z
Antiepileptic Drugs
Dr. Hussain adday aljabery
FICMS ( RAD. )
Pharmacology
z
Basic information
▪
Epilepsy, a chronic disease, occurs approximately 1% of the population. The cause of most
cases of epilepsy is unknown, although some people develop epilepsy as the result of
brain injury , stroke, brain tumor and drug toxicity. Genetic mutations are linked to a small
proportion of thee disease.
▪
Epileptic seizures result from excessive and abnormal cortical nerve c cell activity in the
brain.
▪
Thee diagnosis typically involves ruling out other conditions that cause similar neurological
symptoms. This may be confirmed by brain imaging and electroencephalogram ( (EEG) but
normal test does not exclude the condition.
▪
Antiepileptic drugs (AEDs ) are effective for about 80% of these patients. Lifelong
treatment may be necessary s.
▪
It may take weeks to establish adequate drug plasma levels and to determine the
adequacy of therapeutic improvement. Lack of compliance is responsible for many
treatment failures.
AED s are most effective and have the least e adverse effects
when they are used as monotherapy .
Addition or withdrawal of any drug should be gradual , because
seizures may occur on withdrawal.
Some AEDs are teratogenic this may call for the reduction or
termination of therapy during pregnancy .
z
Definitions
▪
Convulsion:
Sudden attack of involuntary muscular
contractions and relaxations.
▪
Seizure:
Abnormal central nervous system electrical activity.
▪
Epilepsy:
A group of recurrent disorders of cerebral function
characterized by both seizures and convulsions.
z
Background
▪
Epilepsy: Neurological disorder affecting the CNS.
▪
Approximately 2.5 million people in the U.S. (~1% general pop)
▪
Cost per patient ranges from $4,272 for persons with remission after
initial diagnosis and treatment to $138,602 for persons with intractable
and frequent seizures.
▪
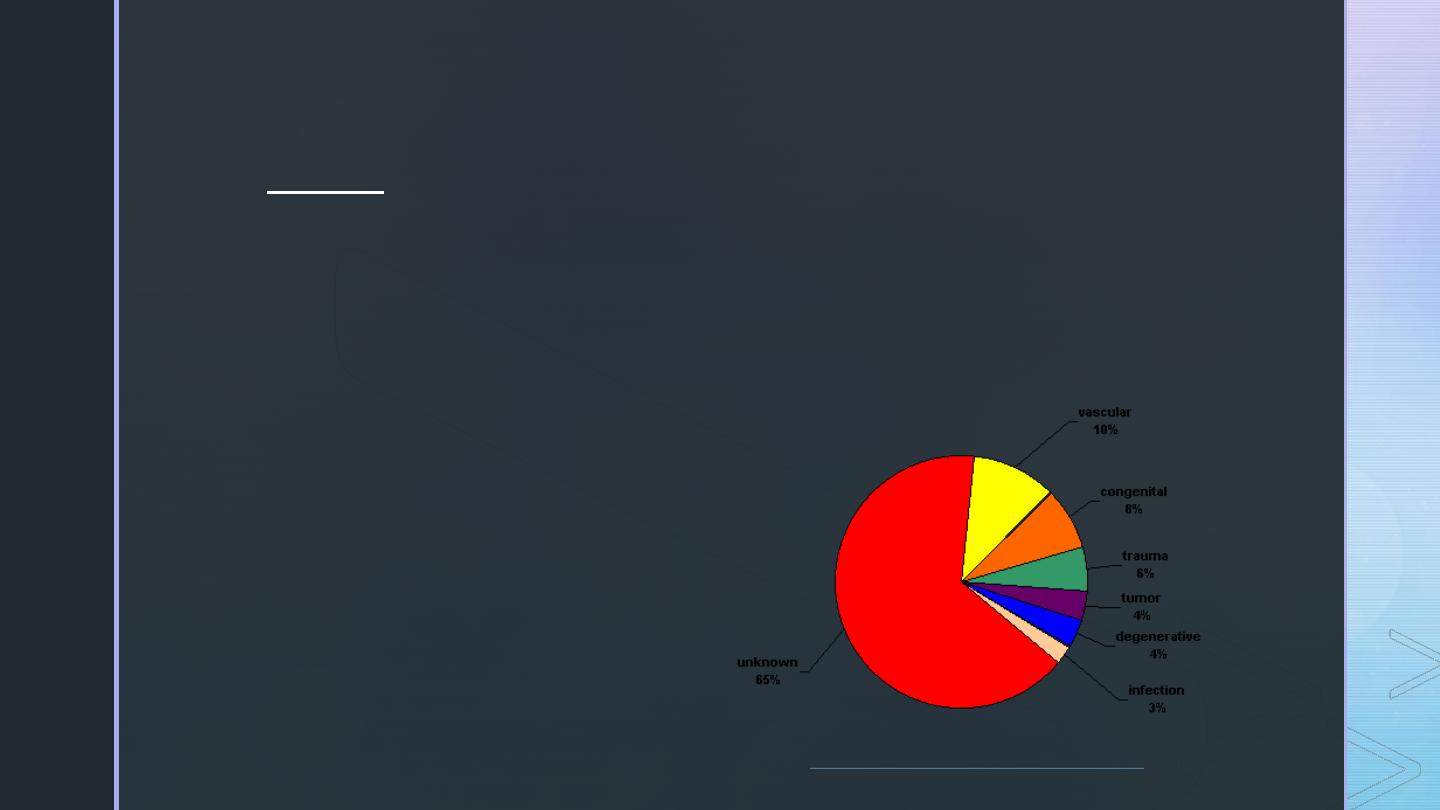
Causes:
▪
Genetic (autosomal dominant genes)
▪
Congenital defects
▪
Severe head trauma
▪
Ischemic injury, tumor
▪
Drug abuse
▪
Unknown
z
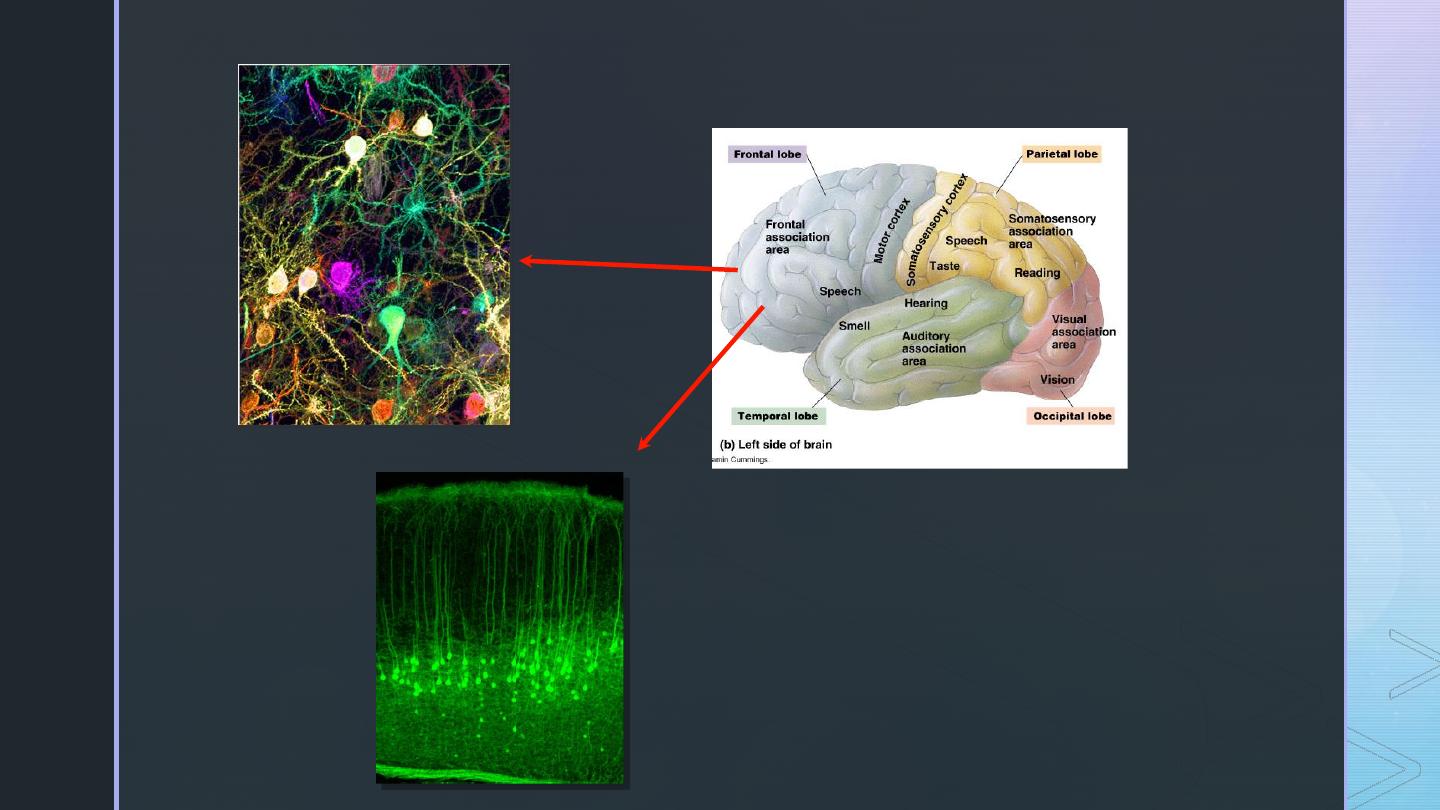
Basic Neuroscience Relevant to Seizure
Disorders and Epilepsy
z
The Brain
An extremely complex organ
made up of billions of
connections between neurons.
