يَرْفَعْ اللَّهُ الَّذِينَ آمَنُوا مِنْكُمْ وَالَّذِينَ أُوتُوا الْعِلْمَ دَرَجَاتٍ وَاللَّهُ بِمَا تَعْمَلُونَ خَبِيرٌ
صدق الله العلي العظيم
سورة المجادلة: الآية:11
Blood Physiology By Dr. Suroor MohamedMBChB. MSc, Physiology
OBJECTIVES:1-Describe Cellular and non-cellular components of blood
2-Recognise features of blood and functions
3-Define Erythropoiesis, leucopoiesis and thrombopoiesis.
4-Recognize sites of RBC formation at different developmental age.
5-What is mean by Polycythemia?
Blood:
It is a specialized circulating fluid connective tissue composed of cells suspended in fluid intercellular substances called plasma.It supplies O2 and nutrients & removes CO2 with waste products to all regions of the body.
Characteristics of Blood
Major Functions of Blood
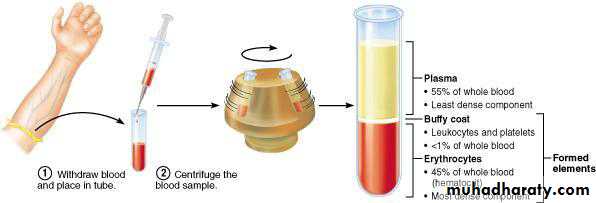
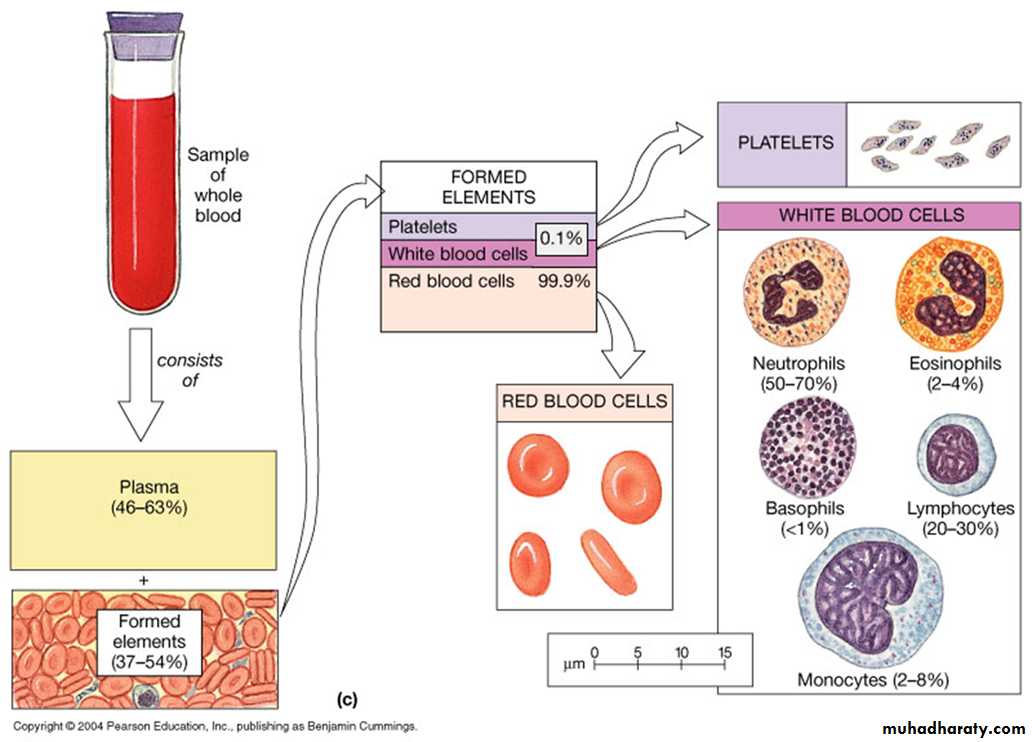
• B-protection from foreign material & infections by leukocytes, antibodies& complement proteinsCellular components:Red Blood Cells (Erythrocytes) transport O2White Blood Cells (Leucocytes) part of the immune systemPlatelets (Thrombocytes) cell fragments involved in clotting Plasma ( liquid “ non cellular” part )98% water, ions, plasma proteins (Albumin, globulin, Fibrinogen , enzymes and hormones)Same ionic composition as interstitial fluid
