
1
Antimicrobial chemotherapy
Drugs have been used for the treatment of infectious diseases since the
17th century (e.g. emetine for amebiasis); however, chemotherapy as a
science began in the first decade of the 20th century with an understanding
of the principles of selective toxicity, the specific chemical relationships
between microbial pathogens and drugs, the development of drug
resistance, and the role of combined therapy.
The development of antimicrobial chemotherapy began in 1935 with the
discovery of the sulfonamide. In 1940, it was demonstrated that penicillin,
discovered in 1929, could be an effective therapeutic substance. During the
next 25 years, research on chemotherapeutic agents centered largely
around substances of microbial origin called antibiotics. The isolation,
concentration, purification, and mass production of penicillin were
followed by the development of streptomycin , tetracyclines and many
other agents.
1- bactericidal drugs :- these have a rapid lethal action, e.g. penicillins,
cephalosporins & aminoglycosides .
2- Bacteriostatic drugs: - these are inhibiting the division, i.e. growth of
organism, e.g. sulfonamides , tetracyclines & chloramphenicol .
Range of action of antibiotics
Antibiotics fall into 3 main categories :-
a – active mainly against G
+ve
organisms like: penicillin, erythromycin &
lincomycin.
b – active mainly against G
-ve
organisms like : polymyxin & nalidixic acid
.
c – active against both G
+ve
& G
-ve
organisms ( broad spectrum activity )
like : ampicillin & ciprofloxacin .
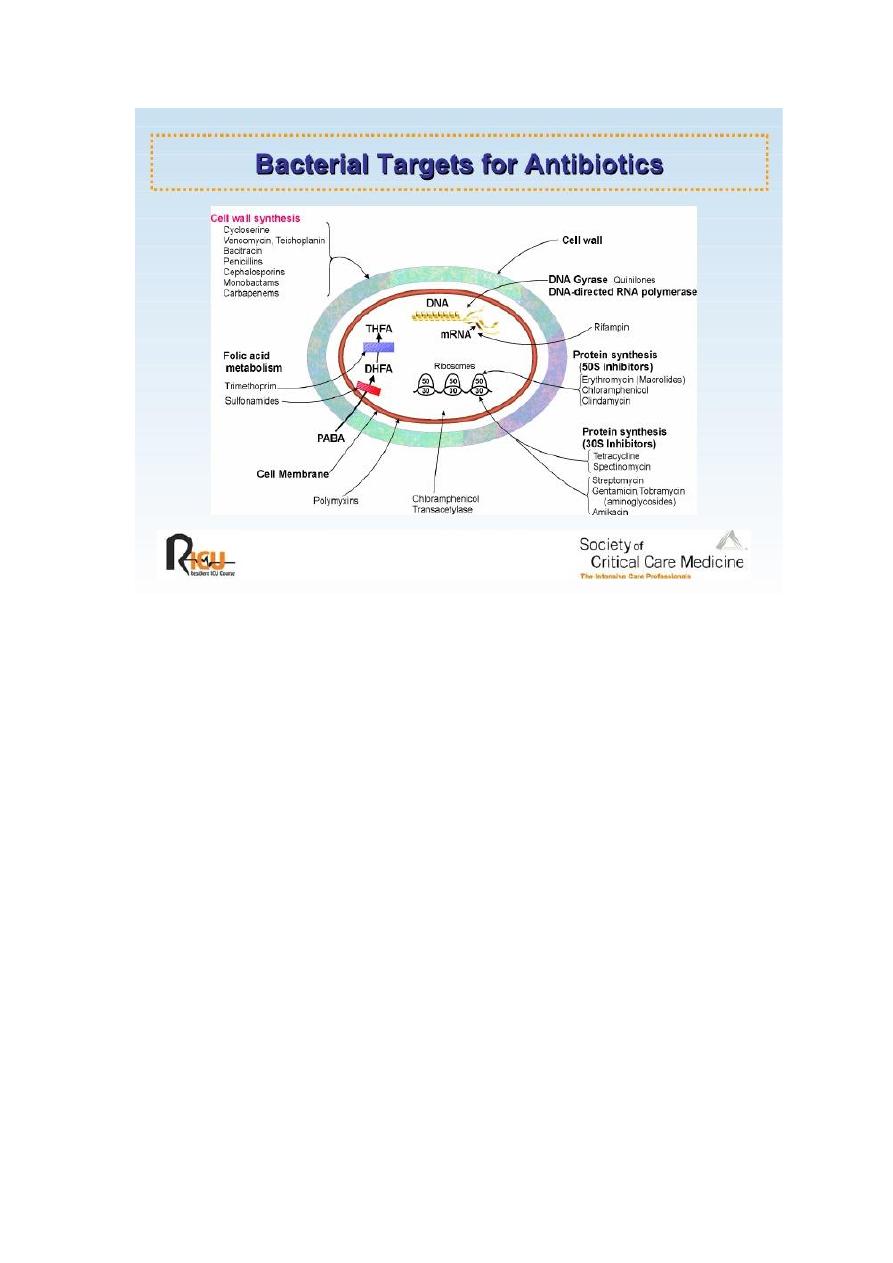
Mechanisms of action of chemotherapeutic agents
An ideal antimicrobial agent should have selective toxicity i.e. it can
kill or inhibit the growth of a microorganism in concentration that are not
harmful to the cells of the host . Disinfectants e.g. phenol and antiseptics
e.g. alcohol & iodine , destroy bacteria but they are highly toxic to tissue
cells & are unsuitable for use as chemotherapeutic agents .