These connections are each
highly controlled and regulated.
z
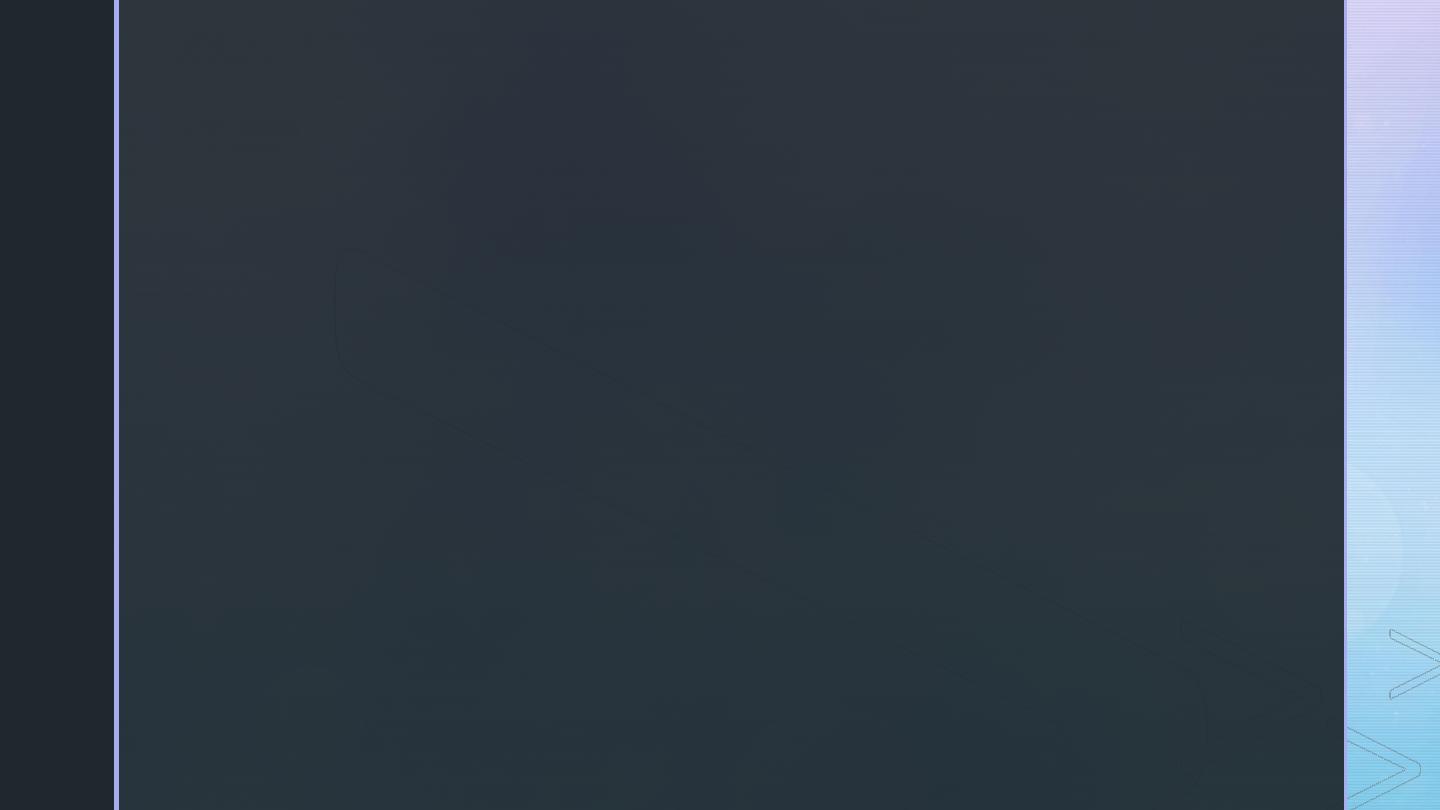
Nerve Cell Communication
▪
Neurons communicate between themselves using small molecules called
neurotransmitters.
▪
These neurotransmitters modulate and regulate the electrical activity of a given neuron,
and tell it when to fire an action potential or when not to.
-
Glutamate = excitatory (tells the neuron to fire)
-
GABA = inhibitory (dampens the neuron firing rate)
▪
The action potential is an electrical signal that travels down the axon, and is created using
sodium ions (Na+), and inhibited by potassium ions (K+).
▪
Usually these processes work synergistically to produce normal behavior and activity.
▪
When dysfunctional, abnormal electrical activity occurs and can produce seizures.
