Malnutrition
Dr. Mazin Al-JadiryOctober 19, 2015
Learning objectives
To define malnutrition and know its causesTo assess malnutrition by using the indicators and anthropometric measures
To know the wellcome classification
To differentiate between Marasmus and Kwashiorkior.
To understand the basics of treatment of severe malnutrition
INTRODUCTION
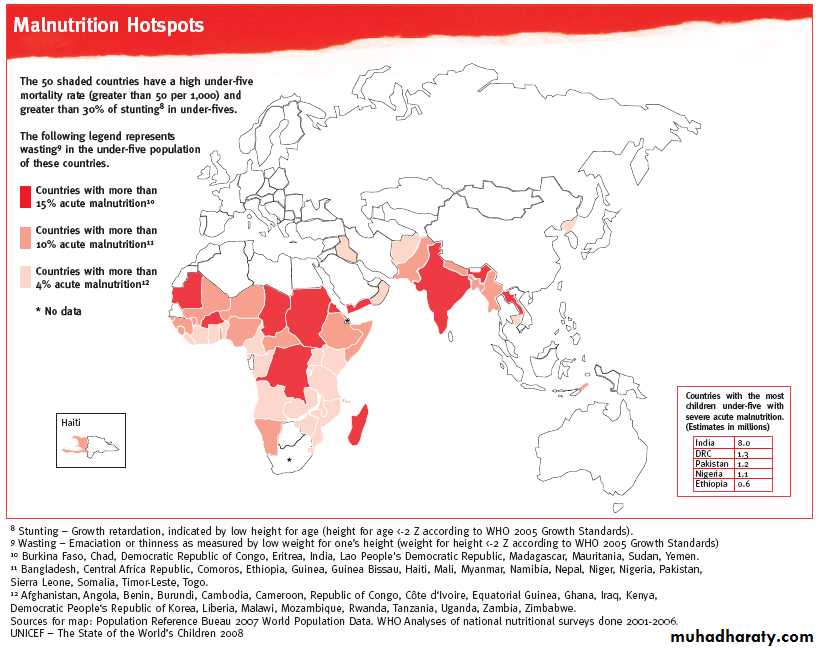
Malnutrition essentially means “bad nourishment”. It concerns not enough as well as too much food, the wrong types of food, or the inability to use nutrients properly to maintain health.The World Health Organization cites malnutrition as the greatest single threat to the world's public health.
Malnutrition in all its forms is a considerable public health concern and is associated with increases risk of disease and early death.
3
Definition
Malnutrition is a general term for the medical condition caused by an improper or insufficient diet.Under nutrition (deficiency of one or more essential nutrients); resulting from inadequate consumption, poor absorption, or excessive loss of nutrients.
Over nutrition (an excess of a nutrient or nutrients); resulting from overeating or excessive intake of specific nutrients.
Undernutrition (malnutrition)
Structural and functional changes due to inadequate intake of nutrients and energy sources.Deficiency of a single nutrient is an example of undernutrition, e.g. iron and iodin.
All children with PEM have micronutrient deficiency
Causes
Primary Malnutrition: resulting from inadequate food intakeSecondary Malnutrition: resulting from increased nutrient needs, decreased nutrient absorption, and/or increased nutrient losses.
Developing countries 1 °> 2 ° malnutrition
Developed countries 2 ° > 1 ° malnutrition
Causes of 1 ° Malnutrition
Accounts for the vast majority of cases:Nutrition: Inadequate food intake due to;
• Insufficient or inappropriate food supplies
• Early cessation of breastfeeding
• Cultural and religious food customs (in some areas)
Causes of 2 ° Malnutrition
Children with chronic illness are at risk for nutritional problems for several reasons, including the following:Anorexia, which leads to inadequate food intake.
Increased inflammatory burden and increased metabolic demands can increase caloric need.
Any chronic illness that involves the liver or small bowel affects nutrition adversely by impairing digestive and absorptive functions. Like:
Cystic fibrosis
Chronic renal failure
Childhood malignancies
Congenital heart disease
Neuromuscular diseases
Chronic inflammatory bowel diseases
Protein-Energy Malnutrition
The term PEM applies to a group of related disorders that include marasmus, kwashiorkor, and intermediate states of marasmus-kwashiorkor.
The distinction between the 2 forms of PEM is based on the presence or absence of edema.
Marasmus; inadequate intake of protein and calories (absence of odema)
Kwashiorkor;fair-to-normal calorie intake with inadequate protein intake (presence of odem).
