
Page 1 of 8
Internal medicine lec.13 Respiratory Dr.Majeed
Objectives
To know the following.ARDS. Occupational and Environmental lung disease
Epidemiology
Etiology
Pathogenesis
Clinical presentation
Diagnosis
Treatment
Complication and prognosis
Acute respiratory distress syndrome (ARDS)
• This describes the acute, diffuse pulmonary inflammatory response to either direct (via airway
or chest trauma) or indirect (blood-borne) insults that originate from extrapulmonary pathology
The criteria defining ARDS are:
• Hypoxaemia.
• chest X-ray showing diffuse bilateral infiltrates .
• Absence of a raised left atrial pressure.
• Impaired lung compliance
Berlin definition of ARDS
• Onset within 1 week.
• Respiratory failure not fully explained by cardiac failure or fluid overload.
▪ Objective assessment (e.g. by echocardiography)
•Severity according to Impaired oxygenation:
Mild
Moderate:
Severe:

Page 2 of 8
It is characterised by:
• neutrophil sequestration in pulmonary capillaries
• increased capillary permeability
• protein-rich pulmonary oedema with hyaline membrane formation
• damage to type 2 pneumocytes leading to surfactant depletion
• alveolar collapse
• reduction in lung compliance
• If the early phase does not resolve with treatment of the underlying cause.
