Microbiology
Notes…
1
Mycobacteria 2
Pathogenicity of mycobacteria:
Route of infection:
Inhalation cause pulmonary tuberculosis, whereas ingestion of contaminated
poultry product with M. bovis lead to cervical & mesenteric lymphadenitis.
▪ M. tuberculosis in alveoli resist destruction by macrophages & multiply forming 1ry
lesion (tubercle); then spread to regional lymph nodes, enter circulation, & reseed
the lungs.
▪ Tissue destruction results from cell-mediated hypersensitivity.
M. tuberculosis virulence factors:
(1) Ability to survive inside macrophages, sulfur containing glycolipids prevent
phagolyzosome formation.
(2) Cord factor (trehalose dimycolate), inhibits migration of leukocytes & elicit
granuloma.
Clinical diseases:
(1)-Primary infection:
▪ Initially infection with M.tuberculosis involves mid & lower lung field, & the focus is
usually single.
▪ Cell mediated immunity controlling the infection & the patient remain asymptomatic.
▪ Scar of 1ry complex (focus of infection + L.adenopathy ) calcify, & bacilli slowly die,
(may remain viable for >20 years).
(2)-Active tuberculosis:
(a) As progression of 1ry infection:
If tubercle bacilli not controlled at the site of 1ry infection, bacilli diffuse through
lymphatic vessels & blood stream to any organ in the body, apex of the lung,
kidneys, bone, L.N., brain, meninges, & intestine.
(b) Reactivation of a latent infection:
May occur 20 years or longer after the 1ry infection following deterioration of
immune resistance to M. tuberculosis.
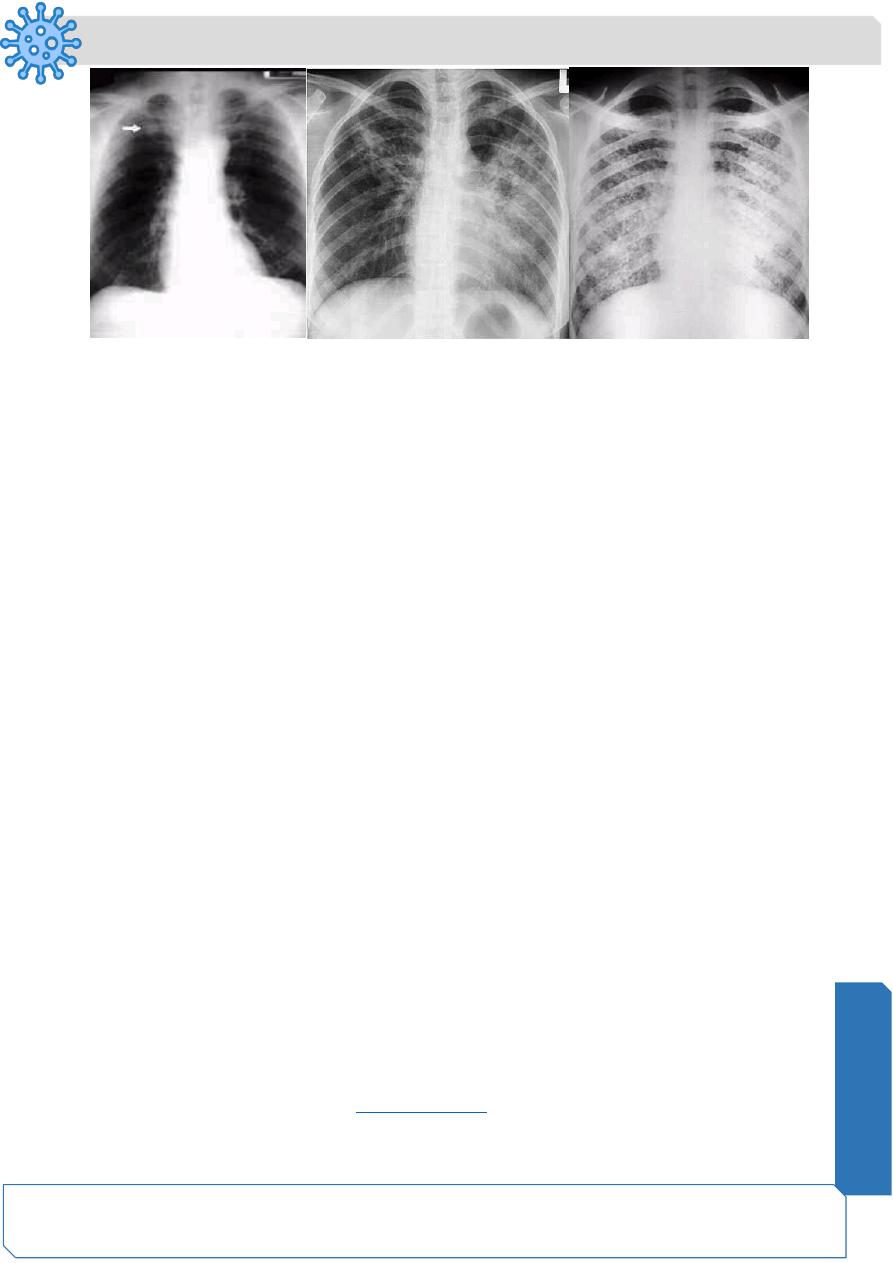
(3)-Disseminated (miliary) tuberculosis:
➢ Very young or elderly individuals & immunocompromised patients are most
frequently affected.
