4
th
year
Systemic pathology
GIT
Dr. mohamed sabaa ch.
M.B.CH.B Ms.Pathology

THE ORAL CAVITY & OROPHARYNX
Many pathological processes can affect the
constituents of the oral cavity. The more important
and frequent conditions will covered in this lecture.
Diseases involving the teeth and related structures
will not be discussed.
PROLIFERATIVE LESIONS
The most common proliferative lesions of the oral
cavity are
1. Irritation Fibroma and Ossifying fibroma
2. Pyogenic granuloma
3. Peripheral giant cell granuloma

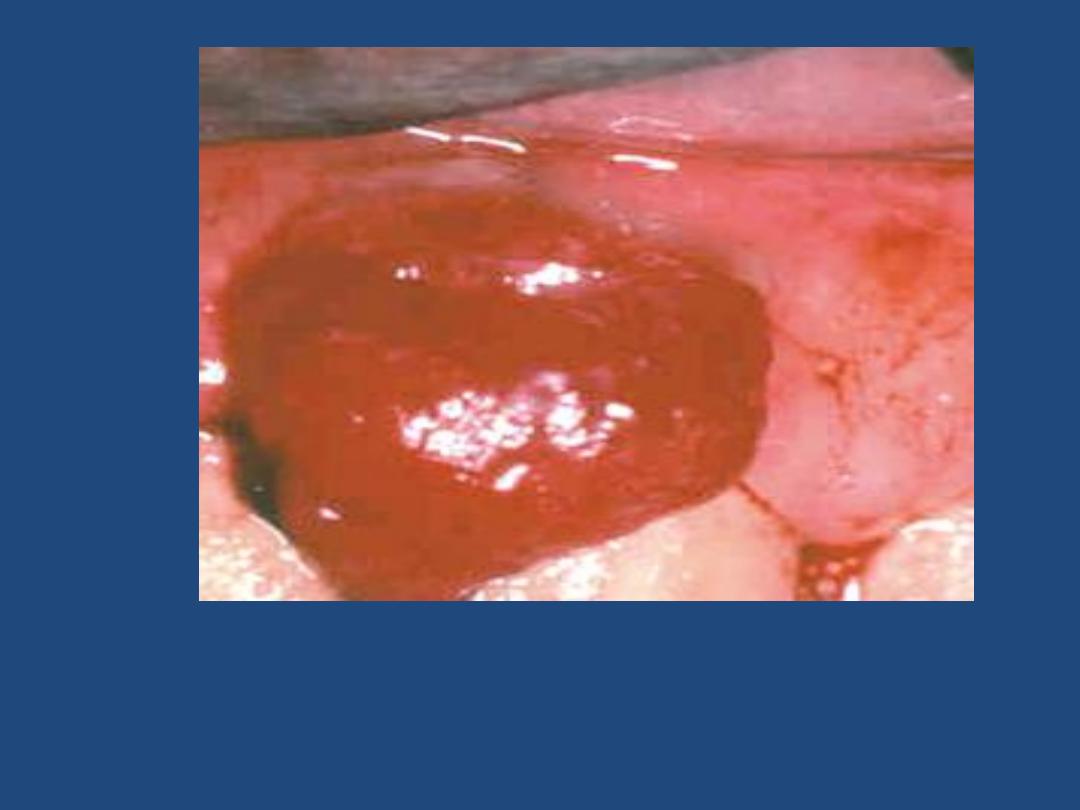
Pyogenic granuloma (granuloma pyogenicum) is a
highly vascular lesion that is usually seen in the
gingiva of children, young adults, and pregnant
women (pregnancy tumor). The lesion is typically
ulcerated and bright red in color (due to rich
vascularity) Microscopically there is vascular
proliferation similar to that of granulation tissue.
The lesion either regresses (particularly after
pregnancy), or undergoes fibrous maturation and
may develop into ossifying fibroma.

INFLAMMATORY CONDITIONS
Inflammatory ulcerations
The most common inflammatory ulcerations of the
oral cavity are
1. Traumatic
2. Aphthous
3. Herpetic
Traumatic ulcers, usually the result of trauma (e.g. fist
fighting) or licking a jagged tooth.
Aphthous ulcers are extremely common, single or
multiple, painful, recurrent, superficial, ulcerations of
the oral mucosa. The ulcer is covered by a thin yellow
exudate and rimmed by a narrow zone of erythema.
Herpetic ulcers (see under herpes simplex infection)

INFECTIONS
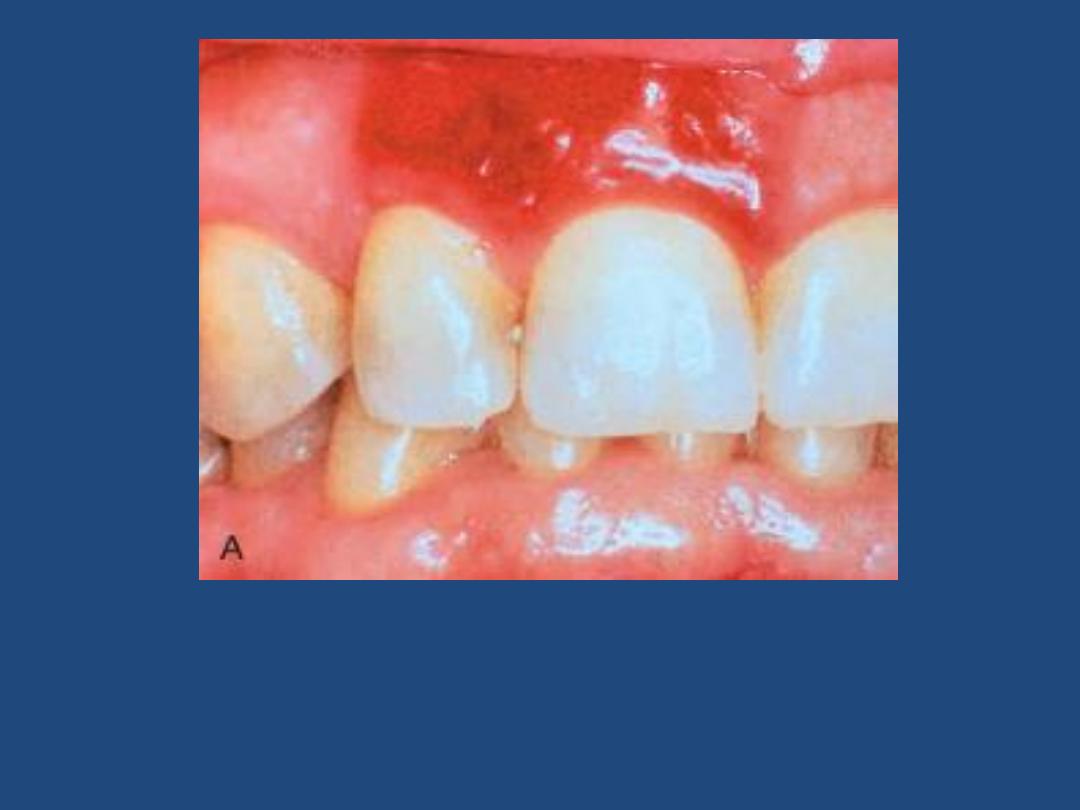
1. Herpes simplex infections
Most of these are caused by herpes simplex virus
(HSV) type 1 & sometimes 2. Primary HSV infection
typically occurs in children aged 2 to 4 years; is often
asymptomatic, but sometime presents as acute
herpetic gingivostomatitis, characterized by vesicles
and ulcerations throughout the oral cavity. The great
majority of affected adults harbor latent HSV-1 (the
virus migrates along the regional nerves and
eventually becomes dormant in the local ganglia
e.g., the trigeminal)

