Childhood
Immunization
Dr.Mazin Al-Jadiry
Sept. 29, 2014
Summary of lecture 1
Passive immunity:
Ready-made immunity provided by
giving pre-formed antibodies
Active immunity: Immunity induced by giving a
preparation of antigens to stimulate a
protective immune response with
specificity and memory to a particular
infectious agent, e.g. a bacteria, virus
or toxin
Live Attenuated Vaccines
Advantage
n
Potent, response close to
the optimal naturally
acquired immune
response
Disadvantage
n
May reproduce features
of the disease as sub-
clinical or mild form of the
infection
n
May revert to virulent
form (e.g. OPV)
n
Cannot be given to
immunosuppressed or
pregnant patients
Inactive Vaccines
Advantages
n
Cannot cause infection
n
Can be given to
immunosuppressed and
pregnant individuals
Disadvantages
n
Less immunogenic and
require addition of
adjuvants and booster
doses

Why do we need to give booster doses?
To boost individual immunity
To maintain herd immunity

Learning objectives
n
To know the Iraqi immunization schedule
n
To understand the details of each vaccine (type,
route, doses, side effects)
n
To recognize the differences between two types
of polio vaccine
n
To understand what to check before giving
vaccine

Vaccination schedule in Iraq
At birth: BCG, OPV-0, HBV-1
2 months completed: Pentavalent vaccine (DTP-1, Hib1, & HBV-
2), OPV1 and Rotavirus1.
4 months completed: Quadruple vaccine (DTP-2, and Hib2)
OPV2 and Rotavirus2.
6 months completed: Pentavalent vaccine (DTP-3, Hib3, and
HBV-3), OPV3 and Rotavirus3.
9 months completed: Measles
15 months completed: MMR1
18 months completed: Quadruple vaccine (DTP, and Hib) OPV.
(booster no.1)
4-6 years: DTP, OPV (booster no.2) and MMR2