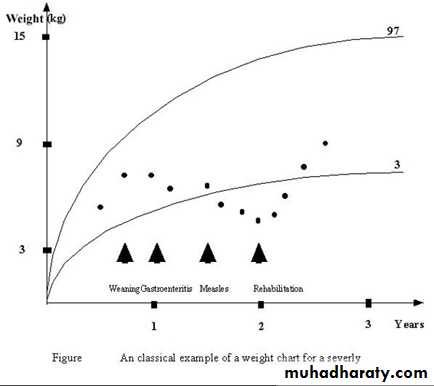
Classic history of PEM
EARLY ABRUPTWEANING
DILUTE DIRTY
FORMULA
REPEATED INFECTIONS
Especially
GASTRO-ENTERITIS
STARVATION
‘THERAPY’
LATE GRADUAL
WEANING
STARCHY
FAMILY DIET
ACUTE INFECTION
BREAST FEEDING
5 months
12 months
NUTRITIONAL
MARASMUS
8 Months
18 MonthsBIRTH
URBANISING INFLUENCES, PREGNANCIES IN RAPID SUCCESSION
KWASHIORKOR
MARASMIC-KWASHIORKOR
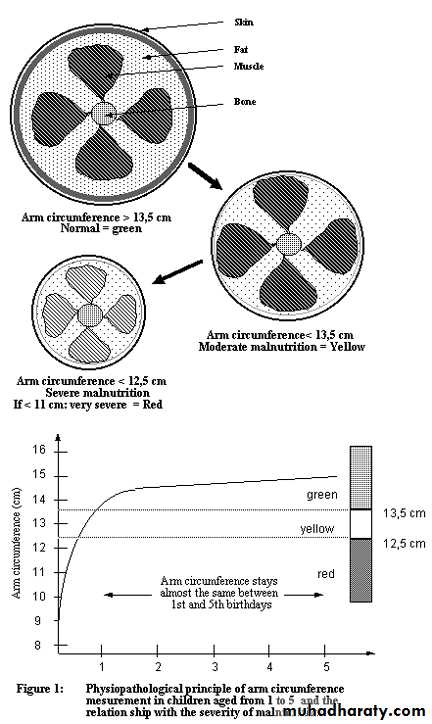
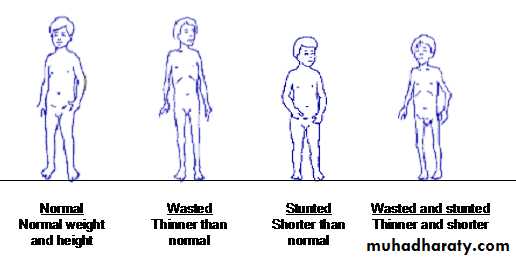
Measuring malnutrition
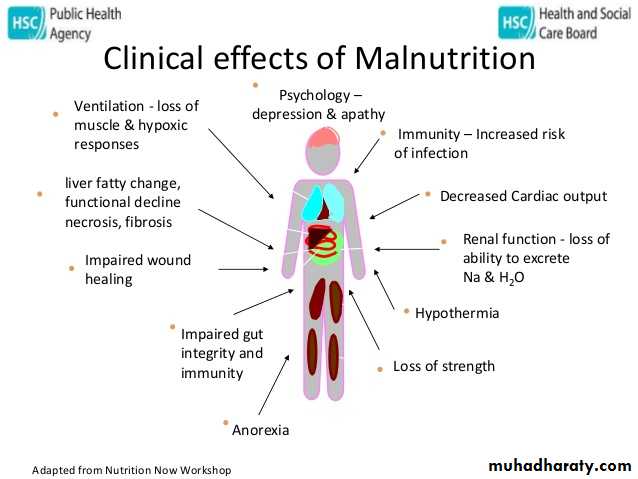
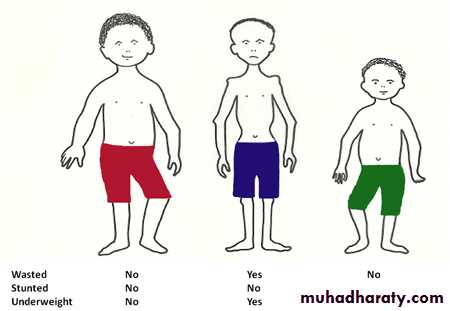
Malnutrition is assessed by a combination of clinical features and anthropometry(body measurements). The indicators used are:Wasting:
Weight for height,
Mid upper arm circumference (MUAC),
Body mass index (BMI)
Stunting: height for age
Wasting and stunting combined: weight for age
Protein Energy malnutrition(anthropometric measurements)
Underweight
Measurements that fall below 2 standard deviations under the normal weight for age.
Stunting
Measurements that fall below 2 standard deviations below height for age.
Wasting
Measurements that fall below 2 standard deviations below weight for height.
Diagnosis
AnthropometryAcute: Wasting: low weight for height
Chronic: Stunted: low height for age
Protein Energy malnutrition(Clinical diagnosis)
Weight for height below
70% of the medianBipedal edema
Visible severe wastingWellcome Classification
• Nutritional Oedema• Grade
• Definition
• Classification
• Weight-for-age %
• Wellcome
• Absent
• Undernourished
• 80-60
• present
• Kwashiorkor• Absent
• Marasmus• <60 (= ─ 4SDS)
• present
• Marasmic-kwashiorkorWellcome Classification
Definition :Marasmus: Weight less than 60% of expected weight - no oedema.
Kwashiorkor: Weight between 60-80% of expected weight + oedema
No oedema Oedema
• <80% =Kwashiorkor
• <80% =Underweight for age
• <60%=Marasmic-Kwashiorkor
• <60%=Marasmus
What do we need?