In some individuals, usually young adults, the virus becomes
reactivated to produce the common but usually mild cold
sore.
Factors activating the virus include
1. Trauma
2. Allergies
3. Exposure to ultraviolet light (sunlight)
4. Upper respiratory tract infections
5. Pregnancy
6. Menstruation
7. Immunosuppression
The viral infection is associated with intracellular and
intercellular edema, yielding clefts that may become
transformed into vesicles. The vesicles range from a few
millimeters to large ones that eventually rupture to yield
extremely painful, red-rimmed, shallow ulcerations.

2. Other Viral Infections
These include:
-
Herpes zoster
-
EBV (infectious mononucleosis)
-
CMV
-
Enterovirus
-
Measles

3. Oral Candidiasis (thrush)
This is the most common fungal infection of
the oral cavity. The thrush is a grayish white,
superficial, inflammatory psudomembrane
composed of the fungus enmeshed in a
fibrino-suppurative exudates. This can be
readily scraped off to reveal an underlying red
inflammatory base

The fungus is a normal oral flora but causes
troubles only
1. In the setting of immunosuppression (e.g.
diabetes mellitus, organ or bone marrow transplant
recipients, neutropenia, cancer chemotherapy, or
AIDS) or
2. When broad-spectrum antibiotics are taken;
these eliminate or alter the normal bacterial flora
of the mouth.
3. In infants, where the condition is relatively
common, presumably due to immaturity of the
immune system in them.

4. Deep Fungal Infections
Some fungal infections may extends deeply to
involve the muscles & bones in relation to oral
cavity. These include, among others,
histoplasmosis, blastomycosis, and
aspergillosis.
The incidence of such infections has been
increasing due to increasing number of
patients with AIDS, therapies for cancer, &
organ transplantation

ORAL MANIFESTATIONS OF SYSTEMIC DISEASE
Many systemic diseases are associated with oral lesions
& it is not uncommon for oral lesions to be the first
manifestation of some underlying systemic condition.
Scarlet fever: strawberry tongue: white coated tongue
with hyperemic papillae projecting
2. Measles: Koplik spots: small whitish ulcerations
(spots) on a reddened base, about Stensen duct
3. Diphtheria: dirty white, fibrinosuppurative, tough
pseudomembrane over the tonsils and retropharynx
4. AIDS
a. opportunistic oral infections: herpesvirus, Candida,
other fungi
b. Kaposi sarcoma
c. hairy leukoplakia

5. AML (especially monocytic leukemia):
enlargement of the gingivae + periodontitis
6. Melanotic pigmentation
a. Addison disease
b. hemochromatosis
c. fibrous dysplasia of bone
7. Pregnancy: pyogenic granuloma ("pregnancy
tumor")

TUMORS AND PRECANCEROUS LESIONS
Many of the oral cavity tumors (e.g., papillomas,
hemangiomas, lymphomas) are not different
from their homologous tumors elsewhere in the
body. Here we will consider only oral squamous
cell carcinoma and its associated precancerous
lesions.
Leukoplakia and Erythroplakia are considered
premalignant lesions of squamous cell
carcinoma.

Leukoplakia
is a white patch that cannot be scraped off and
cannot be attributed clinically or microscopically
to any other disease i.e. if a white lesion in the
oral cavity can be given a specific diagnosis it is
not a leukoplakia. As such, white patches caused
by entities such as candidiasis are not
leukoplakias. All leukoplakias must be considered
precancerous (have the potential to progress to
squamous cell carcinoma) until proved otherwise
through histologic evaluation.


Erythroplakias
are red velvety patches that are much less
common, yet much more serious than
leukoplakias. The incidence of dysplasia and
thus the risk of complicating squamous cell
carcinoma is much more frequent in
erythroplakia compared to leukoplakias. Both
leukoplakia and erythroplakia are usually found
between ages of 40 and 70 years, and are much
more common in males than females. The use of
tobacco (cigarettes, pipes, cigars, and chewing
tobacco) is the most common incriminated
factor.

Squamous cell carcinoma
The vast majority (95%) of cancers of the head
and neck are squamous cell carcinomas; these
arise most commonly in the oral cavity. The 5-
year survival rate of early-stage oral cancer is
approximately 80%, but this drops to about 20%
for late-stage disease. These figures highlight
the importance of early diagnosis & treatment,
optimally of the precancerous lesions.

The pathogenesis of squamous cell carcinoma is
multifactorial.
1. Chronic smoking and alcohol consumption
2. Oncogenic variants of human papilloma virus (HPV).
It is now known that at least 50% of oropharyngeal
cancers, particularly those of the tonsils and the base
of tongue, harbor oncogenic variants of HPV.
3. Inheritance of genomic instability; a family history
of head and neck cancer is a risk factor.
4. Exposure to actinic radiation (sunlight) & pipe
smoking are known predisposing factors for cancer of
the lower lip.

