Infection Control And Sterilization In Dentistry
Dr. Huda YasirRATIONALE FOR INFECTION CONTROL
Microorganisms can spread from one person to another via direct contact, indirect contact, droplet infection and airborne infection.Direct contact occurs by touching soft tissues or teeth of patients. It causes immediate spread of infection by the source.
Indirect contact results from injuries with contaminated sharp instruments, needle stick injuries or contact with contaminated equipment and surfaces.
Droplet infection occurs by large particle droplets spatter which is transmitted by close contact. Spatter generated during dental procedures may deliver microorganisms to the dentist.
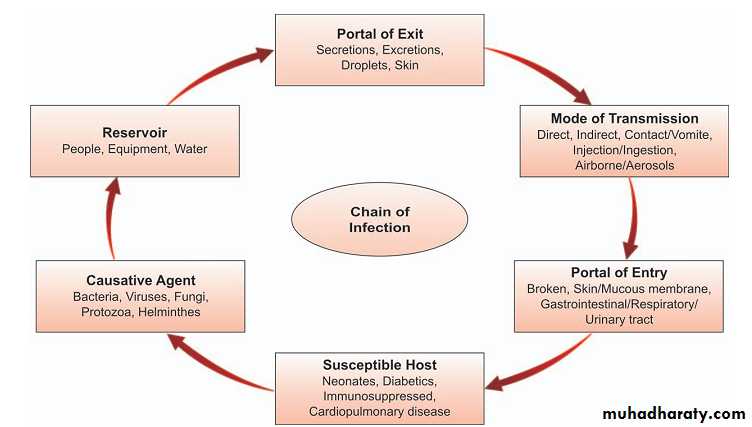
CROSS-INFECTION
Cross-infection is transmission of infectious agents among patients and staff within a clinical environment.Different Routes of Spread of Infection
PatientDHCP
DHCP
Patient
Patient
Patient
Dental office to community
Community to patientOBJECTIVE OF INFECTION CONTROL
The main objective of infection control is elimination or reduction in spread of infection from all types of microorganisms.Basically two factors are important in infection control:
Prevention of spread of microorganisms from their
hosts.
Killing or removal of microorganisms from objects and
surfaces.
STANDARD PRECAUTIONS
The Same Procedures Are Used For All Patients
Assume all patients are potentially infectious
Infection control policies are determined by the procedure, not the patientUNIVERSAL PRECAUTIONS
These are as follows:• Immunization
• Use of personal protective barrier techniques
• Maintaining hand hygiene.
• IMMUNIZATION:
• all members of the dental team (who are exposed to blood or blood contaminated articles) should be vaccinated against hepatitis B.Personal Protection Equipment :
Barrier TechniqueThe use of barrier technique is very important, which includes gown, face mask, protective eyewear and gloves
Gloves
Do not wash gloves before use or for reuseRemove gloves that are cut, torn, or punctured
Hand Hygiene:
For most routine dental procedures washing hands with plain, non-antimicrobial soap is sufficient.
For more invasive procedures, such as cutting of gum or tissue, hand antisepsis with either an antiseptic solution or alcohol-based handrub is recommended.
Definitions
Cleaning: It is the process which physically removes contamination but does not necessarily destroy microorganisms. It is a prerequisite before decontamination by disinfection or sterilization of instruments since organic material prevents contact with microbes, inactivates disinfectants.Disinfection: It is the process of using an agent that destroys germs or other harmful microbes or inactivates them. Disinfectant: It is a chemical substance, which causes disinfection. It is used on non-vital objects to kill surface vegetative pathogenic organisms, but not necessarily spore forms or viruses.
Antisepsis: It is the destruction of pathogenic micro-organisms existing in their vegetative state on living tissue. Antiseptic: It is a chemical applied to living tissues, such as skin or mucous membrane to reduce the number of microorganisms present
Sterilization: Sterilization involves any process, physical or chemical, that will destroy all forms of life, including bacterial, fungi, spores and viruses.