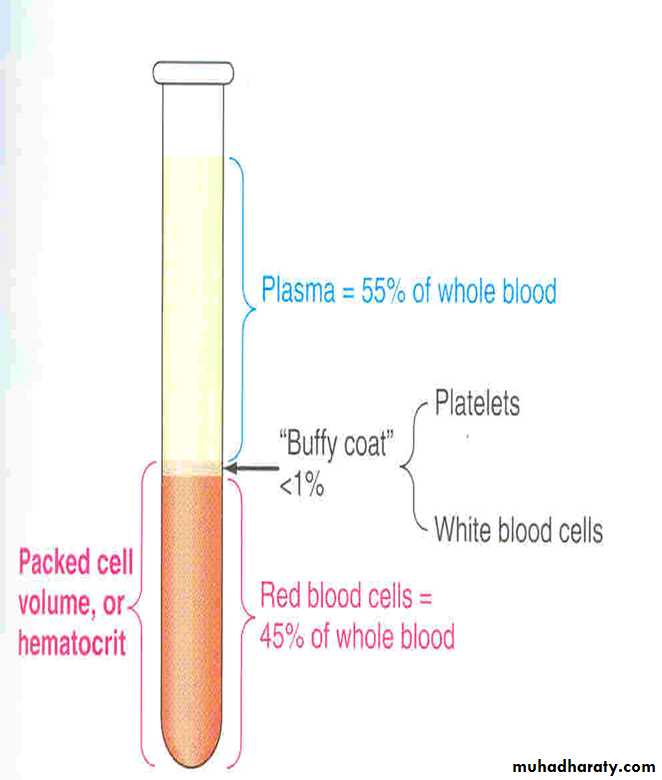
• 5 liter in adult45% is packed cells volume (PCV)
• 55% is plasma volume•
PLASMA
Is the fluid portion of the blood. It contains proteins ,inorganic and organic substances. If left stand, it will clot. Removing the clot will leave serum which is identical to plasma in its constituents except for fibrinogen, clotting factors(prothrombin,factor V and VIII ).Also serum has higher quantities of serotonin (vasoconstrictors because of the breakdown of platelets.
Is similar to, and exchanges fluids with, interstitial fluid
Is matrix of formed elements
Blood plasma Consists of:
•Water 90%
• Plasma Proteins % 6-8
• Electrolytes (Na+ & Cl-) 1%
Other components:
• Nutrients )e.g. Glucose and amino acids(
• Hormones )e.g. Cortisol, thyroxine(
•Wastes )e.g. Urea(
• Blood gases (e.g. CO2, O(2
Plasma Proteins:(albumins, globulins, fibrinogen)
1. Maintaining colloid osmotic balance (albumins)
2. Buffering pH changes
3. Transport of materials through blood (such as water insoluble hormones
4. Antibodies (e.g. gamma globulins, immunoglobulins(
5. Clotting factors (e.g. fibrinogen(
Electrolytes:
* Membrane excitability.
* Osmotic distribution of fluid between ECF
(extracellular fluid) & ICF(intracellular fluid.(
* Buffering of pH changes.
