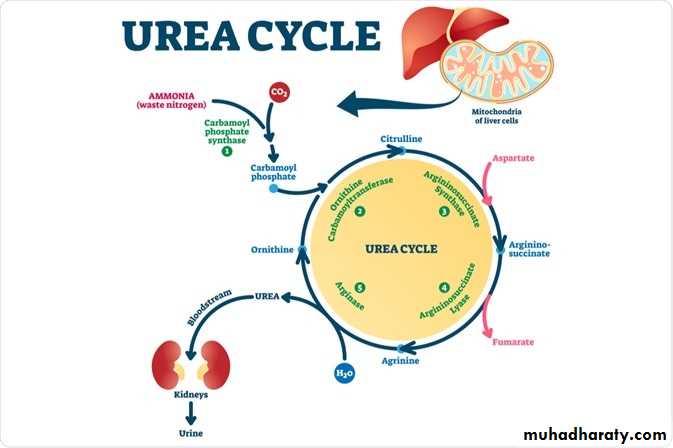
• Urea Cycle
• Dr.Ula Abbas Zeki• Urea is the major disposal form of amino groups that derived from amino acids and accounts for ~90% of the nitrogen-containing components of urine.
• contain 2 nitrogen, one nitrogen is supplied by free ammonia and the other nitrogen by aspartate.
• The carbon and oxygen of urea are derived from CO₂ (as HCO₃⁻)
• produced by the liver and then is transported by the blood to the kidneys to be excreted in urine.
Reactions
• The first two reactions leading to the synthesis of urea occur in the mitochondrial matrix, whereas the remaining cycle enzymes are located in the cytosol• Only the liver can cleave arginine, thereby synthesizing urea.
• Synthesis of urea is irreversible.
enzymes that catalyze urea cycle
1. carbamoyl phosphate synthetase, Rate-limiting reaction enz.2. ornithine carbamoyltransferase
3. argininosuccinate synthetase
4. argininosuccinate lyase
5. arginase
Net reaction of urea cycle
carb. phosphate +aspartate+ 4 ATP → urea + fumarate+ 2ADP + AMP+ PPi
Fate of urea
• •Urea diffuses from the liver and is transported in the blood to the kidneys, where it is filtered and excreted in the urine .• •A portion of the urea diffuses from the blood into the intestine and is cleaved to CO2 and ammonia by bacterial urease. The ammonia is partly lost in the feces and partly reabsorbed into the blood.
• •In patients with kidney failure, plasma urea levels are elevated, promoting a greater transfer of urea from blood into the gut.
• The intestinal action of urease on this urea becomes a clinically important source of ammonia, contributing to the hyperammonemia often seen in these patients.
• Oral administration of antibiotics reduces the number of intestinal bacteria responsible for this ammonia production.
• Ammonia is produced by all tissues during the metabolism of a variety of compounds, and excreted primarily by formation of urea in the liver.
• present at very low levels in blood due both to the rapid removal of blood ammonia by the liver and to the fact that several tissues, particularly muscle, release ammonia low amino acid nitrogen in the form of glutamine and alanine, rather than as free ammonia.
• Ammonia level must be kept very low in blood, because even slightly elevated concentrations (hyperammonemia) are toxic to the central nervous system (CNS).
Sources
• From amino acids: Many tissues, but particularly the liver, form ammonia from amino acids by transdeamination
• From glutamine: The kidneys form ammonia from glutamine by the actions of renal glutaminase and GDH. Most of this ammonia is excreted into the urine as NH₄⁺ which provides an important mechanism for maintaining the body's acid-base balance.
• Ammonia is also obtained from the hydrolysis of glutamine by intestinal glutaminase. The intestinal mucosal cells obtain glutamine either from the blood or from digestion of dietary protein.
3) From bacterial action in the intestine: Ammonia is formed from urea by the action of bacterial urease in the lumen of the intestine. This ammonia is absorbed from the intestine by way of the portal vein and is almost quantitatively removed by the liver via conversion to urea.
4) From amines: Amines obtained from the diet, and monoamines that serve as hormones or neurotransmitters, give rise to ammonia by the action of amine oxidase .
5) From purines and pyrimidines: In the catabolism of purines and pyrimidines, amino groups attached to the rings are released as ammonia.
Hyperammonemia
• Normally capacity of the hepatic urea cycle exceeds the rates of ammonia generation, so the levels of blood ammonia are normally low (5–35 μmol/l).• When liver function is compromised, due either to genetic defects of the urea cycle or liver disease, blood levels can be >1,000 μmol/l.
• Such hyperammonemia is a medical emergency, because ammonia has a direct neurotoxic effect on the CNS.
•• Elevated concentrations of ammonia in the blood cause the symptoms of ammonia intoxication, which include tremors, slurring of speech, drowsiness, vomiting, cerebral edema, and blurring of vision.
• At high concentrations, ammonia can cause coma and death.
two major types of hyperammonemia.
1. Acquired: Liver disease is a common cause in adults and may be due, for example, to viral hepatitis or to hepatotoxins such as alcohol.2. Congenital: Genetic deficiencies of any of the five enzymes of the urea cycle .
• ANY QUESTION?