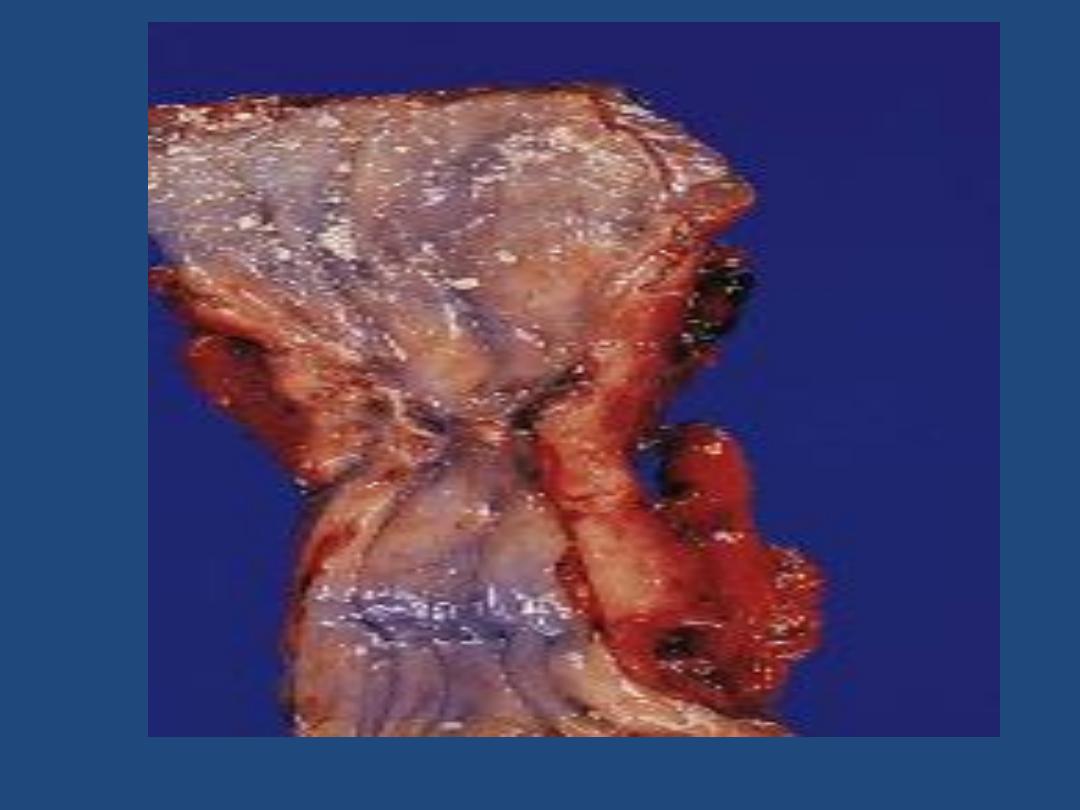
Gross features
Squamous cell carcinoma may arise anywhere in the
oral cavity, but the favored locations are
1. The tongue
2. Floor of mouth
3. Lower lip
4. Soft palate
5. Gingiva
In the early stages, cancers of the oral cavity appear
as roughened areas of the mucosa. As the lesion
enlarges, it typically appears as either an ulcer or a
protruding mass (fungating).

Microscopic features
Early there is full-thickness dysplasia (carcinoma
in situ) followed by invasion of the underlying
connective tissue stroma.
The grade varies from from well-differentiated
keratinizing to poorly differentiated.
As a group, these tumors tend to infiltrate and
extend locally before they eventually metastasize
to cervical lymph nodes and more remotely. The
most common sites of distant metastasis are
mediastinal lymph nodes, lung, liver and bones

SALIVARY GLANDS
There are three major salivary glands—parotid,
submandibular, and sublingual. Additionally, there
are numerous minor salivary glands distributed
throughout the mucosa of the oral cavity.
Xerostomia refers to dry mouth due to a lack of
salivary secretion; the causes include
1. Sjögren syndrome: an autoimmune disorder,
that is usually also accompanied by involvement of
the lacrimal glands that produces dry eyes
(keratoconjunctivitis sicca).
2. Radiation therapy

Inflammation (Sialadenitis)
Sialadenitis refers to inflammation of a salivary
gland; it may be
1. Traumatic
2. Infectious: viral, bacterial
3. Autoimmune
The most common form of viral sialadenitis is
mumps, which usually affects the parotids. The
pancreas and testes may also be involved.

Bacterial sialadenitis is seen as a complication of
1. Stones obstructing ducts of a major salivary
gland (Sialolithiasis), particularly the
submandibular.
2. Dehydration with decreased secretory
function as is sometimes occurs in
a. patients on long-term phenothiazines that
suppress salivary secretion.
b. elderly patients with a recent major thoracic
or abdominal surgery.

Unilateral involvement of a single gland is the
rule and the inflammation may be
suppurative.
The inflammatory involvement causes painful
enlargement and sometimes a purulent ductal
discharge.
Sjögren syndrome causes an immunolgically
mediated sialadenitis i.e. inflammatory
damage of the salivary tissues.

NEOPLASMS OF SALIVARY GLANDS
Neoplasms of the salivary glands (benign and
malignant) are generally uncommon, constituting
less than 2% of human tumors. We will restrict our
discussion on the more common examples.
The relative frequency distributions of these tumors
in relation to various salivary glands are as follows
Parotid gland 80%
Submandibular gland 10%
Minor salivary and sublingual glands 10%

The incidence of malignant tumors within the
glands is, however, different from the above
Sublingual tumors 80%
Minor salivary glands 50%
Submandibular glands 40%
Parotid glands 25%

These tumors usually occur in adults, with a slight
female predominance. Excluded from this rule is
Warthin tumor, which occurs much more
frequently in males than in females. The benign
tumors occur most often around the age of 50 to
60 years; the malignant ones tend to appear in
older age groups. Neoplasms of the parotid
produce distinctive swellings in front of, or below
the ear. Clinically, there are no reliable criteria to
differentiate benign from the malignant tumors;
therefore, pathological evaluation is necessary.

Pleomorphic Adenomas (Mixed Salivary Gland
Tumors)
These benign tumors commonly occur within the
parotid gland (constitute 60% of all parotid tumors).
Gross features
Most tumors are rounded, encapsulated masses.
The cut surface is gray-white with myxoid and light
blue translucent areas of chondroid.
Microscopic features
The main constituents are a mixture of ductal
epithelial and myoepithelial cells, and it is believed
that all the other elements, including mesenchymal,
are derived from the above cells (hence the name
adenoma).