• Late : fibroproliferative phase ensues and causes progressive pulmonary fibrosis.
• It is frequently associated with other organ dysfunction as part of MOF.
Conditions predisposing to ARDS
• Inhalation (direct)
• Aspiration of gastric contents
• Toxic gases/burn injury
• Pneumonia
• Blunt chest trauma
• Near-drowning
Blood-borne (indirect)
• Sepsis
• Necrotic tissue (particularly bowel)
• Multiple trauma
• Pancreatitis
• Cardiopulmonary bypass
• Severe burns
• Drugs (heroin, barbiturates, thiazides)
Page 3 of 8
• Major transfusion reaction
• Anaphylaxis (wasp or bee stings, snake venom)
• Fat embolism
• Carcinomatosis
• Obstetric crises (amniotic fluid embolus, eclampsia)
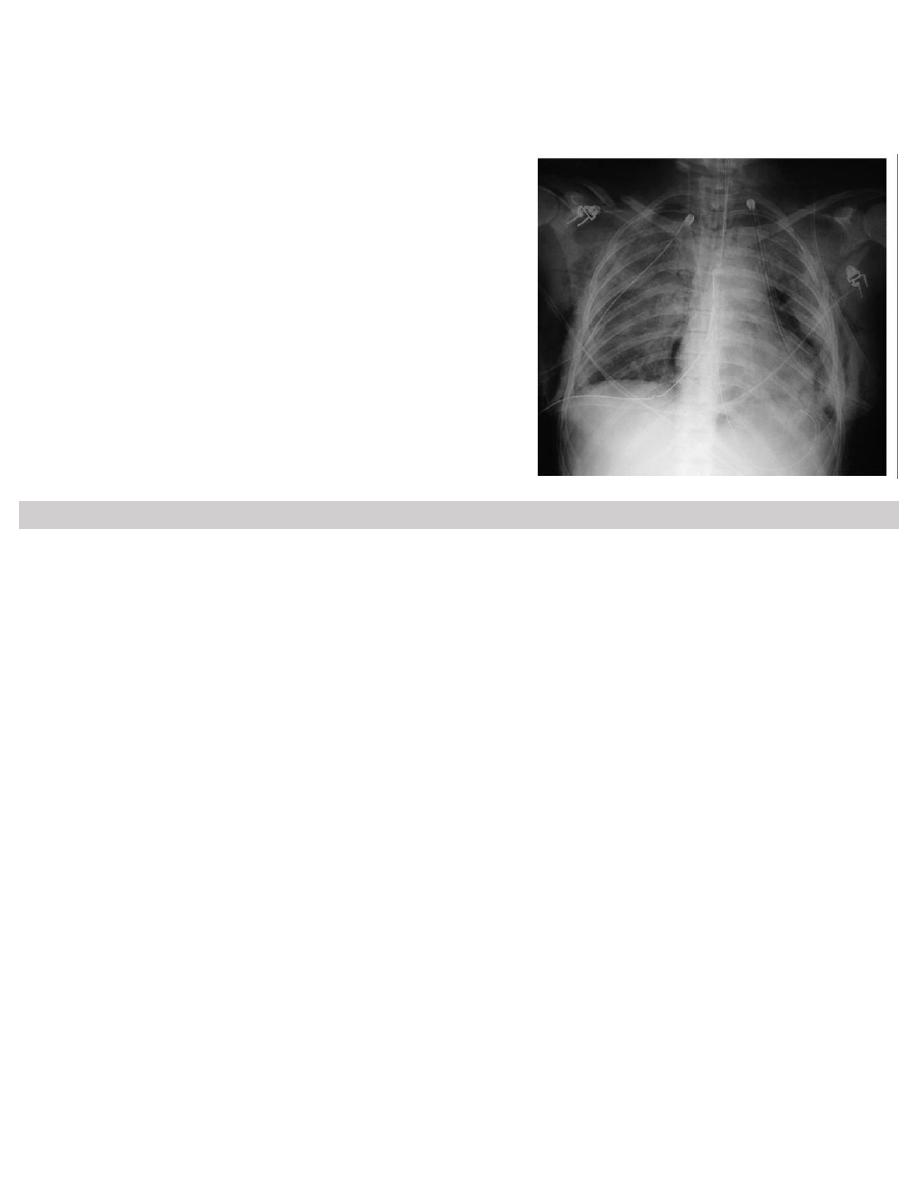
Chest X-ray in acute respiratory distress syndrome
(ARDS). Note bilateral lung infiltrates,
pneumomediastinum,
pneumothoraces with bilateral chest drains, surgical
emphysema, and
fractures of the ribs, right clavicle and left scapula
Occupational and environmental lung disease
I--Occupational airway disease
Occupational asthma . Chronic obstructive pulmonary disease. Byssinosis. Reactive airways
dysfunction syndrome
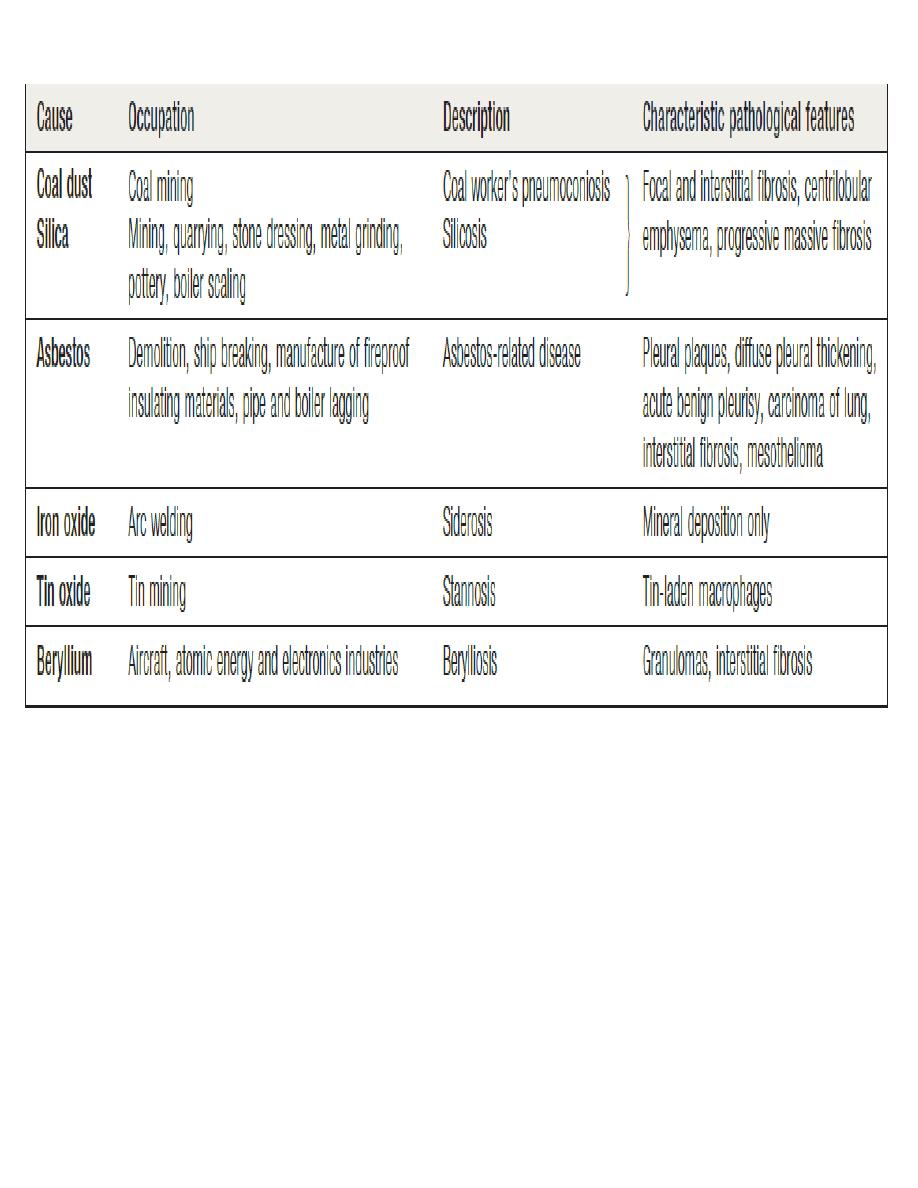
II-Pneumoconiosis
Coal worker’s pneumoconiosis. Silicosis. Berylliosis. Less common pneumoconioses
III-Lung diseases due to organic dusts