STERILIZATION AND DISINFECTION OF DENTAL INSTRUMENTS
DENTAL INSTRUMENTSCLASSIFICATION BASED ON
RISK OF TRANSMISSION AND NEED OF STERILIZATION
-CRITICAL
-SEMI-CRITICAL-NON-CRITICAL
CRITICAL INSTRUMENTS
Penetrate MUCOUS MEMBRANES or CONTACT BONE, BLOODSTREAM, or other normally sterile tissues
HEAT STERILIZE between uses or use sterile single-use, DISPOSABLE devices
Examples include SURGICAL INSTRUMENTS,SCALPEL BLADES, PERIODONTAL SCALERS, AND SURGICAL DENTAL BURS
SEMI-CRITICAL INSTRUMENTS
Contact MUCOUS MEMBRANES but do NOT PENETRATE SOFT TISSUEHEAT STERILIZE or HIGH-LEVEL DISINFECT
Examples: DENTAL MOUTH MIRRORS, AMALGAM CONDENSERS, AND DENTAL HANDPIECESNONCRITICAL INSTRUMENTS AND DEVICES
Contact intact SKIN
Clean and disinfect using a LOW TO INTERMEDIATE LEVEL DISINFECTANT
Examples: X-RAY HEADS, FACEBOWS, PULSE OXIMETER, BLOOD PRESSURE CUFFThe accepted methods of sterilization in our dental practice are:
• Moist/steam heat sterilization• Dry heat sterilization
• Chemical vapor pressure sterilization
4. Ethylene oxide sterilization.
• Moist/steam heat sterilization
• AUTOCLAVE• Sterilization with Steam Under Pressure
• Time required at 1210 C is 15 mins at 15 psi of pressure.
• Advantages
1. Time efficient.2. Good penetration.3. The results are consistently good and reliable.4. The instruments can be wrapped prior
to sterilization.
• Disadvantages
• Blunting and corrosion of sharp instruments.
2. Damage to rubber goods.
• Dry heat sterilization
• Conventional dry heat ovens:• Achieved at temperature above 1600 C
for 2 hours
Advantages of dry heat sterilization
• No corrosion is seen in carbon-steel instruments and burs• Maintains the sharpness of cutting instruments
• Low cost of equipment
Disadvantages
• Long cycle is required because of poor heat conduction and poor penetrating capacity• High temperature may damage heat sensitive items
such as rubber or plastic goods
• Generally not suitable for handpieces
• 3.Chemical vapor pressure sterilization
• Chemiclaving• Operates at 1320 C and 20 lbs of
pressure for 30 minutes.
• Active ingredient – 0.23% Formaldehyde
• Advantages
• Carbon steel and other carbon sensitive burs, instruments
• and pliers are sterilized without rust or corrosion
• Disadvantages
• Items sensitive to elevated temperature will be damaged
• Instruments must be very lightly packed.
• Towel and heavy clothing cannot be sterilized.