Weighing scale
Growth chartFinger
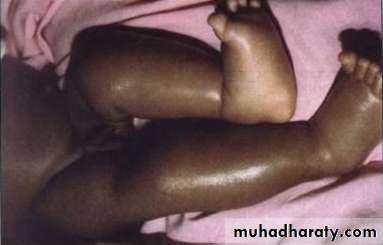
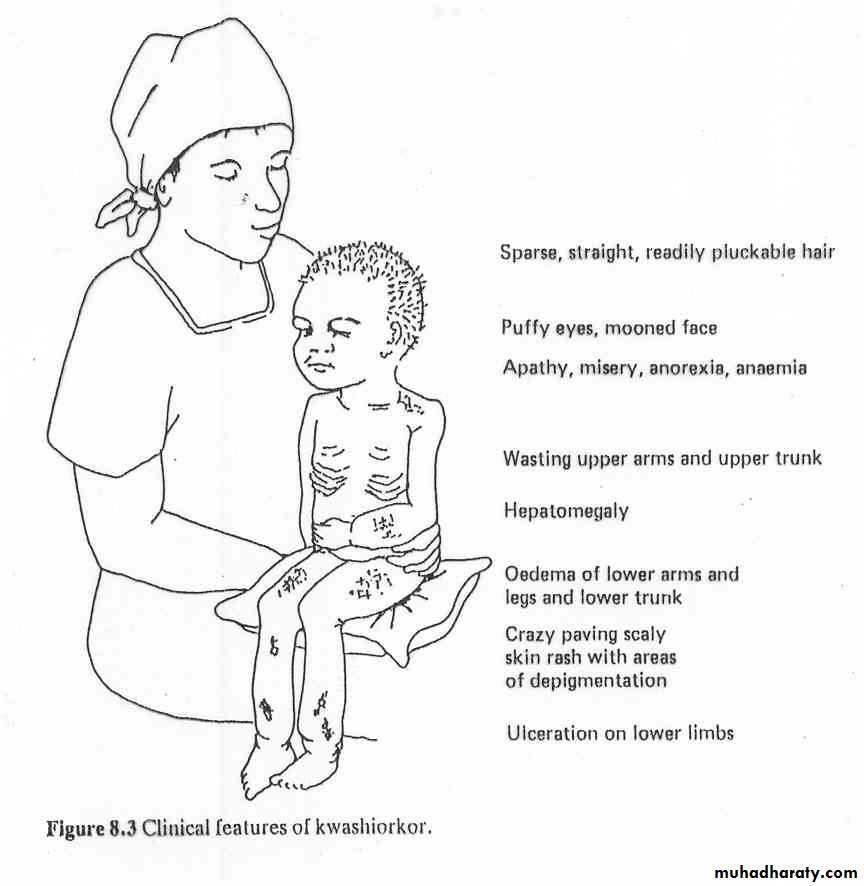
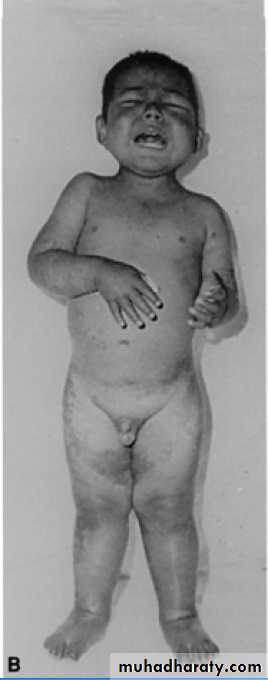
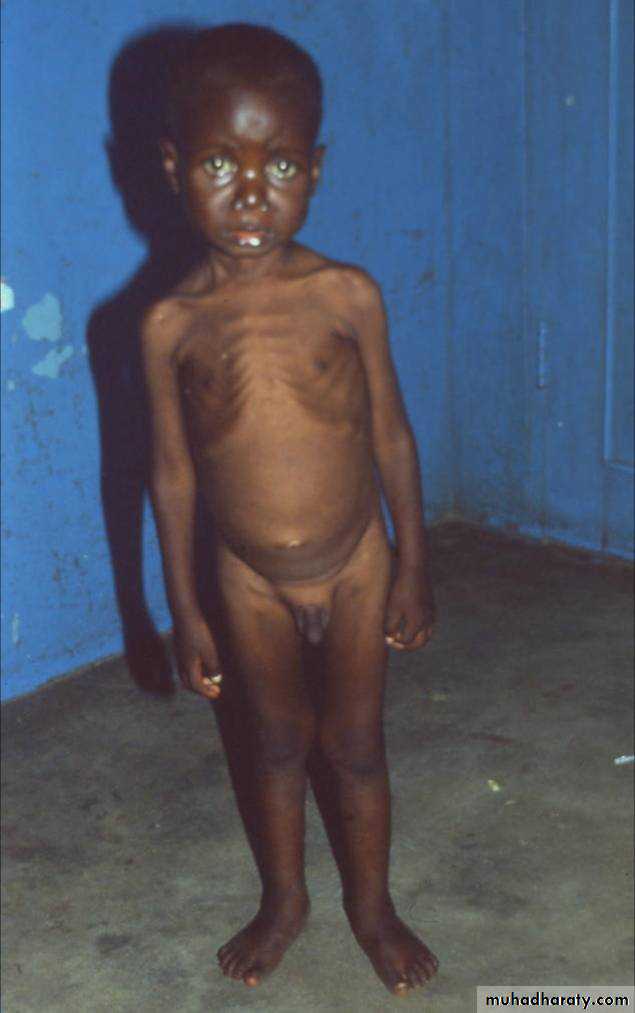
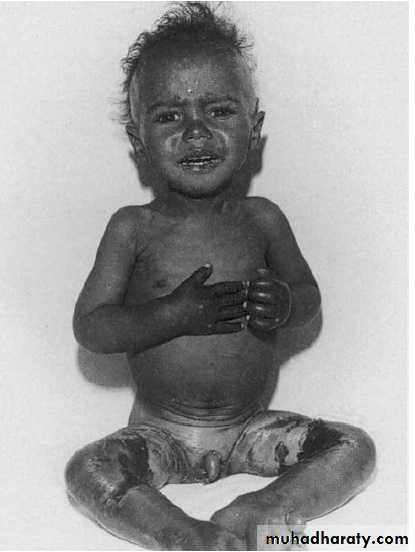
Kwashiorkor
• " the one who is displaced" reflecting the development of the condition in the older child who has been weaned from the breast once a new sibling is born.Kwashior-kor
• Deficiency of protein with relatively adequate energy intake.• Failure of growth:
• Oedema: pitting, bilateral including lower extermities. May be localized or extensive, including eyelids.
• The muscles are wasted; This is particularly noticeable around the chest and the upper arm; the wasting of the legs and around the hips is frequently concealed by oedema.