z
Cellular Mechanisms of
Seizure Generation
⬧ Excitation (too much)
▪
Ionic: inward Na
+
and Ca
++
currents
▪
Neurotransmitter: glutamate, aspartate
⬧ Inhibition (too little)
▪
Ionic: inward CI
-
, outward K
+
currents
▪
Neurotransmitter: GABA
P
-Sli
de
9
Am
e
ric
a
n
Epile
p
s
y
Soc
ie
ty
2
0
1
1
z
Neurotransmitters
Sodium Ions/Channels
Potassium Ions/Channels
Action Potential
(Glutamate, GABA)
z
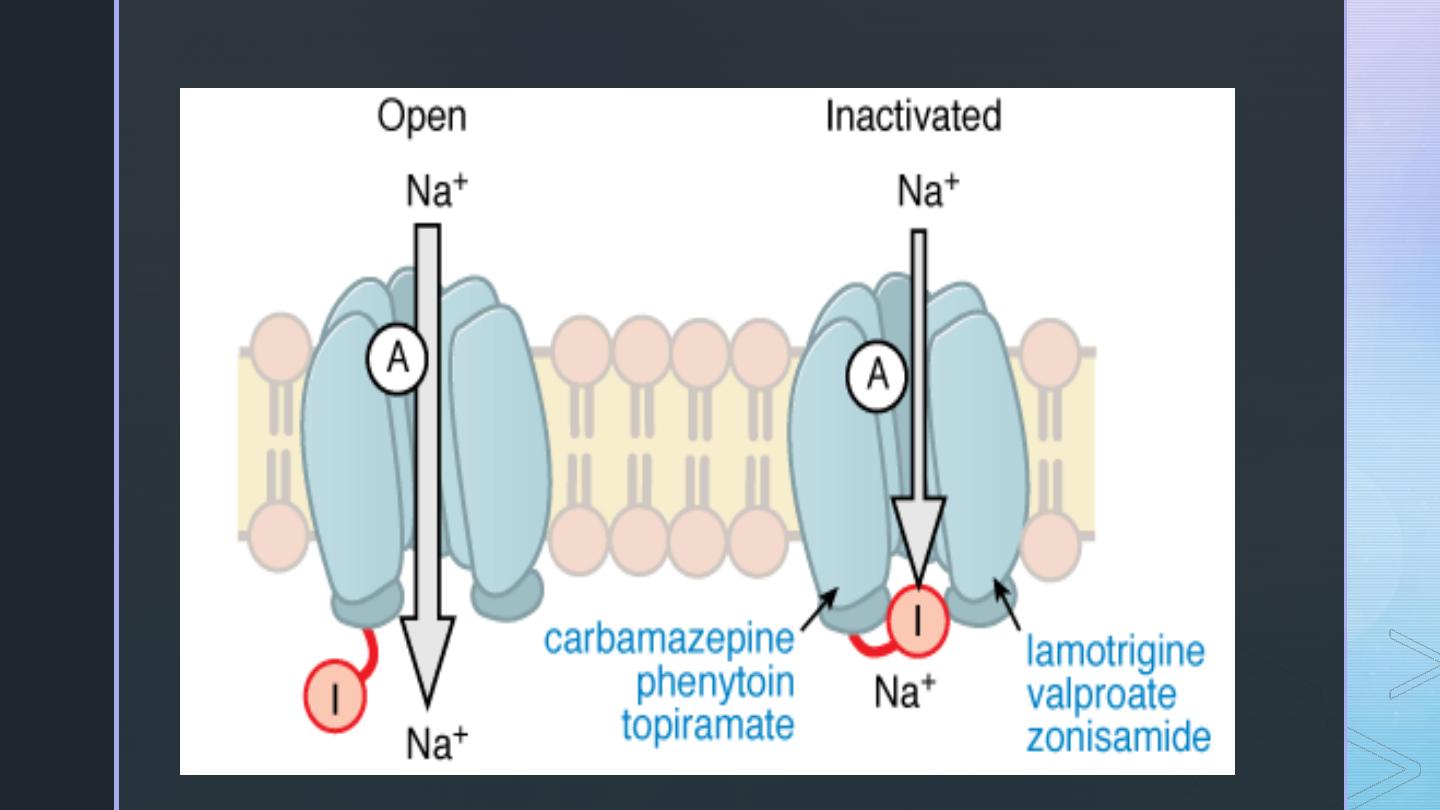
GABA Receptors
GABA is the major inhibitory neurotransmitter in the CNS. There
are 2 types of receptors:
▪
GABA
A
receptor
▪
Postsynaptic fast inhibition
▪
Specific recognition sites (see next slide)
▪
Inhibition mediated by CI
-
current
▪
GABA
B
receptor
▪
Postsynaptic slow inhibition
▪
Pre-synaptic reduction in calcium influx
▪
Inhibition mediated by K
+
current
Am
e
ric
a
n
Epile
p
s
y
Soc
ie
ty
2
0
1
1
P-Slide
14
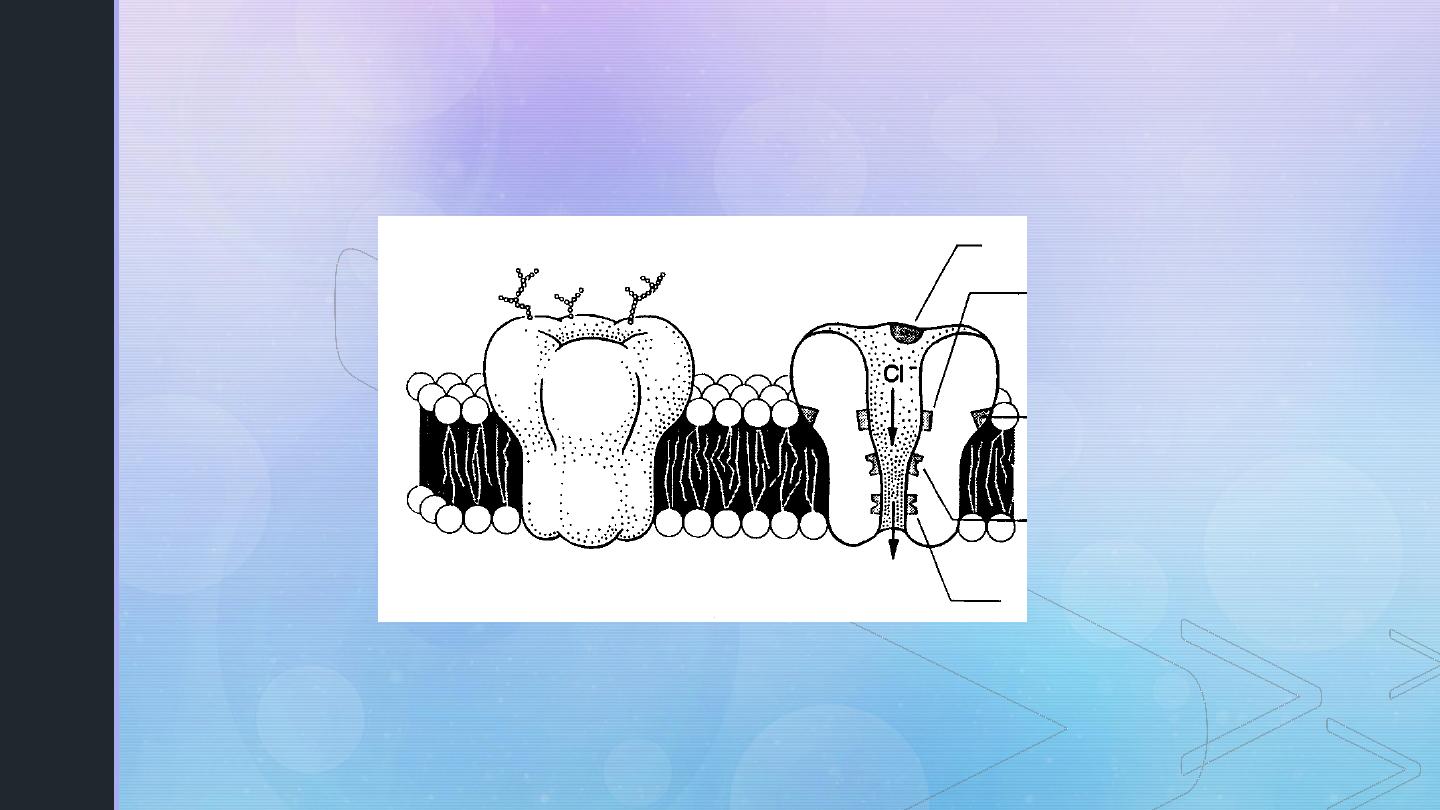
GABA Receptors
Diagram of the GABA
A
receptor
P-Slide 15
GABA site
Barbiturate site
Benzodiazepine
site
Steroid site
Picrotoxin site
z
Glutamate Receptors
▪
Group I mGluRs (mGluRs 1 and 5)
▪
Primarily postsynaptic/perisynaptic
▪
Net excitatory effect (ictogenic)
