
1
Chemotherapy of infections
Chemotherapy: Chemical substance treated clinical case.
Chemotherapy of infection: Is used for the drug treatment of infection as virus, bacteria,
protozoa, fungi, worms are either destroyed or removed without injury to host. It form 2
find effect.
1- Effect on host: by increase or stimulate immunity or increase body resistance
against infection.
2- Effect on microorganism: by destroy microorganism or arrest the growth &
replication.
Antibiotic: A chemical substance that kills microorganism (bacterial, fungi,
helminthes and protozoa) and cures infection is biological source.
Classification of antimicrobial drugs:
May be classified according to the type of organism against which they are active:
- Antibacterial drugs.
Antiviral drugs.-
Antifungal drugs.-
- Antiprotozoal drugs.
-Anthelminthic drugs.
Antimicrobial drugs have been also classified broadly into:
Bacteriostatic drug: Drugs arrest the growth & replication of bacteria at serum
levels achievable in the patients, thus limiting the spread of infection while the
body's immune system attacks, immobilizes & eliminates the pathogens. such as
sulphonamides, tetracyclines, and chloramphenicol. Most bacteriostatic drugs
can be shown to be bactericidal at high concentration, under certain incubation
conditions in vitro and against some bacteria.
Bactericidal drug: Drugs kill bacteria at drug serum levels achievable in the
patient. Because of their more aggressive antimicrobial action, these agents are
often the drugs of choice in seriously ill patient, such as penicillin's,
cephalosporins, aminoglycosides, isoniazide and rifampicin. This act mostly on
rapidly dividing organisms. It is possible for an antibiotic to bacteriostatic for one
organism & bactericidal for another e.g. chloramphenicol is static agent gram –ve
rods & is cidal against other organisms, such as S. pneumoniae.
Minimum inhibitory concentration (MIC): Is the lowest concentration of
antibiotic that inhibits bacterial growth.
Minimum bactericidal concentration (MBC): Is the minimal concentration of
antibiotic that kills the bacteria.
2
CHEMOTHERAPEUTIC SPECTRA
Spectrum: Antimicrobial agent different in their action either broad spectrum,
narrow spectrum.
Narrow spectrum antibiotic:
Chemotherapeutic agents acting on a single or a
limited group of microorganisms ex. Isoniazid.
Broad spectrum antibiotic: Antibiotic that are effective against gram positive
organisms and also against a gram negative bacteria or antibiotics that affect a
wide variety of microbial species. ex. Ampicillin.
Concentration- dependent killing:
❖ Certain
antimicrobial
agents,
including
aminoglycosides
&
fluoroquinolones, show significant increase in the rate of bacterial killing
as the concentration of antibiotics increases from 4 to 64 fold the MIC of
the drug for the infecting organism. Such drugs exhibit a concentration
dependent killing.
❖
By contrast, β-lactams, macrolides & clindamycin don't exhibit this
property. Their clinical efficacy is best predicted by the percentage of time
their blood concentrations remain above the MIC. This effect is called time
dependent killing.
Postantibiotic effect (PAE): The PAE is a persistent suppression of microbial
growth that occurs after levels of antibiotic have fallen below the MIC.
Antimicrobials such as aminoglycosides & fluoroquinolones exhibit a long PAE
(several hours). Antimicrobial drugs exhibiting a concentration-dependent killing
& a long PAE often require only one dose per day.
COMBINATIONS OF ANTIMICROBIAL DRUGS
♦
Antimicrobial combinations should be for one or more of the following
reasons:
1. To provide
broad spectrum
empirical therapy in seriously ill patients.
2. To treat
polymicrobial infections
such as intraabdominal abscesses
3. To decrease the emergence of
resistant strained
as in T.B.
4. To decrease
dose related toxicity
by using reduced doses of one or more
components of the drug regimen.
5. To obtain enhanced inhibition or killing i.e.
synergism
e.g. β-lactams &
aminoglycosides.
♦
Note: coadministration of an agent that causes bacteriostasis plus a
second agent that is bactericidal may result in the first drug interfering
with the action of the second.
♦
DRUG RESISTANCE
♦
Occurs when bacterial growth is not stopped by the maximal level of the
antibiotic that can be tolerated by the host.