The epithelial/myoepithelial components of the
neoplasm are arranged as glands, strands, or sheets.
These various epithelial/myoepithelial elements are
dispersed within a background of loose myxoid tissue
that may contain islands of cartilage-like islands and,
rarely bone.
Sometimes, squamous differentiation is present.
In some instances, the tumor capsule is focally
deficient allowing the tumor to extend as tongue-like
protrusions into the surrounding normal tissue.
Enucleation of the tumor is, therefore, not advisable
because residual foci (the protrusions) may be left
behind and act as a potential source of multifocal
recurrences.
The incidence of malignant transformation increases
with the duration of the tumor.

Warthin Tumor is the second most common salivary
gland neoplasm. It is benign, arises usually in the
parotid gland and occurs more commonly in males
than in females. About 10% are multifocal and 10%
bilateral. Smokers have a higher risk than nonsmokers
for developing these tumors. Grossly, it is round to
oval, encapsulated mass & on section display gray
tissue with narrow cystic or cleft-like spaces filled with
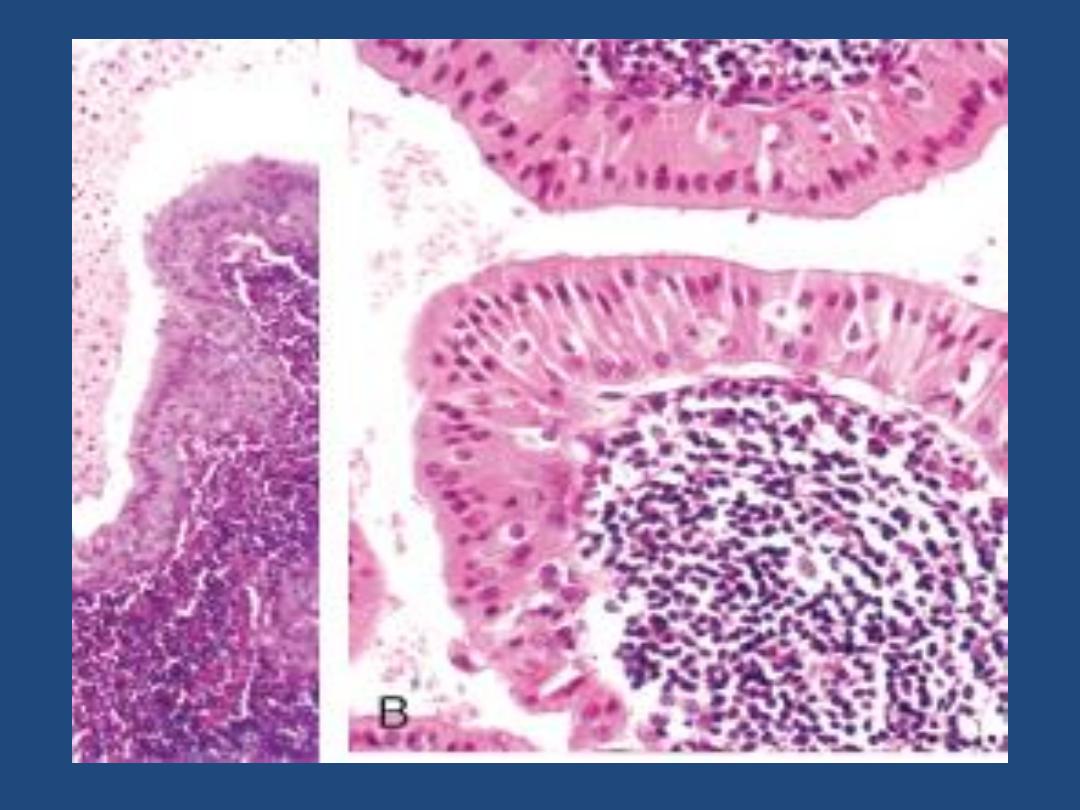
secretion. Microscopically, these spaces are lined by a
double layer of neoplastic epithelial cells resting on a
dense lymphoid stroma, sometimes with germinal
centers. This lympho-epithelial lining frequently project
into the spaces. The epithelial cells are oncoytes as
evidenced by their eosinophilic granular cytoplasm
(stuffed with mitochondria).

ESOPHAGUS
The main functions of the esophagus are to 1.
Conduct food and fluids from the pharynx to the
stomach 2. Prevent reflux of gastric contents into
the esophagus. These functions require motor
activity coordinated with swallowing, i.e. wave of
peristalsis, associated with relaxation of the LES in
anticipation of the peristaltic wave. This is followed
by closure of the LES after the swallowing reflex.
Maintenance of sphincter tone (positive pressure
relative to the rest of esophagus) is necessary to
prevent reflux of gastric contents.

CONGENITAL ANOMALIES
Several congenital anomalies affect the esophagus
including the presence of ectopic gastric mucosa &
pancreatic tissues within the esophageal wall,
congenital cysts & congenital herniation of the
esophageal wall into the thorax. The latter is due to
impaired formation of the diaphragm. Atresia and
fistulas are uncommon but must be recognized &
corrected early because they cause immediate
regurgitation, suffocation & aspiration pneumontis
when feeding is attempted. In atresia, a segment of the
esophagus is represented by only a noncanalized cord,
with the upper pouch connected to the bronchus or
the trachea and a lower pouch leading to the stomach.

Webs, rings, and stenosis
Mucosal webs are shelf-like, eccentric protrusions of the
mucosa into the esophageal lumen. These are most common
in the upper esophagus. The triad of upper esophageal web,
iron-deficiency anemia, and glossitis is referred to as Plummer-
Vinson syndrome. This condition is associated with an
increased risk for postcricoid esophageal carcinoma.
Esophageal rings unlike webs are concentric plates of tissue
protruding into the lumen of the distal esophagus. Esophageal
webs and rings are encountered most frequently in women
over age 40. Episodic dysphagia is the main symptom.
Stenosis consists of fibrous thickening of the esophageal wall.
Although it may be congenital, it is more frequently the result
of severe esophageal injury with inflammatory scarring, as
from gastroesophageal reflux disease (GERD), radiation,
scleroderma and caustic injury. Stenosis usually manifests as
progressive dysphagia, at first to solid foods but eventually to
fluids as well.