▪
Couple to inositol triphosphate
▪
Long-lasting effects (epileptogenic)
▪
Group II (mGluRs 2 & 3) and group III (4,6,7,8)
▪
Primarily presynaptic
▪
Net inhibitory effect; reduce transmitter release
▪
Negatively coupled to adenylate cyclase, reduce cAMP
Am
e
ric
a
n
Epile
p
s
y
Soc
ie
ty
2
0
1
1
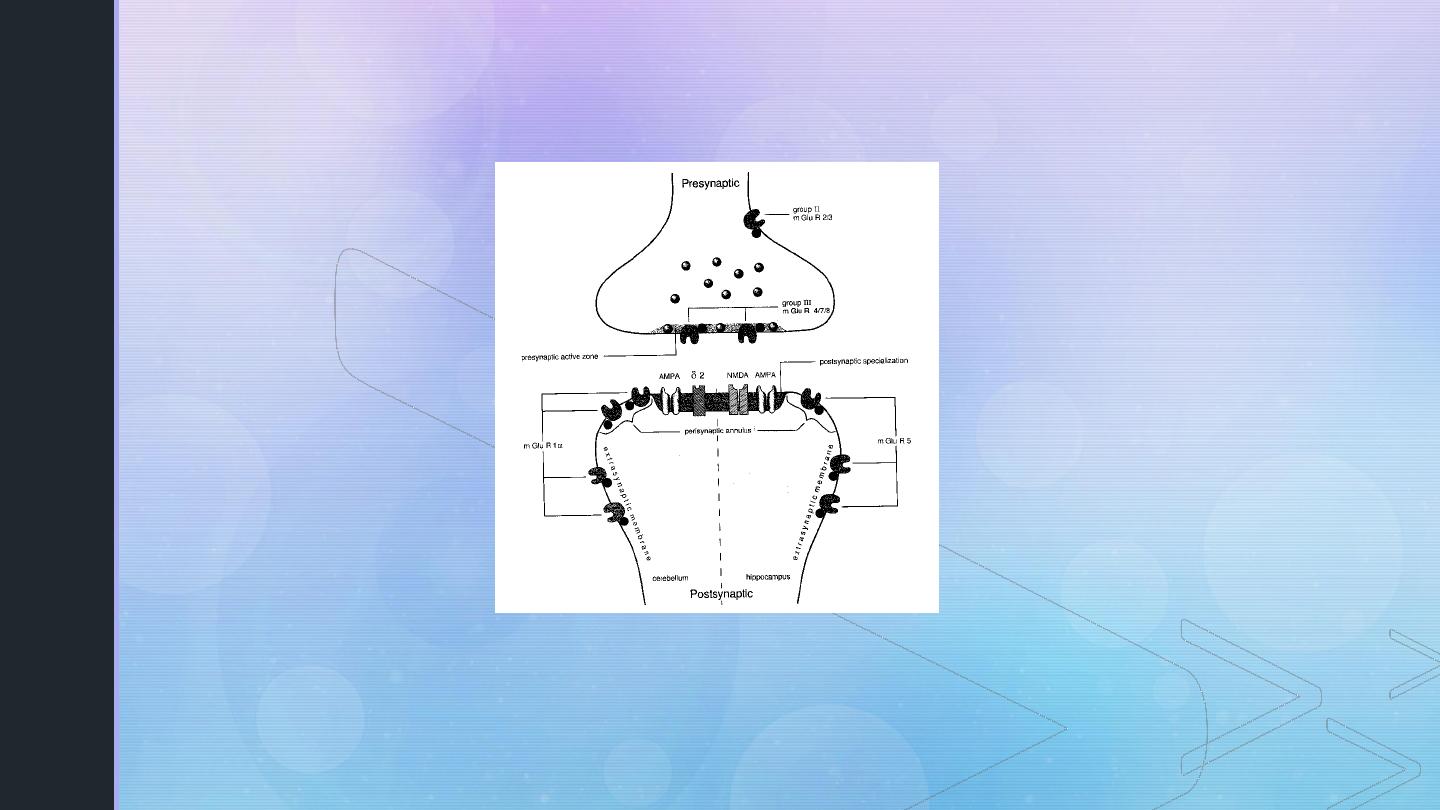
Glutamate Receptors
P-Slide 17
Diagram of the various glutamate receptor
subtypes and locations
z
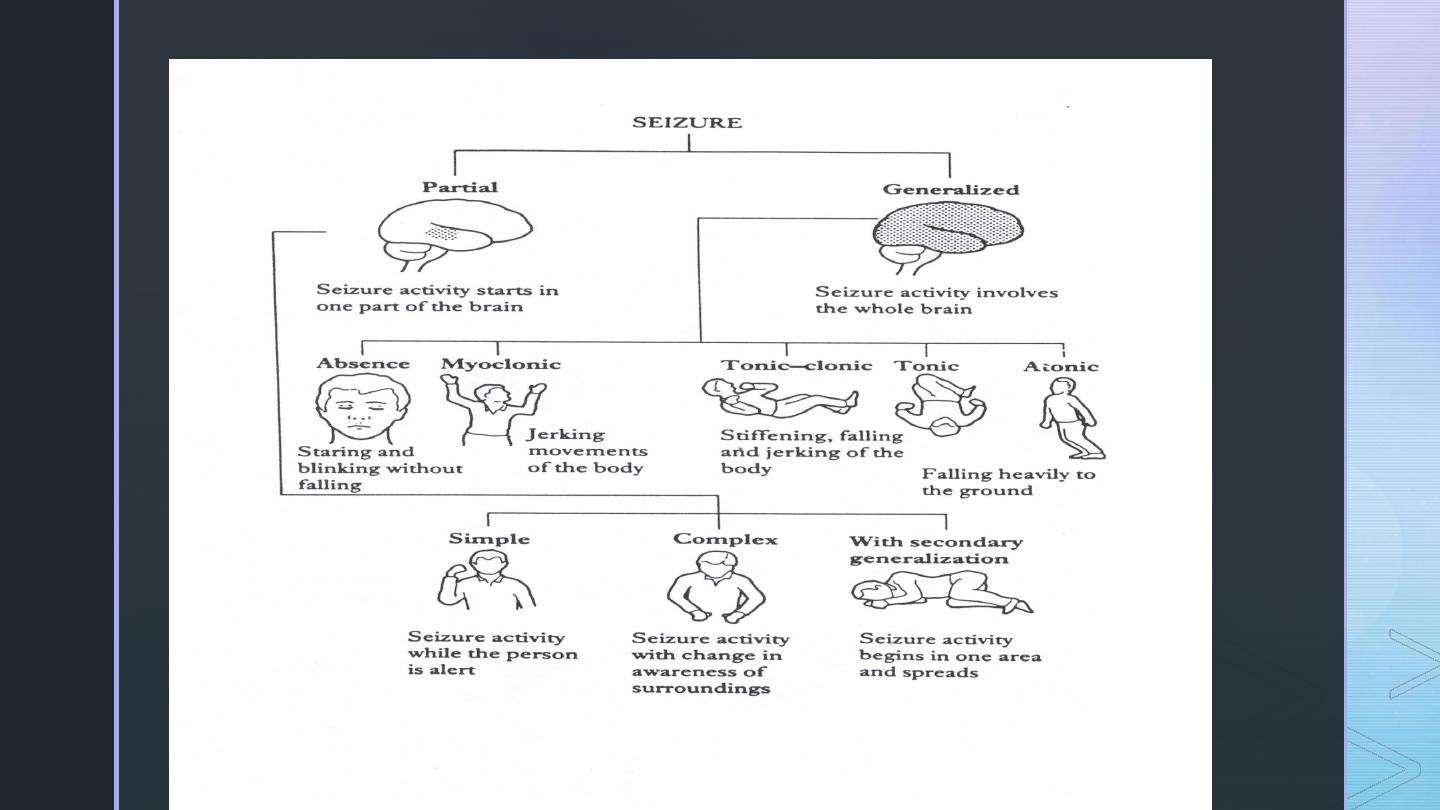
TYPES OF SEIZURES
z
Partial (focal) Seizures
▪
Excessive electrical activity in one cerebral hemisphere. -
Affects only part of the body.
▪
Simple Partial: Person may experience a range of strange or
unusual sensations.
▪
Motor
▪
Sensory
▪
Autonomic
▪
Key feature: preservation of consciousness.
z
Partial (focal) Seizures
▪
Complex Partial:
▪
Loss of awareness at seizure onset. Person seems dazed or
confused and exhibits meaningless behaviors.
▪
Typically originate in frontal or temporal lobes (e.g. Temporal lobe
epilepsy)
z
Generalized Seizures
▪
Excessive electrical activity in both cerebral hemispheres.
▪
Usually originates in the thalamus or brainstem.