Risk of diseases
n
Hib
– inflammation of brain, throat swelling and suffocation, pneumonia,
infection, death
n
Diphtheria
– growth in throat and suffocation, paralysis, death (in 7% of
cases)
n
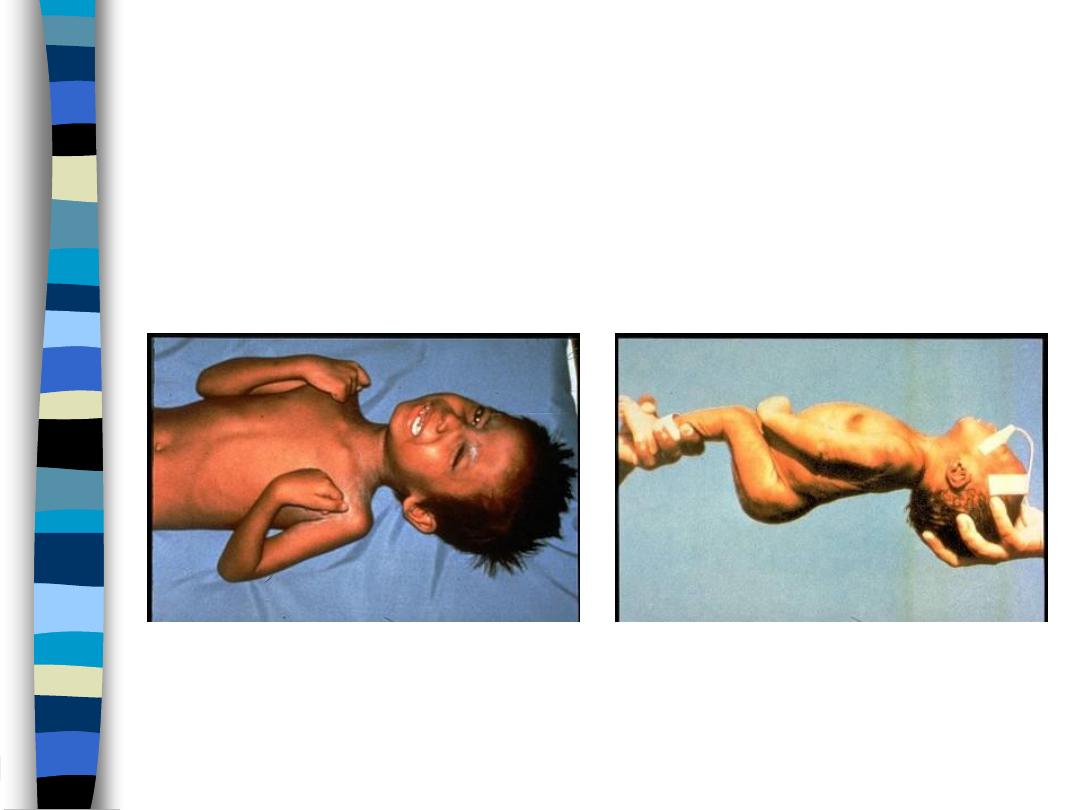
Tetanus
– muscle spasms, breathing problems, convulsions, death if
untreated
n
Whooping Cough
– coughing fits, convulsions, coma, brain damage,
death
n
Polio
– Fever, vomiting, muscle stiffness, nerve damage, muscle
paralysis, death if lung muscles paralysed
n
Measles
– High fever, cough, conjunctivitis, red rash, pneumonia,
inflammation of brain, brain damage, death
n
Mumps
– fever, infection of salivary glands, deafness, swollen testicles
(in males), infertility, brain inflammation
n
Rubella
– swollen glands, joint pain, rash, birth defects in unborn
children
– including blindness, deafness, mental retardation
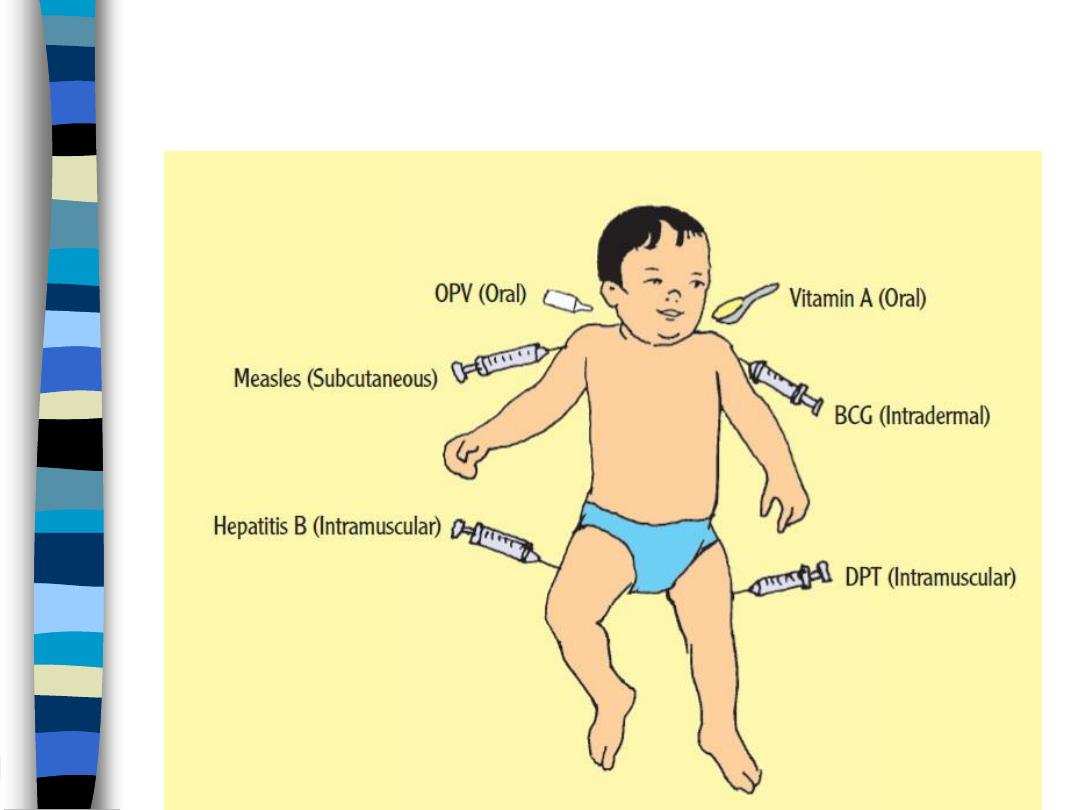
Bacille Calmette-Guẻrin (BCG) vaccine
n
The
live attenuated strain
of
Mycobacterium bovis
known as
bacillus Calmette-Guérin (BCG)
uses
shared antigens
to
stimulate the development of
cross-immunity to
Mycobacterium tuberculosis.
Bacille Calmette-Guẻrin (BCG) vaccine
n
No prevention of tuberculosis.
n
BCG Prevents dissemination of the
bacterium or the development of other
life-threatening complications such as
meningitis.
n
BCG is effective at reducing morbidity
and mortality in children but is less
useful in the prevention of adult
respiratory disease

