
CONNECTIVE TISSUE DISEASES (CTD)s
Lecture one
Prof Sami Salman, FRCP, MRCP, DMR, CES, MB ChB
College of Medicine
University of Baghdad

12-Oct-15
Connective Tissue Diseases SSalman
2

By the end of these two lectures, the student will be able
to:
Describe briefly the pathophysiology of SLE, Systemic
Sclerosis, Sjogren’s and Polymyositis known as
(Connective tissue diseases (CTDs)).
List the common causes, clinical features and how to
diagnose SLE. Have a good idea as to how this condition
can be managed.
Have a good idea on the clinical features and how to
diagnose Systemic sclerosis. Have a good knowledge as to
how this condition can be managed.
Have a good idea on the clinical features and how to
diagnose Polymyositis and Dermatomyositis. Have a good
knowledge as to how this condition can be managed.
Objectives
12-Oct-15
Connective Tissue Diseases SSalman
3

Systemic Lupus Erythematosus
(SLE)
12-Oct-15
Connective Tissue Diseases SSalman
4

Patient
14 year old girl
Presented 2 months previously with dyspnoea
and chest pain.
Initially treated as pneumonia
Progressed to ICU admission
5 seizures in ward (started on phenytoin)
No history of medicines, allergies, family risk
12-Oct-15
Connective Tissue Diseases SSalman
5

History continued
Admitted to Medical City (Baghdad Teaching Hospital)
Blood tests done, started on prednisone
Referred to Renal Clinic for renal biopsy
12-Oct-15
Connective Tissue Diseases SSalman
6

On Examination
Weight: 44,7 kg (25
th
)
Height: 160 cm (75
th
)
Apyrexial, RR 18, HR 119, BP 96/70
Marfanoid habitus, rash on face and body
Not anaemic, no oedema, shotty cervical
glands
CVS: tachycardic
Resp, Abdo, neuro, ENT: normal
Musculo-skeletal: Marfanoid. No arthritis
12-Oct-15
Connective Tissue Diseases SSalman
7

12-Oct-15
Connective Tissue Diseases SSalman
8

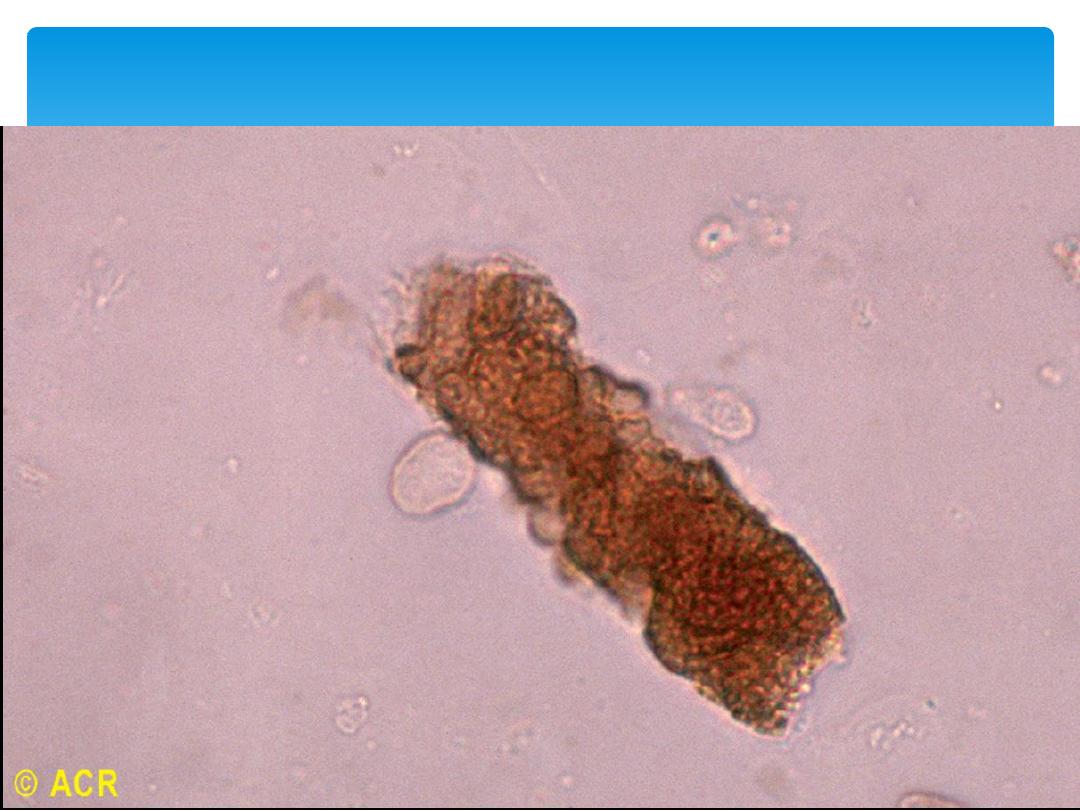
Urine
4+ haemoglobin
, no protein
Red cells
and
granular casts
+
Lab: 18 000 leukocytes
< 1000 RBC’s
Epithelial cells
Gram negative bacilli
12-Oct-15
Connective Tissue Diseases SSalman
9

Laboratory investigations
Hb
11
(MCV 90.6), Plt
200 000
WCC 5.6 (N61%, M4%, L35%)
U+E: normal
ESR
36
, CRP 2.7
INR, PTT, CK, Cholesterol, WR: normal
12-Oct-15
Connective Tissue Diseases SSalman
10

Results from clinic
ANA, ANF, Anti-Sm, Anti dsDNA, Ro, La
Positive
Low
C3, C4
12-Oct-15
Connective Tissue Diseases SSalman
11

