Medical physiology Endocrinology
Dr: ABDULHASAN ALNIYAZI
Ph.D. Medical Physiology
_____________________________________________________________________________________
26
About 99% of calcium is stored in the bones and only about 1% is in the cells, and
0.1 % of body calcium is in the extracellular fluid. The bones can serve as large
reservoirs, releasing calcium when extracellular fluid concentration decreases and
storing excess calcium. 40% of the total blood Ca
2+
is bound to plasma proteins,
mainly albumin, 10% is complexed to anions (e.g., phosphate, sulfate, and citrate)
and 50% are free ionized Ca
2+
and it is the only form of Ca
2+
that is biologically
active. The calcium concentration in the interstitial fluid is 100 times higher than
the intracellular calcium concentration.
Factors affect ECF calcium
Extracellular fluid calcium concentration normally is 2.4 mmol/L, calcium plays a
key role in contraction of muscles; blood clotting; and transmission of nerve
impulses. A number of factors can effect ECF calcium concentration:
1. Increases in plasma protein concentration increases total Ca
2+
concentration.
2. Increases plasma phosphate, decrease the ionized (free) Ca
2+
concentration.
3. Acidosis increases concentration of ionized (free) Ca
2+
.
4. Alkalosis decreases concentration of ionized (free) Ca
2+
.
The usual daily intake of calcium is about 1000 mg. Vitamin D promotes calcium
absorption by the intestines. About 90% (900 mg/day) of the daily intake of
calcium is excreted in the feces.
Parathyroid hormone (PTH)
Physiologic Anatomy of the Parathyroid Glands.