▪
Affects the whole body.
▪
Loss of consciousness is common.
z
Generalized Seizures
▪
Myoclonic: Brief shock-like muscle jerks generalized or restricted to part of one
extremity.
▪
Atonic: Sudden loss of muscle tone.
▪
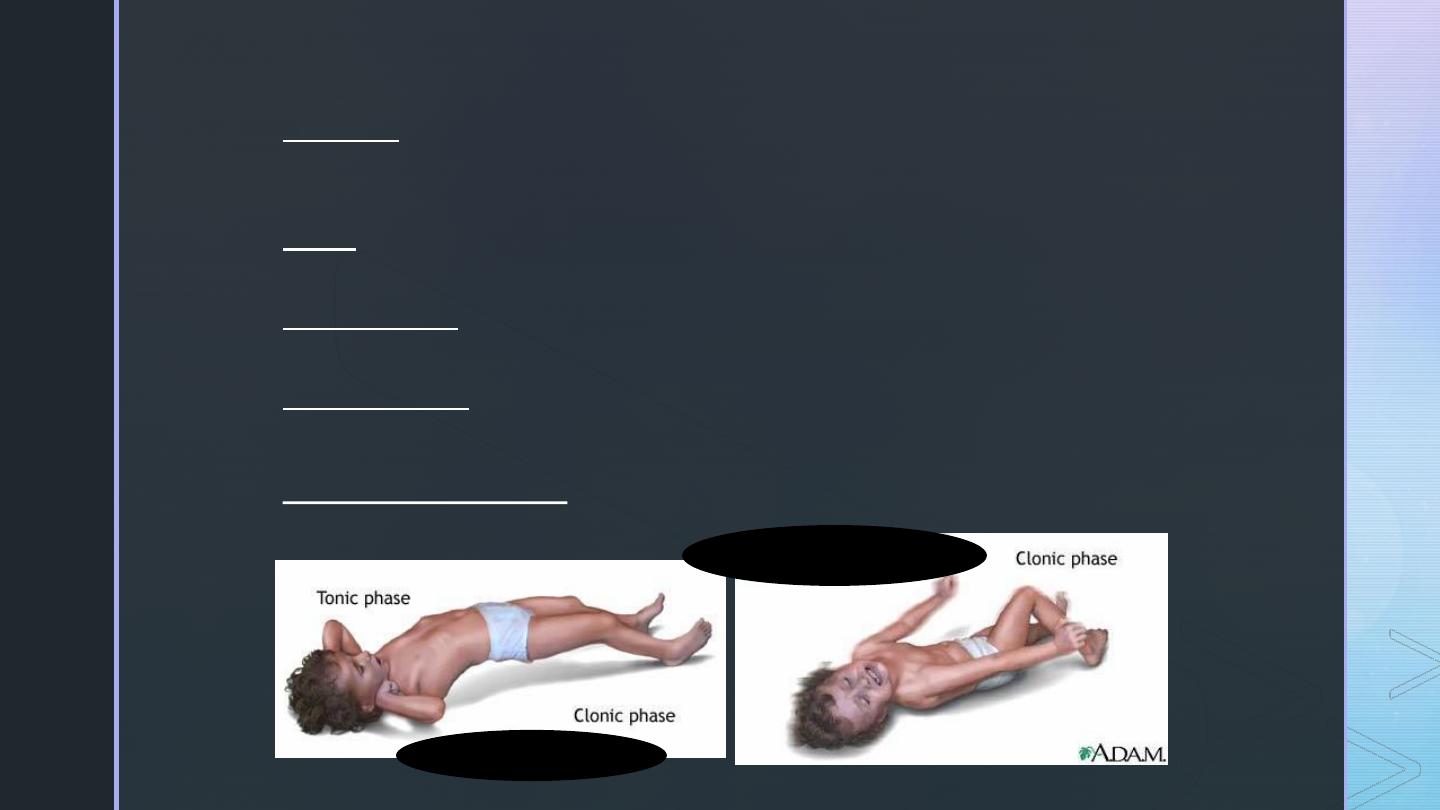
Tonic Seizures: sudden stiffening of the body, arms, or legs
▪
Clonic Seizures: rhythmic jerking movements of the arms and legs without a tonic
component
▪
Tonic-clonic (grand mal):
▪
Tonic phase followed by clonic phase
z
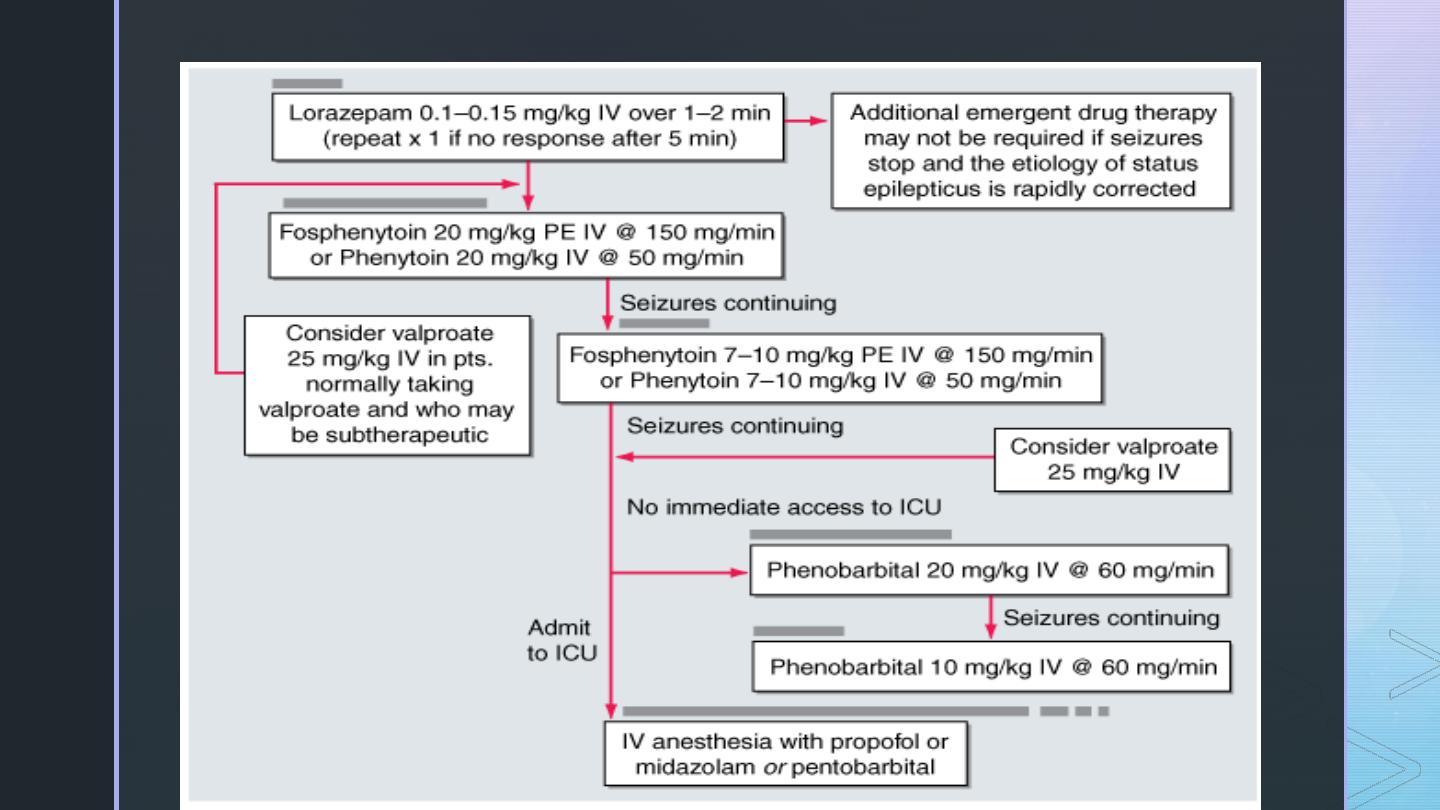
Tonic-Clonic Seizure
Can last from one to several minutes
Therapeutic intervention = lorazepam injection
Status epilepticus :
Prolonged seizure (>20 0 min) of any of the
types previously described; the most common
is life threatening generalized tonic–clonic
status epilepticus.
z
Generalized Seizures
▪
Absence (petit mal):
Person appears to “blank out” - “Daydreaming”
▪
Simple Absence (primarily effects consciousness only)
▪
Complex Absence
▪
Atypical Absence (Includes physical symptoms like eye blinking or lip movements)
▪
Lenox-Glastaut Syndrome.
