• Insulin Therapy
Adel Gassab MohammedMD. CABMS. MSc of Medicine Specialist Endocrinologist,
College of medicine
ORCID iD: https://orcid.org/0000-0001-9084-1038.
Email: adelgassab@utq.edu.iq
• What is Insulin?
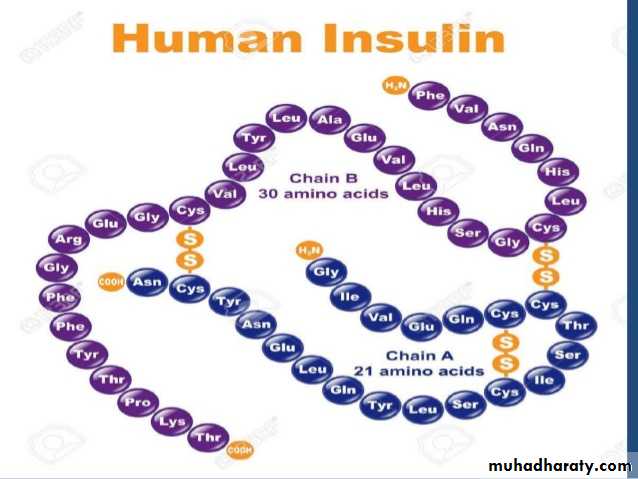
• 2 chains• 2 bonds
• Secreted as basal & meal related (2)
• Meal related in 2 phases
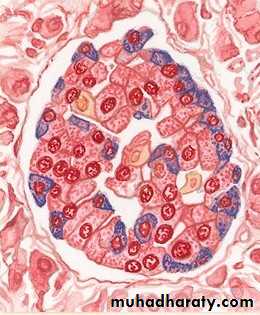
Insulin is a peptide hormone produced by beta cells of the pancreatic islets; it is considered to be the main anabolic hormone of the body.
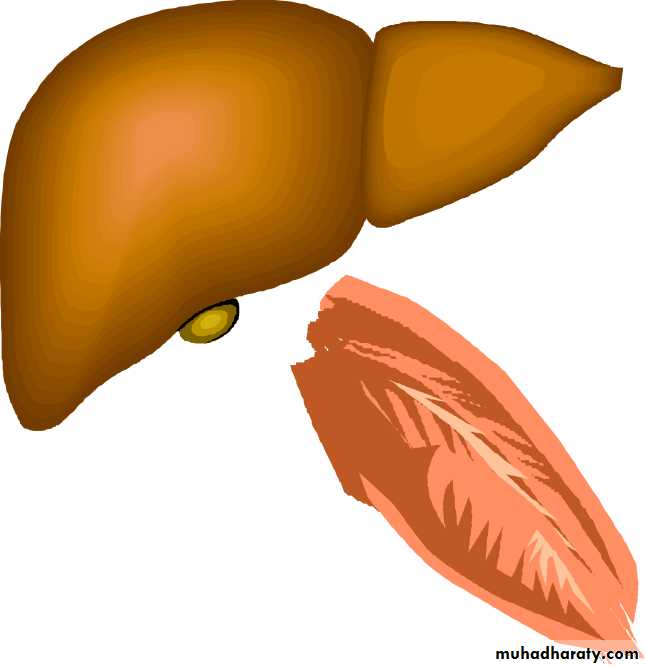
It regulates the metabolism of carbohydrates, fats and protein by promoting the absorption of glucose from the blood into liver, fat and skeletal muscle cells.
• What is Insulin?
• Insulin deficiency results in
• Elevated plasma glucose - hyperglycemia
• Elevated plasma lipid - hypertriglyceridemia
• Altered protein metabolism - Metabolic & Immune defects
• Insulin replacement in diabetes tends to restore normalcy
Time of day
6:000
10
20
30
40
50
60
70
10:00
14:00
18:00
Insulin (µU/ml)
Low, steady, basal
insulin profile
Short-lived, rapidly
generated meal-related
insulin peaks
22:00
2:00
6:00
Normal insulin secretion
Polonsky KS et al. J Clin Invest 1988;81:442–8
Actions of Insulin
• Integrated action on carbohydrate, protein and fat metabolism
• Dominant effect on glucose homoeostasis predominantly exerted in 3 tissues
• Liver
• Skeletal muscle
• Fat
• Actions of Insulin
• In Liver• Inhibition of glycogenolysis & gluconeogenesis
• Stimulation of glycogenesis & storage
• In skeletal muscle & adipocytes
• Stimulation of glucose uptake, utilization & storage
• Increases glucose transport
• Activation/inactivation of enzymes responsible for storage & metabolism of glucose
Insulin:
The Definitive Therapy for Diabetes• DM
• Impaired insulin secretion (insulin deficiency)
• Impaired insulin action (insulin resistance)
• Insulin can overcome both the defects
• Hence: Insulin-the definitive therapy for all types of diabetes
• valuable
• tool for early
• Insulin- a intervention, to
• therapeutic
• attain and maintain target levels of
• blood glucose control.
