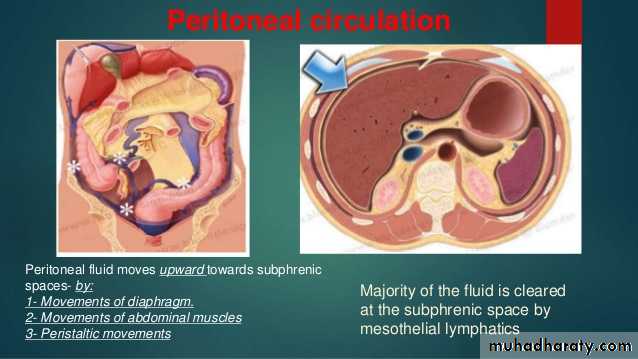
Functions of the peritoneum
In healthVisceral lubrication
Fluid and particulate absorption
In disease
Pain perception (mainly parietal)
Inflammatory and immune responses
Fibrinolytic activity
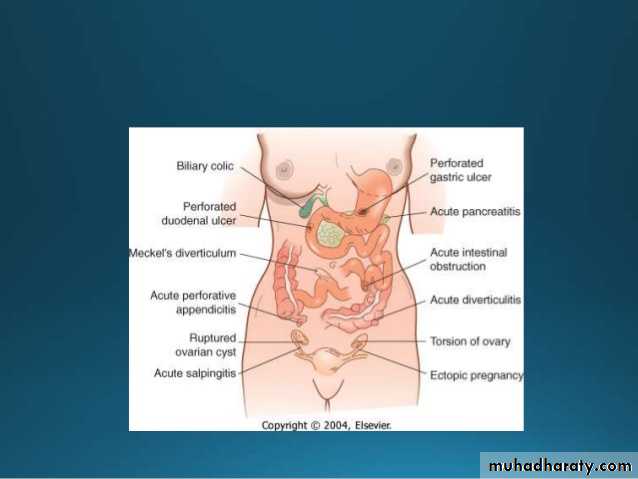
Jejunal perforation due to trauma. Trauma is the common cause for jejunal perforation. It is commonly blunt abdominal injury due to shearing force (traction injury) causing jejunal tear near duodenojejunal junction.
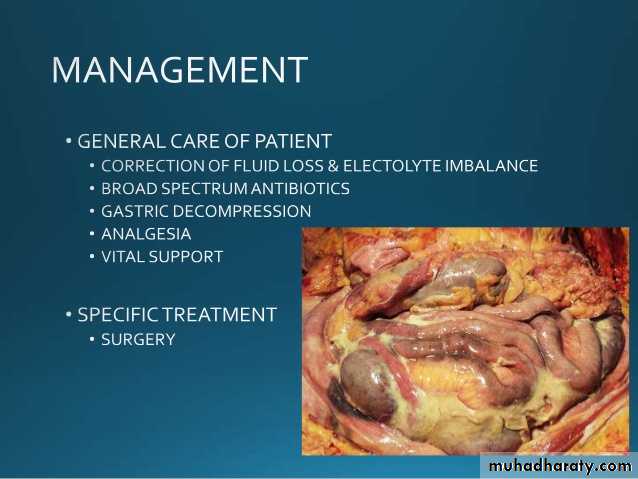
a case of peritonitis, where the peritoneal cavity is filled with pus.
Duodenal ulcer perforation causing peritonitis.
PRIMARY PERITONITIS
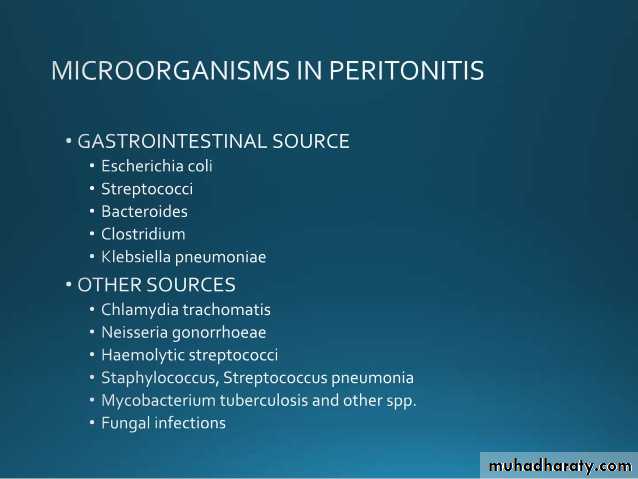
(Monomicrobial, extraperitoneal source, blood spread)
*It is commonly due to pneumococci, and can occasionally be due to streptococci, haemophilus, gonococcus (rare now) and other gram-negative (Escherichia coli) organisms.*It is common in young girls between 3-9 years of age group and
also in women.