Medical physiology Endocrinology
Dr: ABDULHASAN ALNIYAZI
Ph.D. Medical Physiology
_____________________________________________________________________________________
27
There are four parathyroid glands in humans; they are located immediately behind
the thyroid gland. The parathyroid gland contains mainly chief cells and oxyphil
cells. The chief cells are believed to secrete most of the PTH.
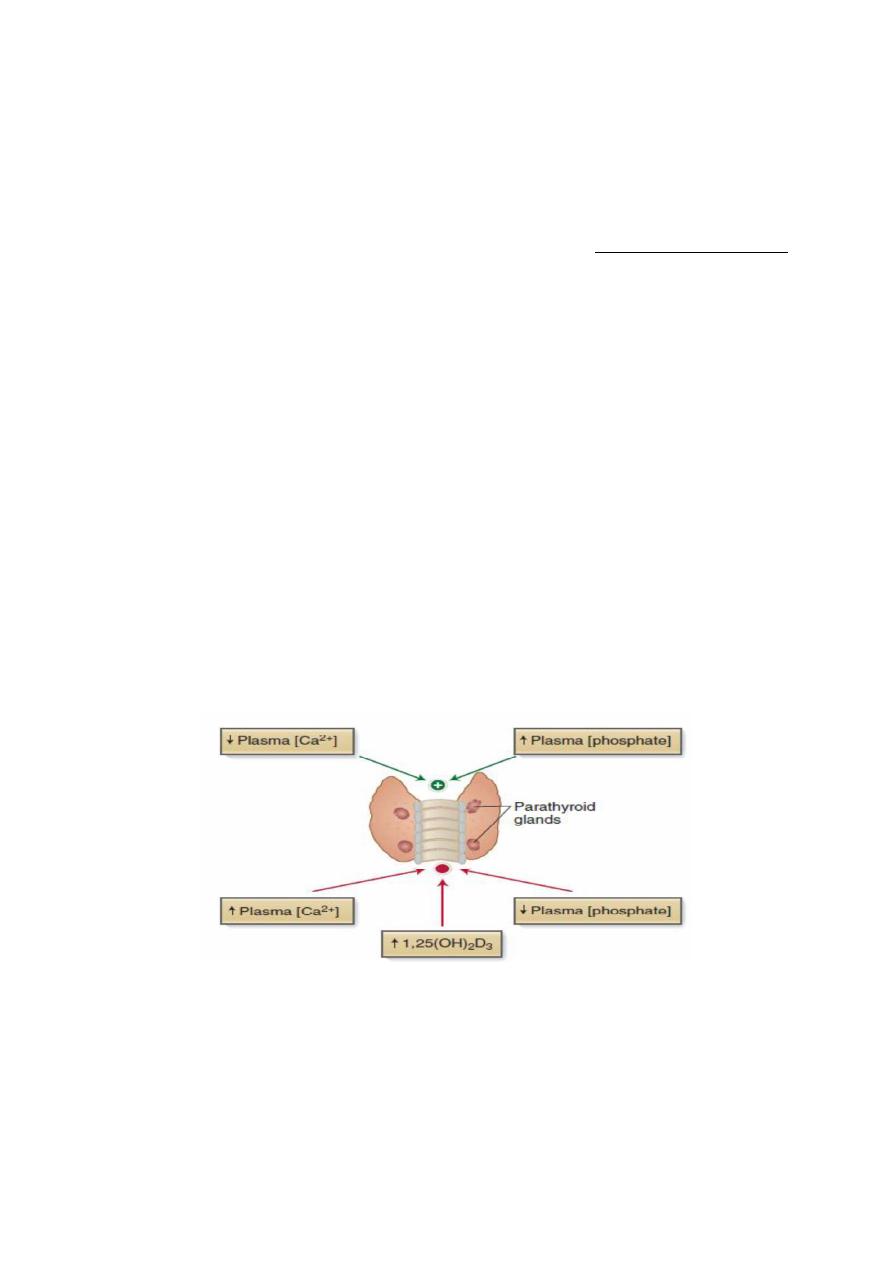
Control of PTH secretion
The rate of PTH secretion is regulated by the following three factors:
1. Plasma free Ca
2+
.
A decrease in the plasma Ca
2+
is the most potent stimulus for PTH secretion. Chief
cells sense plasma Ca
2+
concentration through expression of the extracellular Ca
2+
-
sensing receptor (CaSR).
2. Plasma phosphate.
A prolonged increase in phosphate concentration stimulates PTH secretion.
3. Vitamin D.
PTH stimulates vitamin D synthesis, which exerts negative feedback inhibition on
PTH secretion.
Figure: Control of PTH secretion
Calcium-sensing receptor (CaSR)
Medical physiology Endocrinology
Dr: ABDULHASAN ALNIYAZI
Ph.D. Medical Physiology
_____________________________________________________________________________________
28
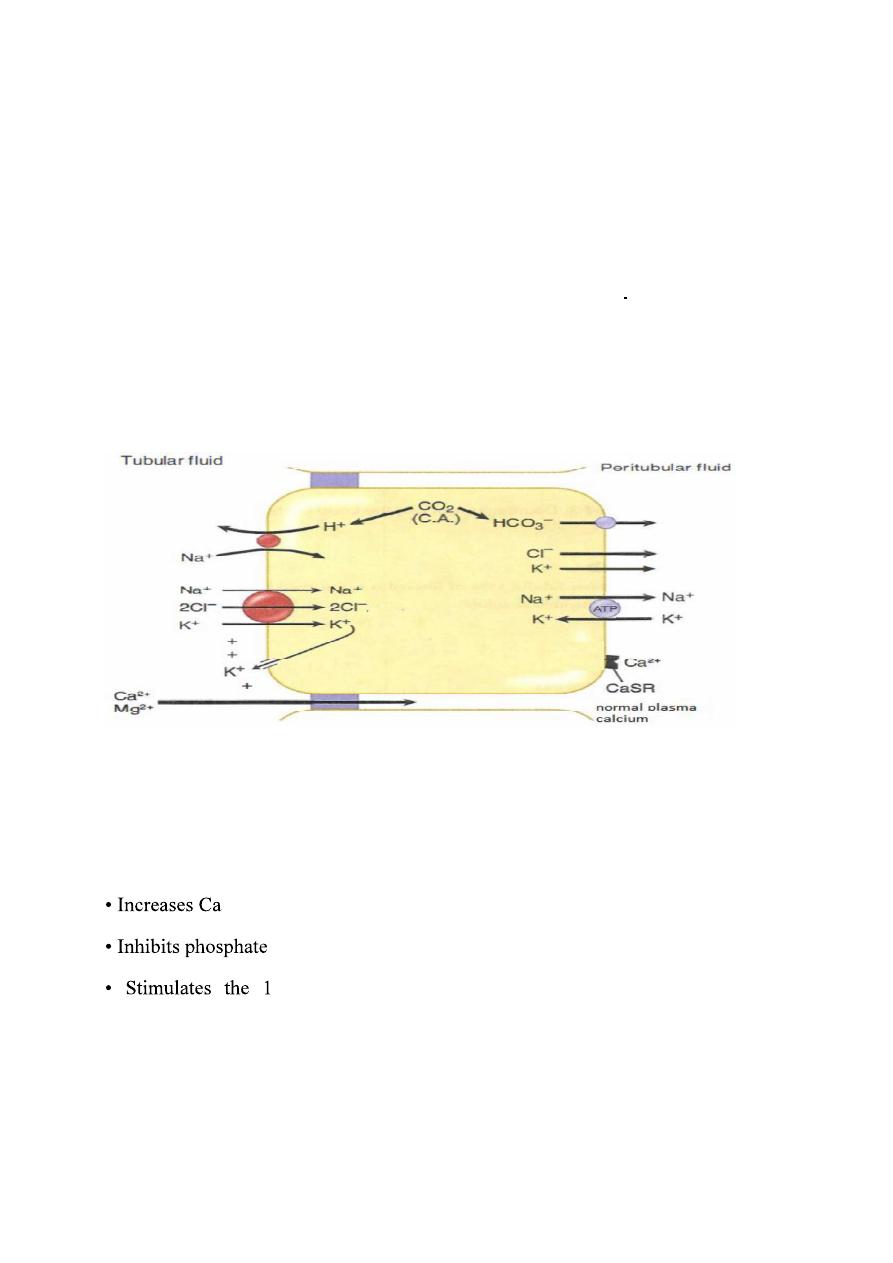
The cells of the parathyroid gland and the basolateral membrane of cells in Thick
segment of loop of Henle contain CaSR, this receptors influence by the plasma
concentration of calcium. when plasma calcium level is high CaSR is activated
which in turn lead to inhibition of the Na
+
-K
+
-2Cl
-
transporter This will decrease
K
+