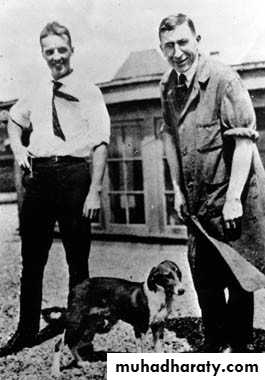
• The discovery of insulin
• 1921 : Isletin isolated• 1922 :
• 1st human experiment• 1923:
• Name changed to “Insulin”• Insula (latin) = island
• Banting & Best
• Discovery of Insulin
• •• •
• 1st patient to receive pancreatic extract (insulin)-14-yr old Leonard Thompson.• 1st attempt (11th Jan 1922)- failed but the 2nd attempt (3rd May 1922) succeeded in reducing urine glucose excretion.
• First patient to benefit from insulin
• –saved from death• Leonard Thompsom-1908-1935
• Grew cheerful, started eating more, gained weight, & cheeks started swelling out
Insulin Structure
Insulin is composed of two peptide chains referred to as the A chain and B chain. A and B chains are linked together by two disulfide bonds, and an additional disulfide is formed within the A chain. In most species, the A chain consists of 21 amino acids and the B chain of 30 amino acids.• Type 1 diabetes
• Pregnant Women with diabetes or gestational diabetes• In type 2 diabetes, inadequately controlled on OADs
• type 2 diabetes in special situations-
– Pancreatitis
– DKA
– during surgery
– acute infections
-Significant symptomatic hyperglycemia (random ≥ 300 mg) or A1c ≥ 10
- In-hospital
Indication of insulin therapy
• Types of Insulin
• 1 .Rapid-acting• 2 .Short-acting
• 3. Intermediate-acting
• 4 .Premixed
• 5 .Long-acting
• (Analogs) (Regular)
• (NPH)
• (70/30)
• (Lantus)
• Types of Insulin
• Basal insulin• Meal insulin
• Basal insulin• Intermediate –acting:
• NPH (Humulin N®, Insulatard® )
• Long-acting:
• Glargine U-100 (Lantus®)
• Glargine U-300 (Toujeo®)
• Glargine biosimilar (Basaglar ®) Detemir (Levemir ®)
• Degludec (Tresiba®)
• Meal Insulin
• Short-acting:
• Regular (Actrapid®, Humulin R®, Novolin R®)
• Rapid-acting: (analogs)
• Lispro (Humalog®)
• Aspart (Novorapid®, Novolog®)
• Glulisine (Apidra®)
All look clear (like water)
Inhaled insulin
Exubera, developed by Inhale Therapeutics (later named Nektar Therapeutics), became the first inhaled insulin product to be marketed, in 2006 by Pfizer, but poor sales led Pfizer to withdraw it in 2007.Afrezza, a monomeric inhaled insulin developed by Mannkind, was approved by the FDA in 2014
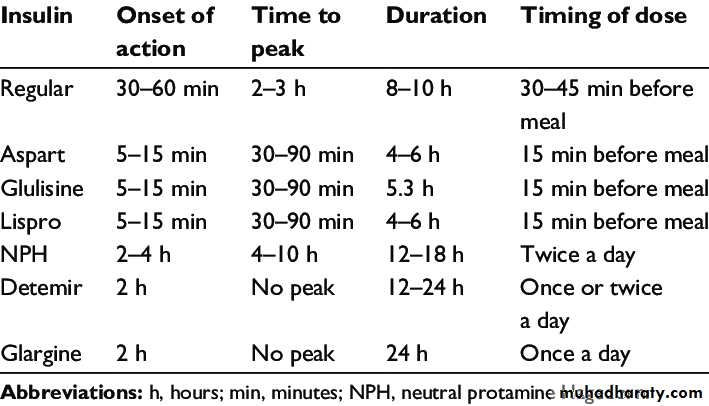
PHARMACOKINETICS OF INSULIN PREPARATIONS
INSULIN REGIEMEN
The choice of regimen depends on• the desired degree of glycemic control,
• the severity of underlying insulin deficiency,
• the patient’s lifestyle, and his or her ability to adjust the insulin dose.