➢ Typically, a necrotic tubercle cause erosion of blood vessel, leading to
hematogenous spread.
Microbiology
Notes…
2
➢ It characterized by numerous granulomatous nodules, result in fulminates infection
in every organ system.
➢ This form of tuberculosis associated with high mortality rate.
Clinical finding:
• Fatigue, weakness, weight loss, afternoon fever, & night sweat .
• Pulmonary involvement give rise to chronic cough, & hemoptysis.
Laboratory diagnosis:
(1) Demonstrating acid-fast bacilli in stained sputum smears or gastric washings contain
swallowed sputum.
(2) Specimens cultured on L-J media.
(3) DTH test for M.tuberculosis antigens , ( tuberculin test ).
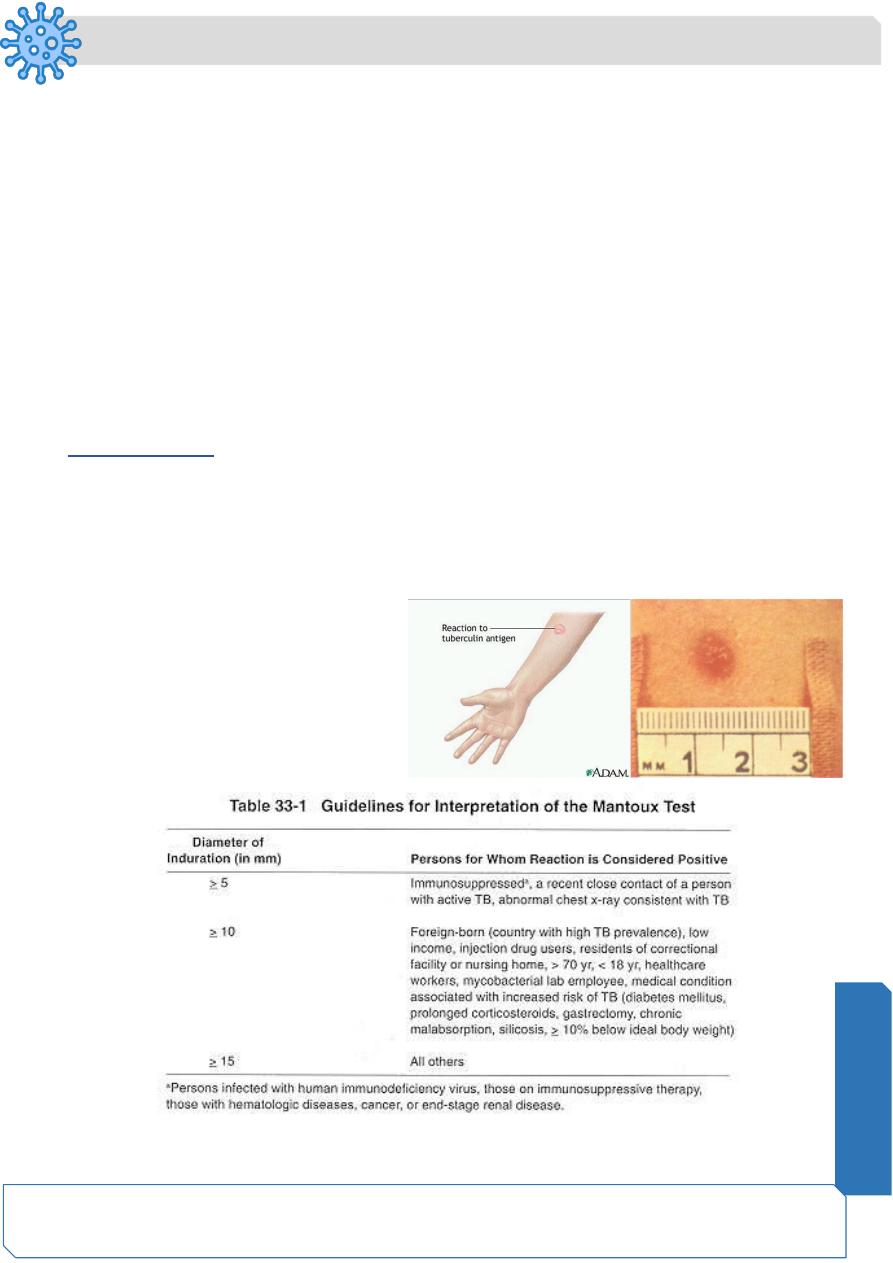
Tuberculin test:
➢ DTH to tuberculin, highly specific for tubercle bacillus.