Kwashior-kor
• Mental changes:: the child is apathetic and miserable.• Hair: becomes fine, straight and often sparse. Children with long straight black hair may show a pale band across the hair, corresponding to an earlier episode of kwashiorkor, the 'flag sign'.
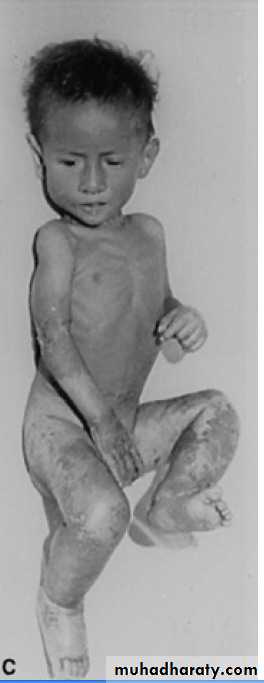
• Skin: pigmentation, desquamation and ulceration. A severe case may look like an extensive burn. The legs, buttocks and perineum are most frequently involved, but any region may be affected.
• Mucous membranes: angular stomatitis, cheilosis and a smooth tongue are commonly seen, as is ulceration around the anus.
• Liver: this may be enlarged.
• Gastrointestinal system: anorexia is usually present and sometimes vomiting. There is nearly always diarrhea, with the passage of stools containing undigested food. The diarrhea may be due to impaired secretion of digestive enzymes, to intestinal mucosal atrophy or to an intestinal infection.
• Anaemia
• Associated vitamine deficiencies: vit. A, thiamine, niacine, folate, vitamin k
• Kwashior-kor
Death does not occur from actual starvation but from secondary infectionKwashior-kor