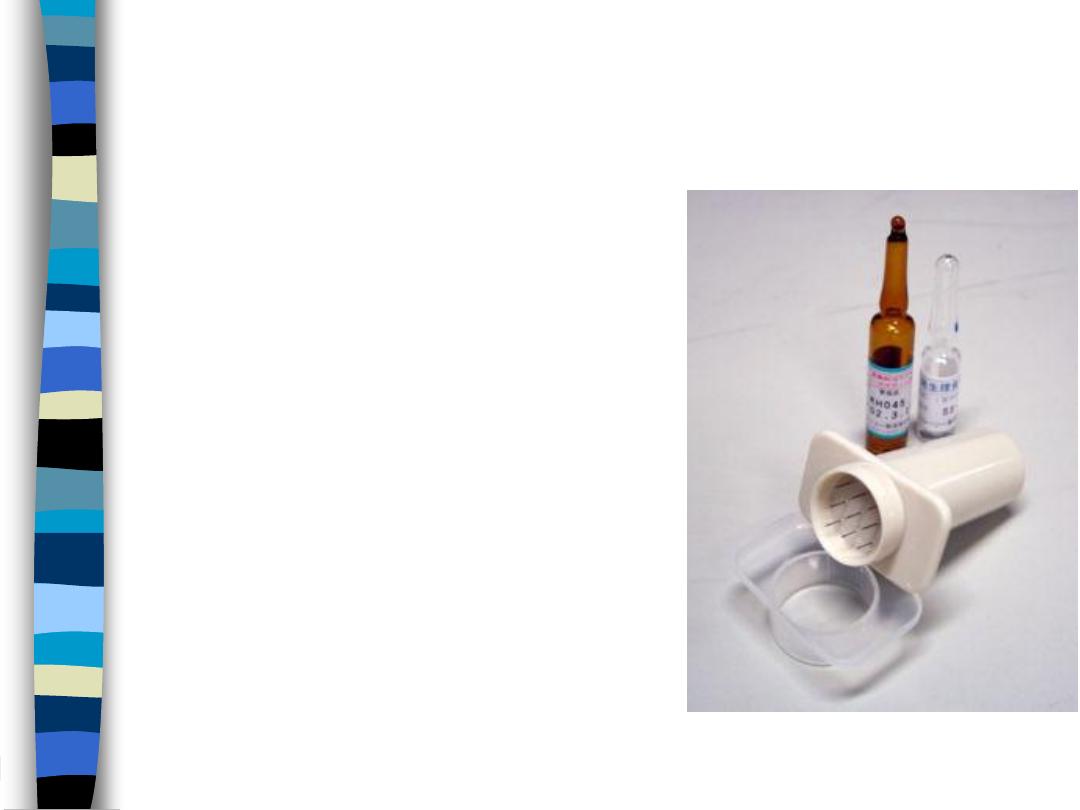
Method of administration
n
BCG is given as a
single intra-dermal
injection at the
insertion of the deltoid into the lateral aspect of the left
upper arm.
n
The insertion of deltoid is most frequently used because
the local complication rate is smallest when that site is
used.
n
13 years old
n
Male
n
Left deltoid
BCG
BCG vaccine complications:
n
Local ulceration and regional suppurative adenitis occur in
0.1-1% of vaccine recipients
n
Keloids; large, raised and ugly scars.
n
If BCG is accidentally given to an immunocompromised
patient, it can cause disseminated or life threatening
infection
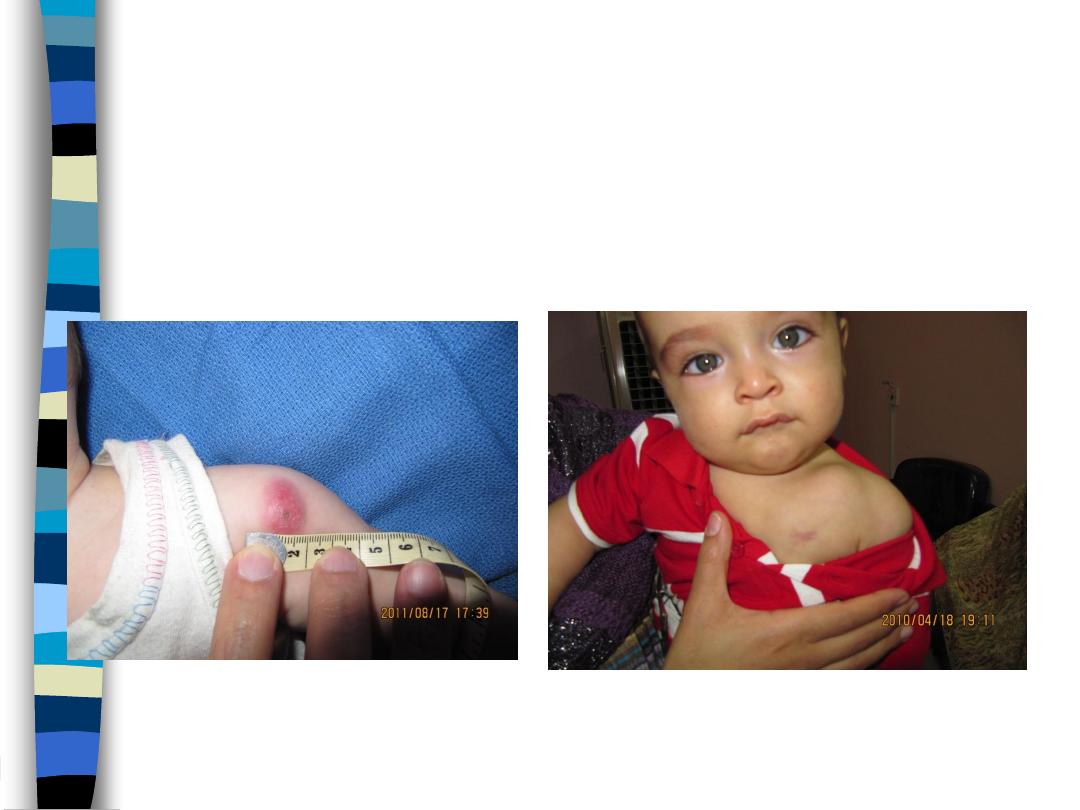
Local ulceration
Lymphadenitis
BCG side effects

Poliovirus
n
Enterovirus (RNA), Three serotypes: 1, 2, 3
n
Human is the reservoir,
n
Transmission by fecal-oral or possible oral-oral,
n
Communicability 7-10 days before onset,
n
The virus present in stool for 3-6 weeks.