•
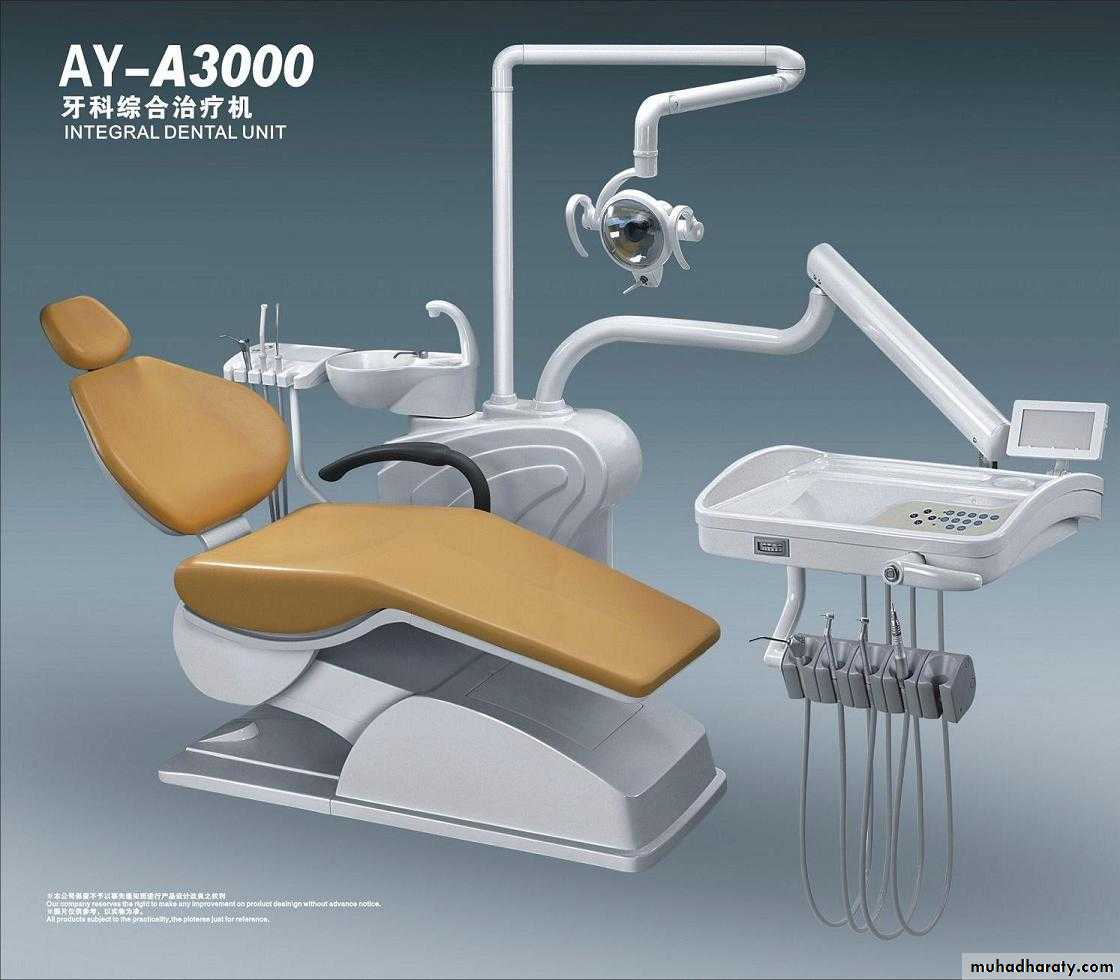
DISINFECTION OF DENTAL UNIT AND ENVIRONMENTAL SURFACES
DENTAL UNIT
Cleaned by DISPOSIBLE TOWELINGEPA-ENVIRONMENTAL PROTECTIVE AGENCY
use an EPA registered hospital disinfectantCleaning Agents Like
PHENOLICS, IODOPHORS, CHLORINE containing compoundsENVIRONMENTAL SURFACES
• CLINICAL CONTACT SURFACES• High potential for DIRECT CONTAMINATION from spray or spatter or by contact with gloved hand.
• HOUSEKEEPING SURFACES
• Do not come into contact with patients or devices
• LIMITED RISK of disease transmission
CLINICAL CONTACT SURFACES
CLEANING CLINICAL CONTACT SURFACES
• Risk of transmitting infections greater than for housekeeping surfaces.• Surface barriers can be used and changed between patients.
• OR
• Clean then disinfect using an EPA-registered low- (HIV/HBV claim) to intermediate-level (tuberculocidal claim) hospital disinfectant.
HOUSEKEEPING SURFACES
Cleaning Housekeeping Surfaces
• Routinely clean with SOAP AND WATER or an EPA-REGISTERED DETERGENT/HOSPITAL DISINFECTANT routinely• Clean MOPS AND CLOTHS and allow to dry thoroughly before re-using.
• Prepare FRESH CLEANING AND DISINFECTING SOLUTIONS daily and per manufacturer recommendations.
THE END