Histology of skin dr. Ahmed Alhuchami
The skin is the largest organ of the body.
Functions of the s kin
1 Protection: The thick epidermal layer, together with its waterproof coating, and pigment content, protect against ultraviolet (UV) light, mechanical, thermal and chemical stresses, and prevent dehydration and invasion by micro - organisms.
2 Sensation: Via receptors for touch, pressure, pain, and temperature.
3 Thermoregulation: Alterations in the peripheral circulation of blood regulate body temperature, as do sweat glands, hair, and adipose tissue.
4 Metabolic functions: Areas of the skin photosynthesize vitamin D, and lipids, including triglyceride (a neutral lipid).
All regions of skin contain the same three basic layers :
an outer layer (the epidermis ), an underlying dermis , and the innermost layer, the hypodermis
The epidermis
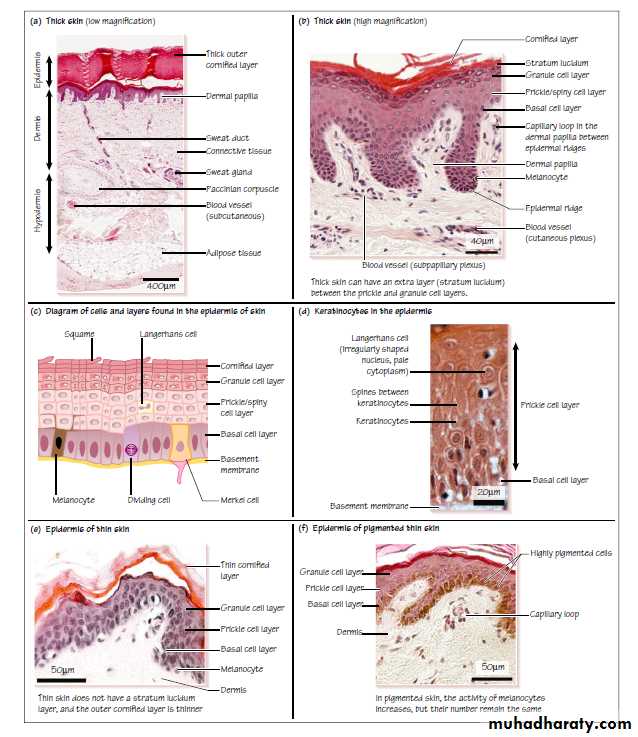
This is the thin outer layer of the skin .It is a stratified, squamous keratinizing epithelium, which contains four layers of cells (sometimes five in areas of thick skin; . It does not contain any blood vessels. The cells in the different layers change their appearance as they move upwards from the basal layer and differentiate.
Basal cell layer ( stratum germinativum or stratum basale)
This consists of a single layer of cells, which lie closest layer to the underlying dermis. The cells adhere tightly to each other via desmosomes, and to the underlying basement membrane via focal adhesions (hemi - desmosomes). The basal cell layer contains several types of cell.
• Stem cells: which divide and renew the stem cell population and produce daughter cells (keratinocytes). They have a huge capacity for self - renewal: the outer layers of the skin turn over completely every 2 weeks.
• Keratinocytes: the most common cells in this layer .They divide 3 – 6 times before moving up into the prickle cell layer, and are cuboidal in shape with a pink cytoplasm and light purple nucleus.
• Melanocytes: pigment (melanin) - producing cells, derived from the neural crest in the embryo. There is 1 melanocyte for every 4 – 10 basal keratinocytes. Their numbers are similar from person to person, but their activity is much higher in dark skin .Melanocytes can be identified by their pale/clear cytoplasm and dark purple (basophilic) nucleus. Pigment is trafficked in vesicles(melanosomes) to the tips of long processes that penetrate into the prickle cell layer, and these are then engulfed (phagocytosed) by keratinocytes. The phagocytosed melanin then forms a layer in front of the nucleus, to protect against UV light.
• Merkel cells: rare neuroendocrine cells, which act as slowly adapting ‘ tactile ’ mechanoreceptors. They are most common in lips and the tongue, but are difficult to identify as they have a similar appearance to melanocytes.