Special investigations
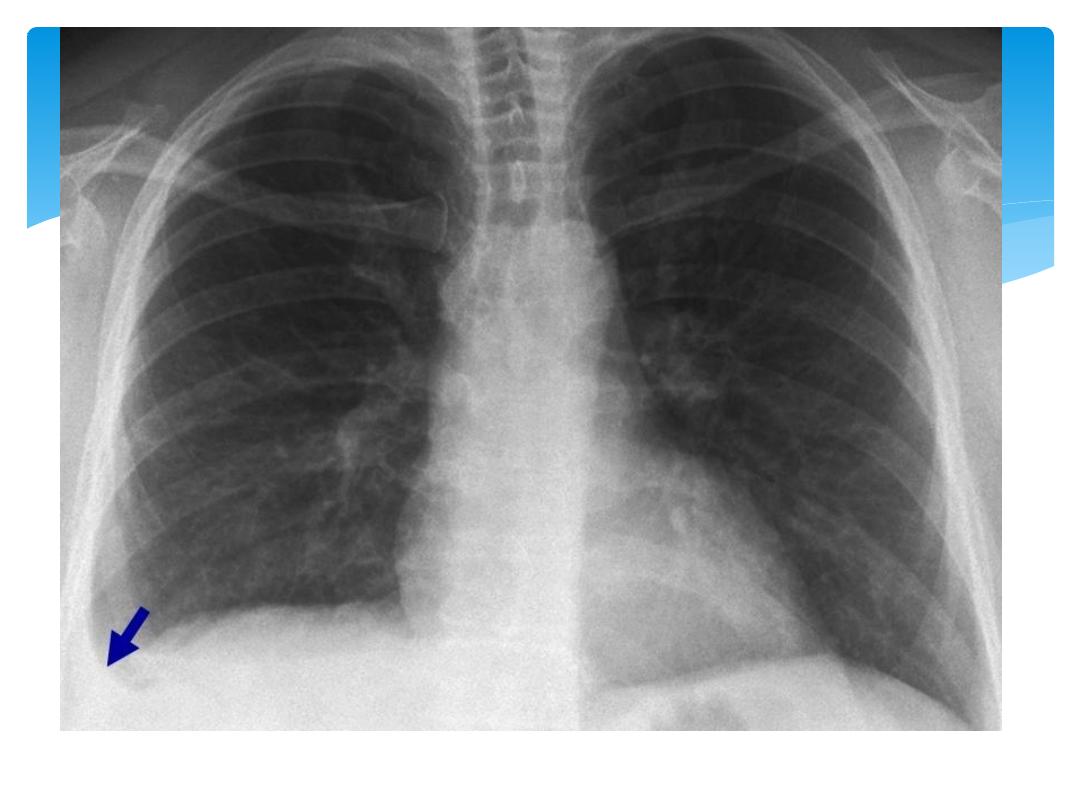
CXR: - residual Pleural effusion in R Lower
recess - Heart size normal
ECG: normal
Echo: pending
12-Oct-15
Connective Tissue Diseases SSalman
12
12-Oct-15
Connective Tissue Diseases SSalman
13

Introduction to SLE
Auto-immune disorder
Multisystem microvascular inflammation
Formation of autoantibodies
Chronic with relapsing and remitting
course
12-Oct-15
Connective Tissue Diseases SSalman
14

Pathophysiology
Mechanism for autoantibodies:
Defect in apoptosis
↑cell death → disturbance in immune tolerance
Plasma + nuclear antigens on cell surface
Dysregulated lymphocytes target Ag (normally
intracellular)
Immune complexes form in microvasculature →
complement activation + inflammation
Ag-Ab complexes deposit in basement
membranes of skin and kidneys
12-Oct-15
Connective Tissue Diseases SSalman
15

Etiology
Unknown
At least 10 gene loci known to ↑ risk
Genetic predisposition (10x monozygotic twins)
Human leukocyte Ag: ↑
HLA-DR2
,
HLA-DR3
+
HLA-B8
Null complement alleles + congenital
↓complement (esp C4, C2 etc)
12-Oct-15
Connective Tissue Diseases SSalman
16

Epidemiology
SLE : the most common CTD.
Prevalence 3/10 000 in Caucasians to 20/10 000 in Afro-
Caribbeans.
90% are women.
Peak age 20-30 yrs.
5-year survival
>
90%.
Mortality is usually due to organ failure or overwhelming
sepsis, both modifiable by early effective intervention.
5X increased mortality. Premature cardiovascular disease
and chronic steroids use.
12-Oct-15
Connective Tissue Diseases SSalman
17

History
Constitutional – fatigue, fever, weight loss
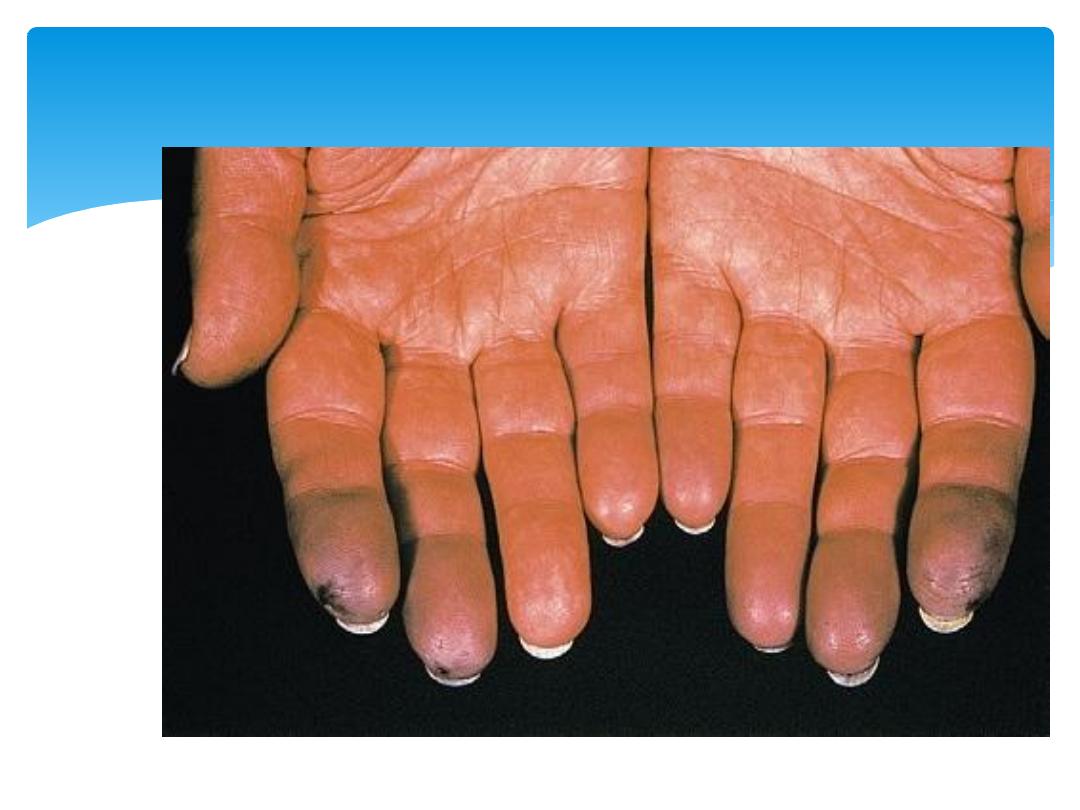
Skin – malar rash, photosensitive, discoid lupus,
alopecia, Raynaud phenomenon, livido reticularis
Musculoskeletal – arthralgia, myalgia, arthritis
Renal
Neuropsychiatric – headache, mood disorders,
cognitive disorders, psychosis, seizures, TIA/ stroke,
movement disorders, mononeuritis
Pulmonary – chest pain, dyspnoea
Gastrointestinal – Abdominal pain, jaundice
Cardiac – heart failure/chest pain
Haematological –‘cytopenias’
Other – miscarriages, autoimmune diseases
12-Oct-15
Connective Tissue Diseases SSalman
18
Raynaud’s Phenomenon
12-Oct-15
Connective Tissue Diseases SSalman
19