• The time–action profile of different insulin regimens, compared to the secretory pattern of insulin in the non-diabetic state
Once-daily regimen
• Long-acting or intermediate-acting insulin is given at bedtime.
• It is suitable only for patients with type 2 diabetes and may be used in combination with oral hypoglycemic agents.
• This regimen may be used when starting insulin in type 2 diabetes and when there is dependence on others to give injections.
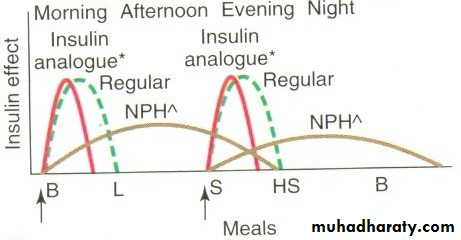
• Intermediate acting insulin(NPH)and short acting (regular) insulin
• 2/3 of insulin – morning (ratio 1:2)• 1/3 of insulin - evening
Two daily regimens
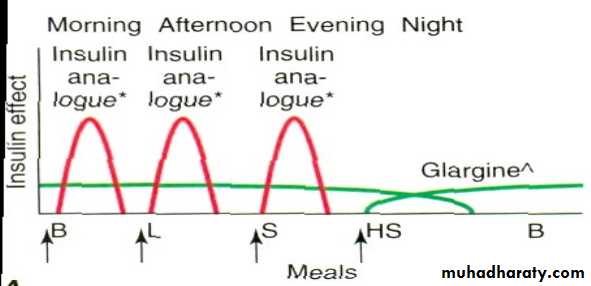
• Basal bolus insulin therapy• Short acting- before meal
• Intermediate or long acting –once or twice daily
• Advantage:-
• allows greater freedom with regard to meal timing
• .
• More variable day to day physical activity
• Insulin vials
• “U-100 “ = every 1 ml has 100 units• 1 vial has 10 ml = 1000 units