LESIONS ASSOCIATED WITH MOTOR DYSFUNCTION
Coordinated motor activity is important for proper
function of the esophagus. The major entities that
are caused by motor dysfunction of the esophagus
are
1. Achalasia
2. Hiatal hernia
3. Diverticula
4. Mallory-Weiss tear

Achalasia
Achalasia means "failure to relax." It is characterized by three
major abnormalities:
1. Aperistalsis (failure of peristalsis)
2. Increased resting tone of the LES
3. Icomplete relaxation of the LES in response to swallowing
In most instances, achalasia is an idiopathic disorder. In this
condition there is progressive dilation of the esophagus above
the persistently contracted LES. The wall of the esophagus
may be of normal thickness, thicker than normal owing to
hypertrophy of the muscular wall, or markedly thinned by
dilation (when dilatation overruns hypertrophy). The mucosa
just above the LES may show inflammation and ulceration.
Young adults are usually affected and present with progressive
dysphagia.

Complications of achalasia are
1. Aspiration pneumonitis of undigested food
2. Monilial esophagitis
3. Esophageal squamous cell carcinoma (about
5% of patients)
4. Lower esophageal diverticula

Hiatal Hernia
Hiatal hernia is characterized by separation of the
diaphragmatic crura leading to widening of the space around
the esophageal wall. Two types of hiatal hernia are
recognized:
1. The sliding type (95%)
2. The paraesophageal type
In the sliding hernia the stomach skates up through the patent
hiatus above the diaphragm creating a bell-shaped dilation. In
paraesophageal hernias, a separate portion of the stomach,
usually along the greater curvature, enters the thorax through
the widened foramen. The cause of hiatal hernia is unknown.
It is not clear whether it is a congenital malformation or is
acquired during life. Only about 10% of adults with a sliding
hernia suffer from heartburn or regurgitation of gastric juices
into the mouth. These are due to incompetence of the LES
and are accentuated by positions favoring reflux (bending
forward, lying supine) and obesity.

Complications of hiatal hernias include
1. Ulceration, bleeding and perforation (both
types)
2. Reflux esophagitis (frequent with sliding
hernias)
3. Strangulation of paraesophageal hernias

Diverticula
By definition a diverticulum is a "focal out pouching of
the alimentary tract wall that contains all or some of
its constituents"; they are divided into
1. False diverticulum is an out pouching of the mucosa
and submucosa through weak points in the muscular
wall.
2. True diverticulum consists of all the layers of the
wall and is thought to be due to motor dysfunction of
the esophagus. They may develop in three regions of
the esophagus
a. Zenker diverticulum, located immediately above the
UES
b. Traction diverticulum near the midpoint of the
esophagus
c. Epiphrenic diverticulum immediately above the LES.

Lacerations (Mallory-Weiss Syndrome)
These refer to longitudinal tears at the GEJ or
gastric cardia and are the consequence of severe
retching or vomiting. They are encountered most
commonly in alcoholics, since they are susceptible
to episodes of excessive vomiting, but have been
reported in persons with no history of vomiting or
alcoholism. During episodes of prolonged vomiting,
reflex relaxation of LES fails to occur. The refluxing
gastric contents suddenly overcome the contracted
musculature leading to forced, massive dilation of
the lower esophagus with tearing of the stretched
wall.

Pathological features
The linear irregular lacerations, which are usually
found astride the GEJ or in the gastric cardia, are
oriented along the axis of the esophageal lumen.
The tears may involve only the mucosa or may
penetrate deeply to perforate the wall.
Infection of the mucosal defect may lead to
inflammatory ulcer or to mediastinitis. Usually the
bleeding is not profuse and stops without surgical
intervention. Healing is the usual outcome. Rarely
esophageal rupture occurs.

Esophageal Varices
Portal hypertension when sufficiently prolonged or
severe induces the formation of collateral bypass veins
wherever the portal and caval venous systems
communicate. Esophageal varices refer to the
prominent plexus of deep mucosal and submucosal
venous collaterals of the lower esophagus subsequent
to the diversion of portal blood through them through
the coronary veins of the stomach. From the varices
the blood is diverted into the azygos veins, and
eventually into the systemic veins. Varices develop in
90% of cirrhotic patients. Worldwide, after alcoholic
cirrhosis, hepatic schistosomiasis is the second most
common cause of variceal bleeding.

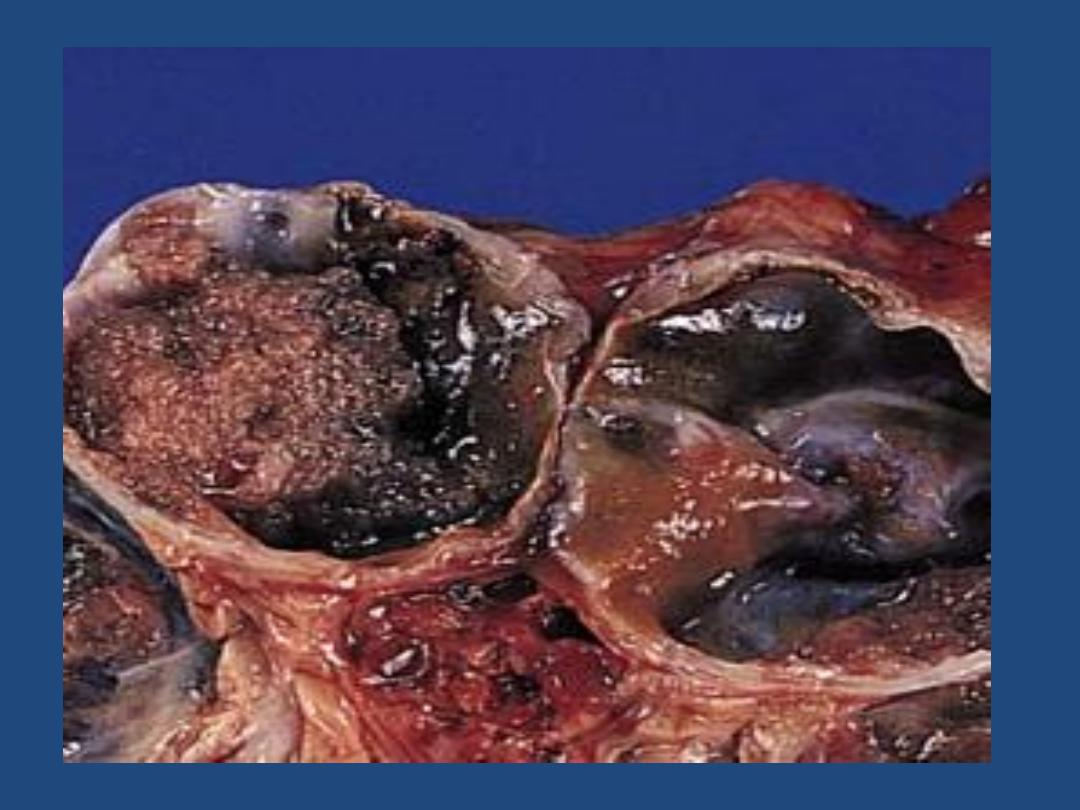
Pathological features
The increased pressure in the esophageal plexus produces
dilated tortuous vessels that are liable to rupture.
Varices appear as tortuous dilated veins lying primarily
within the submucosa of the distal esophagus and proximal
stomach.
The net effect is irregular protrusion of the overlying
mucosa into the lumen. The mucosa is often eroded because
of its exposed position.
Variceal rupture produces massive hemorrhage into the
lumen. In this instance, the overlying mucosa appears
ulcerated and necrotic.
Rupture of esophageal varices usually produces massive
hematemesis. Among patients with advanced liver cirrhosis,
such a rupture is responsible for 50% of the deaths. Some
patients die as a direct consequence of the hemorrhage
(hypovolemic shock); others of hepatic coma triggered by the
hemorrhage.