A. Genetic alterations leading to drug resistance:
3
1. Spontaneous mutations of DNA:
2. DNA transfer of drug resistance:
B. Altered expression of proteins in drug resistant organisms:
1. Modification of target sites:.
2. Decreased accumulation:
3. Enzymatic inactivation:
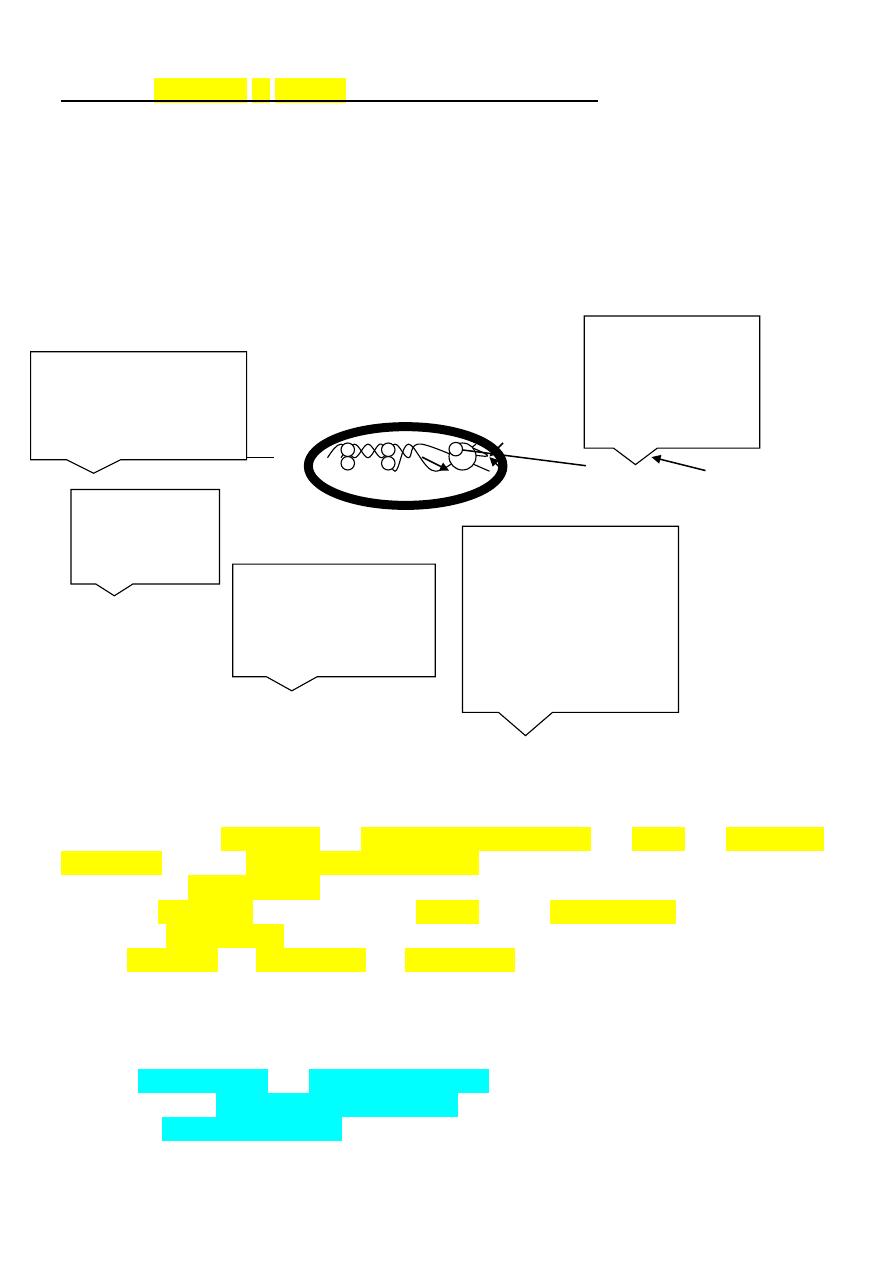
Classification of antibiotic according to the mode of action:
Cell membrane
cell wall
Properities of an ideal antibiotics :-
1-it should be bactericidal , broad range of activity , potent , orally and
parenterally effective distributed to all body parts .
2-should be of selective action .
3-effective blood level should be reached quickly and for prolong period .
4-should be water soluble .
5-its of no toxicity , of no sensitifity , of no resistance against their action .
Dangers of antibiotic therapy :-
1-risk of hypersenstivity and anaphylactic reaction like pencillin .
2-development of resistance strain of organism .
3-risk of foetal abnormalities like tetracycline causing malformation of dental
pulp.
Inhibitors of
nucleic acid
synthesis
-fluoroquinoelone
-rifampin
Inhibitors of folic acid
metabolism:
sulfonamides &
trimethoprim
Inhibitors of
cell wall
synthesis
-β-lactams
Inhibitors of protein
synthesis:
-tetracyclines
-aminoglycosides
-clindamycin
-macrolides
-chloramphenicol
Inhibitors of cell
membrane function:
-isoniazid
-amphotericin B

4
4-risk of masking the severity and diagnosis of the disease .
5-special toxicity and side effects .
6- may potentiate the toxic effects of other drugs if both administrated together
like it cause digoxin toxicity .
Prophylacting uses of antibiotics :-
1-to protect the heart in rheumatic fever like using of benzathine pencillin .
2-to protect the patient from bacterial endocarditis in patient with congenital
heart abnormalities or rheumatic fever undrgo dental extraction .
3-to protect person aganis T.B who in contact with TB patient like using of
isoniazid.
4-to prevent gas gangerne by using large dose pf pencillin in sever contaminating
trauma and for amputaion .
5- to inhibit possibility of secondary bacterial infection in certain condition like
kerosin poising .