• New bottles should be kept in refrigerator [2-8 C°) [not freezer] until expiration date
• Opened vials are valid for 4 weeks
• Opened vials can be kept in refrigerator or in room temperature (15-25 C°)
• Care of insulin vials
• •• •
• •
• •
• •
• •
• Do not keep in hot places.
• Do not keep in a freezer.
• Do not leave in sunlight.
• Never use insulin if expired.
• Write the date on the insulin vial on the day you open it or start keeping it outside the fridge.
• Throw the insulin away 4 weeks after opened or since kept out of the fridge.
• Inspect your insulin before each use.
• Look for changes in color or clarity.
• Look for clumps, solid white particles or crystals in the bottle or pen.
• Insulin that is clear should always be clear and never look cloudy.
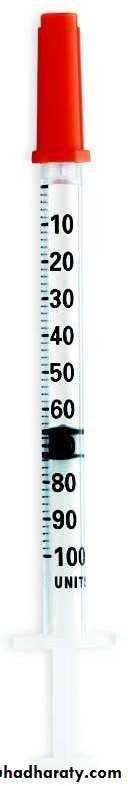
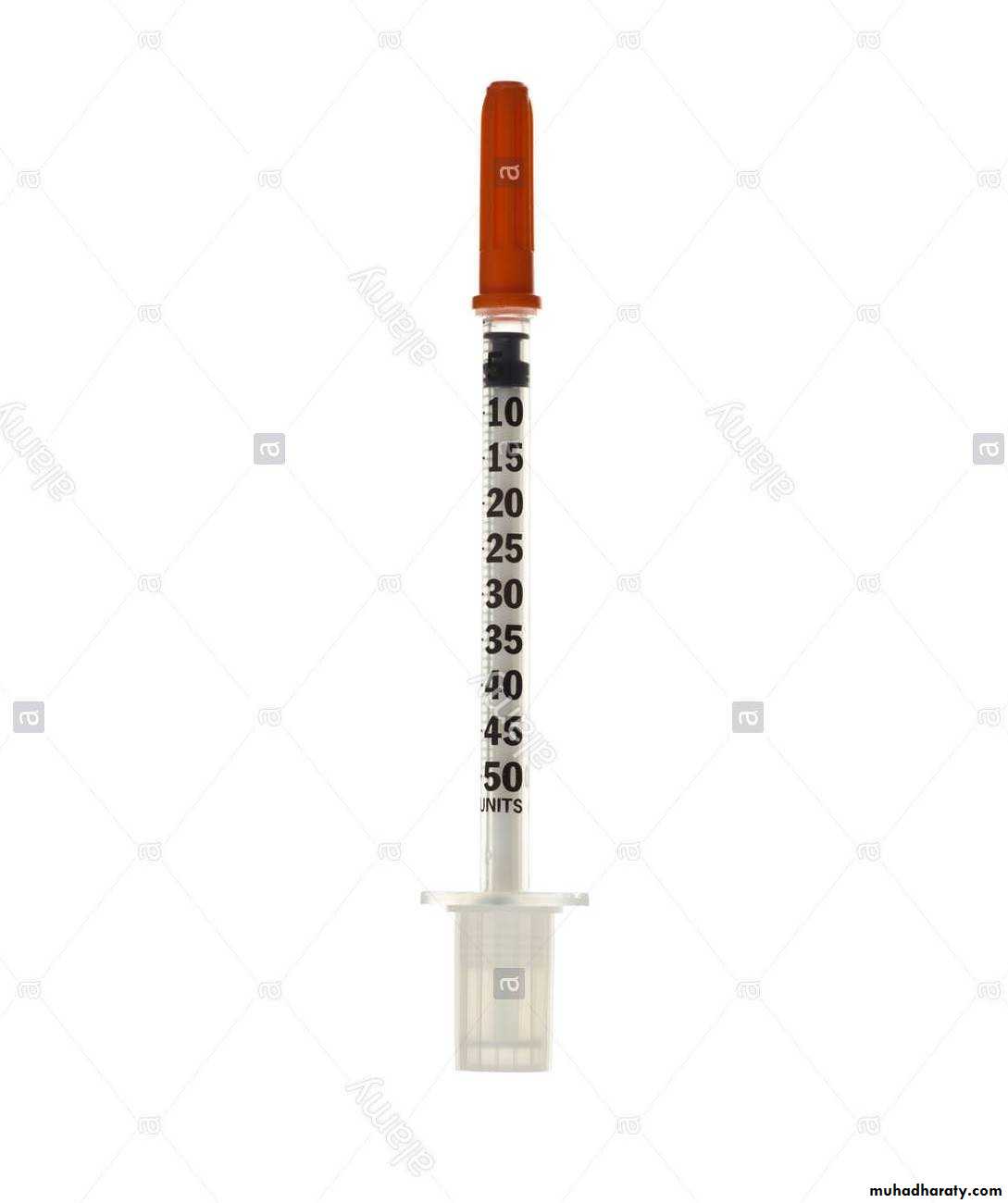
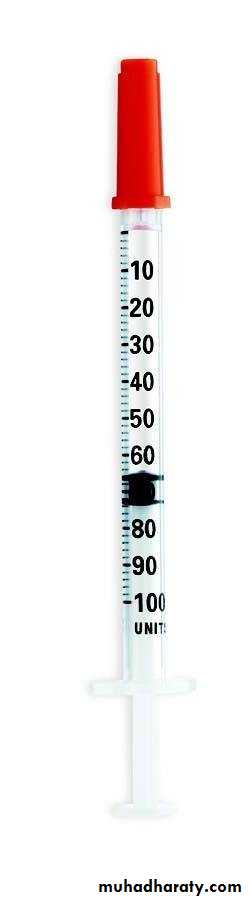
• Insulin syringes
•
• 50 units
• (0.5 ml)• 100 units
• (1 ml)
• 50-units insulin syringe
• Lines arranged in order of 5 (5, 10, 15,….)