In addition, there are free nerve endings (unmyelinated) which respond to pain and temperature.
Stratum spinosum ( prickle cell layer)
This region consists of several layers of keratinocytes , and some Langerhans cells
• Keratinocytes switch keratin expression. Keratin filaments inside the cell are connected to desmosomes to reinforce cell – cell junctions and make tight connections between the cells. These connections can sometimes be seen in histological sections as ‘ spines ’ in the light microscope, giving these cells their ‘ prickly ’ appearance.
• Langerhans cells are specialized antigen - presenting cells (dendritic cells), which account for 3 – 6% of the cells in the stratum spinosum layer .. They contain long processes (dendrites) that ramify between the keratinocytes and contact other Langerhans cells to form a continuous network. When they are exposed to foreign bodies/antigen, they migrate out of the epithelium and into regional lymph nodes to initiate an immune response. Langerhans cells can be recognized by their round cell body, paler appearance of the cytoplasm, and oval – shaped nucleus.
Stratum granulosum ( granule cell layer)
This layer lies on top of the stratum spinosum.
• It contains keratinocytes that have moved upwards and further differentiated into granule cells . They extrude specialized lipids in intracellular granules into the gaps between dead cells (squames) in the layer above. The proteins in these cells become cross – linked to form a tough proteinaceous scaffold. As they move upwards, these cells start to lose their nuclei and cytoplasmic organelles, and die. The dead cells become the keratinized ‘ squames ’ of the uppermostlayer.
The stratum lucidum
This is a fifth layer occasionally found in thick skin between the stratum granulosum and the stratum corneum layer. It is thin and transparent layer and difficult to identify in routine histological sections.
The stratum corneum ( keratinized cell layer)
This is the top, outermost layer and it consists of dead cells, that have become flatted and look like scales (or squames). These cells contain a tough layer of cross - linked keratins, on the inside bound to specialized lipids, on the outside to form a tough waterproof barrier. The squames eventually flake off (forming the main content of household dust).
The thickness of skin varies from 0.5 mm on the eyelids, to about 4.0 mm thick on the soles of the feet. Most of this difference is accounted for by the difference in thickness of the epithelium and, in particular, the cornified/keratinized cell layer .
The dermis
This layer provides protection, sensation, and thermoregulation. It contains nerves, blood vessels, and fibroblasts that secrete the extracellular matrix, and fibers (collagen and elastin). It also contains sweat glands (at the border with the hypodermis), which open out onto the surface of the skin.• The basal layer of the epidermis is folded into epidermal ridges, and between these ridges are folded regions of the underlying dermis, called dermal papillae.
• The dermal papillae are particularly prominent in thick skin (fingertips and the soles of feet).
The dermal papillae :
• increase adhesion between the dermal and epidermal layers;
• increase the overall surface area of the basal layer of the epidermis;and
• provide a large area of contact between the epidermis and blood vessels in the dermis.
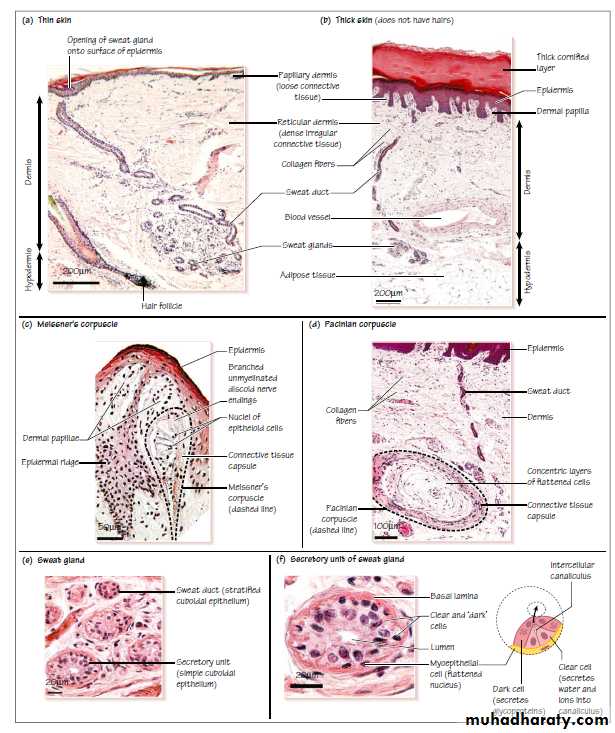
The dermis is divided up into two main regions. The superficial region is called the papillary dermis and the deeper region is called the reticular dermis .