On examination
Constitutional – lymphadenopathy, hepatosplenomegaly
Musculoskeletal – Jaccoud arthropathy
Dermatologic - capillaroscopy
Renal
Neuropsychiatric
Cardiopulmonary – friction rubs, pulmonary embolism,
Libman-Sacks endocarditis
GIT – peritonitis, pancreatitis, mesenteric vasculitis
12-Oct-15
Connective Tissue Diseases SSalman
20

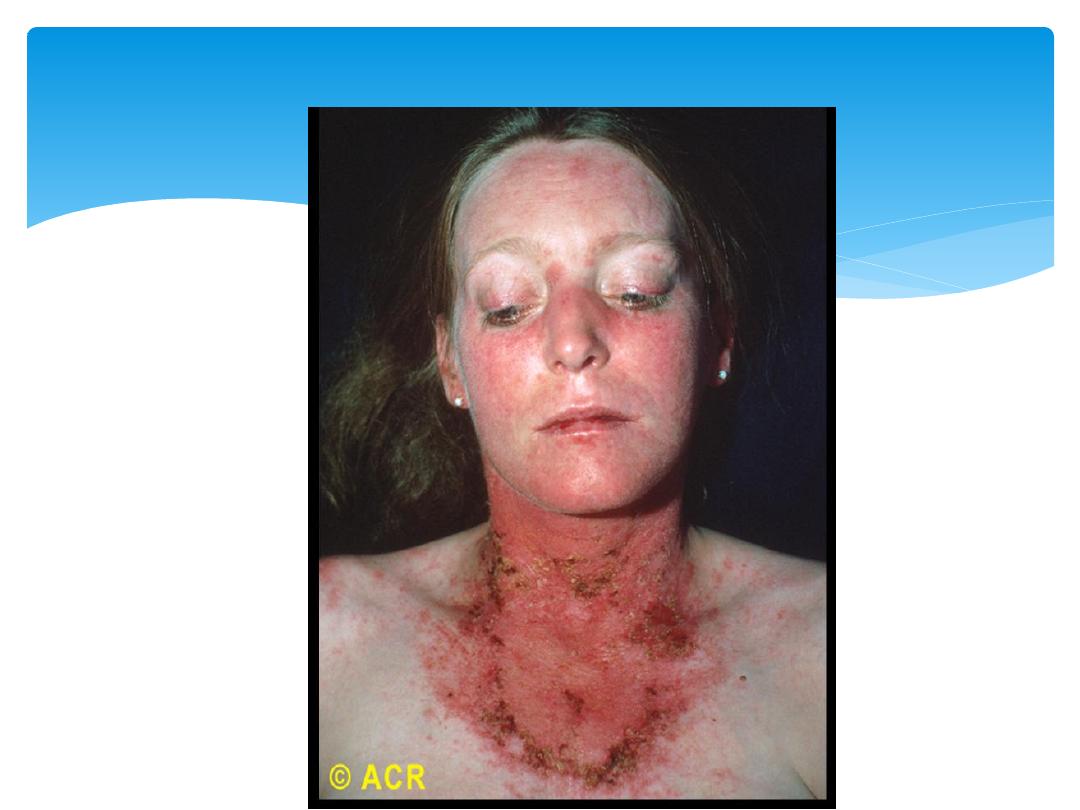
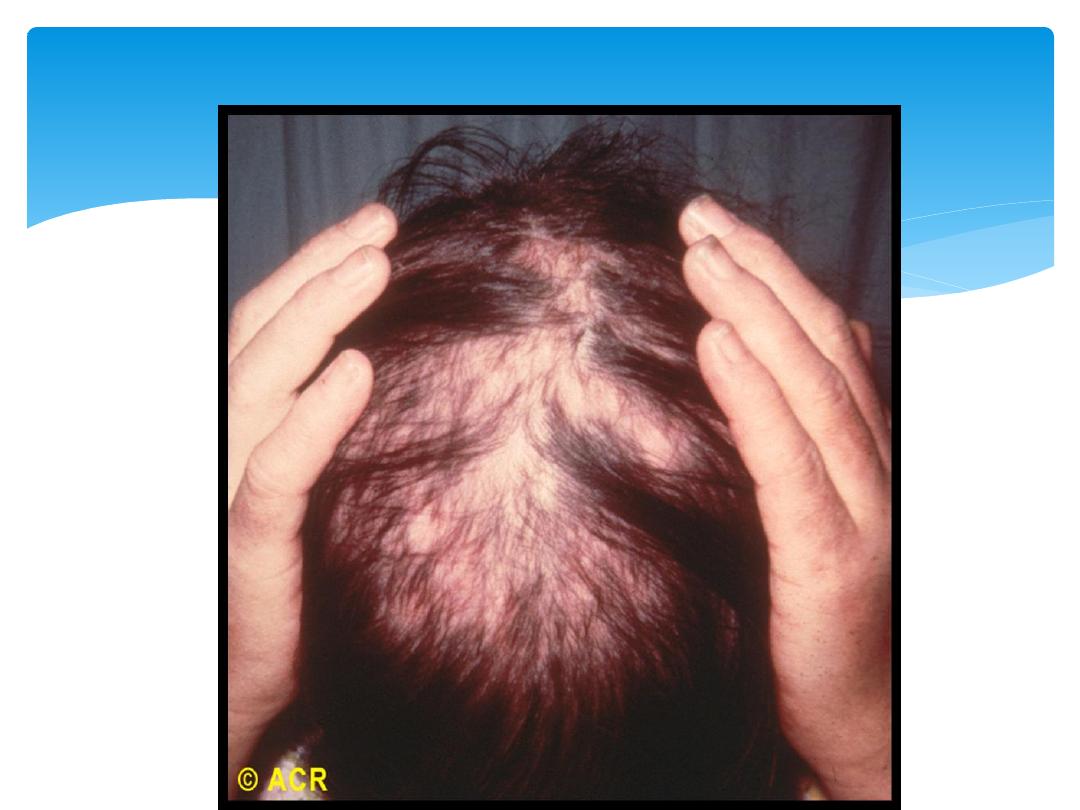
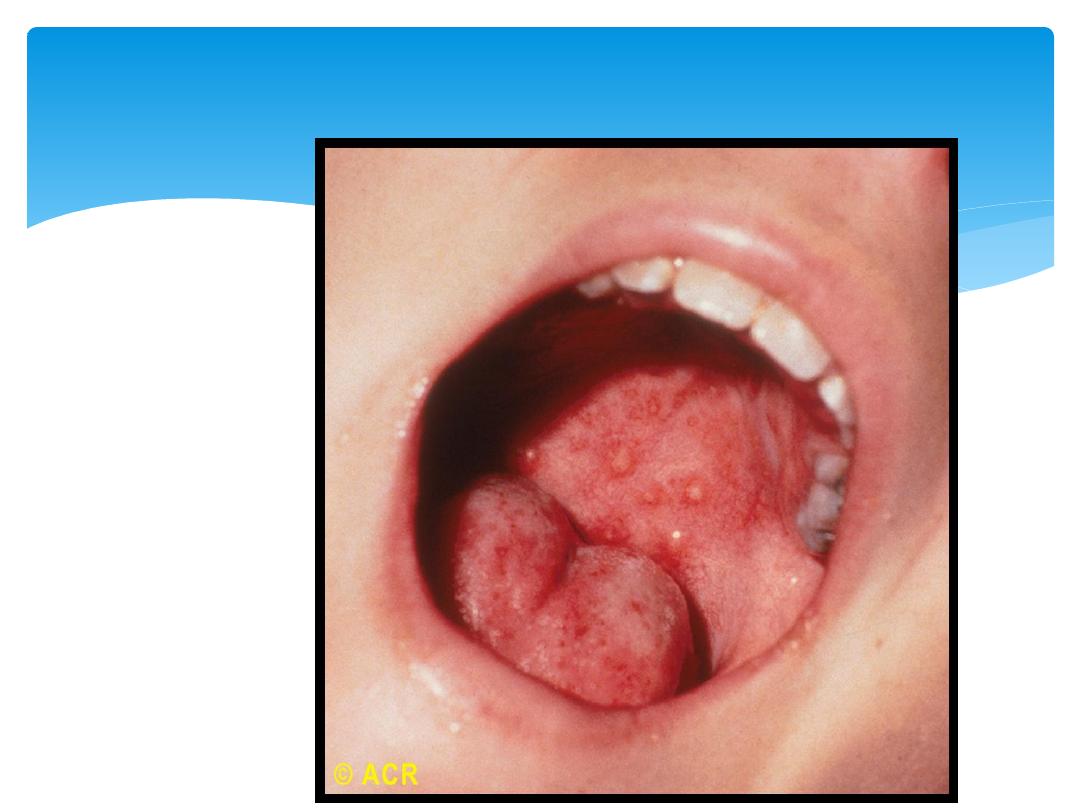
Rash
Common, precipitated by UV light. Three types of rash:
The classic
butterfly facial rash
(up to 20% of patients):
erythematous, raised and painful or itchy, over the cheeks
with sparing of the nasolabial folds.
Subacute cutaneous lupus
erythematosus (SCLE) rashes are
migratory, non-scarring and either annular or psoriaform.
Discoid lupus