• Every line equals one unit of insulin• Example: when injecting 12 units, you draw TWO lines after line 10
• 10
• 15
• 100-units insulin syringe
• lines arranged in order of 10 (10, 20, 30….)• Every line equals two units of insulin
• Example: when injecting 12 units, you draw ONE line after line 10
• 10
• 20
•
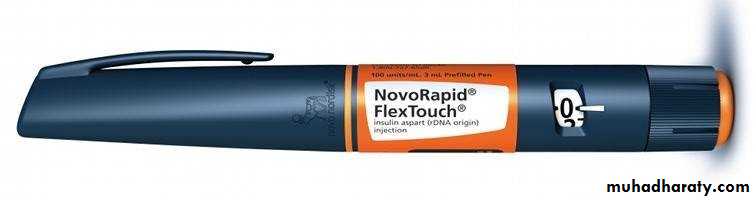
• •
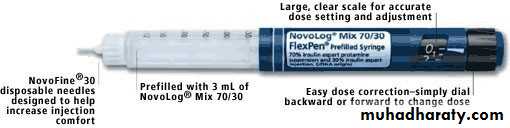
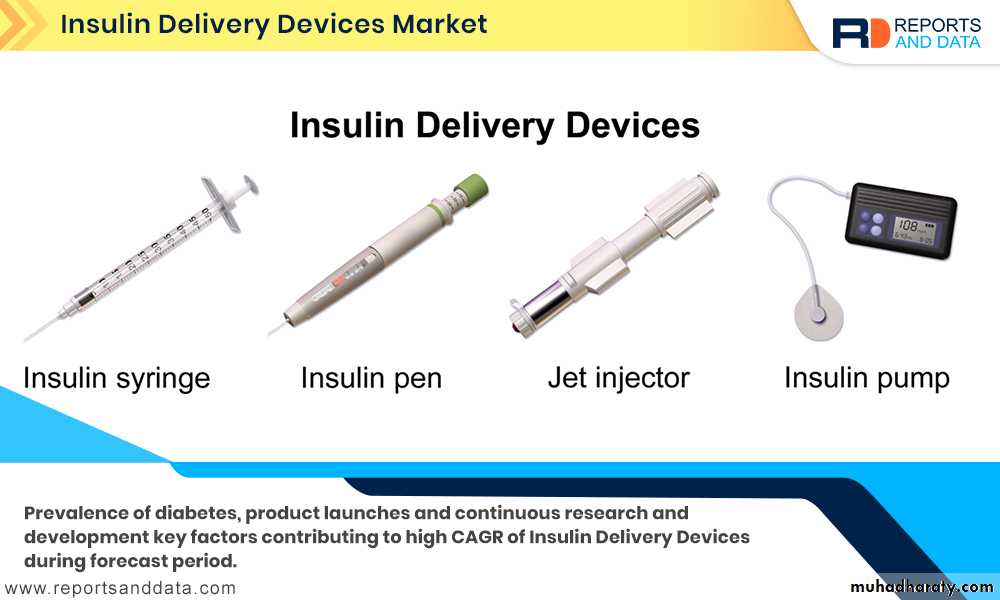
• •• There are 2 types of pens:
• Reusable (cartridges are changed)
• -Pen stays
• Disposable:
• - Whole pen is changed
• Keep new disposable pen or cartridges in refrigerator
• Once pen or cartridge is opened, keep
• in room temperature (validity depends on type)
• Insulin pens
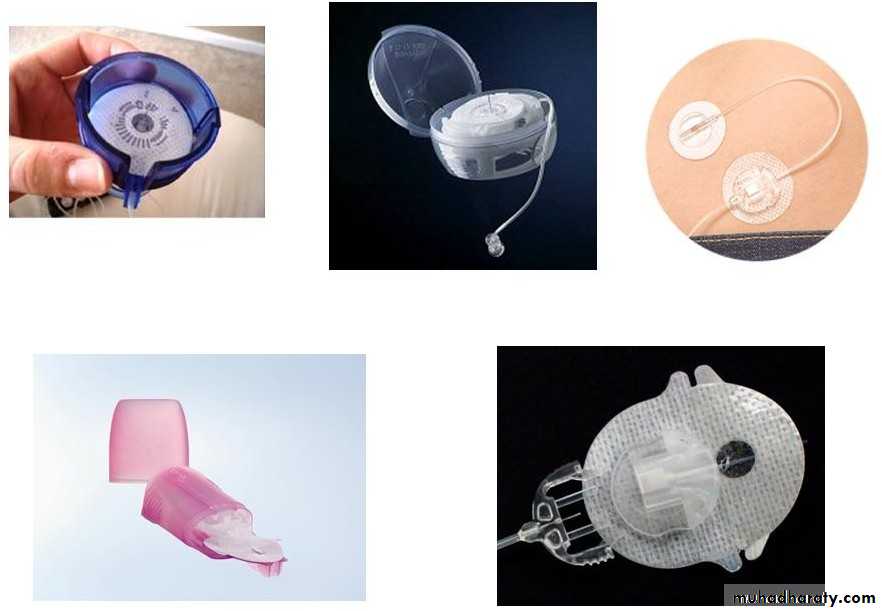
Insulin pumps(Continuous subcutaneous insulin infusion (CSII)
Insulin pumps are small, computerized devices that mimic the way the human pancreas works by delivering small doses of short acting insulin continuously (basal rate). The device also is used to deliver variable amounts of insulin when a meal is eaten (bolus).• Continuous subcutaneous insulin infusion (CSII)
• •• •
• •
• Very effective insulin regimen for type 1 DM Sophisticated device