The papillary dermis is the region of dermis that is found in and close to the dermal papillae. This region accounts for about 20% of the dermis. It contains loose connective tissue , capillaries, and nerves, both of which extend up towards the epidermis between dermal papillae.
The reticular dermis is the remaining region of dermis excluding the papillary dermis. It contains a layer of dense irregular connective tissue that contains collagen fibers, woven into a dense network, and elastin. Both of these are secreted by the Fibroblasts in this layer. These fibers give skin its strength and extensibility.
This layer also contains immune cells such as macrophages and fat cells (adipocytes), and the sweat glands, which are found deep in this region and in the hypodermis.
The hypodermis
This region of the skin mainly contains adipose tissue, and sweat glands . The adipose tissue is important for metabolic functions such as production of triglycerides and vitaminD.
The circulation of skin
• Arteries that supply the skin are found deep in the hypodermis (subcutaneous plexus).
• Branches from the arteries pass up towards the surface to form a deep (cutaneous) and a superficial (subpapillary) plexus.
• The pink color of skin is mainly due to the blood seen in venules.
• In cold conditions, blood flow to the superficial capillaries in skin is reduced to preserved core body temperature. In hot conditions, blood flow to the skin is increased and blood in superficial capillaries is cooled by the evaporation of sweat on the surface of the skin.
Encapsulated sense receptors in the dermis and hypodermis of skin
Meissner ’ s corpuscles : are fast - adapting mechano receptors found in dermal papillae. They contain an unmyelinated nerve fiber (sensory neuron derived from the dorsal root ganglia) which branches repeatedly, forming disc - shaped nerve endings within a capsule of connective tissue. They are found in the fingertips, soles of feet, lips, tongue, and genital areas, and they detect shape and texture.
Pacinian corpuscles .are fast - adapting, pressure – sensitive receptors found in the hypodermis. The afferent nerve ending is encapsulated by multiple concentric layers of flattened cells, surrounded by an external capsule of connective tissue.
Ruffini ’s corpuscles are similar to Pacinian corpuscles, and are found in reticular dermis of skin and in joint capsules (not shown here). They respond to stretch, and adapt slowly to stimulation.
These three receptors, together with Merkel cells are known as low threshold mechanoreceptors. Meissner ’ s and Pacinian corpuscles both respond to initial skin contact.
The epidermis of the skin also contains non - encapsulated, or free nerve endings, which lack connective tissue and Schwann cells, and sense cold, heat, and fine touch.
Glands
There are two types of glands in the skin: sweat glands . and sebaceous glands
The cells that form these glands are derived from the epithelium.
Sweat glands are simple tubular exocrine glands that contain secretory and excretory portions.
• The secretory portion is found deep in the dermis/hypodermis.
• The secretory units have a simple cuboidal epithelium, which contains ‘ clear cells ’ that secrete (by exocytosis) water, Na + and Cl − , and ‘ dark cells ’ that secrete glycoproteins to generate sweat.
This type of secretion is known as merocrine secretion. Sweat can also contain urea, ammonia, and lactic acid, and it is hypotonic to blood plasma.
• Myoepithelial cells surround the secretory units . They contract to help the secretory units expel fluid.
• The excretory portion (ducts) lie throughout the dermis, and open out into coiled excretory ducts on the surface of the epithelium at sweat pores. A stratified (2 layers) cuboidal epithelium lines the ducts .
• Sweat evaporation is important for thermoregulation.