Poliovirus
n
Entry into mouth
• Replication in pharynx, GI tract, local lymphatics
• Hematologic spread to lymphatics and central
nervous system
• Viral spread along nerve fibers leads to Destruction
of motor neurons
0
20
40
60
80
100
Percent
Asymptomatic
Minor non-CNS illness
Aseptic menigitis
Paralytic
Most poliovirus infections are asymptomatic
Outcomes of Poliovirus Infection

Wild Poliovirus 1988
Outcomes of Poliovirus Infection

Infection <2,000
Wild Poliovirus 2008

Salk’s Polio vaccine
n
" Inactivated Polio Vaccine" IPV
n
Contains 3 serotypes of vaccine virus
n
The injected Salk vaccine confers IgG-mediated immunity
in the bloodstream, which prevents polio infection from
progress to viremia and protects the motor neurons, thus
eliminating the risk of bulbar polio and post-polio
syndrome.

Pros and Cons of Salk’s Polio vaccine
n
It offers
no protection to the mucosal lining of the
intestine
, ie; people vaccinated with Salk's vaccine can
still carry the disease and spread it to unvaccinated
individuals.
n
IPV has essentially no adverse effects associated with it
other than possible rare hypersensitivity reactions.
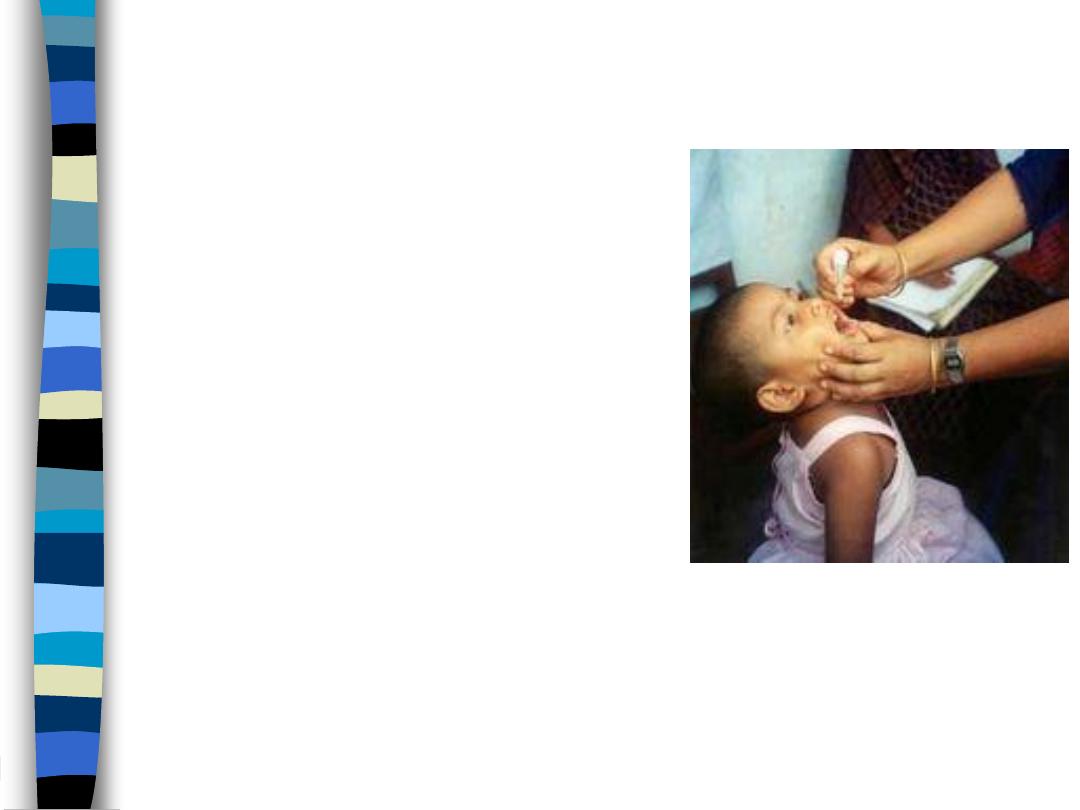
Sabin’s Polio vaccine
n
Sabin's “Oral Polio Vaccine" is a
live-attenuated vaccine;
n
Contains 3 serotypes of vaccine
virus
n
It replicates very efficiently in the
gut, the primary site of infection
and replication,
n
Unable to replicate efficiently
within nervous system tissue.
n
Shed in stool for up to 6 weeks
following vaccination

Pros and Cons of Oral Polio Vaccine
n
The OPV proved to be
superior
in administration, and also
provided
longer lasting
immunity than the Salk vaccine.
n
The trivalent Oral Polio Vaccine (Sabin) on very rare
occasions has been associated with
paralysis
(vaccine-
associated paralytic poliomyelitis, about 1 case per 750,000
vaccine recipients).