Esophagitis
This term refers to inflammation of the esophageal
mucosa. It may be caused by a variety of physical,
chemical, or biologic agents. Reflux Esophagitis
(Gastroesophageal Reflux Disease or GERD) is the
most important cause of esophagitis and signifies
esophagitis associated with reflux of gastric
contents into the lower esophagus. Many causative
factors are involved, the most important is
decreased efficacy of esophageal antireflux
mechanisms, particularly LES tone. In most
instances, no cause is identified. However, the
following may be contributatory

a. Central nervous system depressants including
alcohol
b. Smoking
c. Pregnancy
d. Nasogastric tube
e. Sliding hiatal hernia
f. hypothyroidism
g. Systemic sclerosis
Any one of the above mechanism may be the
primary cause in an individual case, but more than
one is likely to be involved in most instances. The
action of gastric juices is vital to the development of
esophageal mucosal injury.

Gross (endoscopic) features
These depend on the causative agent and on the
duration and severity of the exposure.
Mild esophagitis may appear grossly as simple
hyperemia. In contrast, the mucosa in severe
esophagitis shows confluent erosions or total
ulceration into the submucosa.
Microscopic features
Three histologic features are characteristic:
1. Inflammatory cells including eosinophils within the
squamous mucosa.
2. Basal cells hyperplasia
3. Extension of lamina propria papillae into the upper
third of the mucosa.

The disease mostly affects those over the age of 40
years. The clinical manifestations consist of
dysphagia, heartburn, regurgitation of a sour fluid
into the mouth, hematemesis, or melena. Rarely,
there are episodes of severe chest pain that may be
mistaken for a "heart attack.“
The potential consequences of severe reflux
esophagitis are
1. Bleeding
2. Ulceration
3. Stricture formation
4. Tendency to develop Barrett esophagus

Barrett Esophagus (BE)
10% of patients with long-standing GERD develop this
complication. BE is the single most important risk factor for
esophageal adenocarcinoma. BE refers to columnar
metaplasia of the distal squamous mucosa; this occurs in
response to prolonged injury induced by refluxing gastric
contents. Two criteria are required for the diagnosis of Barrett
esophagus:
1. Endoscopic evidence of columnar lining above the GEJ
2. Histologic confirmation of the above in biopsy specimens.
The pathogenesis of Barrett esophagus appears to be due to a
change in the differentiation program of stem cells of the
esophageal mucosa. Since the most frequent metaplastic
change is the presence of columnar cells admixed with goblet
cells, the term "intestinal metaplasia" is used to describe the
histological alteration.

Gross features
Barrett esophagus is recognized as a red, velvety
mucosa located between the smooth, pale pink
esophageal squamous mucosa and the light brown
gastric mucosa.
It is displayed as tongues, patches or broad
circumferential bands replacing the
squamocolumnar junction several centimeters.
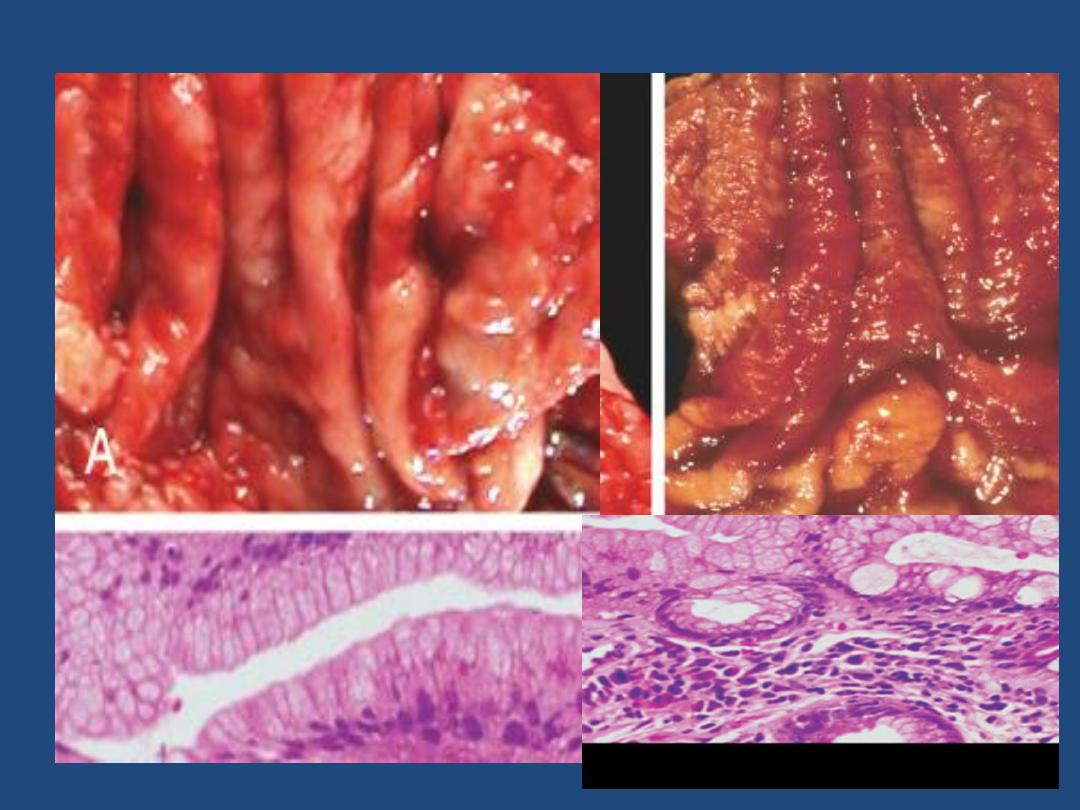

Microscopic features
the esophageal squamous epithelium is replaced by
metaplastic columnar epithelium, including interspersed
goblet cells, & may show a villous pattern (as that of the small
intestine hence the term intestinal metaplasia).
Critical to the pathologic evaluation of patients with Barrett
mucosa is the search for dysplasia within the metaplastic
epithelium. This dysplastic change is the presumed precursor
of malignancy (adenocarcinoma). Dysplasia is recognized by
the presence of cytologic and architectural abnormalities in
the columnar epithelium, consisting of enlarged, crowded,
and stratified hyperchromatic nuclei with loss of intervening
stroma between adjacent glandular structures. Depending on
the severity of the changes, dysplasia is classified as low-
grade or high-grade.