lesions are characterised by hyperkeratosis and
follicular plugging, and may cause scarring alopecia.
Diffuse, non-scarring
alopecia
may occur with active disease.
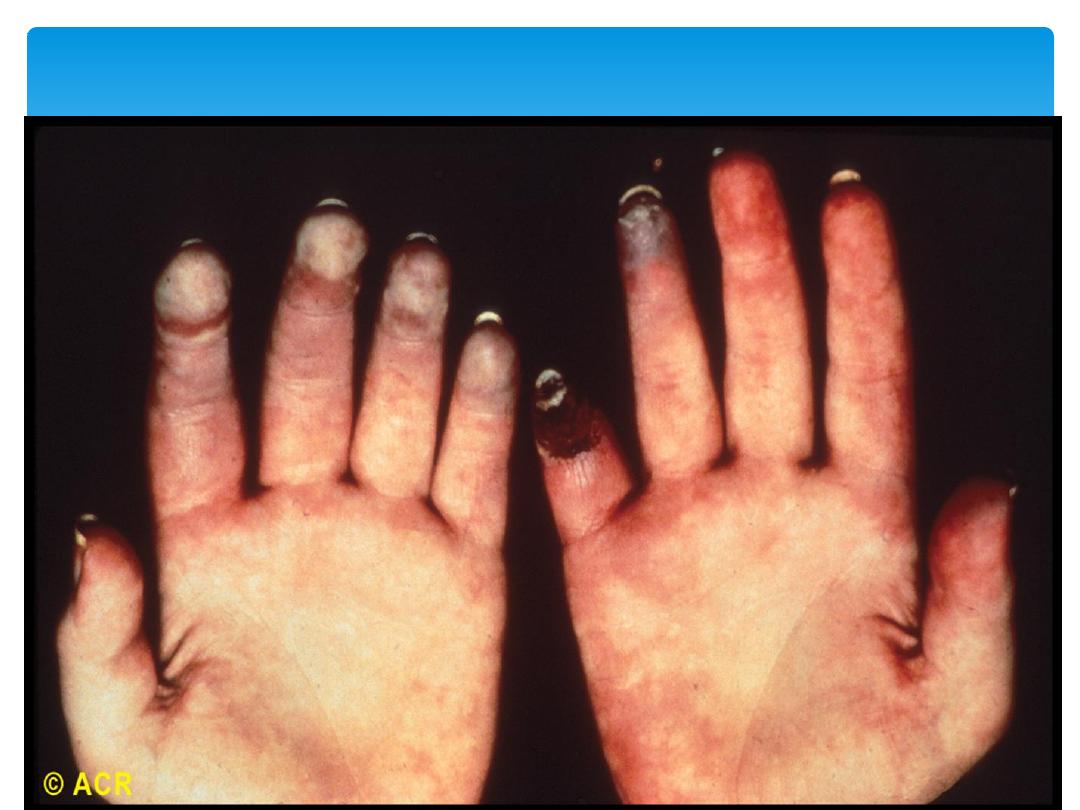
Other skin manifestations include
periungual erythema
(reflecting dilated capillary loops), vasculitis and
livedo
reticularis
, which is also a common feature of the
antiphospholipid syndrome.
12-Oct-15
Connective Tissue Diseases SSalman
21
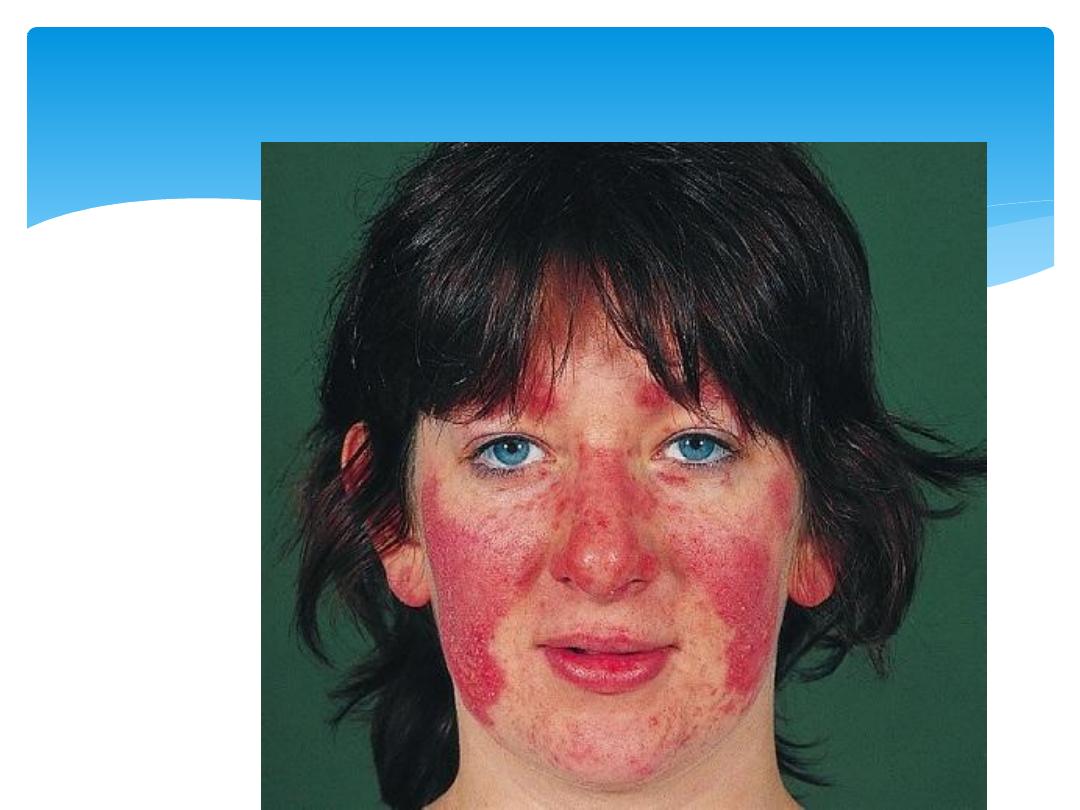
Butterfly Rash
12-Oct-15
Connective Tissue Diseases SSalman
22
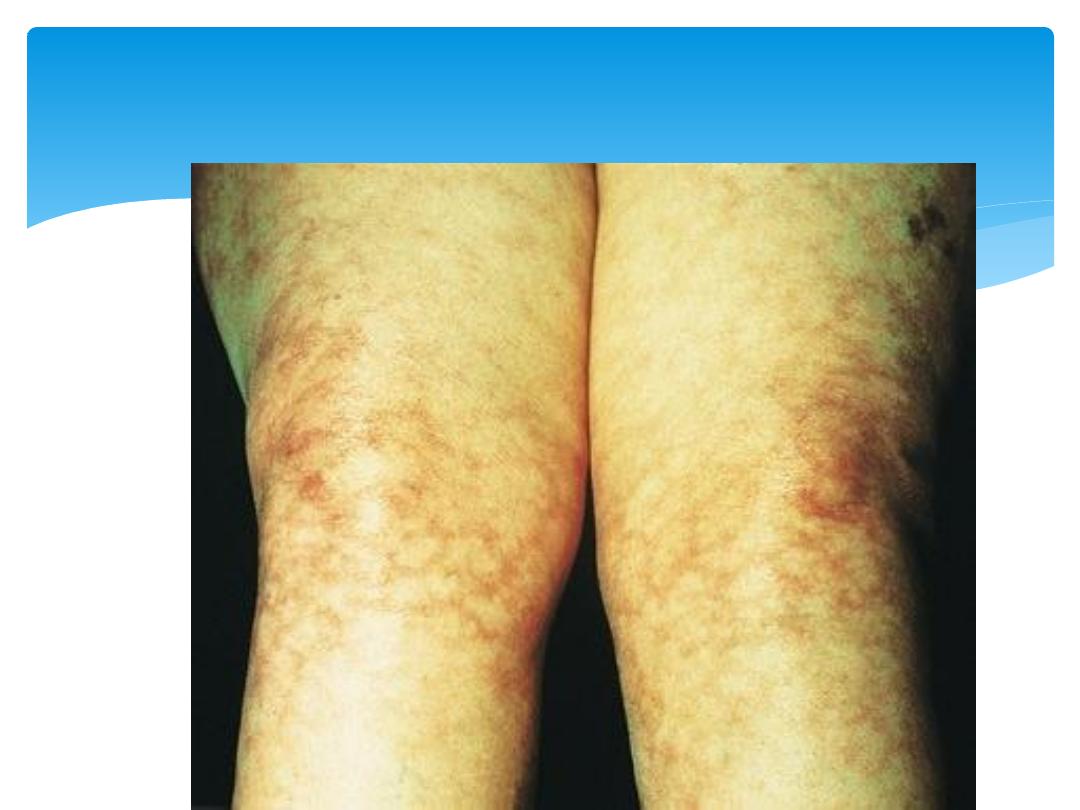
Livedo Reticularis
12-Oct-15
Connective Tissue Diseases SSalman
23
12-Oct-15
Connective Tissue Diseases SSalman
24
Photosensivity
12-Oct-15
Connective Tissue Diseases SSalman
25
alopecia, scalp
12-Oct-15
Connective Tissue Diseases SSalman
26
Digital Gangrene

