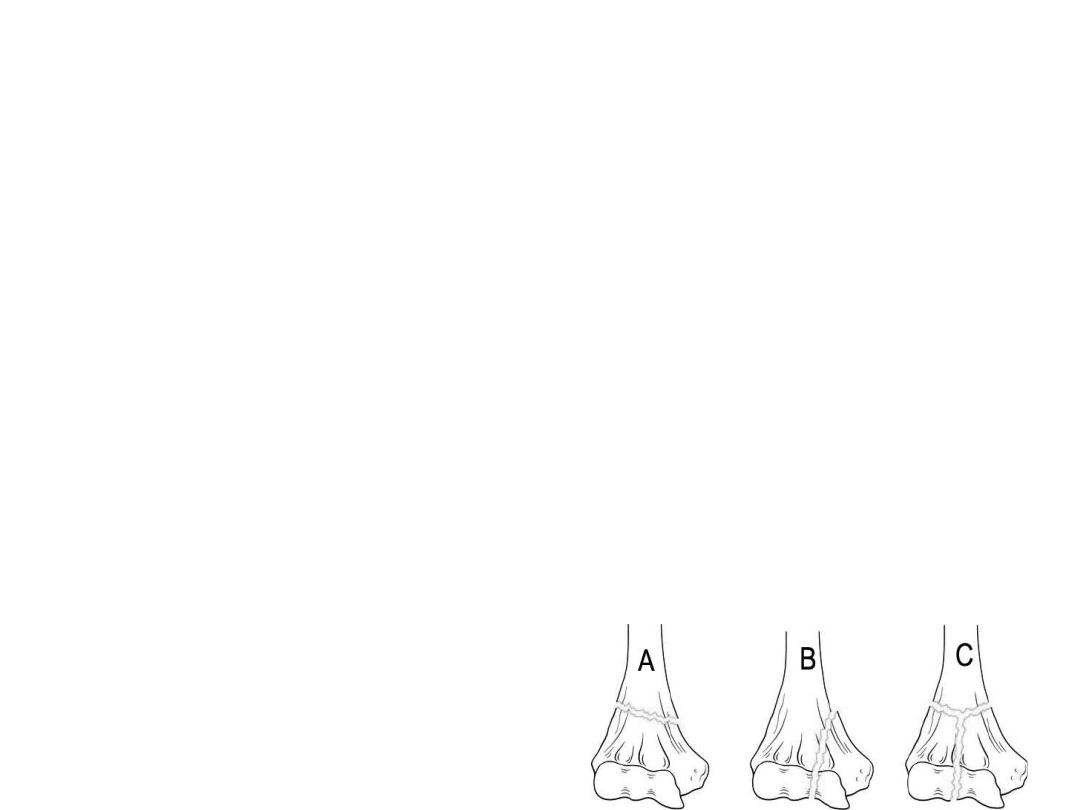
Fractures around the elbow in children
SUPRACGNDYLAR FRACTURES
•
Among the commonest fractures in children.
•
The distal fragment may be displaced either posteriorly or
anteriorly
•
Mechanism of injury
–
Posterior angulation or displacement (95%) suggests a hyperextension
injury, usually due to a fall on the outstretched hand. The humerus
breaks just above the condyles. The distal fragment is pushed
backwards and (because the forearm is usually in pronation) twisted
inwards. The jagged end of the proximal fragment pokes into the soft
tissues anteriorly, sometimes injuring the brachial artery or median
nerve.
–
Anterior displacement is rare; thought to be due to direct violence
(e.g. a fall on the point of the elbow) with the joint in flexion

•
Classification
–
Type I is an undisplaced fracture.
–
Type II is an angulated fracture with the posterior
cortex still in continuity.
•
IIA - a less severe injury with the distal fragment merely
angulated.
•
IIB - a severe injury; the fragment is both angulated and
malrotated.
–
Type III is a completely displaced fracture

•
Clinical features
–
pain
–
elbow is swollen;
–
with a posteriorly displaced fracture the S-deformity
of the elbow is usually obvious
–
It is essential to feel the pulse and check the capillary
return;
–
passive extension of the flexor muscles should be
pain-free.
–
The wrist and the hand should be examined for
evidence of nerve injury.