movement from cell into lumen, reducing the positive luminal potential which
in turn, decreases calcium reabsorption and return plasma calcium concentration
to normal level.
Figure. Calcium-sensing receptor (CaSR).
Actions of PTH
A decrease in the free calcium is the signal to increase PTH secretion and the
function of PTH is to raise free calcium, which it does by several mechanisms.
2+
reabsorption in distal tubule of the kidney.
reabsorption in proximal tubule of the kidney.
-alpha-hydroxylase enzyme in kidney, converting inactive
vitamin D to its active form which in turn increase intestinal reabsorption of Ca
2+
and phosphate.
Medical physiology Endocrinology
Dr: ABDULHASAN ALNIYAZI
Ph.D. Medical Physiology
_____________________________________________________________________________________
29
osteoblasts (cells responsible for osteoid synthesis) inducing the
synthesis of specific proteins, which activate the already present osteoclasts (cells
responsible for bone resorption) and stimulate the formation of new osteoclasts.
Osteoclasts in turn causes bone resorption, releasing Ca
2+
and phosphate into the
blood.
Calcitonin
Calcitonin (CT) is a peptide hormone secreted by the parafollicular cells of the
thyroid gland. It is released in response to elevated free calcium. Calcitonin lowers
plasma calcium by decreasing the activity of osteoclasts, thus decreasing bone
resorption, this results in less demineralization of the bone and therefore a decrease
in the release of calcium and phosphate from the bone into the blood. Calcitonin
has no direct effect on bone formation by osteoblasts.