12-Oct-15
Connective Tissue Diseases SSalman
27
Subacute cutaneous lupus
erythematosus
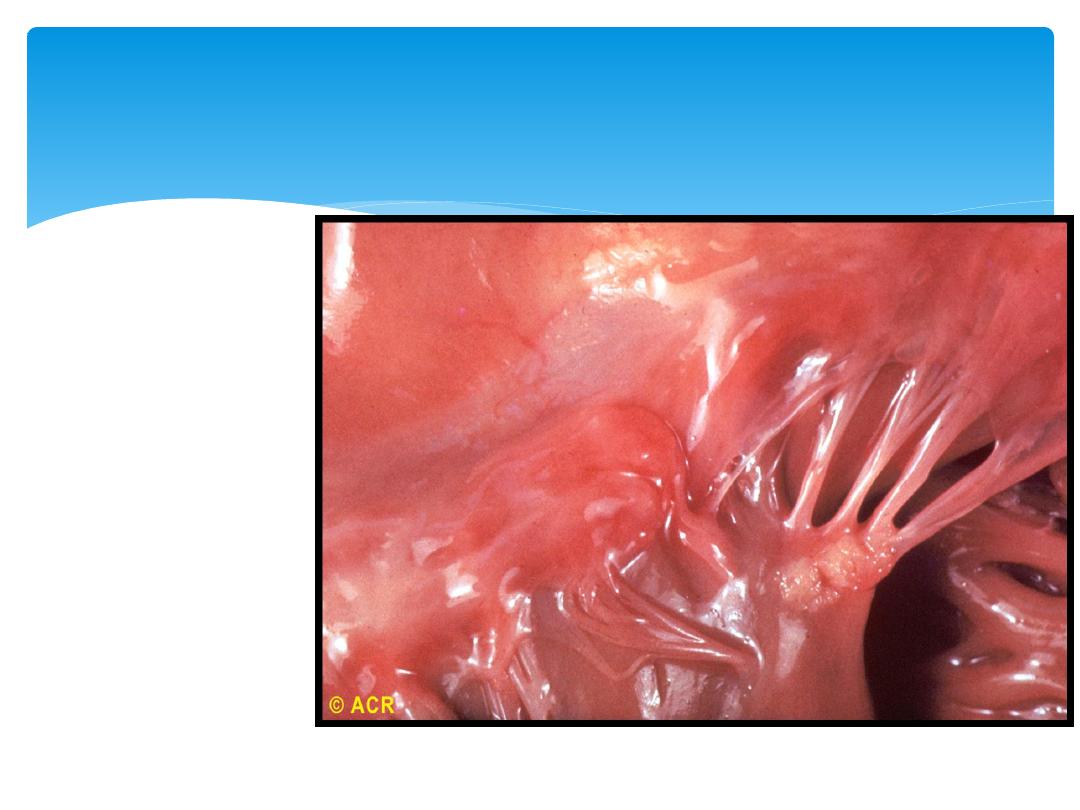
Pericarditis.
Myocarditis
Libman–Sacks
endocarditis
12-Oct-15
Connective Tissue Diseases SSalman
28
Cardiovascular features