➢ Purified protein derivative (PPD) from M.tuberculosis injected intradermally into the
superficial layers of the forearm (Mantoux test).
➢ Diameter of induration at injected site measured at 48 hours.
➢ Reactivity to tuberculin occurs
one month after infection &
usually persists for life.
➢ Positive test reveals previous
mycobacterial infection but it
does not mean active infection.
Microbiology
Notes…
3
Treatment:
❖ Simultaneous administration of at least 2 drugs to avoid emerges of resistant strains
of M.tuberculosis,
❖ Duration of treatment should be continued for several months, depend on severity
of the disease.
❖ 1st line: ( ethambutol, pyrazinamide, INH, streptomycin, rifampin),
❖ 2ndline : ( capreomycin, cycloserine, ethonamide, fluroquinolones, kanamycin,
PAS, rifabutin, viomycin).
Control & Prevention:
❖ A vaccine (a live attenuated bovine strain) called bacilli Calmette & Guerin (BCG)
is currently available for protection against T.B.
❖ BCG is given to children in many countries.
❖ The eradication of tuberculosis in cattle & pasteurization of milk greatly reduced M.
bovis infections.
M. leprae:
▪ M. leprae causative agent of leprosy( Hanson's disease).
▪ The bacterium discovered in 1873 by a Norwegian physician named Gerhard
Hansen.
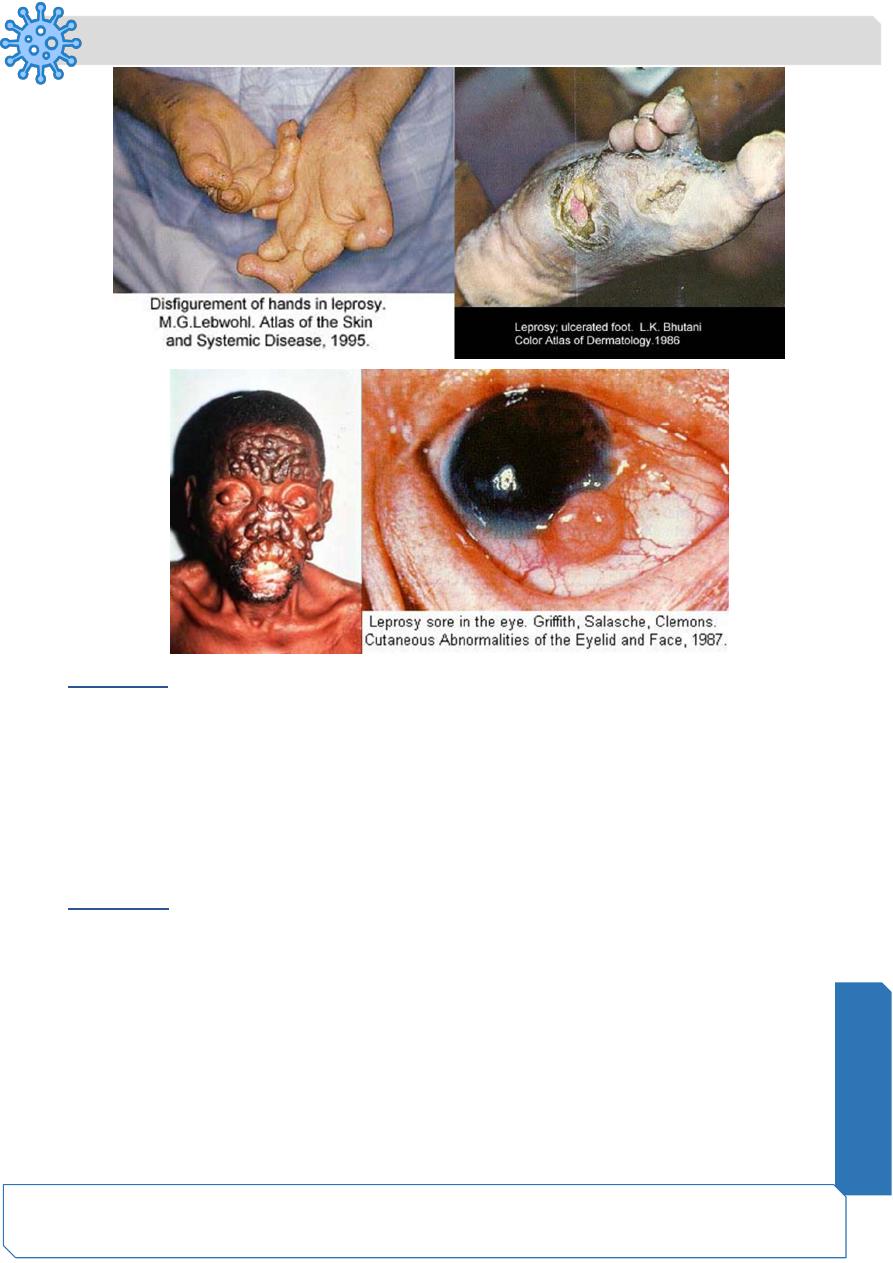
▪ Leprosy is an infection of skin, peripheral nerves, & mucous membranes, leading
to hypo pigmentation, & loss of sensation (anesthesia), particularly in cooler areas
of the body.
▪ M. leprae is aerobic rod surrounded by the characteristic waxy coating unique to
mycobacteria.
▪ In size & shape resembles