Kwashior-kor
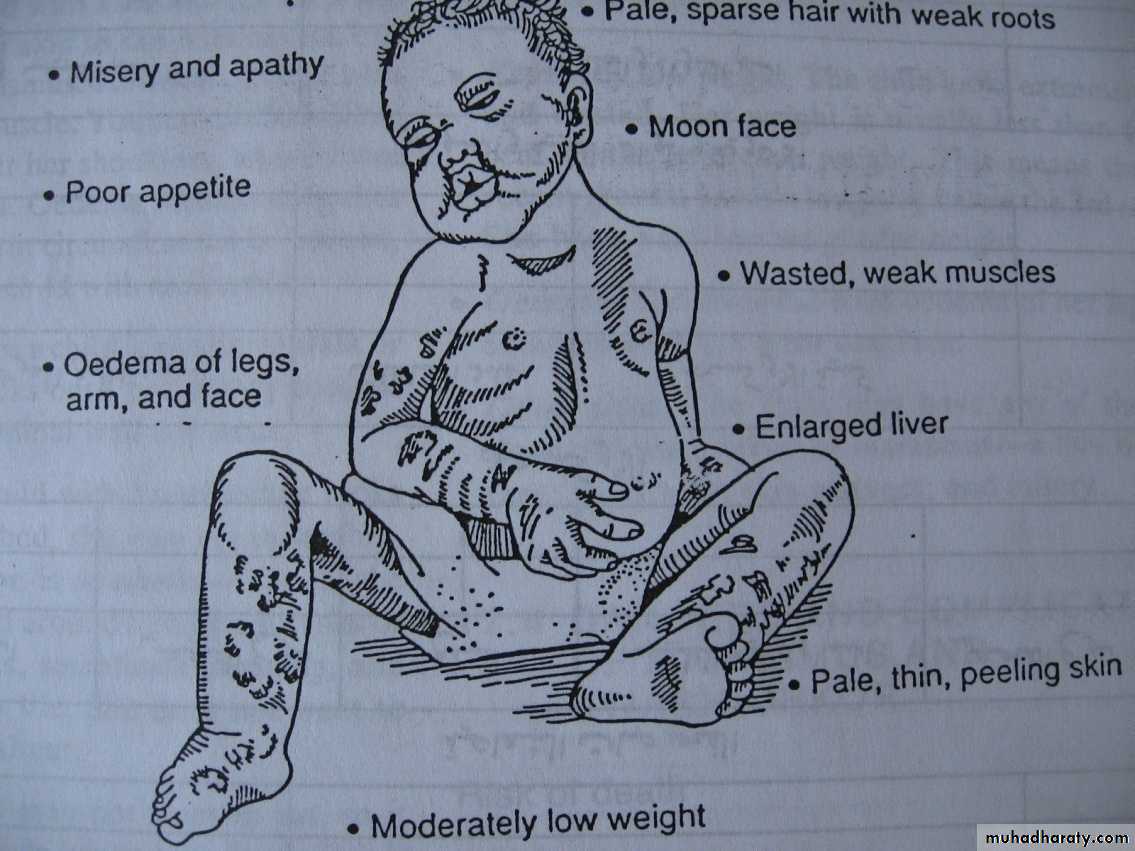
Signs of Kwashiorkor:
Oedema of the legs and arms and face
Moon face
Moderately low weight
Misery and apathy
Poor appetite
Pale, thin, peeling skin
Pale spare hair with weak roots
Enlarge liver
Thining of hair, odema, stomatitis indicates an accompanying vitamine B deficiency
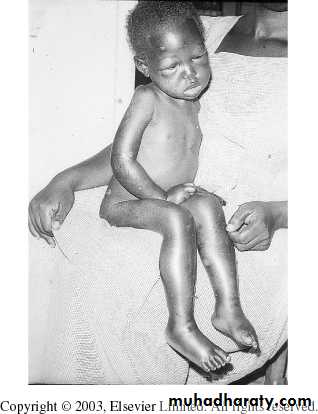
KwashiorkorEdema and skin lesions in a 3-year-old child with kwashiorkor
Kwashiorkor; skin changes
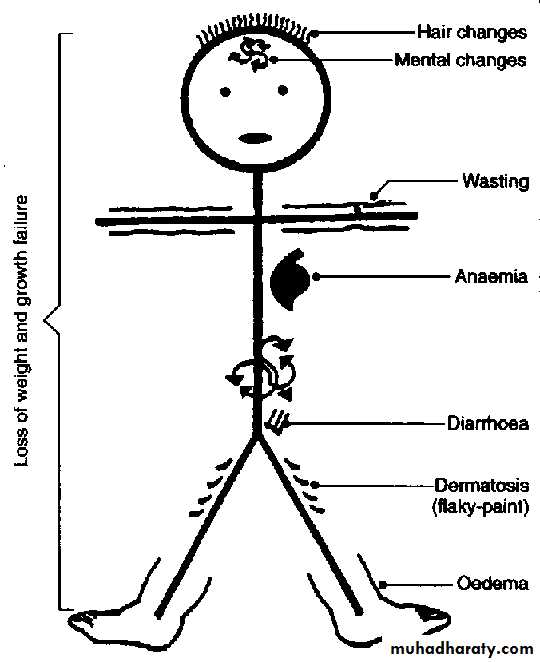
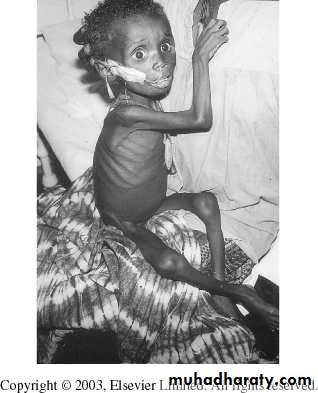
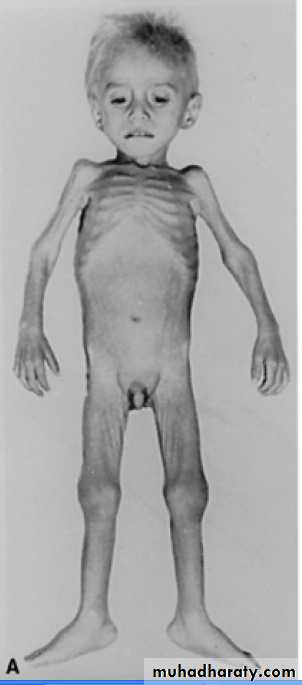
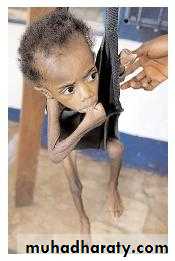
Nutritional marasmusDue to a severe and prolonged restriction of all food, i.e. energy sources & other nutrients + protein.
The two constant features of marasmus are:
Retardation of growth and reduction of weight
Wasting of muscles & loss of subcutaneous fat started from the abdominal wall then the buttocks then from the buccal pad of fat which gave the infant a wizened, old appearance.
Appetite is usually preserved or enhanced & the liver is usually normal, with no fatty infiltration.