Thus, the mechanisms of action of a chemotherapeutic agent must
depend on the inhibition of a metabolic channel or a structure present in
the microbe but not in the host cells . several mechanisms are known :-

2
1 – Inhibition of cell wall synthesis :-
Due to its unique structure & function , the bacterial cell wall is an ideal
point of attack by selective toxic agents , such as ß-lactams that include
penicillins & cephalosporins interfere with cell wall synthesis and cause
bacteriolysis .
2 – Inhibition of cytoplasmic membrane function :-
Some antibiotics cause disruption of the cytoplasmic membrane and
leakage of cellular proteins & nucleotides leading to cell death , for
example polymyxins.
3 – Inhibition of protein synthesis :-
Many chemotherapeutic block protein synthesis by acting on the 30
s
or 50
s
subunit of bacterial ribosomes such as : tetracyclines , erythromycin
and aminoglycosides e.g. tobramycin & gentamycin . Bacteria have 70
s
ribosome while mammalian cells have 80
s
ribosome the composition of
each type ,their subunit and function explain why drugs can inhibit protein
synthesis in bacteria but not in mammal .
4 – Inhibition of nucleic acid synthesis :-
These can act on any steps of the DNA replication or RNA synthesis,
e.g. quinolone, refampicin, novobiocin & sulfonamide. rifampen inhibit
bacterial growth by binding to DNA-dependent RNA polymerase of
bacteria , thus it inhibits RNA synthesis . While quinolones inhibit DNA
synthesis by blocking of DNA gyrase.
5 – Competitive inhibition :-
In which the drugs compete with an essential metabolite for the same
enzyme e.g. p – aminobenzoic acid ( PABA ) is an essential metabolite
for many organisms because its precursor in folic acid synthesis, which is
used in nucleic acid synthesis , sulfonamide are structural analogues to
PABA so its enter into the reaction in place of PABA & compete for the
active center of the enzyme thus inhibiting folic acid synthesis .
3
Mechanisms of resistance to antimicrobial agents
In the treatment of infectious diseases, one of the serious problems is
the development of bacterial resistance to the antibiotic used . The
mechanisms by which the organism develops resistance may be one of the
following:-
1 – The organism produced enzymes that destroy the drug e.g. production
of ß–lactamases that destroy penicillin by penicillin resistant staphylococci
& acetyltransferase which produced by gram negative bacilli to destroy
chloramphenicol.
2 – The organism change its permeability to the drug by modification of
protein in the outer cell membranes, thus impairing its active transport into
the cell e.g. resistance to polymyxins.
3 – The organism develops an altered receptor site for the drug e.g.
resistance to aminoglycosides is associated with alteration of a specific
protein in the 30
s
subunit of the bacterial ribosome that serve as a binding
site in susceptible organisms.
4 – The organism develop an altered metabolic pathway that by passes the
reaction inhibited by the drug e.g. sulfonamide-resistant bacteria acquire
the ability to use performed folic acid with no need for extracellular PABA.

4
Origin of resistance to antimicrobial agents
These mechanisms may be of non genetic or genetic origins:
A – Non genetic drug resistance :- this include
1 – Metabolic inactivity :- Most antimicrobial agents act effectively only
on replicating cells , non multiplying organisms is phenotypically resistant
to drugs such as M. Tuberculosis, which survive for years in the tissues &
their resistance is due to metabolic inactivity, but if they start to multiply
after suppression of cellular immunity of the patient , they become
susceptible to the drugs .