If your child miss Polio vaccines

Diphtheria
n
Aerobic gram-positive bacillus; Clostridium diphtheriae
n
Complication most attributable to toxin
n
Severity generally related to extent of local disease
n
Most common complications are myocarditis and neuritis,
death occurs in 5%-10% for respiratory disease
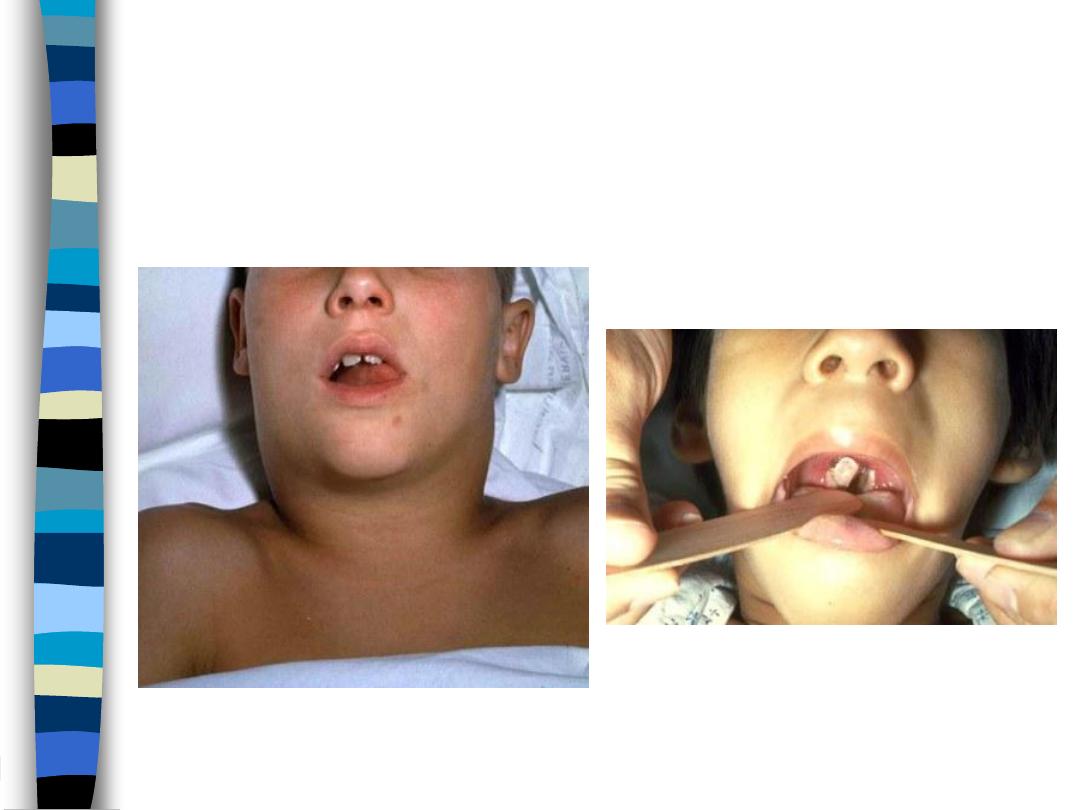
Diphtheria

Tetanus
n
Caused by Anaerobic gram-positive spore-forming
bacteria; Clostridium tetani, Spores found in soil, animal
feces.
n
Tetanus Complications:
– Laryngospasm,
– Aspiration pneumonia and
– Death
Tetanus

Gram-positive, rod-shaped,
obligate anaerobic bacterium
Clostridium tetani.
Source of infection
Tetanus

Pertussis
n
Highly contagious respiratory infection caused by
Bordetella pertussis
n
Complication: Pneumonia, Seizures, Encephalopathy
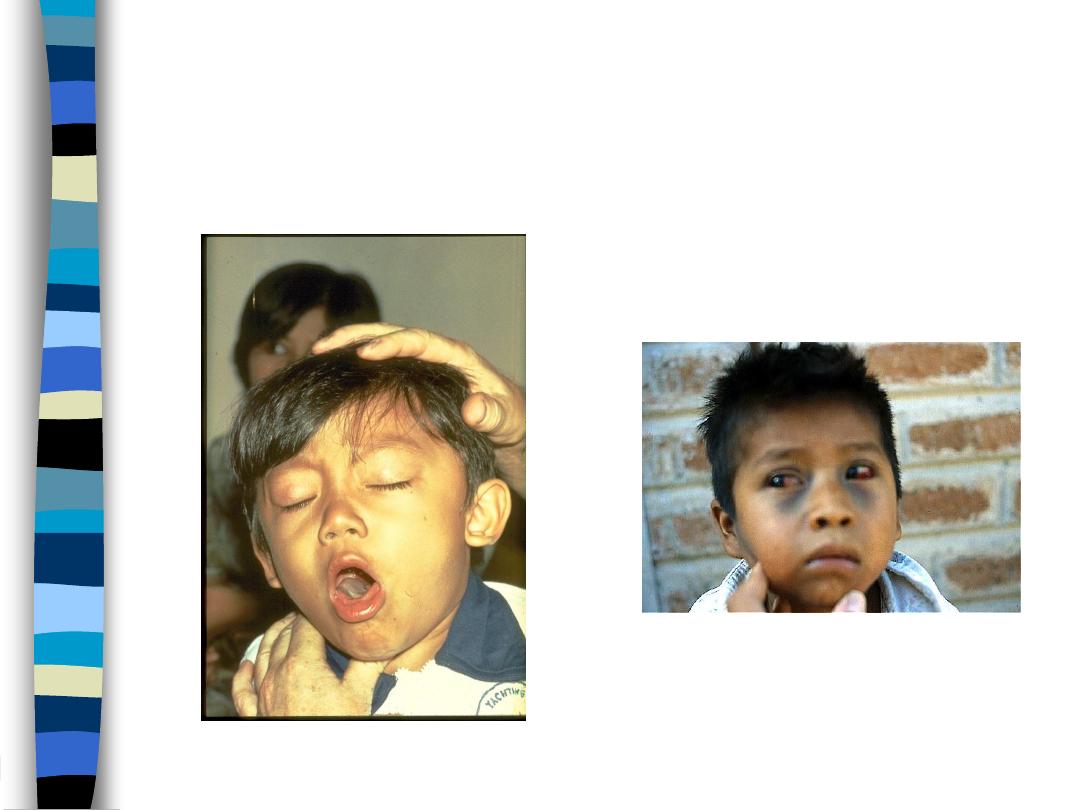
Pertussis
Child with subconjunctival hemorrhage and
bruising on face due to pertussis coughing
Child has pertussis difficult for him to stop
coughing and to get air