Hypersensitivity pneumonitis. Inhalation (‘humidifier’) fever
IV-Asbestos-related lung and pleural diseases
V-Occupational lung cancer.
VI-Occupational pneumonia
OCCUPATIONAL LUNG DISEASE
Exposure to dusts, gases, vapours and fumes at work can lead to the following
types of lung disease:
1. Acute bronchitis and pulmonary oedema from irritants such as Sulphur dioxide, chlorine,
ammonia or oxides of nitrogen
2 . Pulmonary fibrosis from inhalation of inorganic dust, e.g. coal, silica, asbestos, iron and tin
Page 4 of 8
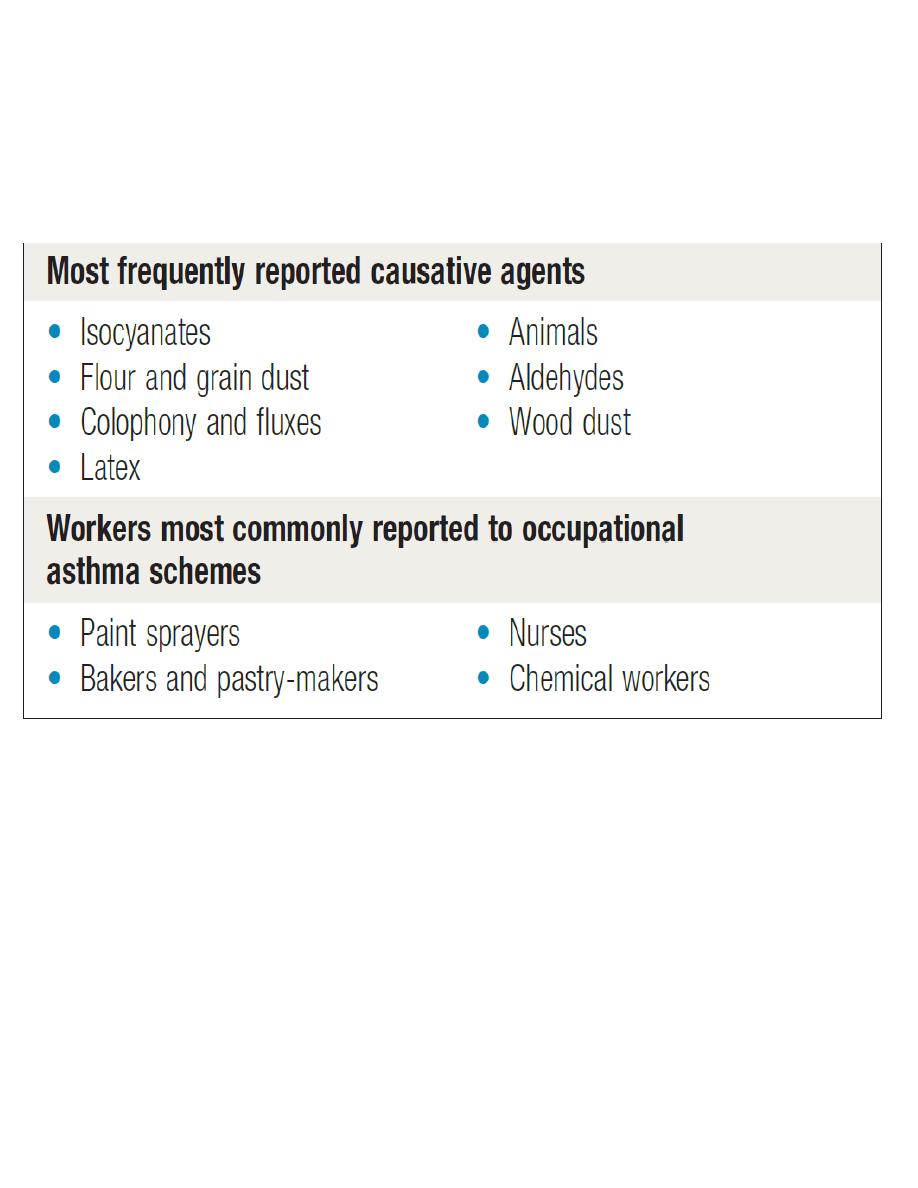
3. Occupational asthma – this is the commonest industrial lung disease in the developed world
4. Hypersensitivity pneumonitis
5 . Bronchial carcinoma due to asbestos, polycyclic hydrocarbons and rado in mines.
Occupational ASTHMA
• Byssinosis occurs in workers of cotton and flax mills exposed to cotton brack (dried leaf and
plant debris)
• Reactive airways dysfunction syndrome or acute irritant-induced asthma refers to the
development of a persistent asthma-like syndrome following the inhalation of an airway
irritant:
II-Pneumoconiosis
Coal worker’s pneumoconiosis:
Cause: prolonged inhalation of coal dust causing pulmonary fibrosis through aggregation of alveolar
macrophages.
• Classification:
• A/ Simple CWP: asymptomatic.
• B/ Progressive massive fibrosis:
Page 5 of 8