Episodes of hypothermia and fasting hypoglycaemia are common
Nutritional marasmus
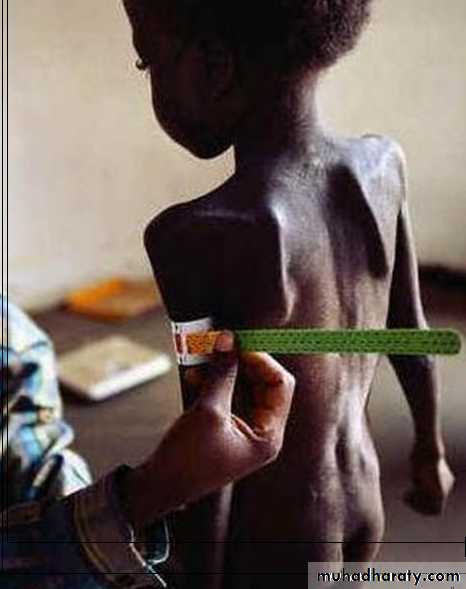
• Emaciated: thin, flaccid skin (the ‘little old man’ appearance), fat and muscle tissue grossly reduced, prominence spine and ribs• Behaviour: alert and irritable
• Electrolyte imbalance, dehydration
• Infection,
• Normal hair
• There are no biochemical or haematological changes diagnostic of the condition
Nutritional Marasmus
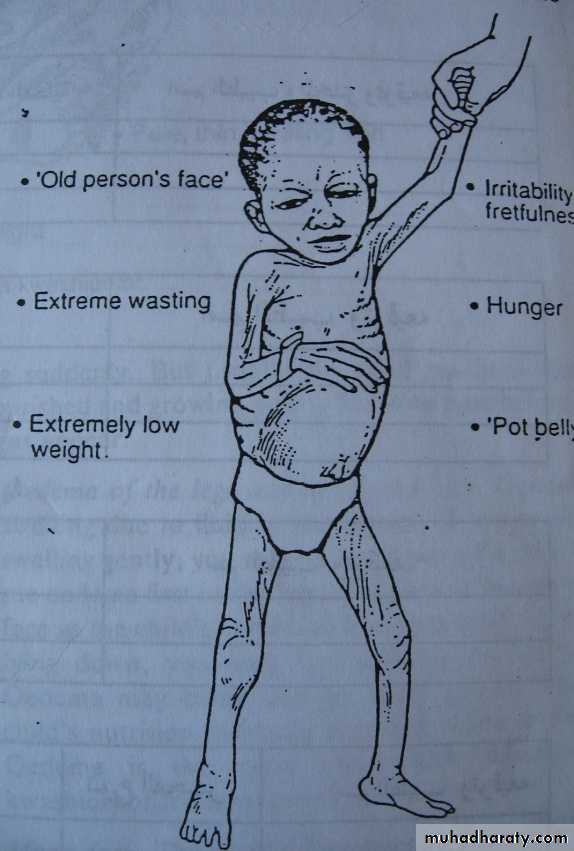
Signs of marasmus:
Extremely low weight
Extreme wasting
An ' old person's face'
Pot belly: the child's abdomen protruded, because the muscles of the abdominal wall are wasted and weak
Irritability
Hunger
Marasmus
Weight for age < 60% expectedNo edema
Often stunted
Hungry, relatively easier to feed
Marasmus
Severe wasting in infant with marasmus
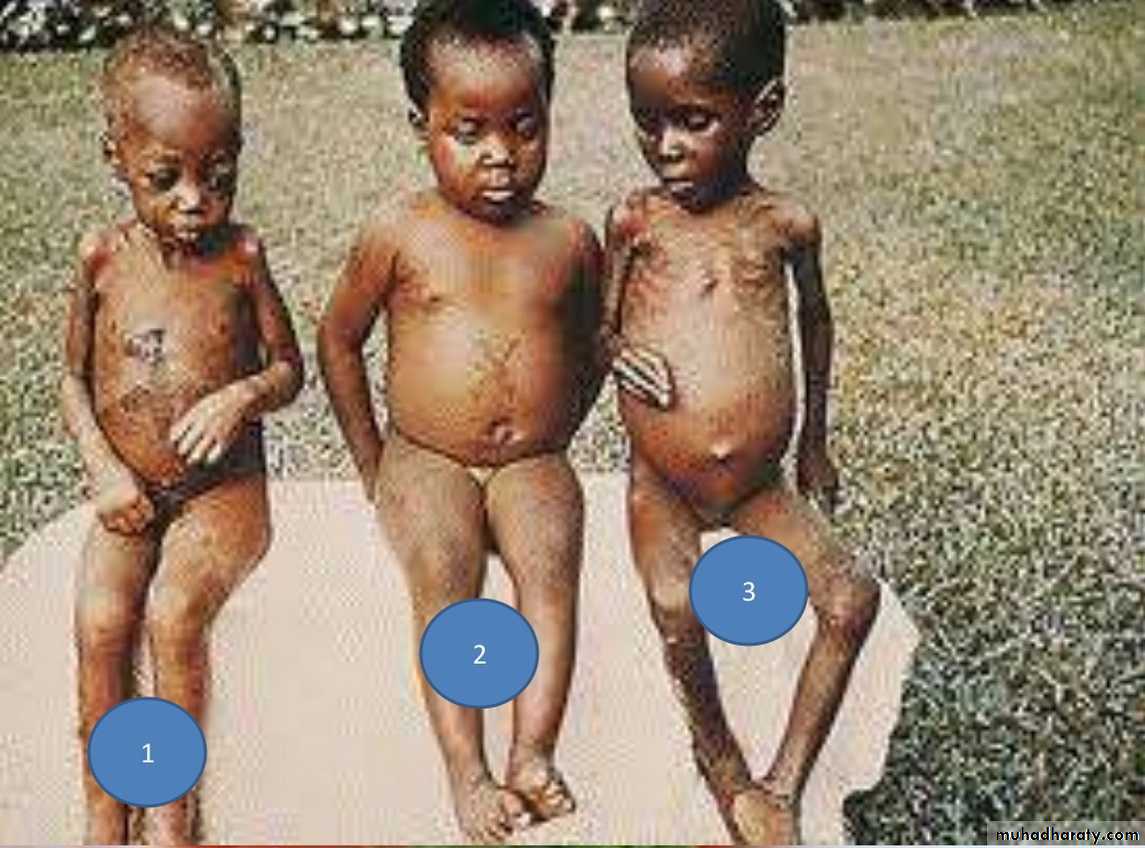
Marasmic-Kwashiorkor
Marasmic kwashiorkor:Wasting in the upper arms
Characteristics of kwashiorkor in the lower limbs
38
PROTEIN-ENERGY MALNUTRITION
MARASMUS39
KWASHIORKOR
Quiz?