12-Oct-15
Connective Tissue Diseases SSalman
29
photosensitive erythematosus rash
12-Oct-15
Connective Tissue Diseases SSalman
30
Mouth ulcers
12-Oct-15
Connective Tissue Diseases SSalman
31
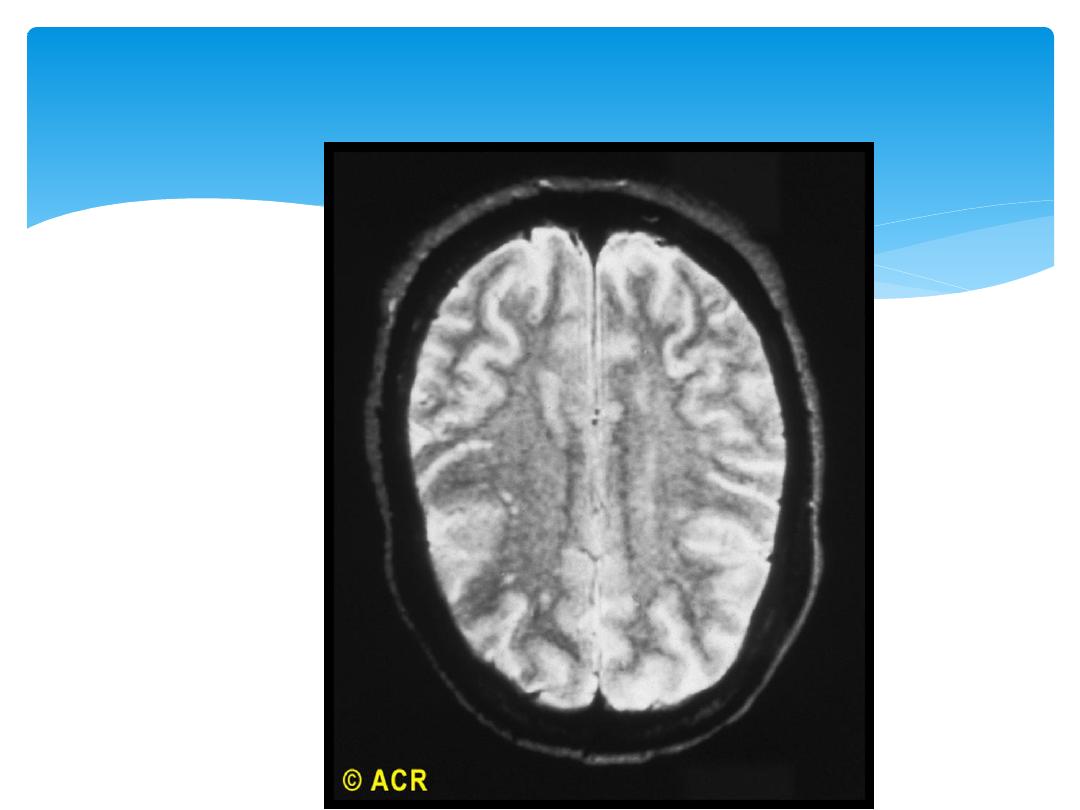
brain (MRI)