DPT
n
DPT is a mixture of three vaccines, to immunize against
Diphtheria, Pertussis, and Tetanus.
n
DTP is administered intramuscularly, five vaccinations
before age 7 years (at 2, 4, 6, and 15–18 months and at 4–
6 years)
DPT complication
n
Minor reactions are quite frequent in 20–50% of vaccines.
Local reactions include: Inflammation, induration or a
painless nodule at the site of injection. These are
progressively more common after the first injection
n
Moderate reaction occur in 0.1% to 1.0% of children and
include:
– ongoing crying (for 3 hours or more in the first 12 hs)
– a high fever (up to 40°C), and
– an unusual (screaming), high-pitched crying

DPT complication
n
Severe problems happen very rarely (1 in 140,000 doses
of DPT). Include;
– a serious allergic reaction,
– prolonged seizures,
– encephalopathy, or even death

Measles
Paramyxovirus (RNA)
Diarrhea
Otitis media
Pneumonia
Encephalitis and Death

MMR
n
Three live attenuated vaccines (Measles, Mumps &
Rubella)
n
Subcutaneous in two doses
n
The first MMR dose is recommended at age 12 to 15
months and the second at the child's entry into school
(age 4 to 6 years)
n
The purpose of the rubella portion of this vaccine is to
protect against congenital rubella syndrome by
preventing the occurrence of rubella, which, by itself, is a
mild disease.

MMR
n
Because MMR is a live-attenuated vaccine, non–allergy-
related side effects are noted 5 to 12 days following
immunization.
– Fever and rash are relatively common, experienced by
5% to 15% of recipients.
– Transient arthritis has been reported.
– Thrombocytopenia (rare)
– Encephalopathy (very rare)
n
About 10% of children get a rash approximately 10 days
after vaccine administration.

MMR Vaccine
Contraindications and Precautions
n
Severe allergic reaction to vaccine component or
following prior dose
n
Pregnancy
n
Immunosuppression
n
Moderate or severe acute illness
n
Recent blood product

Hepatitis B vaccine
n
Hepatitis B vaccine consists of purified HBsAg particles
produced through recombinant DNA technology in yeast.
n
Vaccine usually is given intramuscularly as a three-dose
series, the second and third doses given 1 and 6 months,
respectively, after the first dose (0, 1, 6).
n
Three doses induce seroconversion in 90-95% of healthy
infants, children and adults.

Rotavirus vaccine
n
In early childhood, the single most important cause of
severe dehydrating diarrhea is rotavirus infection.
n
Rotaviruses; Reoviridae family
n
The Pentavalent vaccine protects against rotavirus
gastroenteritis.
n
Live attenuated rotavirus vaccine
n
Oral route
n
Three doses; 2,4, and 6 months.
Haemophilus influenzae type b
n
Severe pneumonia
n
Meningitis and
n
Other invasive diseases
n
15% to 30% of children who survive Hib meningitis may
develop permanent neurological disability, including brain
damage, hearing loss, and mental retardation
n
5% to 10% cases of Hib meningitis are at risk of dying.
Almost exclusively in
children aged < 5 yrs

Haemophilus influenzae type b vaccine
n
Type of vaccine: Conjugate
n
Number of doses: three doses (2,4,6 months) and a
booster shot at 18 months.
n
Adverse reactions: Mild local reaction
n
Injection site: Outer mid-thigh for infants.
n
Injection type: Intramuscular
n
Given as quadruple or pentavalent vaccine
Immunodeficiency
n
Live-bacteria (e.g., oral typhoid) and live-virus vaccines
(e.g., MMR, varicella, and rotavirus) are contraindicated in
most circumstances involving clinically significant
immunosuppression

Vaccination checklist
n
Be sure to ask these questions before giving the vaccines:
n
Is your child sick today? (more than a common cold, earache, etc.)
n
Does your child have any severe (life-threatening) allergies?
n
Has your child ever had a severe reaction after a vaccination?
n
Does your child have a weakened immune system (because of
diseases such as cancer, or medications such as steroids)?
n
Has your child gotten a transfusion, or any other blood product,
recently?
n
Has your child ever had convulsions or any kind of nervous system
problem?
n
Does your child not seem to be developing normally?