▪ M. leprae has never been grown in artificial culture, but will grow in the footpads of
mice.
Microbiology
Notes…
4
Pathogenesis & clinical disease:
o Bacteria spread by direct contact & through air from coughing or sneezing.
o The incubation period long, years.
o There are three forms of leprosy, lepromatous being the most severe, tuberculoid,
& borderline leprosy.
o Patients with strong cell mediated responses to M leprae antigens, develop
tuberculoid leprosy.
o Patients with weak to absent CMI to M leprae, develop lepromatous leprosy.
o Virulence factors include a waxy exterior coating by mycolic acid unique to
mycobacteria.
Clinical feature:
▪ The onset of leprosy is insidious.
▪ Lesions in the cooler area of the body, skin, superficial nerves, nose, pharynx,
larynx, eyes, & testicles.
▪ Skin lesions : - Pale, anesthetic macular lesions 1-10 cm.
- Diffuse or discrete erythematous nodules 1-5 cm.
- Diffuse skin infiltration.
▪ Neurological disturbances: nerve thickening, anesthesia, neuritis, paresthesia,
trophic ulcers, & bone resorption with shortening of digits.
▪ Eye involvement is common.
Tuberculoid leprosy:
(1) Benign & non progressive.
(2) Macular skin lesions.
(3) Severe asymmetric nerve involvement.
(4) Few bacilli present in the lesions. (paucibacillary).
(5) Positive lepromin skin test.
Lepromatous leprosy:
(1) Progressive & malignant.
(2) Nodular skin lesions.
(3) Slow symmetric nerve involvement.
(4) Abundant acid fast bacilli in skin lesions.(multibacillary)
(5) Negative lepromine skin test.
Microbiology
Notes…
5
Diagnosis:
▪ Clinical sign & symptoms.