Diagnostic criteria
American College of Rheumatology
4/11 criteria
(sens 85%, specif 95%)
“SOAP BRAIN MD”
S
erositis – heart, lung, peritoneum
O
ral ulcers – painless esp palate
A
rthritis – non-erosive
P
hotosensitivity
12-Oct-15
Connective Tissue Diseases SSalman
32

Diagnostic criteria continued
B
lood disorders - ↓RBC (Coombs +), PLT, WCC,
Lymphocytes
R
enal involvement – proteinuria /± casts
A
NA – titer > 1:160
I
mmunologic phenomena – LE cells, anti-dsDNA Ab,
anti-Sm Ab, antiphospholipid Ab, false WR +
N
eurological disorders – seizures/ psychosis
M
alar rash – cheeks + nasal bridge
D
iscoid rash – rimmed with scaling, follicular plugging
12-Oct-15
Connective Tissue Diseases SSalman
33

Laboratory studies
High clinical suspicion/ high ANA titres
SLE Screen:
1.
FBC and diff
2.
S-creatinine
3.
Urinalysis with microscopy
4.
Basic inflammatory markers
5.
Antibodies to dsDNA
6.
Complement
7.
ANA subtypes (anti-Sm, Ro, La, RNP Ab’s)
12-Oct-15
Connective Tissue Diseases SSalman
34

Autoantibody tests used in SLE
ANA – screening test (95% sensitivity)
Anti-dsDNA (high specificity, sens 30%)
Anti-Sm (most specific Ab for SLE, 30% sens)
Anti-Ro/anti-La (15% in SLE, neonatal disease)
Anti-ribosomal P (uncommon, assoc lupus cerebritis)
Anti-RNP (overlap)
Anticardiolipin (antiphospholipid Ab syndrome)
Lupus Anticoagulant (antiphospholipid syndrome)
Coombs test (Ab on RBC’s)
Anti-histone (drug-induced lupus)
12-Oct-15
Connective Tissue Diseases SSalman
35

Radiological studies
Joint x-rays: no erosions, periarticular
osteopenia + soft tissue swelling
CXR/CT chest: Pleural effusion, interstitial
lung disease, pneumonitis, pulmonary
emboli, alveolar hemorrhage
CT Brain or Brain MRI ± angiography: lupus
white matter changes, vasculitis or stroke
Echo: pericardial effusion, pulmonary
hypertension or Libman-Sacks endocarditis
12-Oct-15
Connective Tissue Diseases SSalman
36

12-Oct-15
Connective Tissue Diseases SSalman
37
Jaccoud's arthropathy
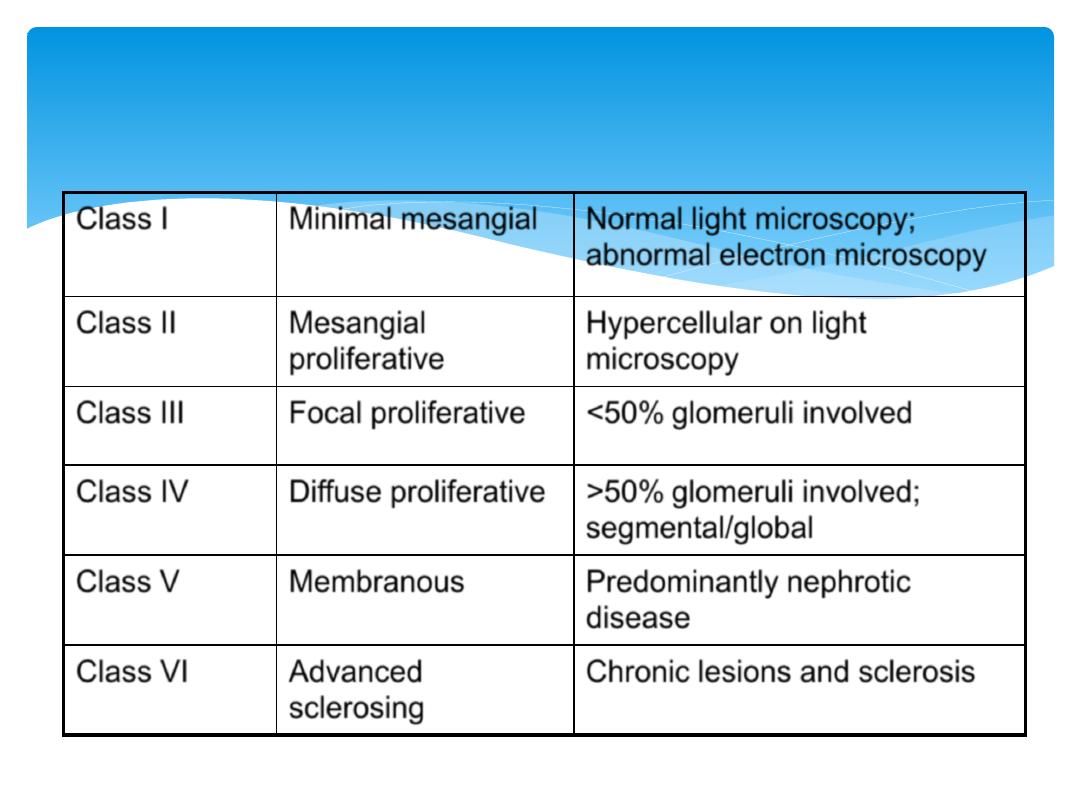
Lupus nephritis
Class I
Minimal mesangial
Normal light microscopy;
abnormal electron microscopy
Class II
Mesangial
proliferative
Hypercellular on light
microscopy
Class III
Focal proliferative
<50% glomeruli involved
Class IV
Diffuse proliferative
>50% glomeruli involved;
segmental/global
Class V
Membranous
Predominantly nephrotic
disease
Class VI
Advanced
sclerosing
Chronic lesions and sclerosis
12-Oct-15
Connective Tissue Diseases SSalman
38
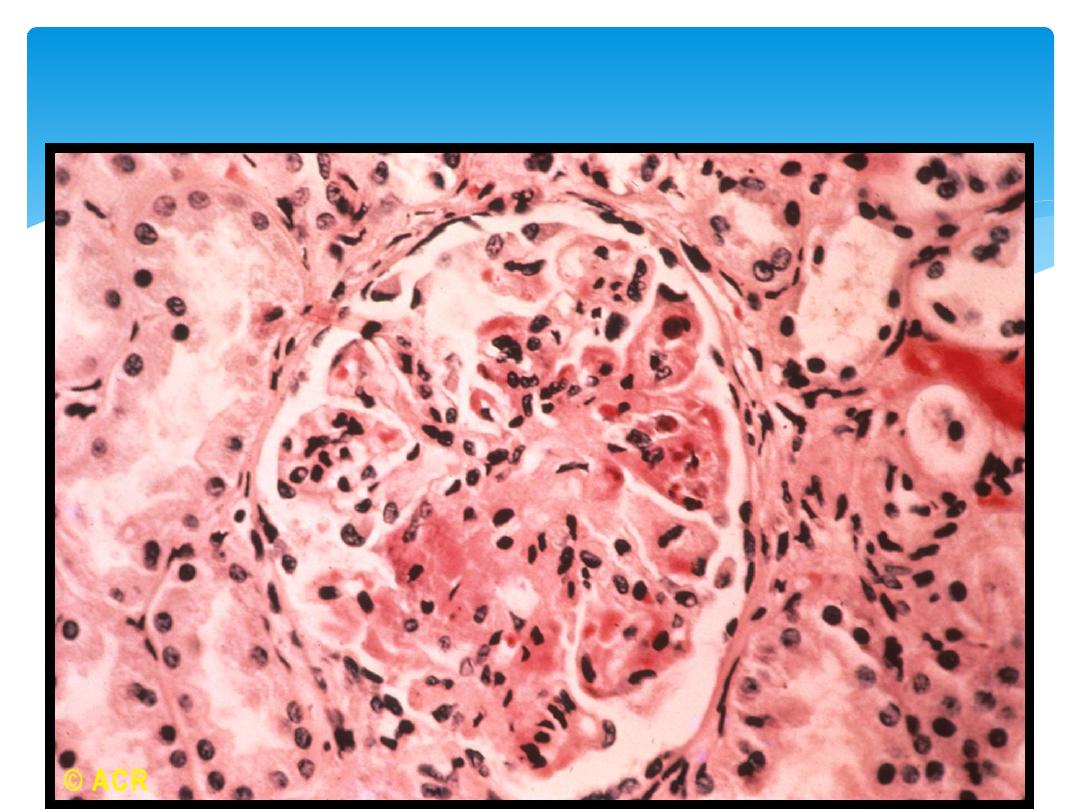
glomerulonephritis with necrosis
12-Oct-15
Connective Tissue Diseases SSalman
39
12-Oct-15
Connective Tissue Diseases SSalman
40
Red blood Cast in Urine

