
Anaerobic bacteria
lect:1
Dr. Khalid Waleed
M.B.ch.B., Msc., PhD. Immunology
Objectives
The objectives of this lecture are to know
1. General characters of anaerobic bacteria.
2. Factors that predispose patients to anaerobic infections.
3. Virulence factors of anaerobic bacteria.
4. General methods used for la
boratory diagnosis.
Definition
—
An anaerobe is a bacterium able to replicate in the absence of
oxygen. Some anaerobes are killed almost immediately in the presence of
oxygen (e.g., Clostridium novyi). These are referred to as obligate, or
strict, anaerobes. To grow obligate anaerobes, the laboratory needs to use
oxygen-free growth conditions.
Other anaerobes can survive some
oxygen exposure but will not be able to perform metabolic processes
unless placed into an anaerobic environment. These organisms are
referred to as aerotolerant, or moderate, anaerobes. Many pathogens
encountered in the clinical microbiology laboratory fall into this group
(e.g., Bacteroides fragilis).
Where anaerobes are found?
—
They can be found in soil, in fresh water and saltwater sediments,
and as components of the endogenous microbiota of humans and other
animals. Anaerobes that exist outside the bodies of animals are referred
to as exogenous anaerobes; the infections they cause are termed
exogenous infections. Conversely, anaerobes that exist inside the bodies
of animals (endogenous microbiota) are termed endogenous anaerobes
and are the source of endogenous infections. Exogenous anaerobic
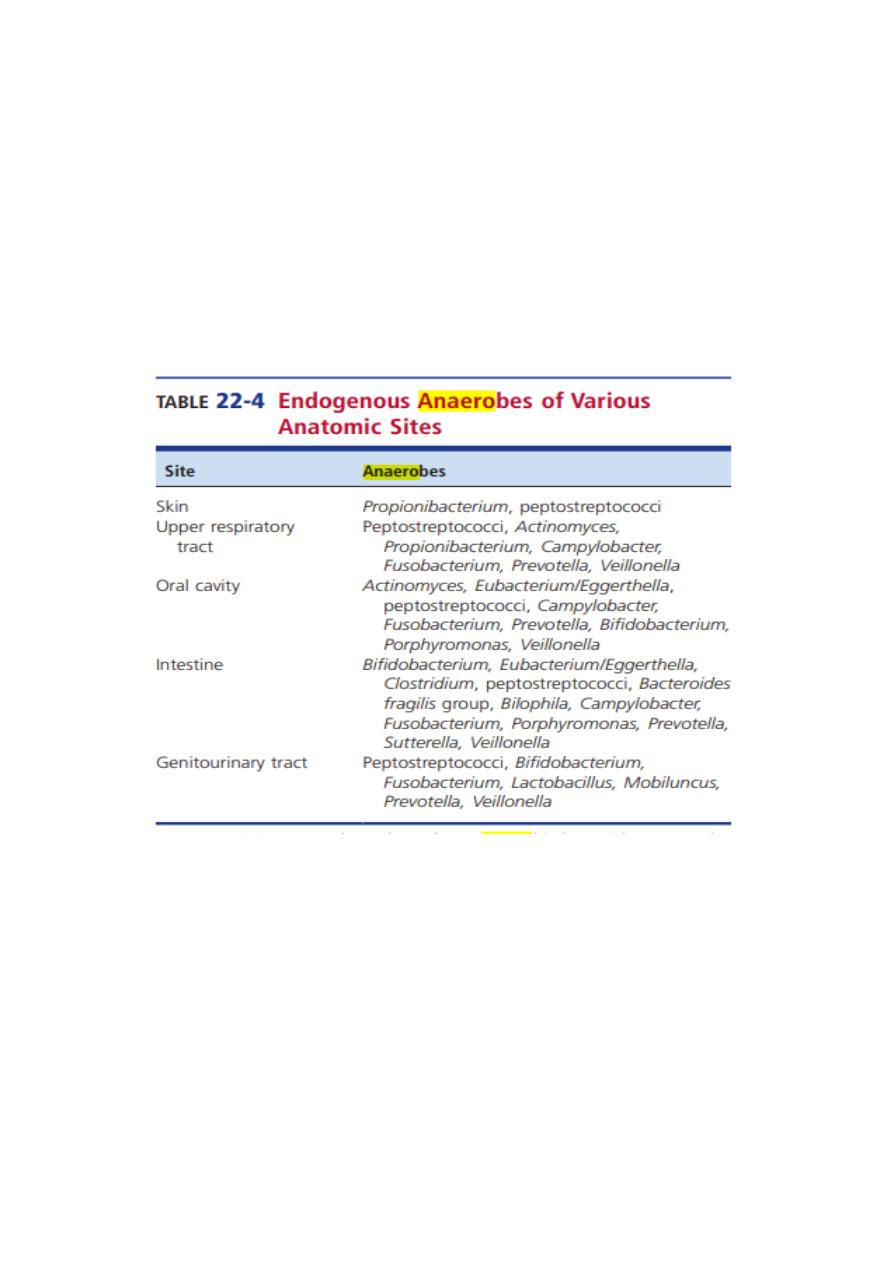
infections are usually caused by gram positive, spore-forming bacilli
belonging to the genus Clostridium.