▪
Atypical absence, atonic and myclonic
▪
Status Epilepticus: A seizure lasting longer than 30 min, or 3 seizures without a normal period in
between
▪
May be fatal
▪
Emergency intervention required
z
Absence Seizure
Can last from a second to several minutes
z
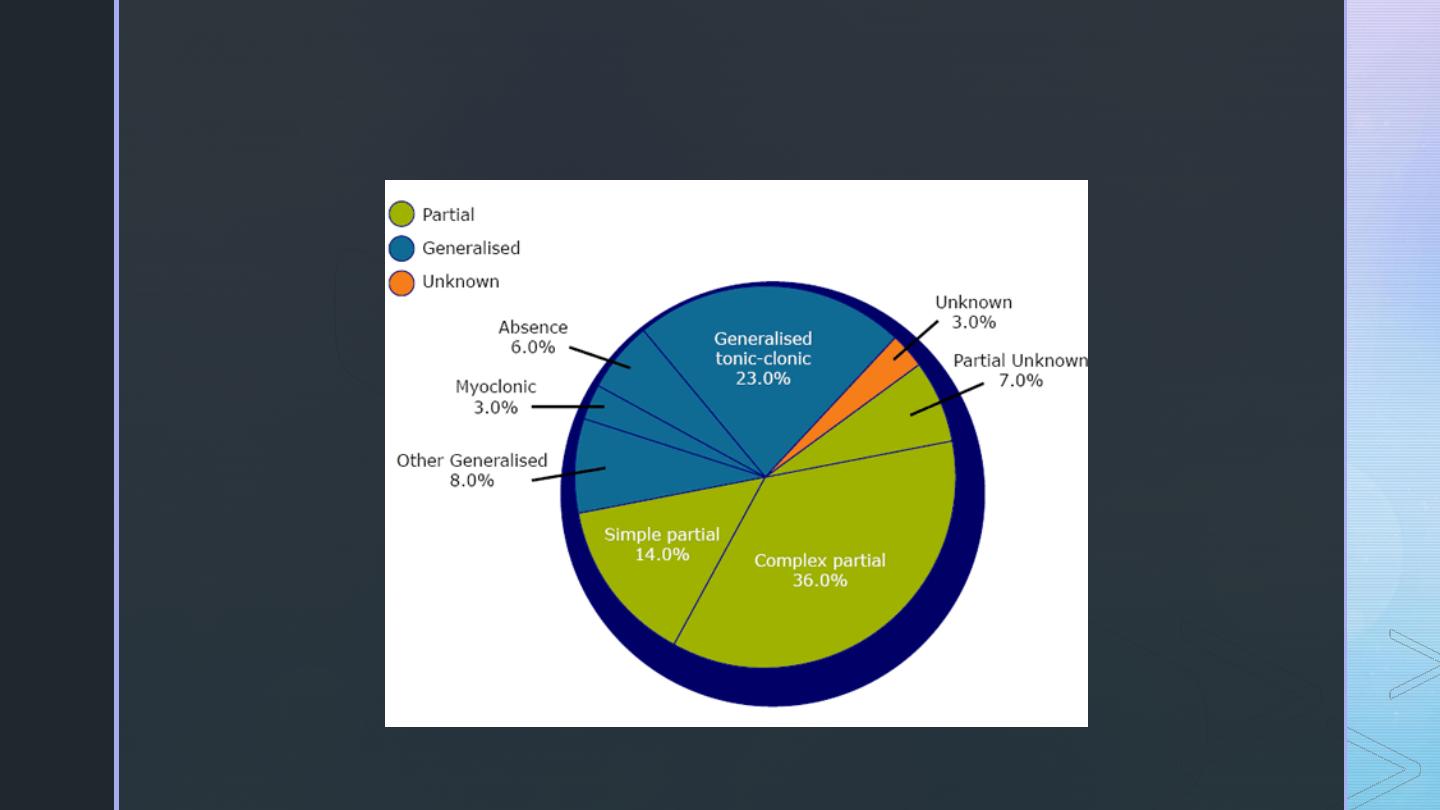
Incidence of Seizure Types
Mayo Clinic Proceedings 1996; 71:576-568
z
Seizure Facts
▪
Seizures are not usually life threatening.
▪
The brain almost always stops the seizure on its own.
▪
Breathing may cease for a few seconds, and the patient may turn
blue.
▪
People don’t feel pain during a seizure; muscles may be sore
afterward.
▪
Person may be “different” for a while after the seizure.
z
Antiepileptic Drug
▪
An antiepileptic drug (AED) is a drug which decreases the
frequency and/or severity of seizures in people with epilepsy
⬧
Treats the symptom of seizures, not the underlying epileptic
condition
⬧
Does not prevent the development of epilepsy in individuals
who have acquired a risk for seizures (e.g., after head
trauma, stroke, tumor)
▪
Goal of therapy is to maximize quality of life by eliminating
seizures (or diminish seizure frequency) while minimizing
adverse drug effects
P
-Sli
de
29
Am
e
ric
a
n
Epile
p
s
y
Soc
ie
ty
2
0
1
1
z
Treatment
▪
Try to find a cause. (e.g. fever, head trauma, drug abuse)
▪
Recurrent seizures that cannot be attributed to any cause are seen in
patients with epilepsy.
▪
Therapy is aimed at control
▪
drugs do not cure.
▪
The type of seizure determines the choice of drug!
▪
More than 80% of patients with epilepsy can have can have their
seizures controlled with medications.
z
Treatment
▪
Monotherapy with anticonvulsant
▪
Increase dose gradually until seizures are controlled or adverse effects
become unacceptable.
▪
Multiple-drug therapy may be required.
▪
Achieve steady-state kinetics
▪
Monitor plasma drug levels
▪
Avoid sudden withdrawal
Diphenylhydantoin ( Phenytoin)
Mechanism:
it blocks Na + , K + and Ca2+
channels in the brain (and heart) leading to decrease propagation of
abnormal impulses. It produces some degree of drowsiness.
Therapeutic uses
Partial and generalized seizures
Status epilepticus : it should be given i.v. in the form of fosphenytoin (prodrug
).
Ventricular arrhythmia .
Adverse effects
– CNS : Nystagmus, diplopia, ataxia.
– Hepatotoxicity .
– Microsomal enzyme induction .
– Bone marrow depression & Megaloblastic anemia (due to ↓ folic acid).
– Teratogenicity a y: craniofacial abnormalities.
– Gingival hyperplasia : 2ry to increased expression of platelet derived growth
factor (PDGF )).