• requires education of the patient and frequent interactions with diabetes management team
• Advantages:
• •
• –
• –
• –
• programmed dose
• basal infusion rates altered during exercise
• different doses of insulin can be matched based on meals
• •
• Disadvantages---
• infection
• hyperglycemia
• DKA
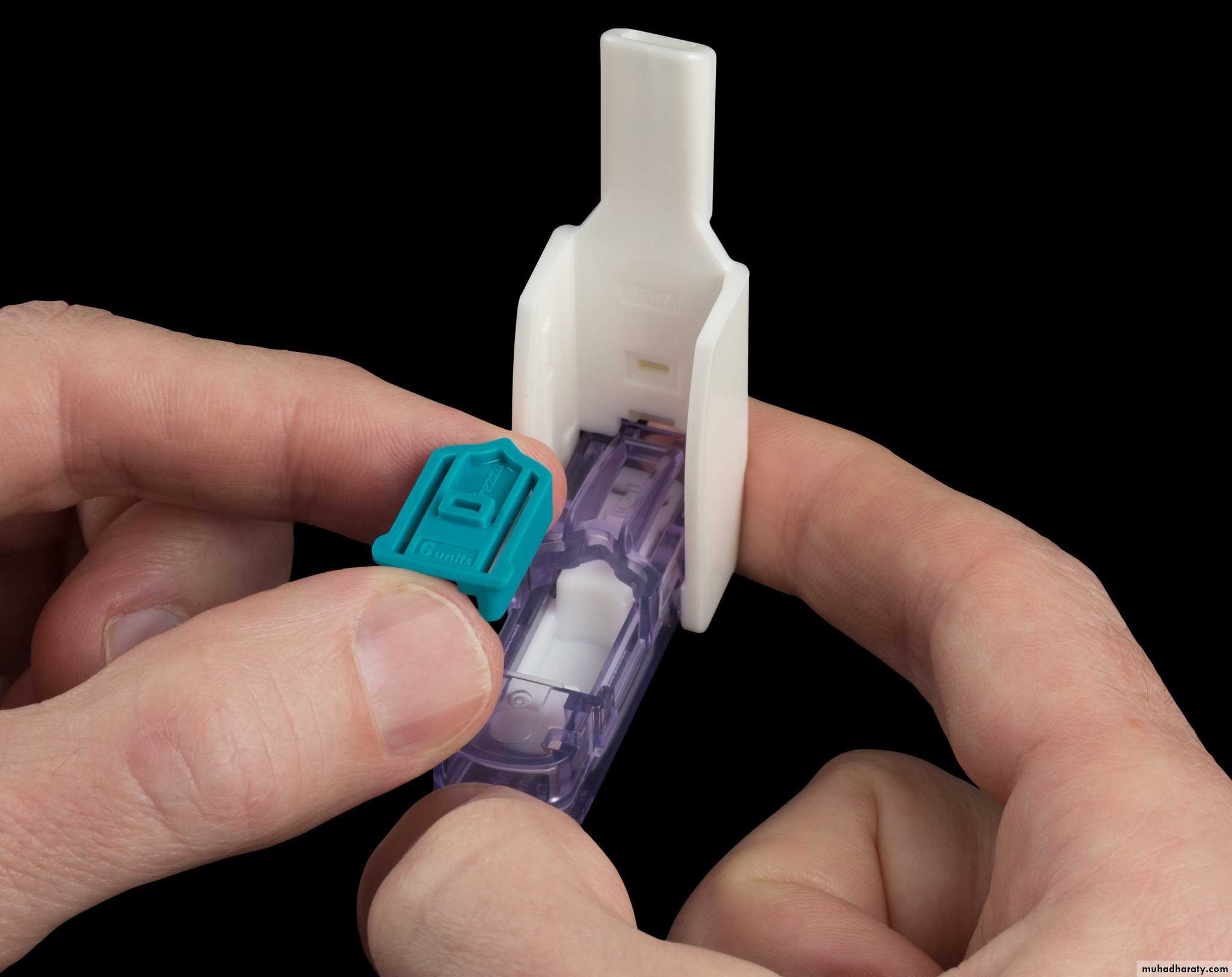
• CSII sets
• Insulin pen care
• Insulin pens must be stored at room temperature: Storing your insulin pen in extreme temperatures can lead to changes in the concentration of the pen's insulin.• Do not share your insulin pen with anyone: even if you are changing the needles. Infections (HBV, HIV) happened as insulin itself can be contaminated
• Do not withdraw insulin from the pen cartridge:
• can lead to inaccurate dose measurement the next time the insulin pen is used for dose delivery. The reason for this is related to air entering the pen unintentionally, interfering with the proper mechanics of the pen
• Insulin pen care
• Do not leave an open needle attached to an insulin pen
• It can lead to unintentional air entering into the insulin pen and ultimately improper dosing of insulin. It could also lead to insulin contamination.