•
X-ray
–
The fracture is seen most clearly in the lateral view.
–
In an undisplaced fracture the ‘fat pad sign’ should raise
suspicions
–
In the common posteriorly displaced fracture the fracture line
runs obliquely downwards and forwards and the distal fragment
is tilted backwards and/ or shifted backwards.
–
In the anteriorly displaced fracture the crack runs downwards
and backwards and the distal fragment is tilted forwards.
–
An AP View is often difficult to obtain without causing pain
–
It may show that the distal Fragment is shifted or tilted sideways
and rotated usually medially

•
TREATMENT
–
TYPE I UNDISPLACED FRACTURE
•
The elbow is immobilized at 90 degrees and neutral
rotation in a light-weight splint or cast and the arm is
supported by a sling.
•
It is essential to obtain an x-ray 5-7 days later to check
that there has been no displacement.
•
The splint is retained for 3 weeks and supervised
Movement is then allowed

•
TYPE II A: FOSTERIORLY ANGULATED FRACTURE -MILD
–
the fracture can be reduced under GA by the following step-
wise manoeuvre:
•
(l ) traction for 2-3 minutes in the length of the arm with counter-
traction above the elbow;
•
(2) correction of any sideways tilt or shift and rotation
•
(3) gradual flexion of the elbow to 120 degrees, and pronation of the
forearm, while maintaining traction and exerting finger pressure
behind the distal fragment to correct posterior tilt,
–
Following reduction, the arm is held in a collar and cuff; the
circulation checked repeatedly during the first 24 hours. An x-ray
is obtained after 3-5 days to confirm that the fracture has not
slipped.
–
The splint is retained for 3 weeks, after which movements are
begun.
•
TYPES ll B AND lll ANGULATED AND MALROTATED
OR POSTERIORLY DISPLACED
–
These are usually associated with severe swelling, are
difficult to reduce and are often unstable
–
The fracture should be reduced under G.A as soon as
possible, by the method described above, and then
held with percutaneous crossed K-wires;
–
this obviates the necessity to hold the elbow acutely
flexed.
–
Postoperative management is the same as for Type Il
A.

•
OPEN REDUCTlON: This is sometimes necessary for
–
a Fracture which simply cannot be reduced closed;
–
an open fracture; or
–
a fracture associated with vascular damage
•
CONTINUOUS TRACTION: Traction through a screw in the
olecranon, with the arm held overhead, can be used
–
if the fracture is severely displaced and cannot be reduced by
manipulation;
–
if; with the elbow flexed 100 degrees, the pulse is obliterated
and image intensification is not available to allow pinning and
then straightening of the elbow;
–
for severe open injuries or multiple injuries of the limb.
Once the swelling subsides, a further attempt can be made at
closed reduction.

•
TREATMENT OF ANTERIORLY DISPLACED
FRACTURES
–
The fracture is reduced by pulling on the forearm
with the elbow semiflexed, applying thumb
pressure over the front of the distal fragment and
then extending the elbow fully.
–
Crossed percutaneous pins are used if unstable.
–
A posterior slab is put and retained for 3 weeks.
–
Thereafter, the child is allowed to regain flexion
gradually.

•
Complications
–
EARLY
•
Vascular lnjury :
brachial artery,
–
Peripheral ischaemia may be immediate and severe
–
the pulse may fail to return after reduction,
More commonly the injury is complicated by forearm oedema
and a mounting, compartment syndrome
–
The flexed elbow must be extended and all dressings removed
–
if the circulation does not promptly improve,then angiography
(on the operating table if it saves time) is carried out,
–
the vessel repaired or grafted and a forearm fasciotomy
performed.

•
Nerve injury :The radial nerve, median nerve
(particularly the anterior interosseous branch)
or the ulnar nerve may be injured
–
recovery can be expected in 3 to 4 months, If
there is no recovery the nerve should be explored.
–
If it occur after manipulation nerve should be
explored
•
LATE
–
Malunion is common,
•
Backward or sideways shifts are gradually smoothed out by
remodelling
•
Forward or backward tilt may limit flexion or extension, but
disability is slight
•
Uncorrectcd sideways tilt (angulation) and rotation are much
more important and may lead to varus (or rarely valgus)
deformity
•
If it is marked, it will need correction by supracondylar
osteotomy usually once the child approaches skeletal
maturity

•
Elbow stiffness and myositis ossifficans
–
Extension in particular may take months to return
–
Passive or forced movement is prohibited
–
Prevented by Proper rehabilitation