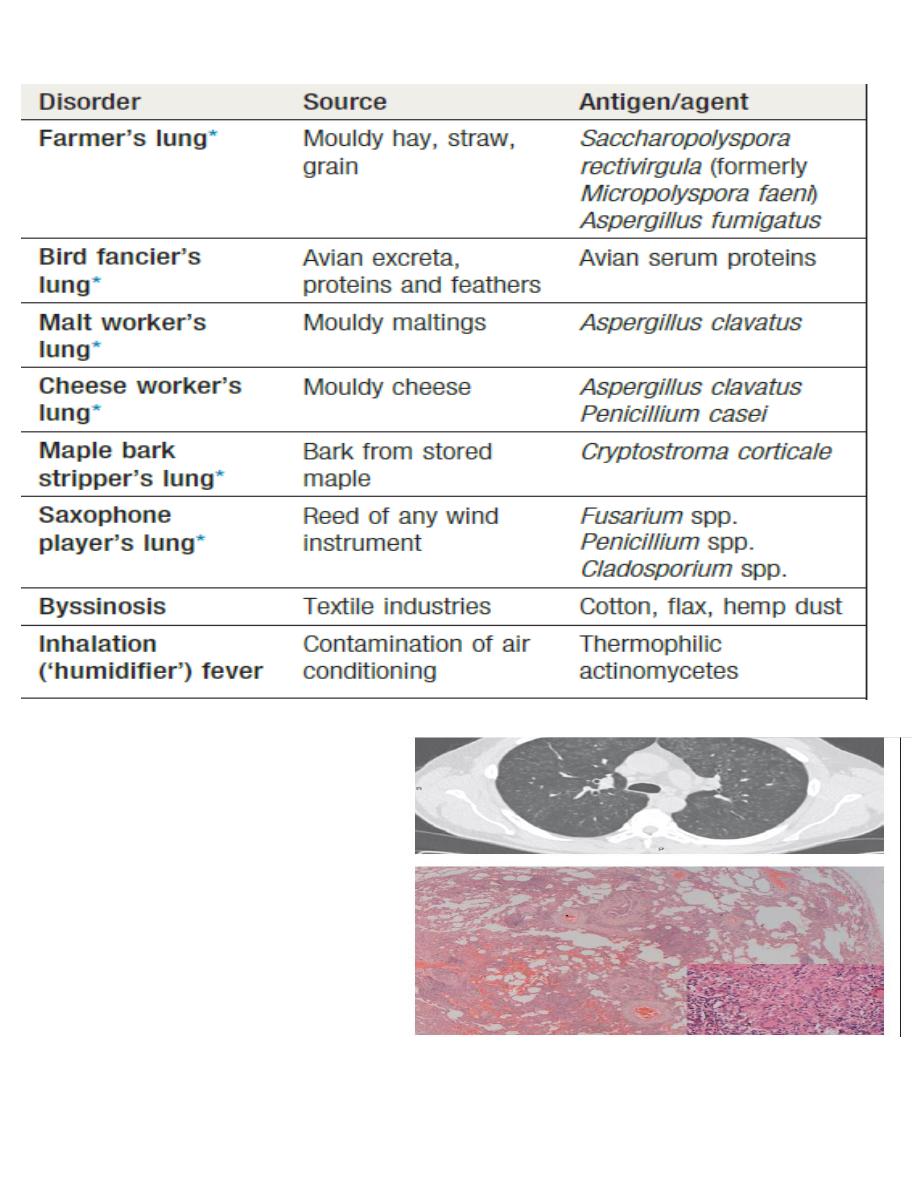
III--Lung diseases due to organic dusts:
• A wide range of organic agents may cause respiratory disorders .
• inhalation of organic dust leading to type III or IV diffuse immune complex reaction with in the
alveolar & bronchial walls.
Hypersensitivity pneumonitis (extrinsic allergic alveolitis)
❑ farmers (farmer’s lung)
❑ pigeon fanciers (bird fancier’s lung) with symptoms related to the extent of exposure to the
triggering organic dusts.
• Symptoms either acute as influenza-like syndrome or chronic with progressive pulmonary
fibrosis.
Page 6 of 8
Hypersensitivity pneumonitis
Clinical predictors:
Exposure to a known offending antigen
• Positive precipitating antibodies to
offending antigen
• Recurrent episodes of symptoms
• Inspiratory crackles on examination
• Symptoms occurring 4–8 hours after
exposure
• Weight loss

Page 7 of 8
Investigations:
CXR-
HRCT-.
Pulmonary function test- restrictive defect,
Serology-.
Management:
1. Avoid exposure to possible triggers.
2. Wearing masks.
3. Glucocorticoids.
4. O2 therapy.
Complications:
❑ Pulmonary fibrosis,
❑ respiratory failure,
❑ pulmonary hypertension
❑ right side heart failure.
Case-studies
CASE NO 1
A 65-year-old man presents with progressive shortness-of-breath. On examination he is found to have