—
The colon is the major location of bacteria in the body. Roughly 20% of
the feces consists of bacteria, approximately 1011 organisms/g. More
than 90% of the fecal flora are anaerobes, the most important of which is
Bacteroides fragilis. The most abundant facultative bacteria are the
coliforms, of which Escherichia coli is the most important.
—
What are the factors that predispose patients to anaerobic infections?
1. Human or animal bite wounds.
2. Aspiration of oral contents into the lungs after vomiting.
3. Tooth extraction, oral surgery, or traumatic puncture of the oral cavity.
4. GI tract surgery or traumatic puncture of the bowel.
5. Genital tract surgery or traumatic puncture of the genital tract.
6. Introduction of soil into a wound.
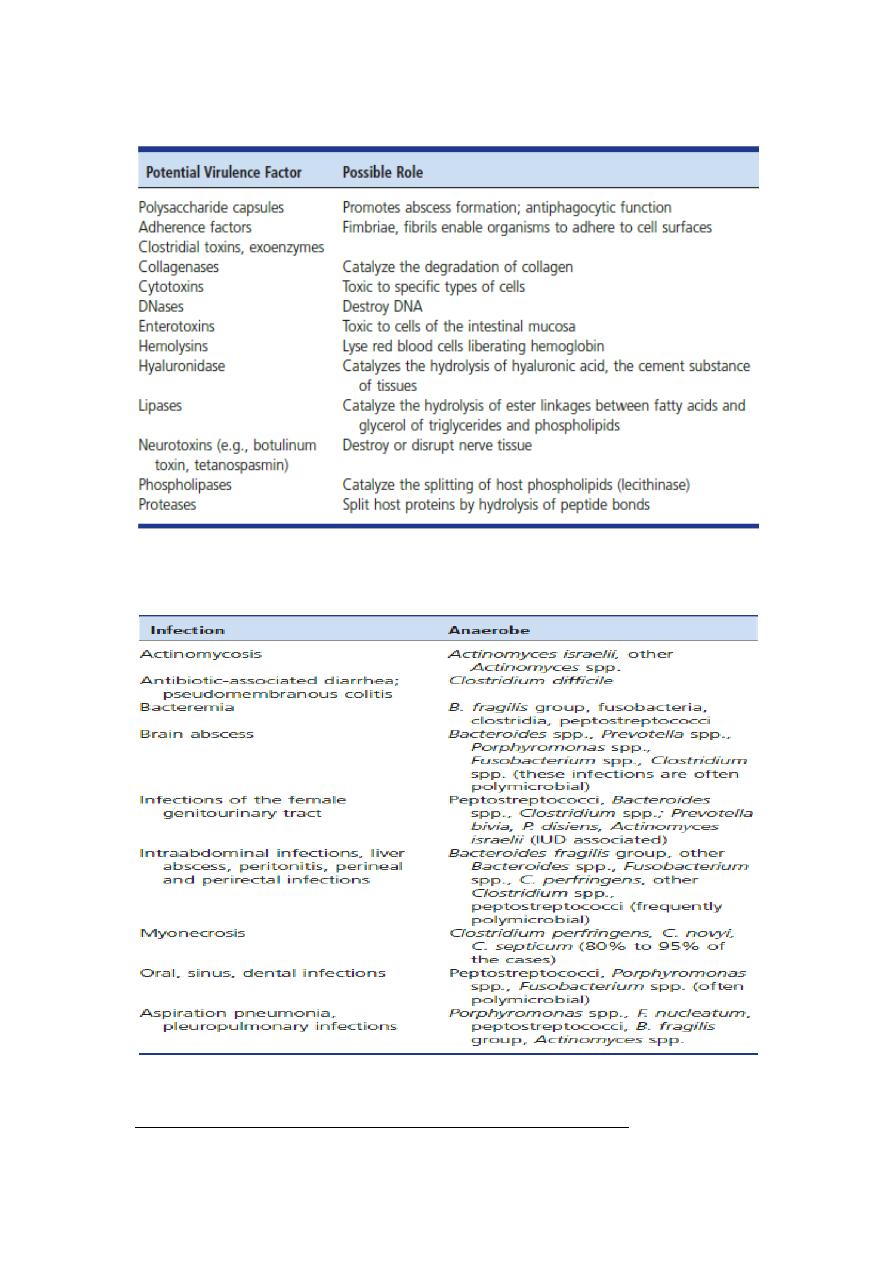
What are the potential virulence factors of anaerobic bacteria?
What are the endogenous anaerobes that commonly involved in
human infections?
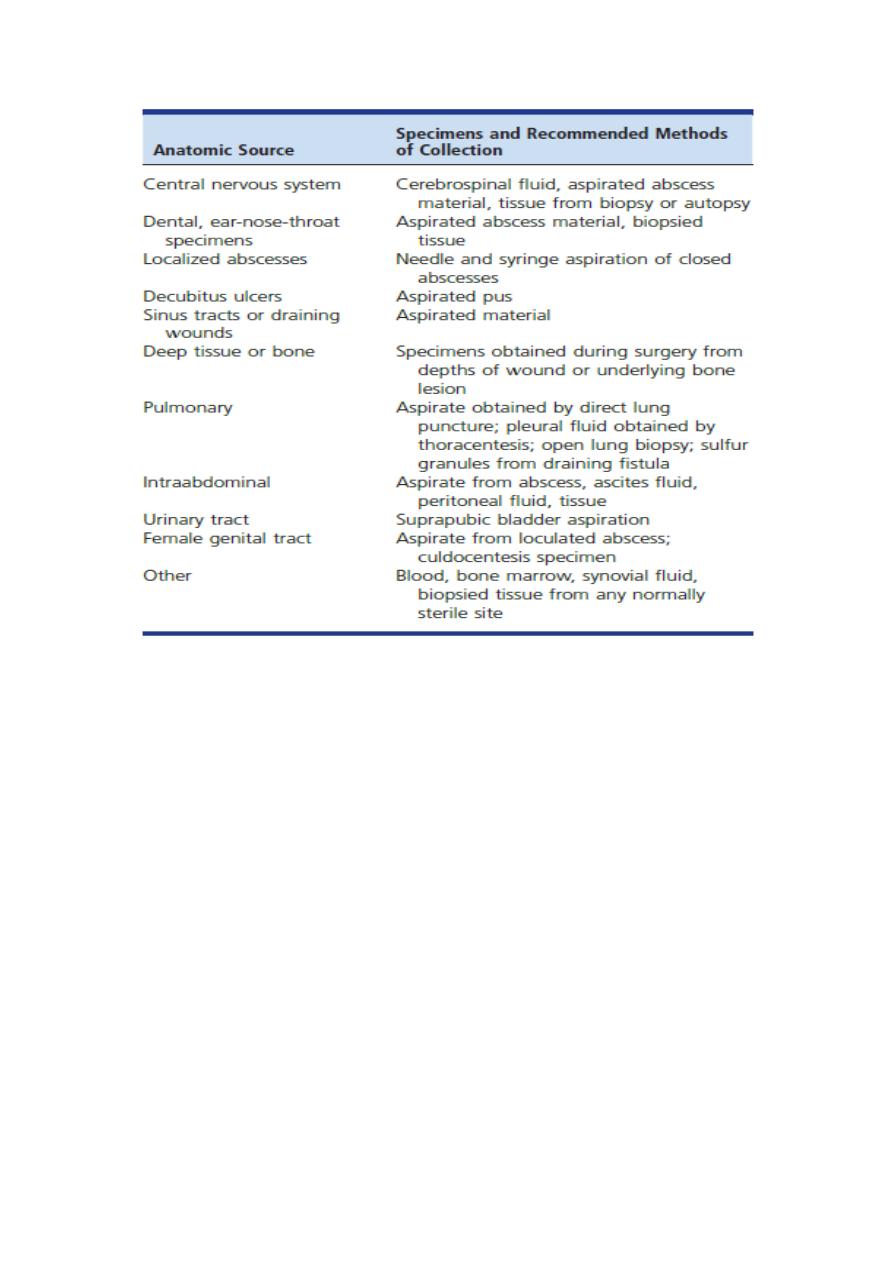
Laboratory diagnosis of anaerobic bacteria
Specimen Selection, Collection, Transport, and Processing

Specimen must be transported and processed as rapidly as possible and
with minimum exposure to oxygen. Specimens are usually collected from
a warm, moist environment that is low in oxygen. It is important to