Approximately 50% of patients with high-grade
dysplasia may already have adjacent
adenocarcinoma.
Most patients with the first diagnosis of Barrett
esophagus are between 40 and 60 years. Barrett
esophagus is clinically significant due to
1. The secondary complications of local peptic
ulceration with bleeding and stricture.
2. The development of adenocarcinoma, which in
patients with long segment disease (over 3 cm of
Barrett mucosa), occurs at a frequency that is 30- to
40 times greater than that of the general
population.

Other causes of esophagitis
In addition to GERD (which is, in fact, a chemical
injury), esophageal inflammation may have many
origins. Examples include ingestion of mucosal
irritants (such as alcohol, corrosive acids or alkalis as
in suicide attempts), cytotoxic anticancer therapy,
bacteremia or viremia (in immunosuppressed
patients), fungal infection (in debilitated or
immunosuppressed patients or during broad-
spectrum antimicrobial therapy; candidiasis by far
the most common), and uremia.

TUMORS
Benign Tumors
Leiomyomas are the most common benign tumors
of the esophagus.
Malignant Tumors
Carcinomas of the esophagus (5% of all cancers of
the GIT) have, generally, a poor prognosis because
they are often discovered too late. Worldwide,
squamous cell carcinomas constitute 90% of
esophageal cancers, followed by adenocarcinoma.
Other tumors are rare.

Squamous Cell Carcinoma (SCC)
Most SCCs occur in adults over the age of 50. The
disease is more common in males than females.
The regions with high incidence include Iran &
China. Blacks throughout the world are at higher
risk than are whites.
Etiology and Pathogenesis
Factors Associated with the Development of
Squamous Cell Carcinoma of the Esophagus are
classified as

1. Dietary
Deficiency of vitamins (A, C, riboflavin, thiamine,
and pyridoxine) & trace elements (zinc)
Fungal contamination of foodstuffs
High content of nitrites/nitrosamines
Betel chewing (betel: the leaf of a climbing
evergreen shrub, of the pepper family, which is
chewed in the East with a little lime.)

2. Lifestyle
Burning-hot food
Alcohol consumption
Tobacco abuse
3. Esophageal Disorders
Long-standing esophagitis
Achalasia
Plummer-Vinson syndrome
4. Genetic Predisposition
Long-standing celiac disease
Racial disposition

The marked geographical variations in the incidence
of the disease strongly implicate dietary and
environmental factors, with a contribution from
genetic predisposition. The majority of cancers in
Europe and the United States are attributable to
alcohol and tobacco. Some alcoholic drinks contain
significant amounts of such carcinogens as
polycyclic hydrocarbons, nitrosamines, and other
mutagenic compounds. Nutritional deficiencies
associated with alcoholism may contribute to the
process of carcinogenesis.
Human papillomavirus DNA is found frequently in
esophageal squamous cell carcinomas from high-
incidence regions.

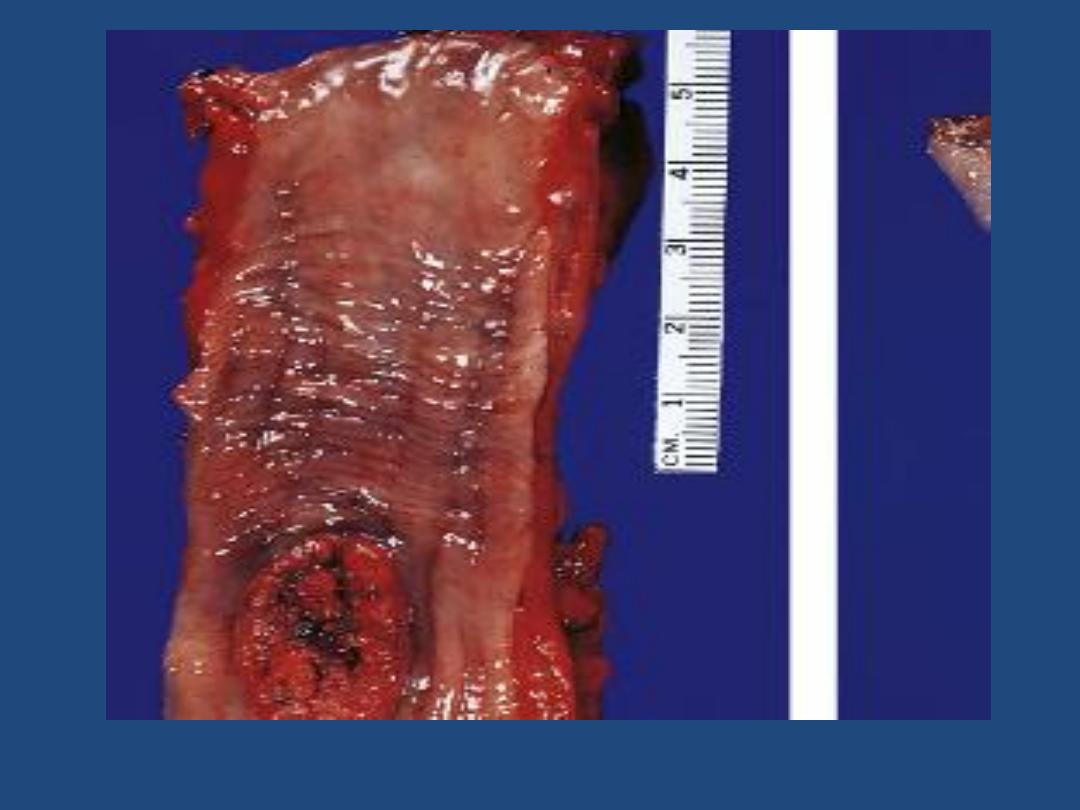
Gross features
Like squamous cell carcinomas arising in other locations,
those of the esophagus begin as in situ lesions.
When they become overt, about 20% of these tumors are
located in the upper third, 50% in the middle third, and 30%
in the lower third of the esophagus.
Early lesions appear as small, gray-white, plaque-like
thickenings of the mucosa but with progression, three gross
patterns are encountered:
1. Fungating (polypoid) (60%) that protrudes into the lumen
2. Flat (diffusely infiltrative) (15%) that tends to spread within
the wall of the esophagus, causing thickening, rigidity, and
narrowing of the lumen
3. Excavated (ulcerated) (25%) that digs deeply into
surrounding structures and may erode into the respiratory
tree (with resultant fistula and pneumonia) or aorta (with
catastrophic bleeding) or may permeate the mediastinum and
pericardium.