Plasma component
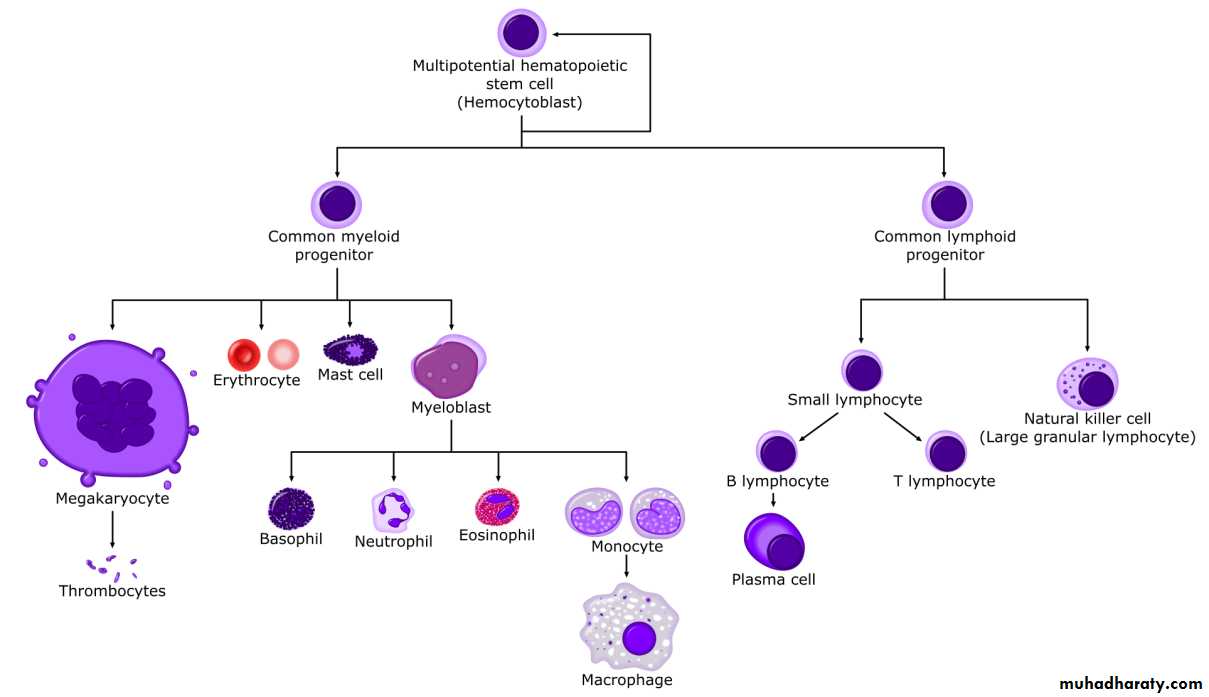
• HemopoiesisHematopoiesis the formation and development of blood cellsIn adults the cellular elements are produced in the bone marrow.Some WBCs are produced in the lymphatic tissue and bone marrow.***All blood cells formed come from a hematopoietic stem cell.Process of producing formed elements by myeloid and lymphoid stem cells Erythropoiesis: Formation of RBC (erythrocytes)Leucopoiesis: Formation of WBC (leucocytes) Thrombopoiesis: Formation of platelets (thrombocytes)
In the adult, red blood cells, many white blood cells, and platelets are formed in the bone marrow. In the fetus, blood cells are also formed in the liver and spleen, and in adults such extramedullary hematopoiesis may occur in diseases in which the bone marrow becomes destroyed or fibrosed.
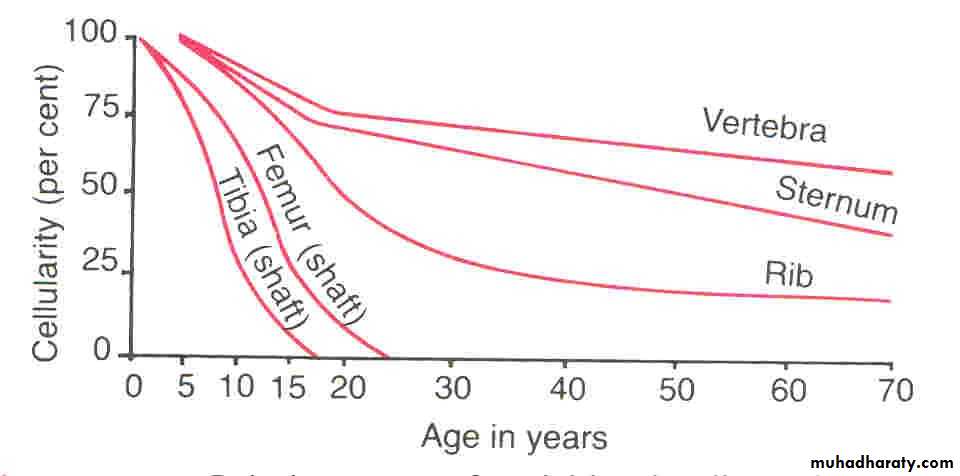
In children, blood cells are actively produced in the marrow cavities of all the bones. By age 20, the marrow in the cavities of the long bones, except for the upper humerus and femur, has become inactive . Active cellular marrow is called red marrow; inactive marrow that is infiltrated with fat is called yellow marrow.