- Lymphadenopathy
z
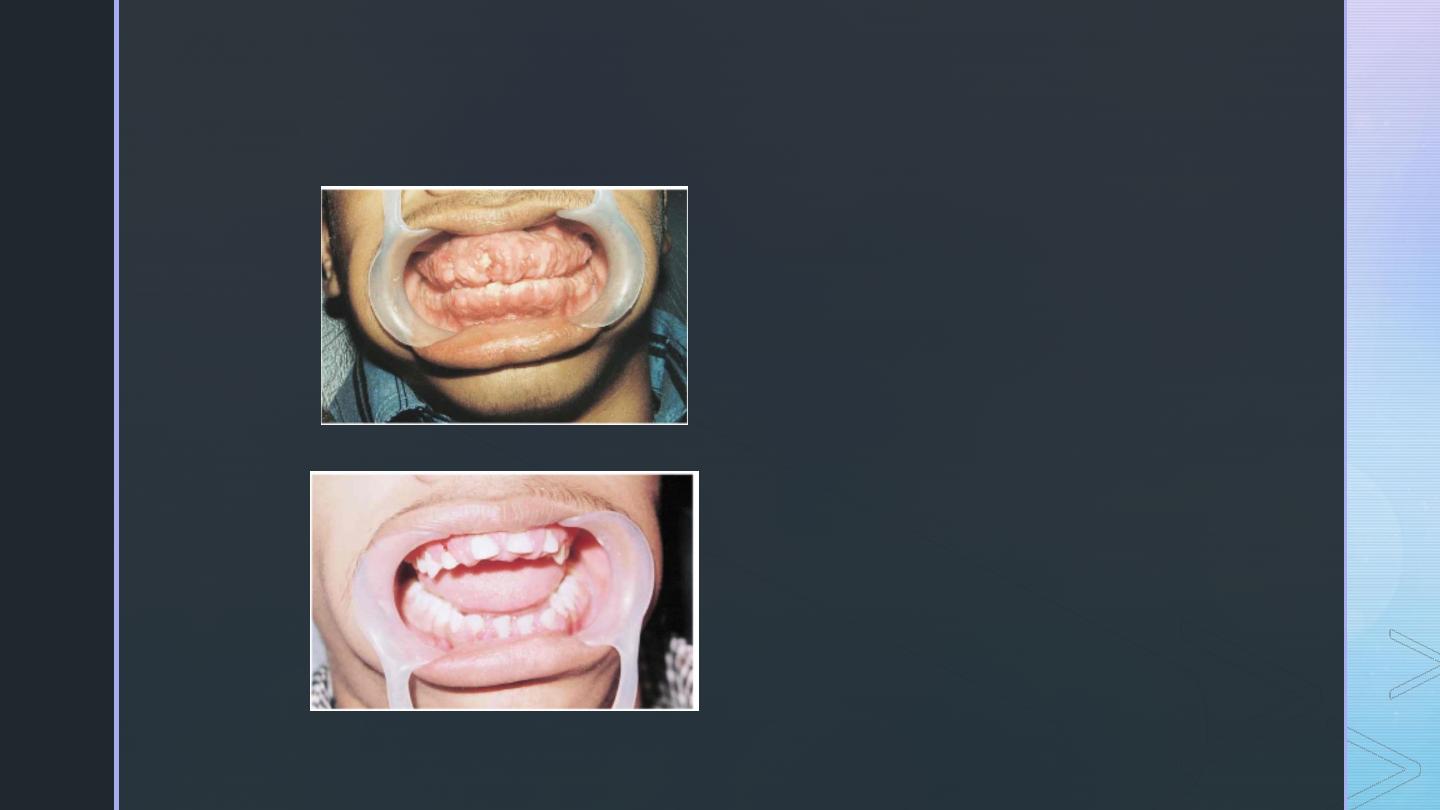
Phenytoin Induced Gingival Hyperplasia
17 year old boy treated with
300mg/day phenytoin for 2
years (unsupervised)
Partial recovery at 3 months
after discontinuation
Images in Clinical Medicine (Feb 2000) 342:325
2. Carbmazepine (Tegretol)
Mechanism: it blocks Na+ channels & ↓ excitability of cortical neurons.
Therapeutic uses
Partial and generalized seizures (grand mal epilepsy).
Trigeminal neuralgia.
Adverse effects
– CNS: diplopia & ataxia.
– Hepatotoxicity.
– Microsomal enzyme induction.
– Bone marrow depression.
– Congestive heart failure (CHF).
3.
Valproic acid (Depakene)
Mechanism: it activates glutamic acid decarboxylase enzyme→ ↑ GABA synthesis.
Therapeutic uses: all types of epilepsy.
Adverse effects
– Sedation
– Microsomal enzyme inhibition
– Teratogenicity.
– Alopecia
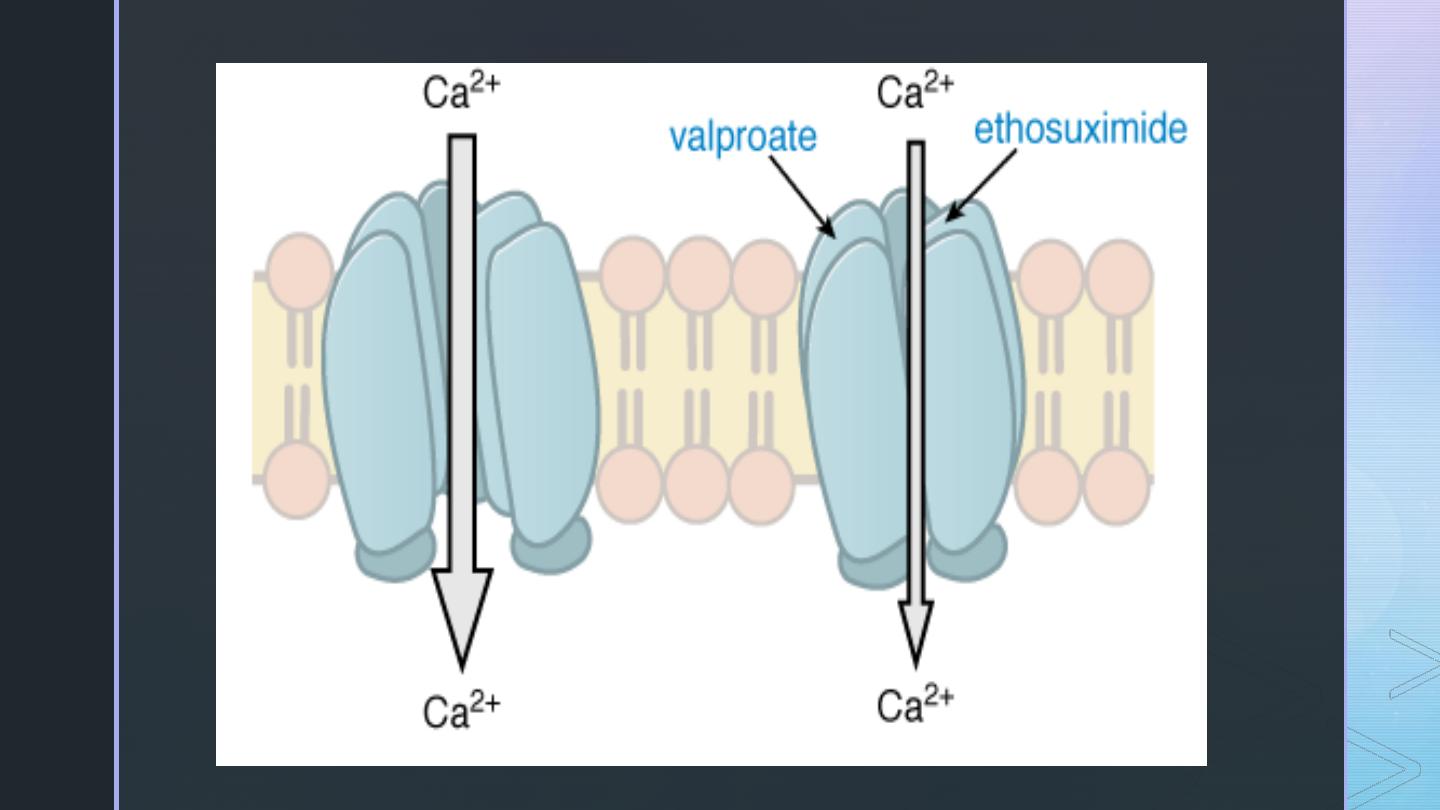
4.
Ethosuximide (Zarontin
)
Mechanism: blocks neuronal voltage-dependent Ca2+ and Na+ channels.
Therapeutic uses: absence seizures (petit mal epilepsy) (1st choice).
Adverse effects
– Sedation
– Vomiting
– Leucopenia
5.