*Here there is no documented source of infection.
Infection usually spreads from
lower genitals through fallopian tubes,
from upper respiratory tract infection or
from middle ear in males.
*It is uncommon after 10 years of age.
It is common in malnourished child and child with nephritis. Child is toxic, severely ill and develops septicaemia very early .
It is also seen in ascites,
patient with indwelling catheter for peritoneal dialysis,patients with peritoneovenous shunt.
It can also be due to Chlamydial, fungal or mycobacterial
infection.TC is very high, > 30,000/mm3.
Treatment
Diagnostic tapping, tube peritoneal drainage and laparoscopic
drainage and wash are useful methods.
Laparotomy and peritoneal toilet.
Broad spectrum antibiotics including combination of aminoglycosides, cephalosporins and metronidazole.
Local instillation of antibiotics, into the peritoneal cavity to achieve quick and effective results.
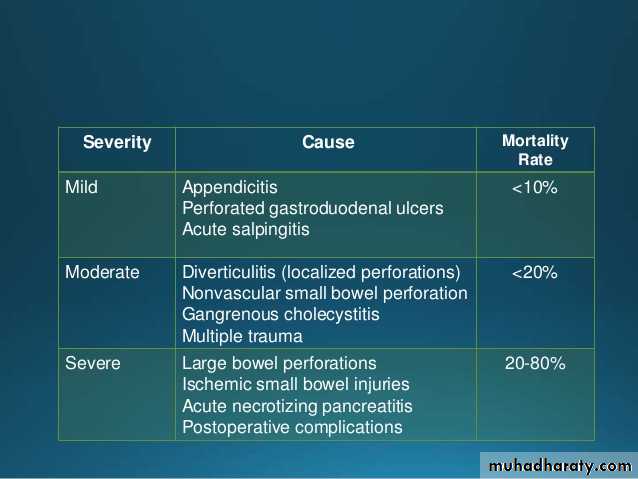
Mortality is high.
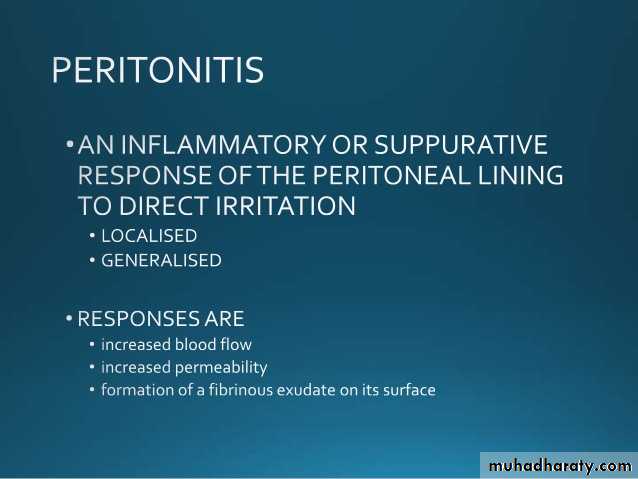
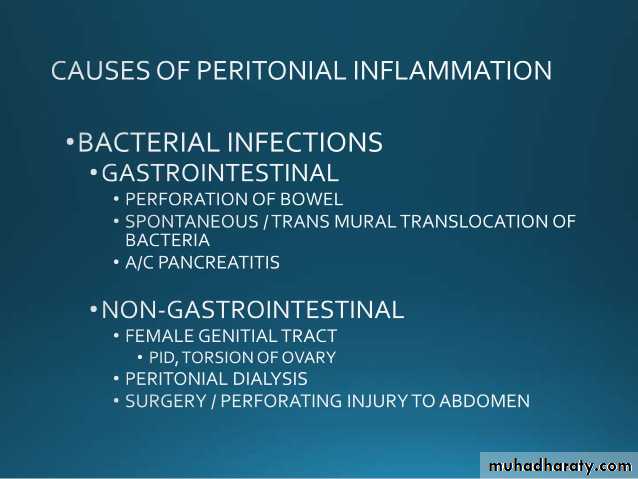
SECONDARY PERITONITIS
(Most common, polymicrobial, intraperitoneal source)
It is secondary to any bowel or other visceral pathology, e.g.