Normally, 75% of the cells in the marrow belong to the white blood cell-producing myeloid series and only 25% are maturing red cells, even though there are over 500 times as many red cells in the circulation as there are white cells. This difference in the marrow reflects the fact that the average life span of white cells is short, whereas that of red cells is long.
The bone marrow contains multipotent uncommitted stem cells (pluripotential stem cells) that differentiate into one or another type of committed stem cells (progenitor cells). These in turn form the various differentiated types of blood cells. There are separate progenitor cells for megakaryocytes, lymphocytes, erythrocytes, eosinophils, basophils, neutrophils and monocytes .
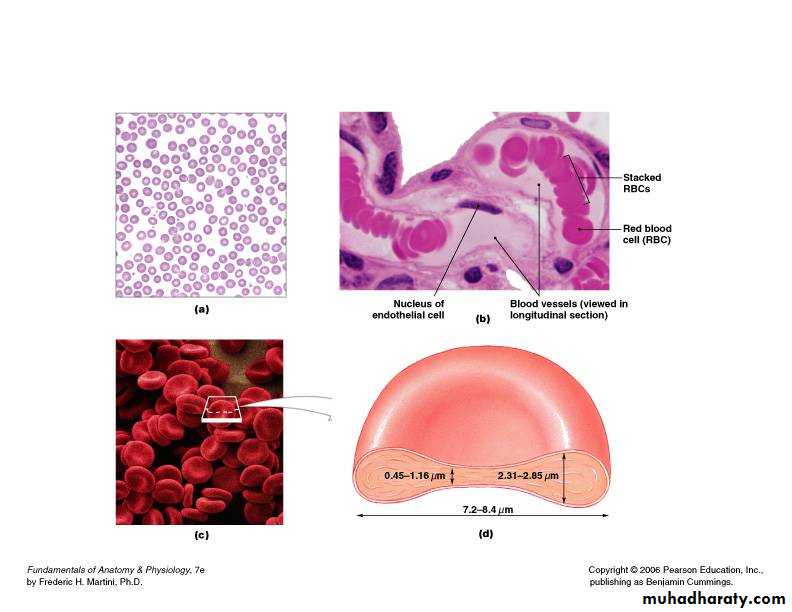
RBCs Erythrocyte
• Most abundant cell in the blood (4 million – 6 million per microliter of blood)• Formed in the bone marrow
• Mature forms do NOT have a nucleus , mitochondria and ribosomes
• Shaped as biconcave disc (why?)
• 6-8 micrometers in diameter
***Life span of about 120 days
RBCs are narrow & flexible for excellent fluidity especially within the small capillaries
• Hemoglobin (iron protein)is found in the RBC , Hb carries oxygen from the lungs to the rest of the body and carbon dioxide binds to the RBC and is taken to the lungs to be exhaled.
• Production of RBC
• Early few weeks of embryo nucleated RBCs are formed in yolk sac.• Middle trimester mainly in liver & spleen & lymph nodes.
• Last months RBCs are formed in bone marrow of all bones
• Bone marrow of flat bone continue to produce RBC into adult life
• Shaft of long bone stop to produce RBC at puberty while epiphysis continued
• Hematopoiesis and Erythropoiesis: hematopoiesis (hemopoiesis) - the maturation, development and formation of blood cells
• A- red bone marrow (myeloid tissue) - location of hematopoiesis; mainly in axial skeleton and heads of femur & humerus
B-hemocytoblast (stem cell) - the mitotic precursor to blood cells before differentiation
• Erythropoiesis - the maturation, development, and formation of Red Blood Cells
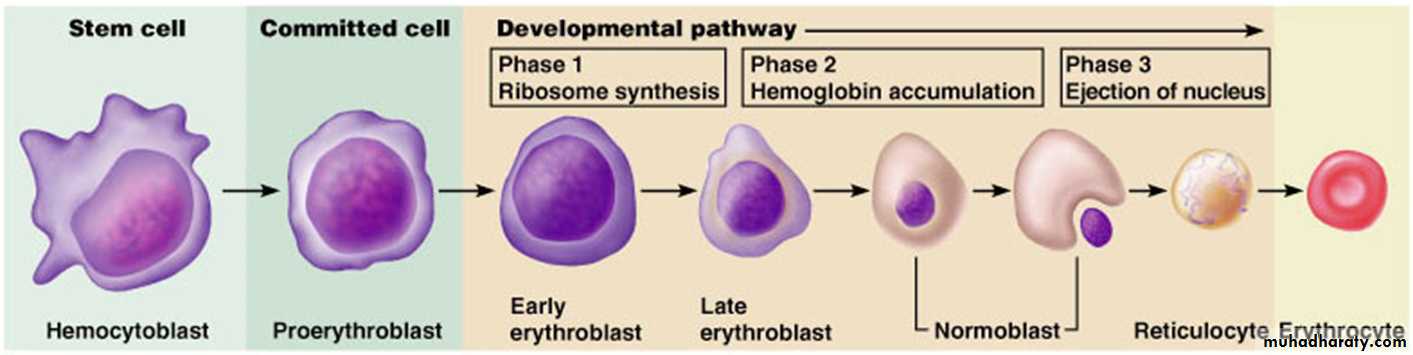
• hemocytoblast ->proerythroblast ->early (basophilic) erythroblast ->late (polychromatophilic) erythroblast ->(hemoglobin) normoblast -> (nucleus ejected when enough hemoglobin)reticulocyte -> (retaining some endoplasmic reticulum)
ERYTHROCYTE life span:
hemocytoblast -> reticulocyte 3-5 DAYSreticulocyte -> ERYTHROCYTE 2 DAYS (in blood)
ERYTHROCYTE lifespan 100-120 Days
(primarily destroyed by macrophages in the spleen)
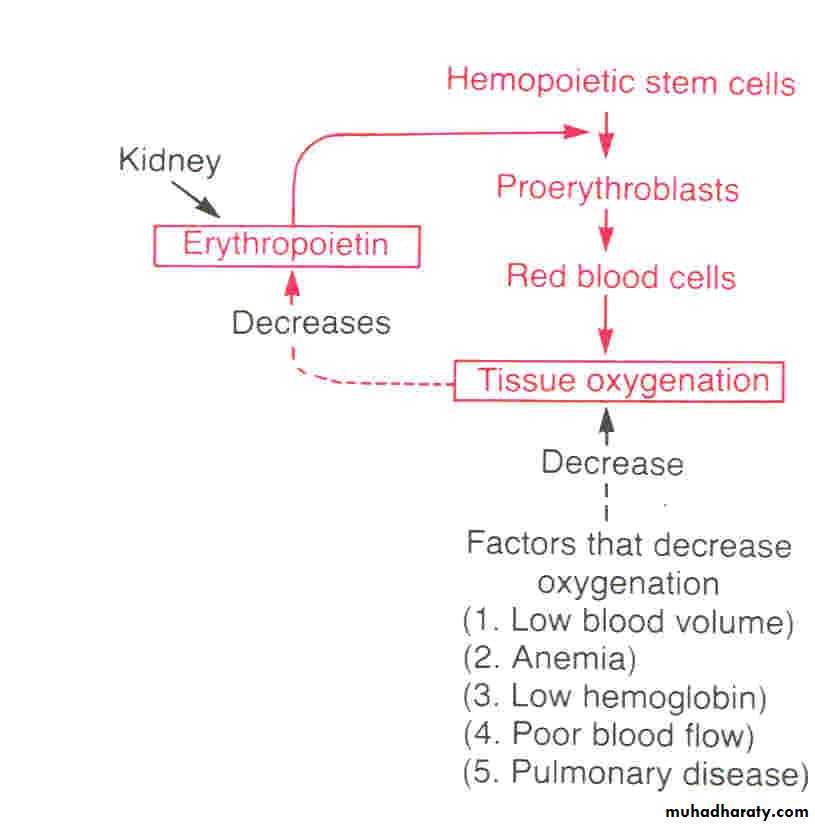
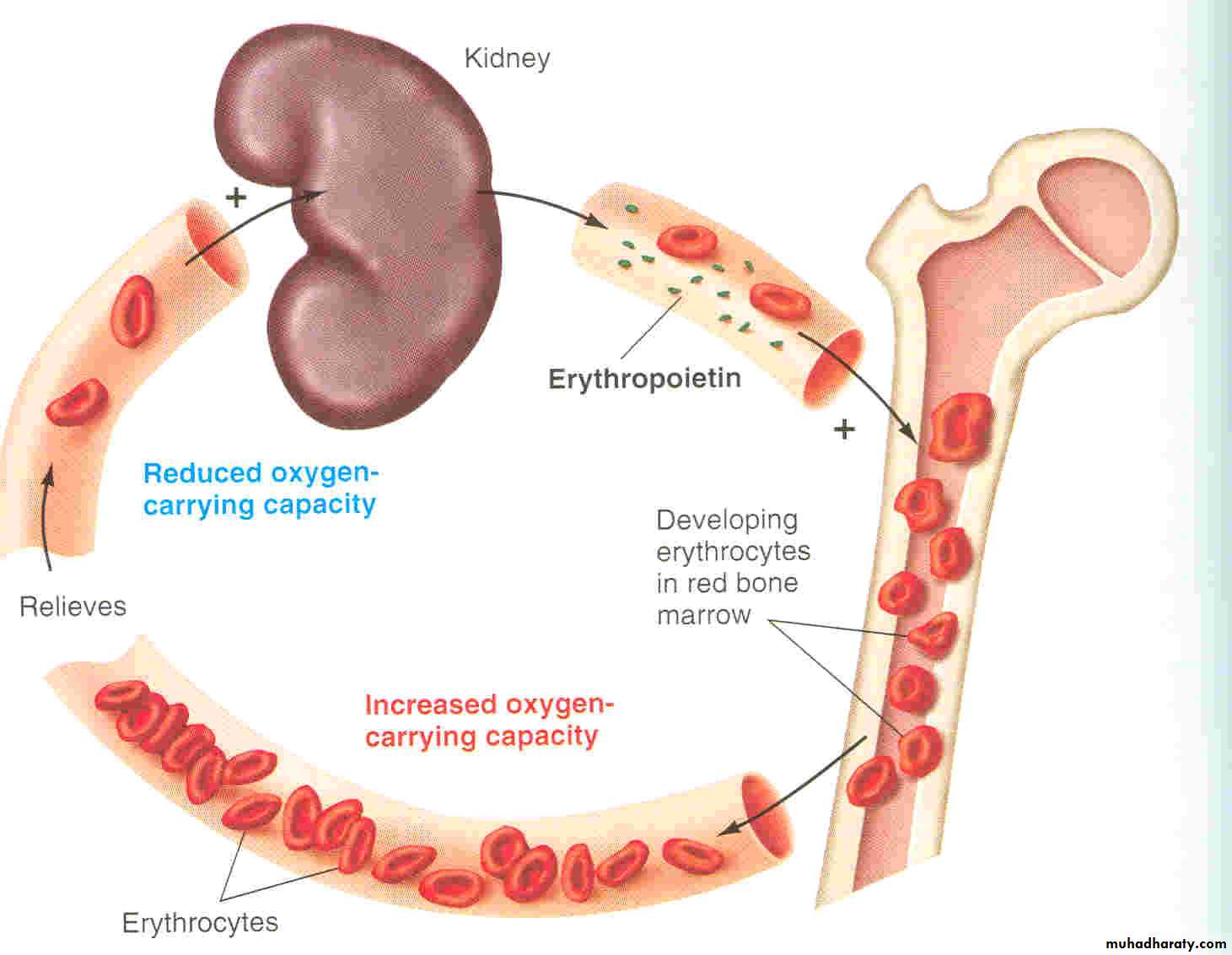
• Regulation of Erythropoiesis
1- Erythropoiesis is stimulated by erythropoietin hormone produced by the kidney in response to hypoxia (low oxygen in the blood)
• Hypoxia caused by:
• . Less RBCs from bleeding
• . Less RBCs from excess RBC destruction
• . Low oxygen levels (high altitude, illness)
• . Increased oxygen demand (exercise)
• . Erythropoietin
• Is Glycoprotein 90% from renal cortex 10% liver• Stimulate the growth of early stem cells
• Does not affect maturation process
• Can be measured in plasma & urine
• High levels of erythropoietin
• anemia
• -High altitude Polycythemia
• Heart failure
• Lungs disease
• B- Iron - essential for hemoglobin to carry oxygen
• 1- 65% of Fe in body is in hemoglobin
• 2-liver and spleen store most excess Fe bound to ferritin and hemosiderin
• . 3-Fe in blood bound to transferrin
• 4-daily Fe loss: 0.9 mg men/l.7 mg women
• C – Vitamins as B-complex - Vit B12 and Folic Acid essential for DNA synthesis in early mitotic divisions leading to erythrocytes
abnormally high hematocrit (too many RBCs incirculation)
• Increase production of RBCs (count 6-8 milio/mm3)its of 2 types:
• 1.primarypolycythemia vera(count7-8 milio/mm3)
• 2.Secondary due to tissue hypoxia like in high altitude or chronic smokers
-Primary: erythropoiesis proceeds at an excessive, uncontrolled rate, not subjected to normal erythropoietin regulatory mechanism that makes blood super viscous.
Polycythemia Vera (Erythremia) :. It a pathological condition, in which the red blood cell count may be 7 to 8 million/mm3 and the hematocrit may be 60 to 70 per cent instead of the normal 40 to 45 per cent. Polycythemia vera is caused by a genetic aberration in the hemocytoblastic cells that produce the blood cells. The blast cells no longer stop producing red cells when too many cells are already present. In polycythemia vera, the hematocrit increase,and the total blood volume also increases, up to twice normal
-Secondary: an appropriate erythropoietin-induced adaptive mechanism to improve blood’s oxygen carrying capacity in response to a prolonged reduction in oxygen delivery to the tissues. (normally in people at high elevations- where less oxygen is available in the atmosphere) due to hypoxia affect.
• Polycythemia :
• Secondary Polycythemia. When the tissues become hypoxic because of too little oxygen in the breathed air, such as at high altitudes, or because of failure of oxygen delivery to the tissues, such as in cardiac failure, the blood-forming organs automatically produce large quantities of extra red blood cells. This termed secondary polycythemia, and the red cell count commonly rises to 6 to 7 million/mm3, about 30 per cent above normal.
• A common type of secondary polycythemia, called physiologic polycythemia, occurs in natives who live at altitudes of 14,000 to 17,000 feet, where the atmospheric oxygen is very low , pregnancy & smoking person.
• Effect of polycythemia on circulation
• 1. increases the viscisity of blood leads to sluggish circulation this leads to thrombosis.
• 2.Blood pressure increases , increase work load on the heart leads to heart failure.
• Tretment by venesection