Benzodiazepines: Clonazepam and diazepam
Mechanism: allosteric modulation of GABA action to facilitate its effects.
Therapeutic uses
Clonazepam: petit mal epilepsy.
Diazepam: status epilepticus.
Adverse effects: see before.
6.
Barbiturates: Phenobarbitone
Mechanism: enhancement of GABA-mediated inhibition of glutamate excitation.
Therapeutic uses: grand mal epilepsy (contraindicated in petit mal epilepsy).
Adverse effects: see before.
█
NEWER ANTIEPILEPTIC DRUGS
1.
Felbamate
Mechanism
Block glycine site on the N-methyl-D-aspartate (NMDA) receptors.
2+ +
Block voltage-dependent Ca & Na channels.
Therapeutic uses: wide variety of partial and generalized seizures.
Adverse effects
– Hepatotoxicity
– Microsomal enzyme induction.
– Bone marrow depression.
2.
Lamotrigine
Mechanism
Decreases glutamate and aspartate, which are excitatory neurotransmitters
Blocks sodium channels and high voltage-dependent calcium channels leading
to ↓ excitability.
Therapeutic uses: wide variety of partial and generalized seizures and typical
absence seizures in children and adults.
3.
Gabapentin
Mechanism: unknown but may interfere with voltage-dependent Ca2+ channels
Therapeutic uses: as adjuvant therapy in wide variety of partial and generalized
seizures.
Adverse effects: headache, nystagmus, dizziness & ataxia.
4.
Tiagabine
Potent and specific inhibitor of GABA uptake into glial and other neurons. Thus, it
enhances the action of GABA by decreasing its removal from the synaptic
z
Status epilepticus management
z
During pregnancy
Safer antiepileptics
▪
Carbamazepine
▪
Oxcarbamazepine
▪
Lamotrigine
▪
Ethosuximide
Folic acid supplement
z
Summary
z
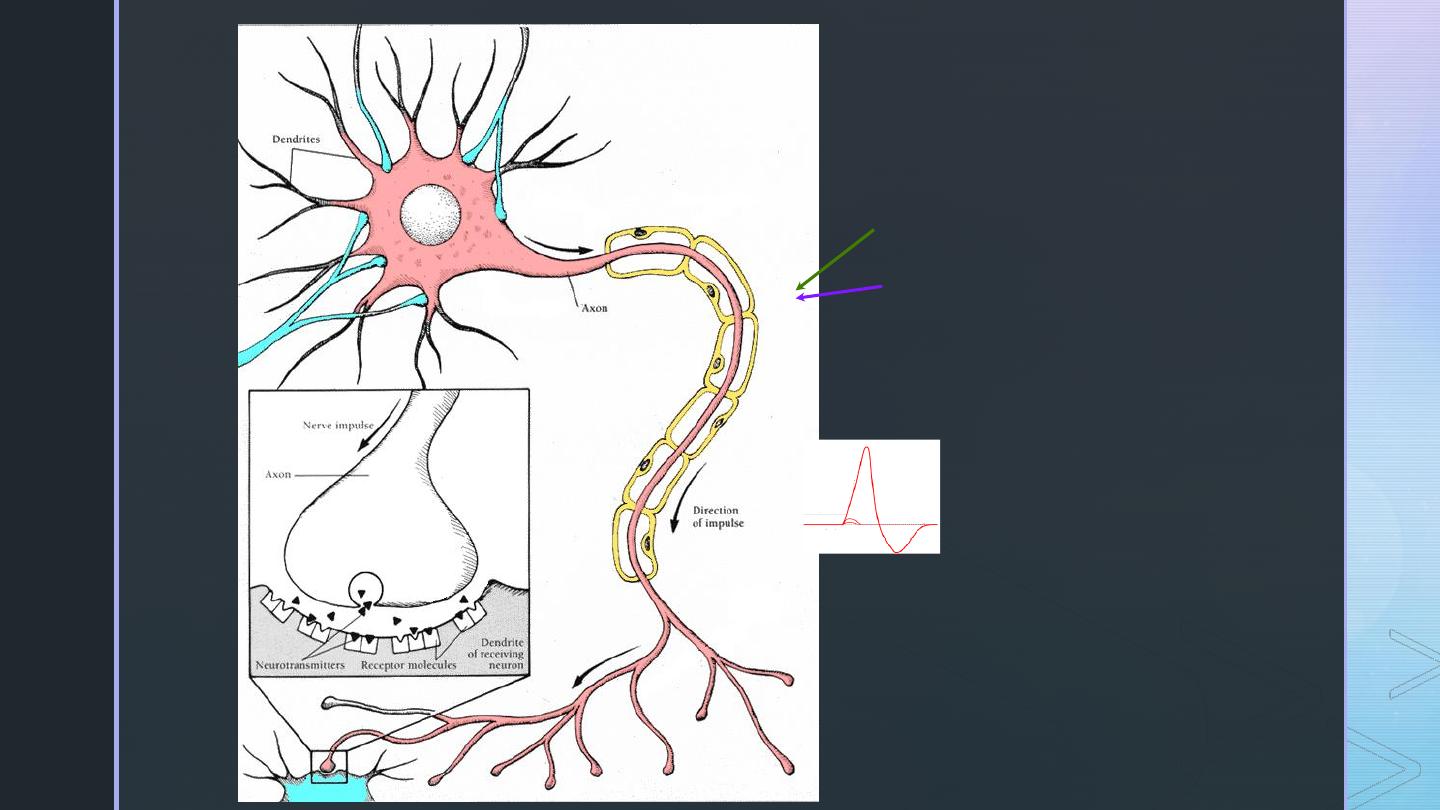
Na+ Channel Drugs
▪
Phenytoin (Dilantin, Phenytek)
▪
Cabamazepine (Tegretol, Carbatrol)
▪
Valproic Acid (Depakene, Depakote)
▪
Lamotrigine (Lamictal)
▪
Topiramate (Topamax)
▪
Zonisamide (Zonegran)
▪
Lidocaine
z
GABA Drugs
▪
Barbiturates:
▪
Phenobarbital (Luminal)
▪
Pimidone (Mysoline)
▪
Benzodiazepines:
▪
Diazepam (Valium)
▪
Lorazepam (Ativan)
▪
Clonazepam (Klonopin)
▪
Clorazepate (Tranxene-SD)
•Tiagabine (Gabitril)
•Valproic Acid (Depakene, Depakote)
•Topiramate (Topamax)
•Zonisamide (Zonegran)
z
Ca
2+
Channel Drugs
▪
Ethosuximide (Zarontin)
▪
Valproic Acid (Depakene, Depakote)
▪
Zonisamide (Zonegran)
▪
Gabapentin (Neurontin)
▪
Pregabalin (Lyrica)
▪
Levetiracetam (Keppra)
z
Other/Unknown MOA
▪
Magnesium chloride
▪
Paraldehyde
z
Primary Generalized Tonic-Clonic
(Grand Mal) Seizures
▪
Drugs of Choice:
▪
Phenytoin
▪
Carbamazepine
▪
Oxcarbazepine
▪
Valproate
•Alternatives
•Lamotrigine
•Topiramate
•Zonisamide
•Levetiracetam
•Primidone
•Phenobarbital
•Diazepam
z
Partial, Including Secondarily
Generalized Seizures
▪
Drugs of Choice:
▪
Phenytoin
▪
Carbamazepine
▪
Oxcarbazepine
▪
Valproate
•Alternatives
•Lamotrigine
•Topiramate
•Zonisamide
•Levetiracetam
•Primidone
•Phenobarbital
•Gabapentin
•Pregabalin
•Tiagabine
z
Absence (Petit Mal)
▪
Drugs of Choice:
▪
Ethosuximide
▪
Valproate
•Alternatives
•Clonazepam
•Zonisamide
z
Atypical Absence, Myoclonic, Atonic
Seizures
▪
Drug of Choice:
▪
Valproate
•Alternatives
•Clonazepam
•Topiramate
•Zonisamide
•Levetiracetam