Local extension into adjacent mediastinal structures
occurs early, possibly due to the absence of serosa
for most of the esophagus. Tumors located in the
upper third of the esophagus also metastasize to
cervical lymph nodes; those in the middle third to
the mediastinal, paratracheal, and tracheobronchial
lymph nodes; and those in the lower third most
often spread to the gastric and celiac groups of
nodes.

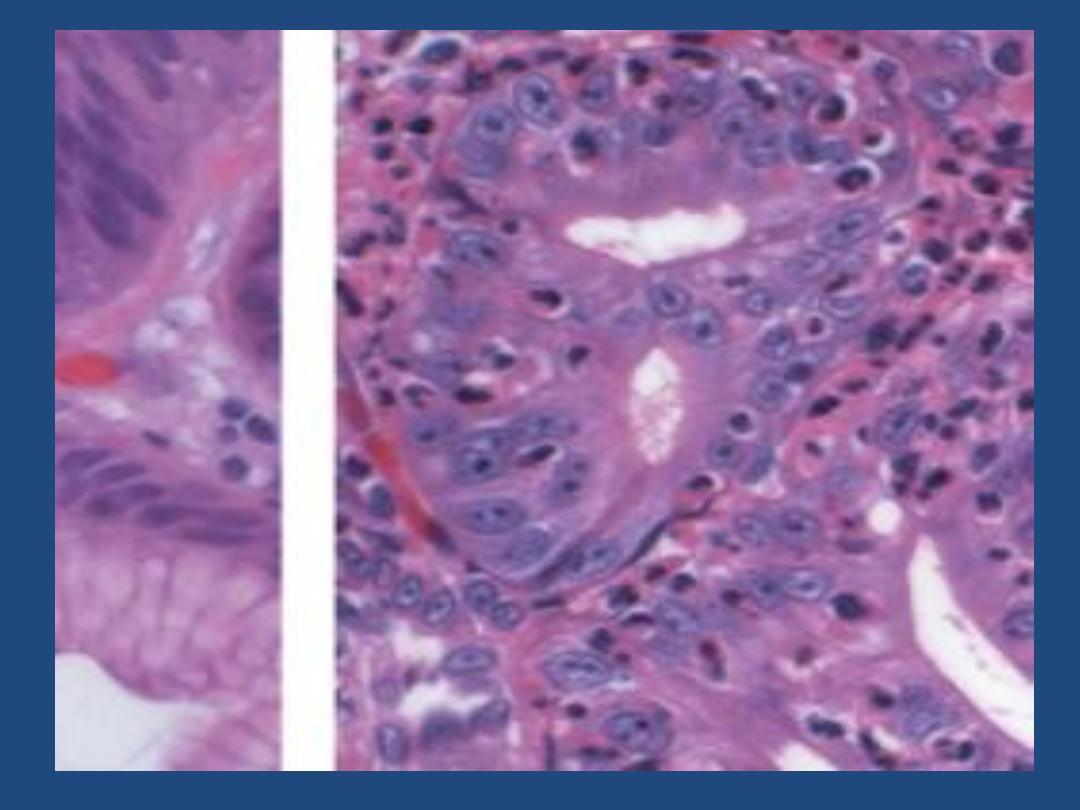
Microscopic features
Most squamous cell carcinomas are moderately to well-
differentiated,
They are invasive tumors that have infiltrated through the wall or
beyond.
The rich lymphatic network in the submucosa promotes extensive
circumferential and longitudinal spread.
Esophageal carcinomas are usually quite large by the time of
diagnosis, produces dysphagia and obstruction gradually. Cachexia
is frequent. Hemorrhage and sepsis may accompany ulceration of
the tumor.
The five-year survival rate in patients with superficial esophageal
carcinoma is about 75%, compared to 25% in patients who
undergo "curative" surgery for more advanced disease. Local
recurrence and distant metastasis following surgery are common.
The presence of lymph node metastases at the time of resection
significantly reduces survival.

Adenocarcinoma
With increasing recognition of Barrett mucosa,
most adenocarcinomas in the lower third of the
esophagus arise from the Barrett mucosa.
Etiology and Pathogenesis
These focus on Barrett esophagus. The lifetime risk
for cancer development from Barrett esophagus is
approximately 10%. Tobacco exposure and obesity
are risk factors. Helicobacter pylori infection may be
a contributing factor.

Gross features:
adenocarcinomas arising in the setting of Barrett
esophagus are usually located in the distal
esophagus and may invade the adjacent gastric
cardia.
As is the case with squamous cell carcinomas,
adenocarcinomas initially appear as flat raised
patches that may develop into large nodular
fungating masses or may exhibit diffusely infiltrative
or deeply ulcerative features.

Microscopic features
Most tumors are mucin-producing glandular
tumors exhibiting intestinal-type features.
Multiple foci of dysplastic mucosa are frequently
present adjacent to the tumor.
Adenocarcinomas arising in Barrett esophagus
chiefly occur in patients over the age of 40 years
and similar to Barrett esophagus, it is more common
in men than in women, and in whites more than
blacks (in contrast to squamous cell carcinomas).

As in other forms of esophageal carcinoma, patients
usually present because of difficulty swallowing,
progressive weight loss, bleeding, and chest pain.
The prognosis is as poor as that for other forms of
esophageal cancer, with under 20% overall five-year
survival. Identification and resection of early
cancers with invasion limited to the mucosa or
submucosa improves five-year survival to over 80%.
Regression or surgical removal of Barrett esophagus
has not yet been shown to eliminate the risk for
adenocarcinoma.