fine crackles in both lung bases and oxygen saturations of 93% on room air.
Case 2
A diagnosis of idiopathic pulmonary fibrosis is suspected. Which one of the following chest x-ray
findings develops first in patients with idiopathic pulmonary fibrosis?
A/ Asymmetrical upper zone 'ground-glass' changes
B/ Small, peripheral opacities in the lower zones
C/ Perihilar horizontal septal lines
D/ Honeycombing
E/ Loss of left heart border
CASE 3
Page 8 of 8
On examination, he is comfortable at rest with oxygen saturations 95% on air. There is no evidence
of lymphadenopathy, clubbing or cyanosis. He has fine crackles at both lung bases that do not alter
on coughing.
Which of the following investigation findings would support a diagnosis of idiopathic pulmonary
fibrosis?
A/ Reticular changes on CT imaging that is worse at the bases
B/ Obstructive picture on spirometry
C/ Extensive ground glass opacities on CT imaging
D/ Increased transfer factor on spirometry
E/ A lymphocytosis on bronchoalveolar lavage
CASE 4
A 68-year-old male patient presents with a 6-month history of shortness of breath that is worse on
exertion with reduced exercise tolerance & no associated wheeze, or haemoptysis but does have a dry
cough.
He has hypertension and takes amlodipine 5mg once a day. He has never smoked or worked with
asbestos