avoid shocking the anaerobes by exposing them to oxygen or permitting
them to dry out.
Samples for anaerobic bacteriology:
Aspirates: abscess specimens collected by needle and syringe are better
for anaerobic bacteriology than those collected by swab because they are
less likely to be contaminated by endogenous microbiota present at the
mucosal or skin surface.
Tissue: tissue specimens collected by biopsy or at autopsy from usually
sterile sites are acceptable specimens for anaerobic culture. Small pieces
of tissue can be placed in anaerobic transport tubes or vials containing
prereduced, anaerobically sterilized (PRAS) medium to keep the tissue
moist.
Blood: Blood must be cultured as to recover any bacteria or yeasts that
might be present. This usually requires aseptic inoculation of anaerobic
and aerobic blood culture bottles. Once inoculated, bottles should be
rapidly transported to the laboratory, where they are incubated at 35°C to
37°C.
Swabs: swabs, in general, are not appropriate for anaerobic culture. They
should be used only when aspiration of material is not possible and a
biopsy specimen is not available.
What are the acceptable specimens for anaerobic bacteriology?
What are the media used for isolation of anaerobic ?
1. Anaerobic blood agar (CDC)
2. Bacteroides bile esculin (BBE) agar
3. Brucella blood agar (BRU/BA)
4. Anaerobic broth (e.g., thioglycollate and chopped or cooked meat).
Presumptive identification of clinically significant anaerobes
1. Fluorescence: Many strains of pigmented Porphyromonas and Prevotella
fluoresce brick red under long-wave UV light. However, some strains
fluoresce colors other than brick red (e.g., brilliant red, yellow, orange,
pink-orange).
2. Catalase test: Place some of the colony onto a small area of a glass
microscope slide. A drop of 15% hydrogen peroxide is added to the
colony (onto a small area of a glass microscope slide). The production
of bubbles of oxygen gas is a positive result. The catalase test is valuable
in differentiating aerotolerant strains of Clostridium (catalase-negative)
from Bacillus (catalase-positive).
3. Urease test: A rapid urease test can be accomplished by Urease Test
Tablet to 1 mL of distilled water. The isolate is then heavily inoculated
into the water and incubated at 37° C. A positive reaction can occur
within 15 minutes, but the tube must be held for up to 6 hours before a
true negative reaction is determined.
4. Motility test: motility is determined by wet mount using either very
young (4 to 6 hours old) broth cultures or 24- to 48-hour-old colonies on
agar. Motile gram-negative anaerobes include some Campylobacter spp.