Vaccination schedule in Iraq
At birth: BCG, OPV-0, HBV-1
2 months completed: Pentavalent vaccine (DTP-1, Hib1, and
HBV-2), OPV1 and Rotavirus1.
4 months completed: Quadruple vaccine (DTP-2, and Hib2)
OPV2 and Rotavirus2.
6 months completed: Pentavalent vaccine (DTP-3, Hib3, and
HBV-3), OPV3 and Rotavirus3.
9 months completed: Measles
15 months completed: MMR1
18 months completed: Quadruple vaccine (DTP, and Hib) OPV.
(booster no.1)
4-6 years: DTP, OPV (booster no.2) and MMR2
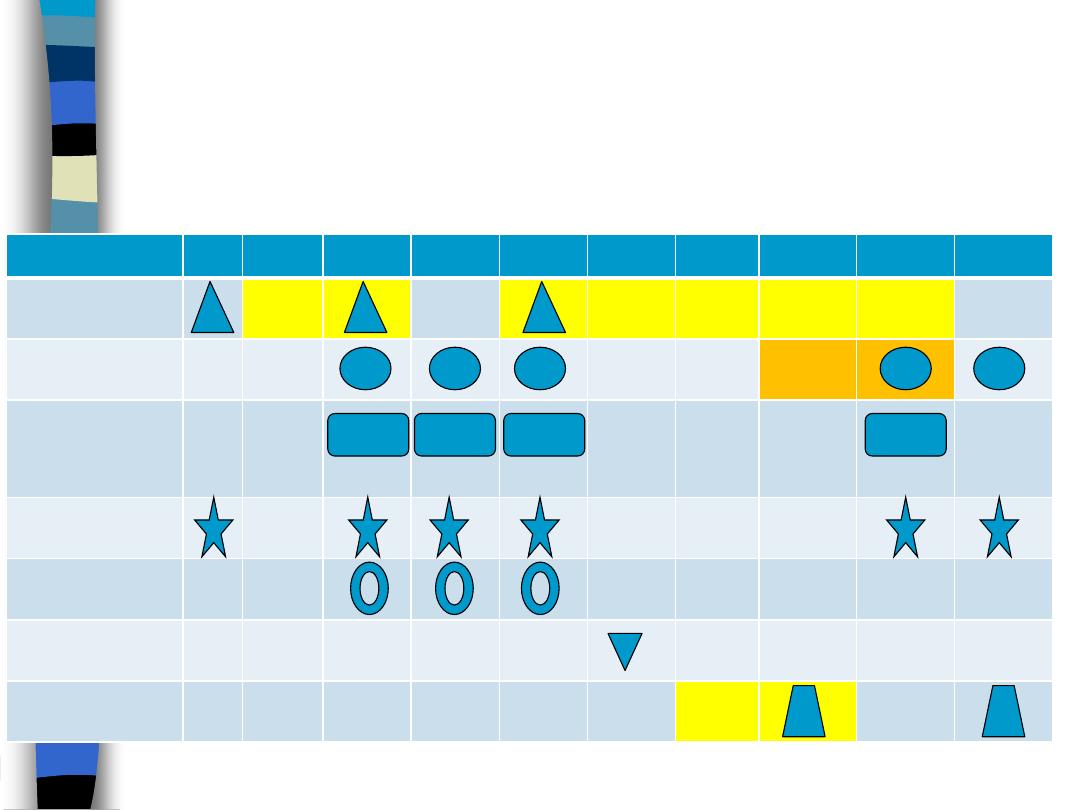