perforation, appendicitis.Escherichia coli (70%) is the most common organism involved. Other bacteria are—aerobic and anaerobic streptococci, Clostridium welchii, bacteroides, staphylococci, Klebsiella, Salmonella typhi.
TERTIARY PERITONITIS
(Due to superadded infection peritonitis following treatment of secondary/primary)*It occurs after any abdominal surgeries, which is usually severe and the patient may go in for SIRS or MODS early.
*Tertiary peritonitis is defined as persistent or recurrent intraabdominal infection after an adequate treatment for primary or secondary peritonitis—usually after 48 hours.
*It is common in immunosuppressed individual with ineffective
peritoneal host defenses against microbes.*Infection due to E. faecalis, E. faecium, S. epidermidis, P. aeruginosa,
C. albicans are common in such patients.*Virulence and resistance to drugs are other factors.
*It is difficult to diagnose clinically causing delay in therapy.*CT abdomen, total and platelet count, LFT, monitoring of renal functions, hourly urine output assessment, chest X-ray are required investigations.
Treatment
is aggressive antibiotic therapy, antifungal therapy, TPN, maintaining of haemodynamic stability, exploration of abdomen, thorough wash, colostomy/ileostomy or exteriorisation of bowel segment.
FFP, packed cells, platelet transfusions may be required. Ventilator, ICU care is often needed.
Mortality rate is > 50%.
Problems are—DIC, septicaemia, uraemia (haemodialysis may be needed), haemorrhage, pneumonia, ARDS.
Severe peritonitis showing pus in the peritoneal cavity.
PERITONEAL TUBERCULOSIS
Post-primaryBecoming more common
Activation of long-standing latent focus
Blood spread
Can develop from diseased mesenteric lymph node, intestine or fallopian tubes
Pathology in Peritoneal Tuberculosis
* Enormous thickening of the parietal peritoneum with
multiple tiny yellowish tubercles.* Dense adhesions in peritoneum and omentum with content
inside as small bowel looking like abdominal cocoon.It may precipitate intestinal obstruction.
*Multiple dense adhesions between bowel loops and between bowel and peritoneum and omentum.
*Thickening of bowel wall with adhesions.
Types1. Acute Type—Mimics Acute Abdomen
Acute peritoneal tuberculosis
*Rare*On-table diagnosis
*Features of peritonitis
*Due to perforation or rupture of mesenteric tuberculous
lymph nodes
Acute peritoneal tuberculosis
Exploratory laparotomy reveals straw-coloured fluid with
tubercles in the peritoneum, greater omentum and bowel wall. It is an on-table diagnosis. Fluid is evacuated and collected for AFB study and culture. Omental biopsy is taken. Abdomen is closed (without a drain) with tension sutures to prevent burst abdomen. ATD is started.
On-table findings in intestinal tuberculosis, of extensive involvement with multiple tiny tubercles, thickening , adhesions and involvement of mesenteric lymph nodes.
2. Chronic Tuberculous Peritonitis
Present as abdominal pain, fever, ascites, loss of weight and appetite, abdominal mass, doughy abdomen (10%).Peritoneum is thickened with multiple tubercles. Omentum is thick, fibrosed, rolled up.
Infection is usually from mesenteric lymph nodes, ileocaecal tuberculosis, from fallopian tubes, rarely blood born (from lungs).Laparoscopy is very useful in this type to diagnose
Ascitic formAscitic form shows enormous distension of abdomen with
dilated veins.It presents with congenital hydrocele in male with patent
processus vaginalis, umbilical hernia, rolled up omentum,
shifting dullness, fluid thrill, and mass abdomen.
Ascitic tap reveals straw coloured fluid from which AFB can
be isolated. Fluid is pale yellow, clear, rich in lymphocytes,with high specific gravity.