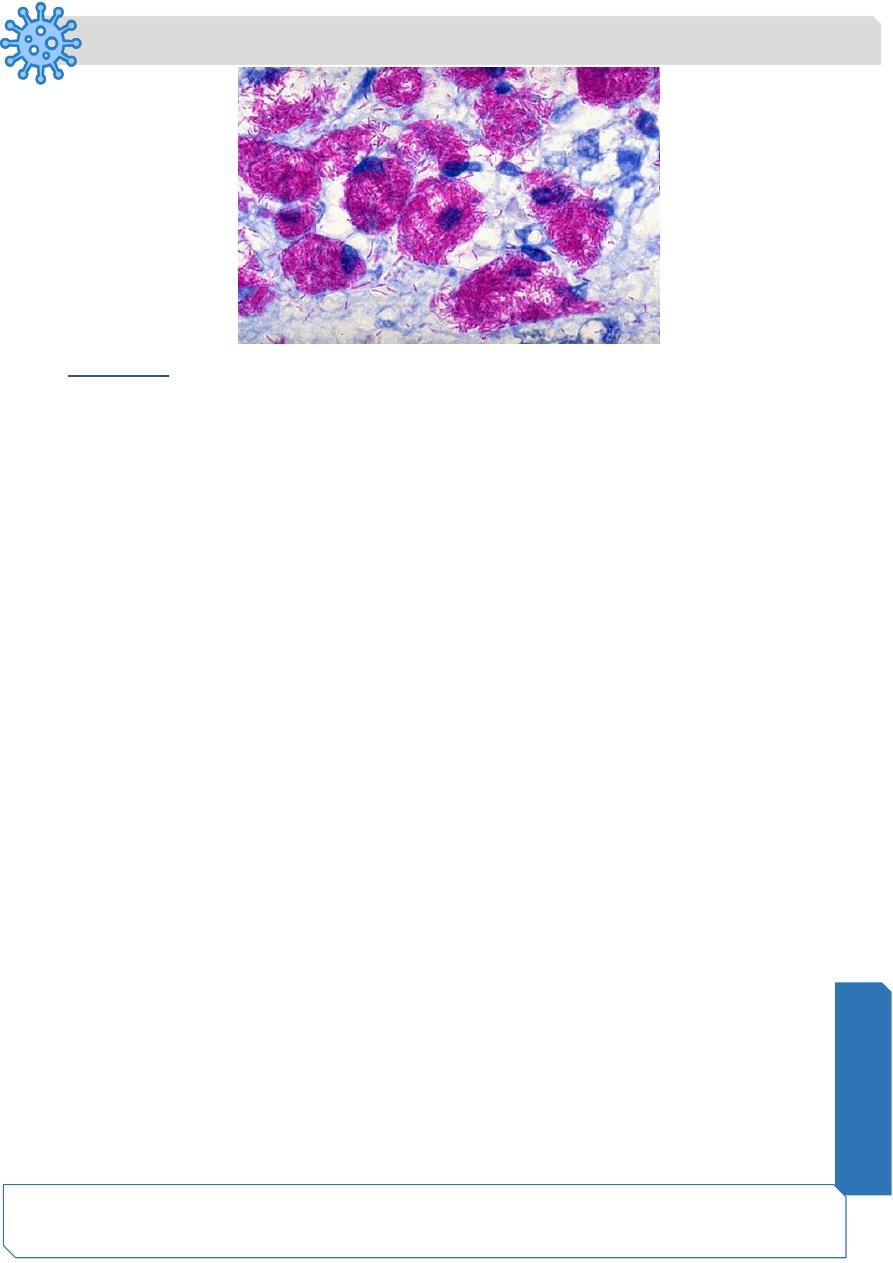
▪ Scraping or biopsies from lesions reveals characteristic histopathology & in
lepromatous disease large number of acid fast bacilli with globular arrangements
characteristics of M leprae.
▪ Lepromin test: positive lepromine test (tuberculoid leprosy) has positive diagnostic
value.
Treatment:
• Dapsone (diamino diphenyl sulfone) successfully used over fifty years to treat
leprosy, but recently, the bacilli are becoming more resistant to treatment.
• Multidrug therapy (MDT), usually consisting of:
Rifampicin.
Clofazamine.
Dapsone.
MDT use to treat all cases of leprosy to diminish the development of resistance genes.
Microbiology
Notes…
6
Prevention
❑ In 1997, there were approximately 1.2 million cases worldwide, with Africa & Asia
reporting the highest numbers.
❑ About 600,000 new cases are reported annually.
❑ The disease is not highly contagious, leprosy can be avoided by covering the face
& hands in the presence of infected individuals.
❑ Disinfection of contaminated articles & hand washing.
❑ The availability of MDT in recent years has lessened the worst symptoms of
leprosy.
❑ Modern antibiotics & new treatment regimens are helping to keep the number of
severely disfigured individuals to a minimum.