Vaccination schedule in Iraq
vaccine
B
1m
2m
4m
6m
9m
12m 15m
18m
4-6y
Hepatitis B
DTP
Haemophilus
influenzae
type b
OPV
Rotavirus
Measles
MMR
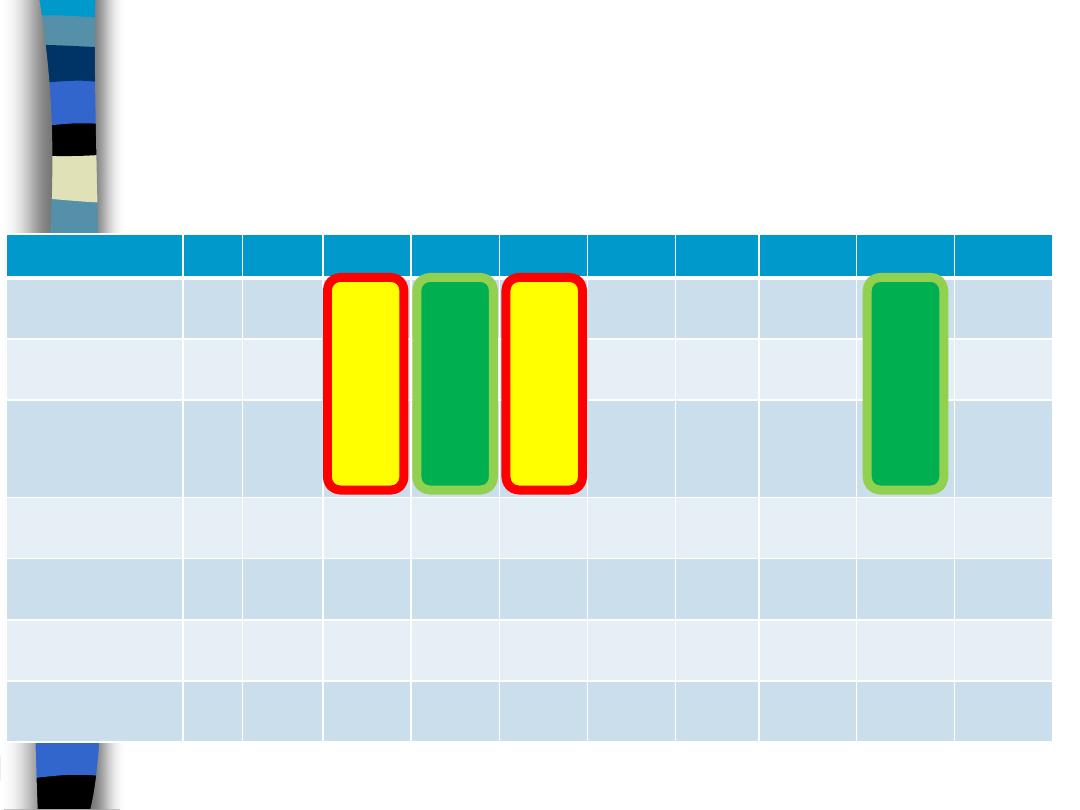
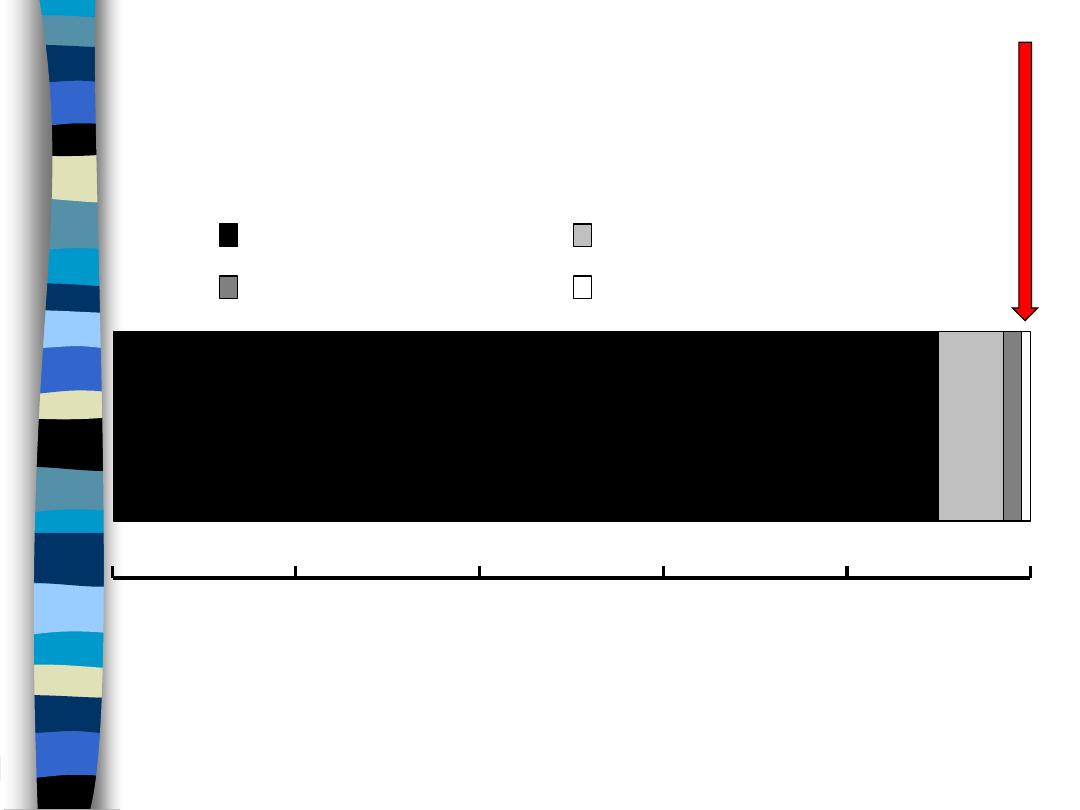
Vaccination schedule in Iraq
vaccine
B
1m
2m
4m
6m
9m
12m 15m
18m
4-6y
Hepatitis B
▲
▲
▲
DTP
▲ ▲ ▲
▲ ▲
Haemophilus
influenzae
type b
▲ ▲ ▲
▲
OPV
▲
▲ ▲ ▲
▲ ▲
Rotavirus
▲ ▲ ▲
Measles
▲
MMR
▲
▲
Pen
ta
va
le
nt
Pen
ta
va
le
nt
Quad
ru
pl
e
Quad
ru
pl
e
Thank you
Rota &
Hib
MMR