Differential diagnosis
Drug induced lupus erythematosis
Vasculitis
Leukemia
HIV
Multiple sclerosis
Parvovirus or other viral infections
12-Oct-15
Connective Tissue Diseases SSalman
41

Treatment principles
Depends on disease severity
Fever, skin, musculoskeletal and serositis = milder
disease
CNS and renal involvement – aggressive Rx
Emergencies
: - severe CNS involvement
- systemic vasculitis
- profound thrombocytopenia
(TTP-like syndrome)
- rapidly progressive nephritis
- diffuse alveolar hemorrhage
12-Oct-15
Connective Tissue Diseases SSalman
42

Medications used
NSAIDS
Chloroquine
Steroids
Cyclophosphamide
Azathioprine
Mycophenolate
(Rituximab)
Plasma exchange/ IVIG
12-Oct-15
Connective Tissue Diseases SSalman
43

Preventive care
Medication-related (steroid) complications (Ca,
vit D, bisphosphonates)
Aggressive BP and lipid control
Immunization (complement deficient)
Stress-dose steroid for patients on
corticosteroids (surgery/ infection)
Avoid UV exposure
Avoid estrogen therapies
Pregnancy planning
12-Oct-15
Connective Tissue Diseases SSalman
44

Patients with mild disease restricted to skin and
joints can be managed with analgesics and/or
NSAIDs, + hydroxychloroquine (200–400 mg/d).
Short courses of oral steroids for rash, synovitis,
pleurisy and pericarditis.
Management
12-Oct-15
Connective Tissue Diseases SSalman
45

Life-threatening disease affecting the kidney, CNS or
cardiovascular system requires high-dose steroids and
immunosuppressives.
Pulse methylprednisolone (500 mg–1 g i.v)
+cyclophosphamide (2 mg/kg i.v.), at 2–3 weekly intervals
on 6–8 occasions.
Mycophenolate mofetil (MMF) with high dose steroids
for renal involvement in SLE have fewer adverse effects.
Then switch to oral prednisolone (40–60 mg daily) and
azathioprine, methotrexate or MMF.
Co-trimoxazole (960 mg thrice weekly) for preventing
Pneumocystis pneumonia, and mesna is given with bolus
cyclophosphamide to reduce haemorrhagic cystitis.
Antiphospholipid syndrome who had previous thrombosis
require life-long warfarin. If repeated thromboses occur
despite warfarin, the INR target should be 3.0–4.0.
Management
12-Oct-15
Connective Tissue Diseases SSalman
46

Prognosis
Benign to rapidly progressive
Better for skin + musculoskeletal vs renal + CNS
Death rate 3X age-general population
Mortality
Nephritis (most within 5 yrs of symptoms)
Infections (active SLE + Rx – most common)
CVS disease (50X more MI than other woman)
Malignancy (chronic inflammation + Rx)
12-Oct-15
Connective Tissue Diseases SSalman
47

Summary
Autoimmune disorder
Multiple manifestations
Aggressive investigation and treatment
Continued surveillance
12-Oct-15
Connective Tissue Diseases SSalman
48

Davidson’s Principles and
Practice of Medicine 21
st
Edition
Slide collection of American
College of Rheumatology (ACR)
References
12-Oct-15
Connective Tissue Diseases SSalman
50
THANK U 4 LISTENING !!
DR SAMI SALMAN, FRCP, MRCP, DMR, CES, MB,ChB
PROFESSOR OF MEDICINE & RHEUMATOLOGY
Baghdad Medical College
Personal Website:
http://www.samisalman.comyr.com
Arab rheumatologists listing:



