3rd Stage
Helicobacter pylori
Microbiology
lab
1
Helicobacter pylori
History of H. pylori
• 1890’s: Spirochetes in animal stomachs
• 1900’s: Spirochetes in human stomachs
• 1954: No bacteria in gastric biopsies of 1000 patients
• 1975: Gram negative bacteria in 80% of GU’s (Pseudomonas)
• 1983: Warren and Marshall characterize H. pylori
• 2005 Nobel prize in 2005
Background
Human stomach long considered inhospitable for bacteria
Spiral shaped organisms occasionally visualized in gastric mucous
layer, but no evidence of disease association
Organism classified first as Campylobacter pylori
Now Helicobacter pylori
Other species of Helicobacter isolated from stomach, intestine of
other animals
Marshall and Warren culture organism from human gastric mucosa
and show association with gastric inflammation
Helicobacter
( Warren and Marshal )
• Campylobacter like organisms
• Spiral shaped colonizes Gastric mucosa
• Etiological agent in Gastritis and peptic ulcer
• Most important bacteria.
Helicobacter pylori
Colonizes 50 % of the Individuals
3rd Stage
Helicobacter pylori
Microbiology
lab
2
General Characteristics of Helicobacter
• Helicobacter pylori is major human pathogen associated with gastric
antral epithelium in patients with active chronic gastritis
• Stomach of many animal species also colonized
• Urease (gastric strains only), mucinase, and catalase positive highly
motile microorganisms
• Other Helicobacters: H. cinnaedi and H. fenneliae
• Colonize human intestinal tract
• Isolated from homosexual men with proctitis, proctocolitis, enteritis,
and bacteremia and are often transmitted through sexual practices
• Gram –ve spiral shaped , motile with unipolar tuft of lopotrichus
flagella
H. pylori Bacteria
• Gram negative
• Spiral rod
• Unipolar flagella
• Microaerophilic
• Urease positive
(Most important character)
Morphology & Physiology of Helicobacter
• Gram-negative; Helical (spiral or curved) (0.5-1.0 um X 2.5-5.0 um);
Blunted/rounded ends in gastric biopsy specimens; Cells become rod-
like and coccoid on prolonged culture
• Produce urease, mucinase, and catalase
• H. pylori tuft (lophotrichous) of 4-6 sheathed flagella (30um X 2.5nm)
attached at one pole
• Single polar flagellum on H. fennellae & H. cinaedi
3rd Stage
Helicobacter pylori
Microbiology
lab
3
• Smooth cell wall with unusual fatty acids
H. pylori Infection transmission
• Transmissible
• Oral-oral and oral-fecal
• Infects the human stomach
• Produces inflammatory response
• This brings up the point of the importance of “hand washing”
Dynamics of H.pylori infection
Culturing and Biochemical characters
• Grows on chocolate agar, Campylobacter media
• Grows under Microaerophilic conditions
• With presence of 5 – 20% co2
• Oxidase +
• Catalase –
• Urease strongly +++
• H2S
3rd Stage
Helicobacter pylori
Microbiology
lab
4
Pathology and pathogenesis
• H.pylori colonizes gastric mucosa
• Spread by oral – oral contact
• Feco oral spread prominent
• Poverty and overcrowding predisposes
• Poor Hygiene
• Causes mild to acute gastritis
• Gastric antrum - causes gastric metaplasia
• Any part of the stomach can be involved
• Colonizes overlying mucosa but donot invade mucosa
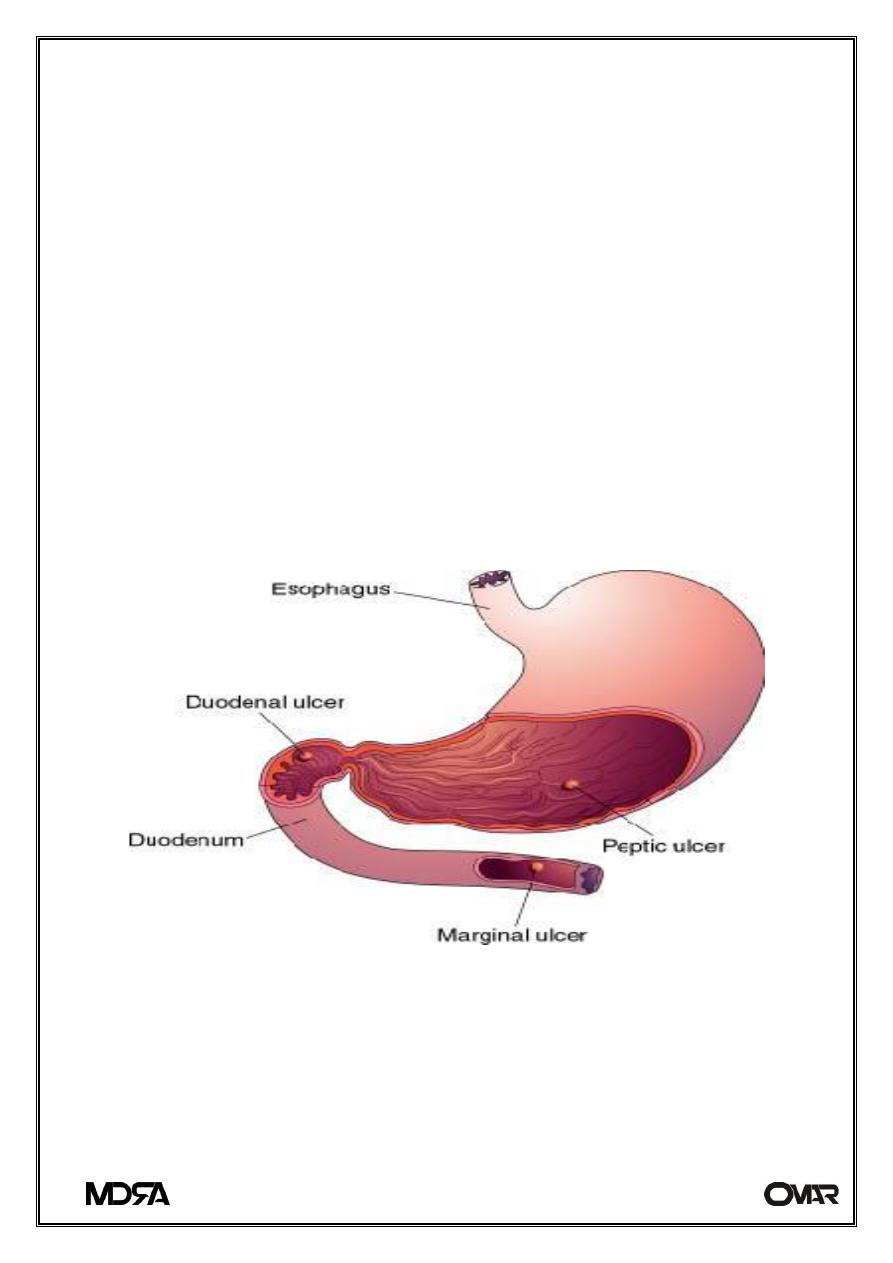
Major Location of H.Pylori infections
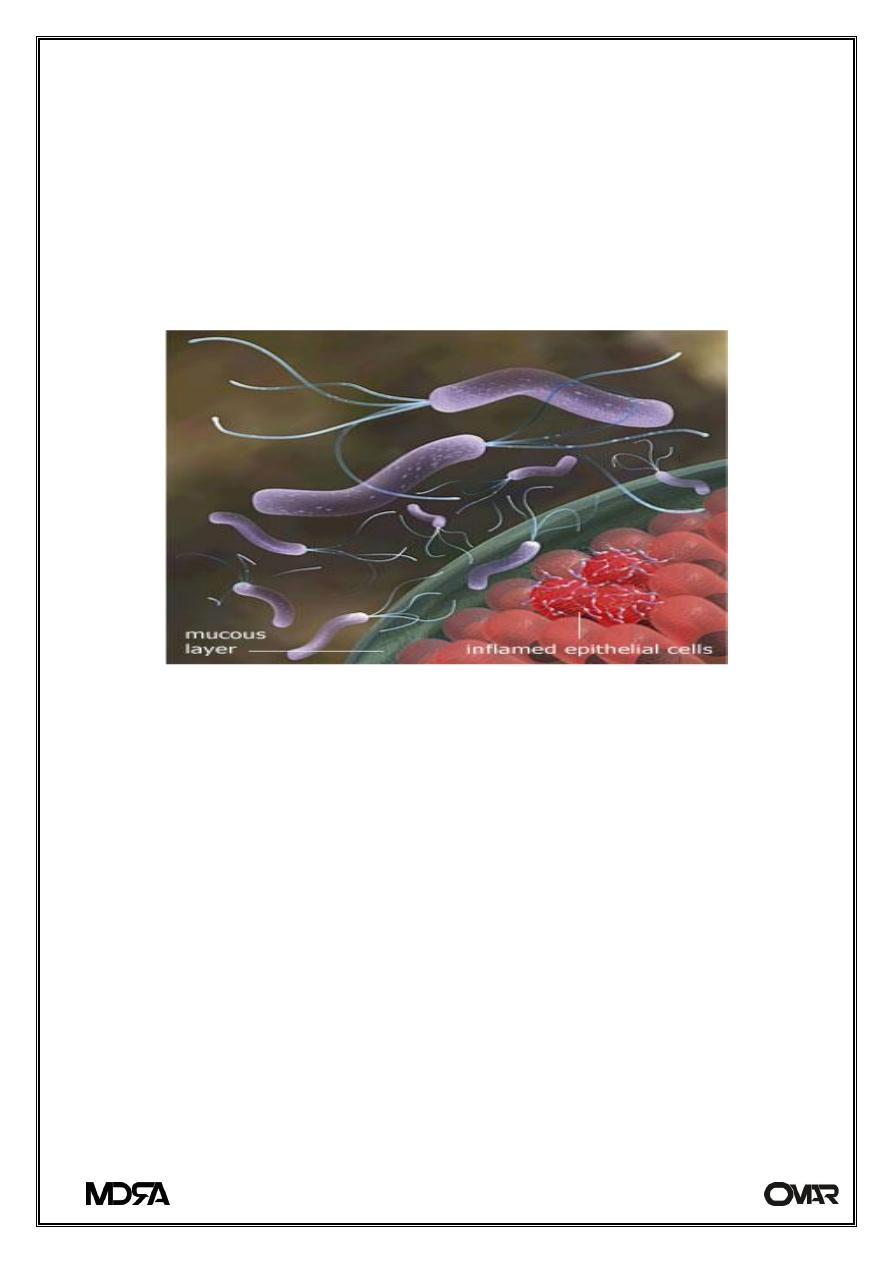
Pathogenesis of Helicobacter Infections
Colonize mucosal lining of stomach & duodenum in man & animals
• Adherent to gastric surface epithelium or pit epithelial cells deep
within the mucosal crypts adjacent to gastric mucosal cells
3rd Stage
Helicobacter pylori
Microbiology
lab
5
• Mucosa protects the stomach wall from its own gastric milleu of
digestive enzymes and hydrochloric acid
• Mucosa also protects Helicobacter from immune response
Most gastric adenocarcinomas and lymphomas are concurrent with or
preceded by an infection with H. pylori
H.pylori infecting Mucosal layer
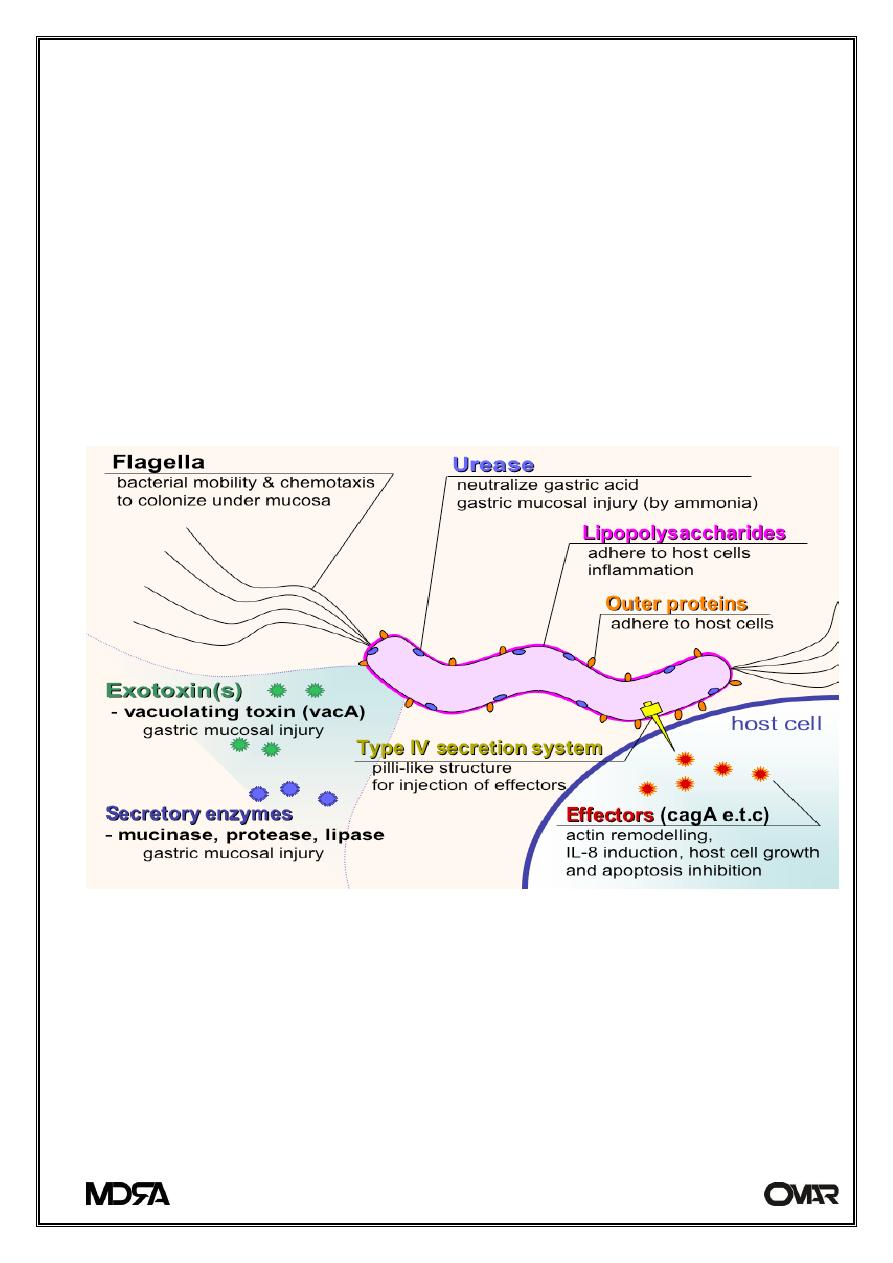
Virulence Factors of Helicobacter
Multiple polar, sheathed flagella
Corkscrew motility enables penetration into viscous environment
(mucus)
Adhesins: Hemagglutinins; Sialic acid binding adhesin; Lewis blood group
adhesin
Mucinase: Degrades gastric mucus; Localized tissue damage
Urease converts urea (abundant in saliva and gastric juices) into
bicarbonate (to CO
2
) and ammonia
Neutralize the local acid environment
Localized tissue damage
Acid-inhibitory protein
3rd Stage
Helicobacter pylori
Microbiology
lab
6
Tissue damage:
Vacuolating cytotoxin: Epithelial cell damage
Invasin(s)(??): Poorly defined (e.g., hemolysins; phospholipases;
alcohol dehydrogenase)
Protection from phagocytosis & intracellular killing:
Superoxide dismutase
Catalase
Types of H. pylori Tests
Laboratory Diagnosis
• Diagnosed by Invasive and Non Invasive tests
• Invasive, Endoscopic Biopsy of Gastric mucosa
• Microscopy – Biopsy
• Culture
• Staining by special stains
• Gram staining
• Culture more sensitive 3 – 7 days
• Biopsy testing for urease detection in urea medium
•
Endoscopy
•
Rapid urease tests
•
Histology
•
Culture
•
Serologic (antibody)
•
Stool antigen tests
•
13
C Urea blood test
•
Urea breath tests
•
14
C
-urea
•
13
C
-urea
3rd Stage
Helicobacter pylori
Microbiology
lab
7
Laboratory Identification
Recovered from or detected in endoscopic antral gastric biopsy
material; Multiple biopsies are taken
Many different transport media
Culture media containing whole or lysed blood
Microaerophilic
Grow well at 37oC, but not at 25 nor 42oC
Like Campylobacter, does not use carbohydrates, neither
fermentatively nor oxidatively
Diagnosis by Non invasive methods
• Serology ELISA
• Urea breath test patient swallows urea solution
In this test patient drinks urea solutions labeled with an isotope carbon
If H.pylori is present in the urea is converted to ammonia and co2 in the
breath measured.
Treatment
• Use of antibiotics, bismuth salts
• Ingestion of Bismuth subsalicylate
• Antibiotics Tetracycline's and metronidazole for two weeks
• Use of Omeprazole
• Clarithromycin
• Do not treat for Asymptomatic colonization
• Drug resistance is a growing problem