5. Spot Indole test: The spot indole test uses a small piece of filter paper
saturated with p-dimethylamino-cinnamaldehyde. A blue or green color
indicates a positive test. whereas a pink or orange color indicates a
negative test. The spot indole test is useful in identifying
Propionibacterium acnes (indole-positive).
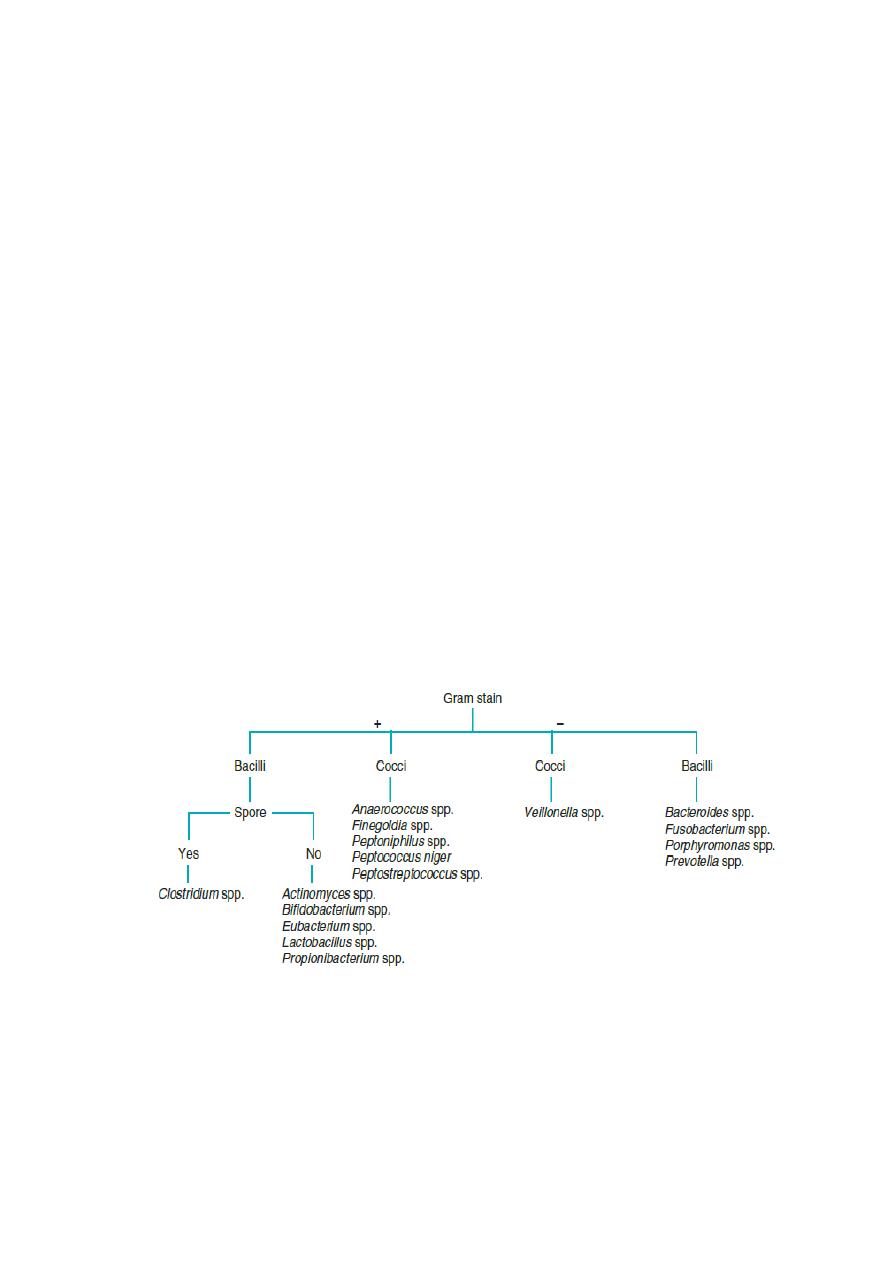
Morphology and Gram reaction of Anaerobic Bacteria (of medical interest)
Refrences:
Textbook of diagnostic microbiology. fifth edition.