MK
K
M
Evaluation
Practical nutritional assessmentComplete history, including a detailed dietary history
Growth measurements, including weight and length/height; head circumference in children younger than 3 years
Complete physical examination
Evaluation
Laboratory investigations are generally unhelpfulTests that may be useful in the assessment of PEM and management of complications:
laboratory studies evaluating protein status
hematological studies
Blood glucose
GUE & culture
Stool exam & culture
CXR
MANAGEMENT
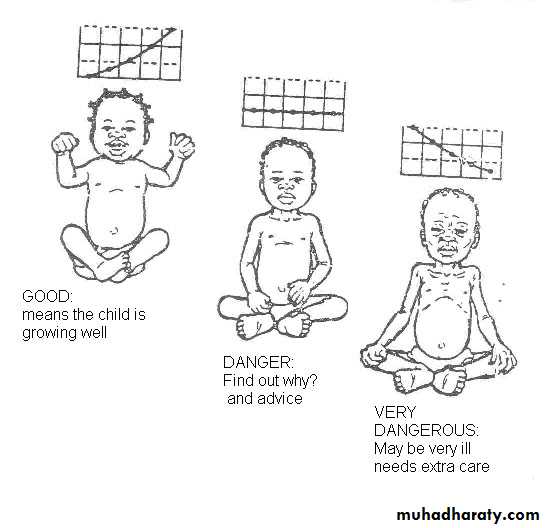
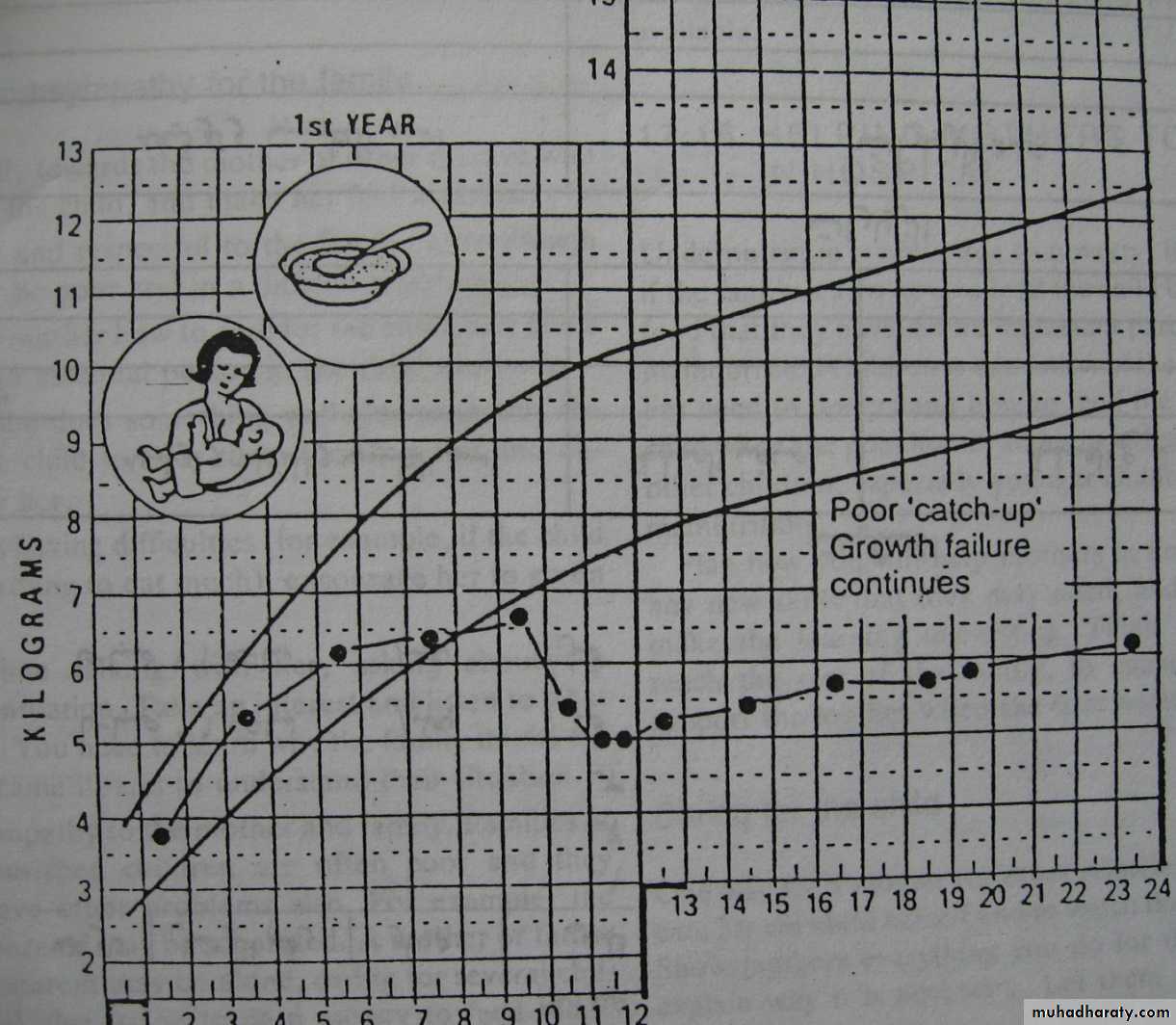
Successful management of malnutrition should mean complete catch-up followed by sustained normal growth, health and development.
Treatment of severe malnutrition
• Weight• Height
• Oedema
• Vomiting
• Diarrhea
• Temperature
• Heart rate
• Respiratory rate
Phases of treatment
Management of severe malnutrition is best divided into three phases.Following clinical evaluation, the Initial Phase (days 1-7 )involves resuscitation, treatment of infection and correction of disordered metabolism.
The principal tasks are:
To treat or prevent hypoglycemia and hypothermia;
To treat or prevent dehydration and restore electrolyte balance;
To treat septic shock, if present;
To start to feed the child
To treat infection;
To identify and treat any other problems, including vitamin deficiency, severe anemia and heart failure
Initial Phase
At each feed the food should be offered by mouth, after which the remainder is given by NG tube.
Severely malnourished patients do not tolerate the usual amounts of dietary protein, fat, and sodium, and require a diet low in these component and in osmolality, but high in carbohydrate.
Initial Phase
Phases of treatment
Usually within a week, the recovery is heralded by the following criteriaEating well
Mental status has improved; smiles, responds to stimuli, interested in surroundings
Normal temperature (36.5-37.5°C)
No vomiting or diarrhea
No oedema
Gaining weight:> 5g/kg of body weight per day for 3 successive days
Response
Phases of treatment
The second or Rehabilitation Phase (weeks 2-6 )The principal tasks are:
To encourage the child to eat as much as possible
To re-initiate and/or encourage breastfeeding as necessary
To stimulate emotional and physical development; and
To prepare the mother to continue to look after the child after discharge
Rehabilitation Phase
Phases of treatment
At this stage, the formula feed is changed to one that provides more energy (up to 150kcal/kg/24hr ) and protein (4g/kg/24hr) for growth.
The child’s dietary intake increases steadily, the frequency of feeding is reduced and weight gain is rapid, up to 20 times normal, on average 10 g/kg/day.
The child’s mother must be taught of nutrition and food preparation and hygiene.