• Proper insulin pen mixing:
• Every time you use a pen containing NPH or premixed mixtures . The insulin should look uniformly cloudy or milky after mixing. If there are clumps floating in the insulin, or white particles stuck to the bottom or sides of the pen giving it a frosted look, don't use it.
• How long is the opened pen or unopened pen outside the refrigerator valid for ?
• Aspart, Lispro, Glulisine: 4 weeks• NPH: 2 weeks
• Glargine: 4 weeks
• Detemir: 6 weeks
• Degludec: 8 weeks
• Aspart 70/30: 2 weeks
• Premixed 70/30, Lispro 75/25, Lispro 50/50: 10 days
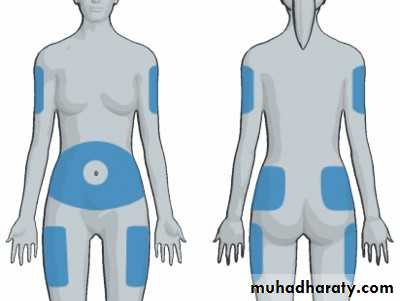
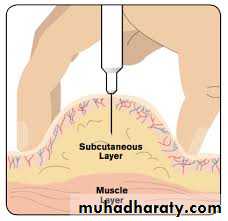
• Sites of Insulin Injection
• Abdomen, Arms ,Thighs• ** Rotate injection sites
• What time to give insulin?
• NPH:
• At bedtime
• Or usually twice/day (usually mixed with meal insulin)
• Glargine/Detemir:
• At bedtime (or AM)
• Some need twice daily
• Degludec:
• Once daily (at same time of the day)
• What time to give insulin?
• Regular:• 30 minutes before meals (once, twice or 3 times/day)
• Rapid-acting insulins:
• 5 minutes before meals (once, twice or 3 times/day)
• Can be given immediately after meals
• Starting dose of insulin
• T1DM: 0.5 to 1.0 unit per kg per day.• T2DM: 0.4 to 1.0 units/kg/day
• In split mixed regimen-
• 2/3 as intermediate
• acting & 1/3 as short- acting
• In basal bolus regimen: ½ basal at bed time and ½ bolus in 3 divided doses. Dosage is individualized and titrated soon
Why Early insulin initiation?
Clinical & Pharmacological Reasons(4)
Improves beta-cell function (reduces glucotoxicity & lipotoxicity)
• Improves Quality of Life
insulin• Beneficial effects on lipids
• Beneficial effects on lipids
• Insulin vials and syringes
• Inhalation device or insulin
Side effects of Insulin• 5 Side effects
• Hypoglycemia
• Allergic Reactions –
• Local redness, itching – self limiting, disappears with continuation of therapy
• Systemic allergy – angioedema, anaphylaxis; rare, requires desensitization
• 3 .Insulin lipoatrophy
• 4 .Insulin lipohypertrophy
• 5 .Insulin Edema & weight gain
• Barriers to insulin therapy
• Fear of hypoglycemia
• Inconvenient timing of injection
• Complicated regimen
• to be taken 30 minutes before meal
• lifestyle to fit therapy
• Hyperglycemia immediately after meal
• Hypoglycemia before next meal
• Fear of injection