2 – Loss of target structure :- Protoplast or L-forms of bacteria are
penicillin resistant because they lost their cell wall which is a structural
target site of the drug .
3 – Bacteria may infect the host in the sites where antimicrobial is
excluded or not active.
B – Genetic drug resistance :- this include
1 – Plasmid mediated resistance :- Plasmid is an extra-chromosomal
genetic elements associated with bacterial resistance to antibiotics ,
plasmids frequently carry many genes that code for the production of
enzymes that inactivate or destroy the antibiotics e.g. ß- lactamases which
destroys the ß- lactam ring in penicillin & cephalosporin , plasmids may
result in epidemic resistance among bacteria by moving from one to the
other by conjugation , transduction or transformation .
2 - Transposon-mediated resistance :- Many transposons carry genes
that code for drug resistance , as they move between plasmids &
chromosomes they can transfer this property to bacteria . The process
called transposition .
3 – Chromosomal drug resistance :- This develops as a result of
spontaneous mutation in a gene that controls susceptibility to an
antimicrobial agent , the most common result of chromosomal mutation is
an alteration of the receptors for a drug . For example : streptomycin
resistance can result from a mutation in the chromosomal gene that controls
the receptor for streptomycin located in the 30s
bacterial ribosome .

5
Complications of antibacterial chemotherapy
1 – Development of drug resistance :-
This is one of the most serious complications of chemotherapy , the
emergence of resistant mutants is encouraged by inadequate dosage ,
prolonged treatment , the presence of closed focus of infection and the
abuse of antibiotics without in vitro susceptibility testing . The problem is
more serious when resistant strain develops in the community, e.g. in
hospitals its common finding that about 90 % of Staphylococcus aureus
strains are resistant to penicillin .
2 – Drug toxicity :-
Many of antibacterial drugs have toxic side effects , this can be due to
the over dosage , prolonged use or narrow margin of selective toxicity, e.g.
streptomycin effect on the 8
th
cranial nerve leading to deafness ,
aminoglycosides are nephrotoxic , tetracyclines inhibit growth &
development of the bones and teeth in the developing infants & children .
3 – Super infection :-
a – this may occur by pre-existing resistance strains present in the
environment e.g. penicillin resistance Staph. aureus in hospital infection .
b – Another type of super infection is due to suppression of normal flora
by the antibiotic used and their replacement with drug resistant organisms
which cause disease like : Candida in the mouth causing oral thrush .
4 – Hypersensitivity :-
The drug may act as hapten, binds to tissue proteins and stimulates an
immune response leading to tissue damage i.e hypersensitivity .
Any type of hypersensitivity reaction can occur with the several
antibiotics . The most serious is anaphylactic shock which may occur with
penicillin & cephalosporins . Mild manifestations are urticaria , skin rash ,
diarrhea , vomiting and jaundice .

6
Chemoprophylaxis
Is the use of antimicrobial agents to prevent rather than to treat
infectious diseases . The following are the principal conditions for which
prophylactic antibiotics are positively indicated:-
1 – The use of benzathine penicillin G injections every 3-4 weeks to
prevent reinfection with Streptococcus pyogenes in rheumatic patients
2 – A single large dose of amoxicillin given immediately prior to dental
procedures is recommend for patients with congenital or rheumatic heart
disease to prevent endocarditis .
3 – Rifampicin 600 mg twice a day for 2 days give to the exposed patients
during epidemics of meningitis .
4 – Oral administration of tetracycline to prevent cholera .
5 – The use of ampicillin to prevent neonatal sepsis & meningitis in
children born to mothers carrying group B streptococci in the vagina .
6 – Ceftriaxone to prevent gonorrhea .
7 – Chemoprophylaxis in surgery .
Clinical use of antibiotics
The following principles should be observed :-
1 – Antibiotics should not be given for viral infections .
2 – They used for prophylaxis in special conditions .
3 – Treatment should be based on a clear clinical and bacteriological
diagnosis .
4 – Antibiotics for systemic treatment must be given in a full therapeutic
doses for adequate period .
5 – Combined therapy with two or more antibiotics is required for some
conditions : -
a. serious resistant infections such as meningitis .
b. Severe mixed infections e.g. peritonitis following perforation of the
colon.