US picture showing ascites. Straw coloured ascitic fluid tapping done under US guidance.
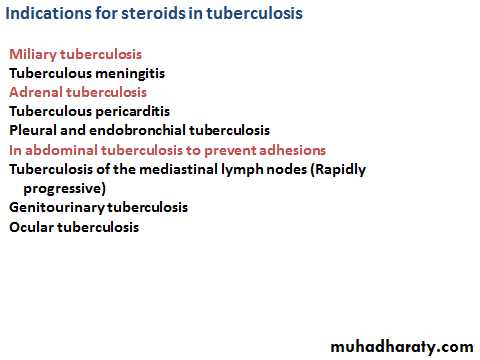
Chest X-ray, Mantoux test are other required investigations.ATDs for one year is required.
Repeat tapping may be required initially as part of the treatment.Encysted (Loculated) ascites
Ascites gets loculated because of the fibrinous deposition.Dullness, which is not shifting, is the typical feature.
They may present as intra-abdominal mass, which may
mimic ovarian cyst, retroperitoneal cyst or mesenteric cyst.
Treatment is U/S guided aspiration along with ATD‘s.
Laparoscopic picture of loculated ascites due to abdominal tuberculosis. Fluid is getting aspirated using a needle under laparoscopic vision.
Plastic type
Here there are wide spread adhesions between the coils ofthe intestine (ileum commonly), abdominal wall, omentum,
with distension of the small bowel, leading to blind loop,
ileus, intestinal obstruction (subacute, acute), thickened
parietal peritoneum.
They get recurrent colicky abdominal pain, diarrhoea,
wasting, and loss of weight, mass abdomen, and doughyabdomen.
Laparoscopy showing plastic type of abdominal tuberculosis and multiple tubercles over parietal and visceral surface of the peritoneum.
Purulent form
It is invariably due to tuberculous salpingitis, presentingas a mass in the lower abdomen containing pus, omentum,
fallopian tubes, small and large bowel.
Cold abscess gets adherent to the abdominal wall, umbilicus
and may form an umbilical fistula.
Patient commonly has got genitourinary tuberculosis.
U/S, discharge study, X-ray abdomen and other investigations
are useful.Treatment: ATD’s are started exploration of umbilicus,
exploration of fistula and bowel by pass is done.
Prognosis is poor in this type.
TUBERCULOUS MESENTERIC
LYMPHADENITISInfection is usually through the Peyer‘s patches of the intestine
(i.e. through oral cavity). Usually several lymph nodes
are involved often causing massive lymph node enlargement.
Commonly right-sided lymph nodes are involved, but
left sided nodes can also get involved.
It presents with general symptoms (fever, malaise, weight loss).
It may present with features of acute appendicitis.
Mesenteric tuberculous lymphadenitis on table findings
Often coils of intestine get adherent to the caseated mesenteric lymph nodes leading to intestinal obstruction.
Most often caseating material may collect between the
layers of the mesentery, forming a cold abscess, mimickinga mesenteric cyst (Pseudomesenteric cyst).
Massive enlargement of mesenteric lymph nodes due to
tuberculosis is called as tabes mesenterica.Mesenteric tuberculous adenitis is more common in children.
Present with anaemia, fever, loss of appetite and reduced weight, failure to thrive, palpable mass in right iliac fossa which is firm and nodular.Note the location of mesenteric tuberculous lymphadenitis in the rigth iliac fossa. But it can occur anywhere in the line of mesentery.
On-table caseating tuberculosis lymphadenitis is also shown.
Presentations of mesenteric tuberculous lymphadenitis
Mesenteric tuberculous adenitis—acute/chronic in right iliacfossa—mass
Pseudomesenteric cyst
Cold abscess within the mesentery
Tabes mesenterica
Differential Diagnosis
Carcinoma caecum.
Lymphoma.
Retroperitoneal tumour.
Nonspecific lymphadenitis.
(Acute nonspecific mesenteric lymphadenitis is called as
nurses’ syndrome).
Investigations
X-ray abdomen shows calcification.U/S may confirm the diagnosis.
Mantoux test may be positive.
Diagnostic laparoscopy—is very useful in TB lymphadenitis.
Mesenteric cold abscess can be drained safely
through laparoscopy.