Rehabilitation Phase
Phases of treatmentIdeally, the child is visited at increasing intervals for up to 3 years to ensure that recurrence of malnutrition is prevented
Follow-Up Phase (weeks 7-26 )
Treatment of Malnutrition
Follow WHO Guidelines• Treat/prevent hypoglycaemia
• Treat/prevent hypothermia
• Treat/prevent dehydration
• Correct electrolyte imbalance
• Treat/prevent infection
• Correct micronutrient deficiencies
• Initiate refeeding
• Facilitate catch-up growth
• Provide sensory stimulation & emotional support
• Prepare for follow-up after recovery
Time-frame for the management of a child with severe malnutrition
• Follow up
• Rehabilitation
• Initial treatment
• Activity
• Weeks 7-26• Weeks 2-6
• Days 3-7
• Days 1-2
• Hypoglycemia
• Hypothermia
• Dehydration
• Correct electrolyte
• imbalance
• Treat infection
• With iron
• without iron
• Correct micronutrient
• deficiencies• Begin feeding
• Increase feeding to
• recover lost weight
• ("catch-up growth")
• Stimulate emotional and
• sensorial development
• Prepare for discharge
Treatment of Malnutrition
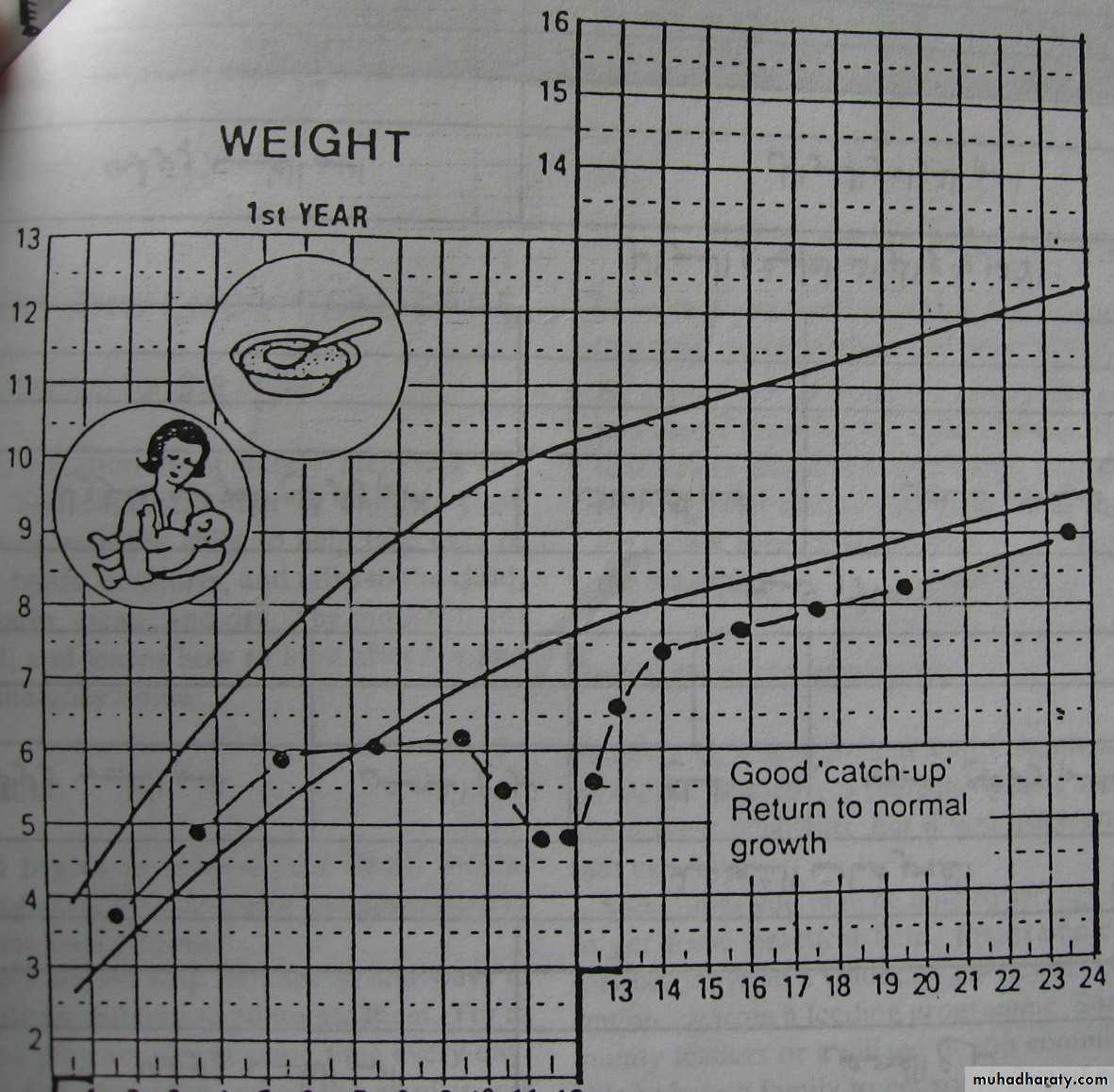
Catch-up growth
Poor “catch-up” Growth failure continues
Good “catch-up” Return to normal growthTick sign
Catch-up growth
Complication
Severe kwashiorkor and marasmus has a mortality of around 20% even in a well equipped hospital.Most deaths occur in the first 10 days
The usual cause of death are intercurrent infections and severe malnutrition.
Time Magazine, August, 2008
• Hypoglycemia• Hypothermia
• Dehydration
• Infection
• Severe anemia
Direct causes of death:
Prognosis
The sick children usually do not achieve their full growth potential or regain cognitive deficits.Over half of childhood mortality in developing countries is either directly or indirectly secondary to malnutrition.