Calcitonin is useful in the treatment of severe hypercalcemia, osteoporosis and
Paget's disease (disease characterized by a significant increase in osteoclast activity
and, thus, a high rate of bone turnover and hypercalcemia),
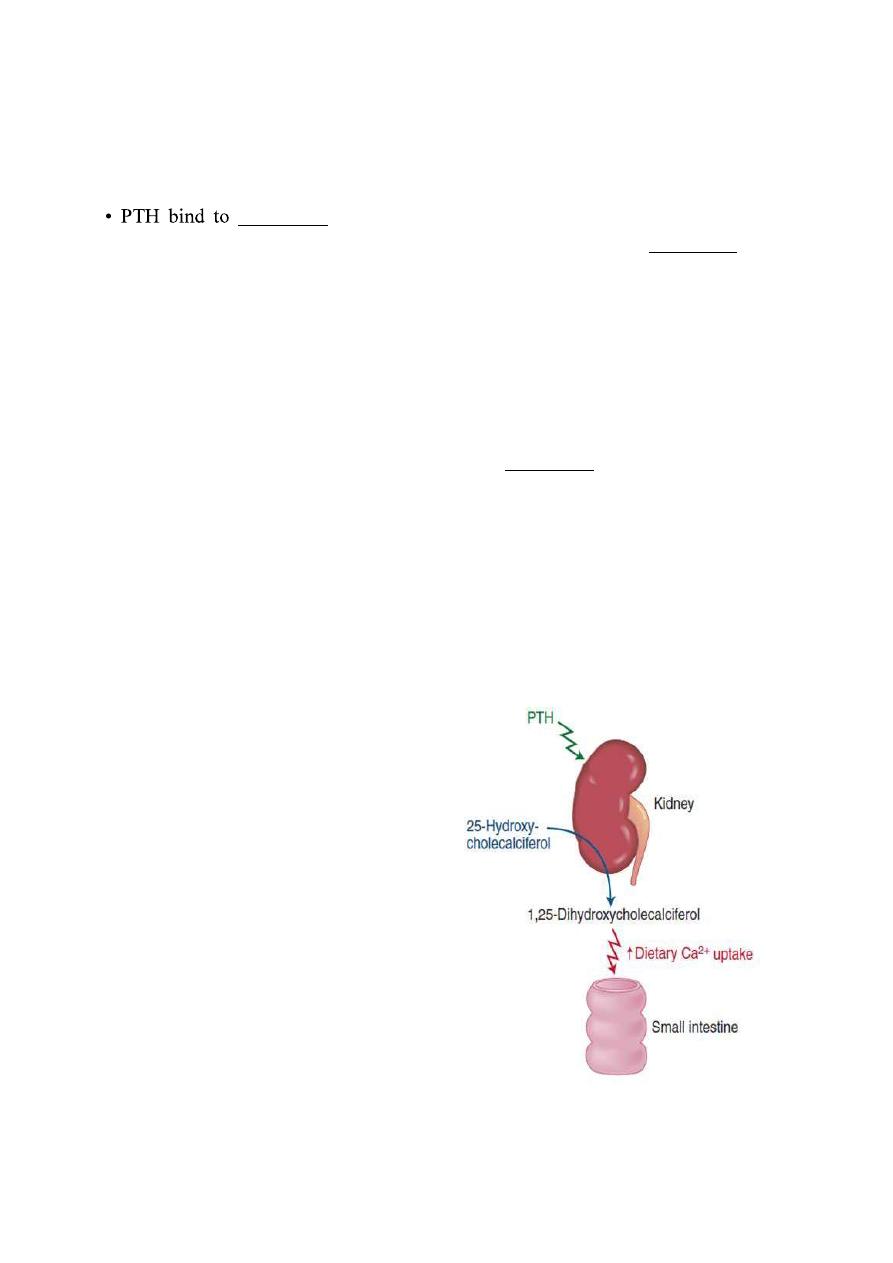
Vitami D (calcitriol)
Vitamin D3 (also called cholecalciferol)
is formed in the skin as a result of
irradiation of 7-dehydrocholesterol, by
ultraviolet rays from the sun. Vitamin D
also provided in the diet. The first step
in the activation of cholecalciferol is to
hydroxylate
it
into
25-
hydroxycholecalciferol, in the liver
which also is inactive. In the kidney, 25-
hydroxycholecalciferol hydroxylated at
the C1 position to produce 1,25-
dihydroxycholecalciferol, which is the
physiologically
active
form.
C1
hydroxylation is catalyzed by the
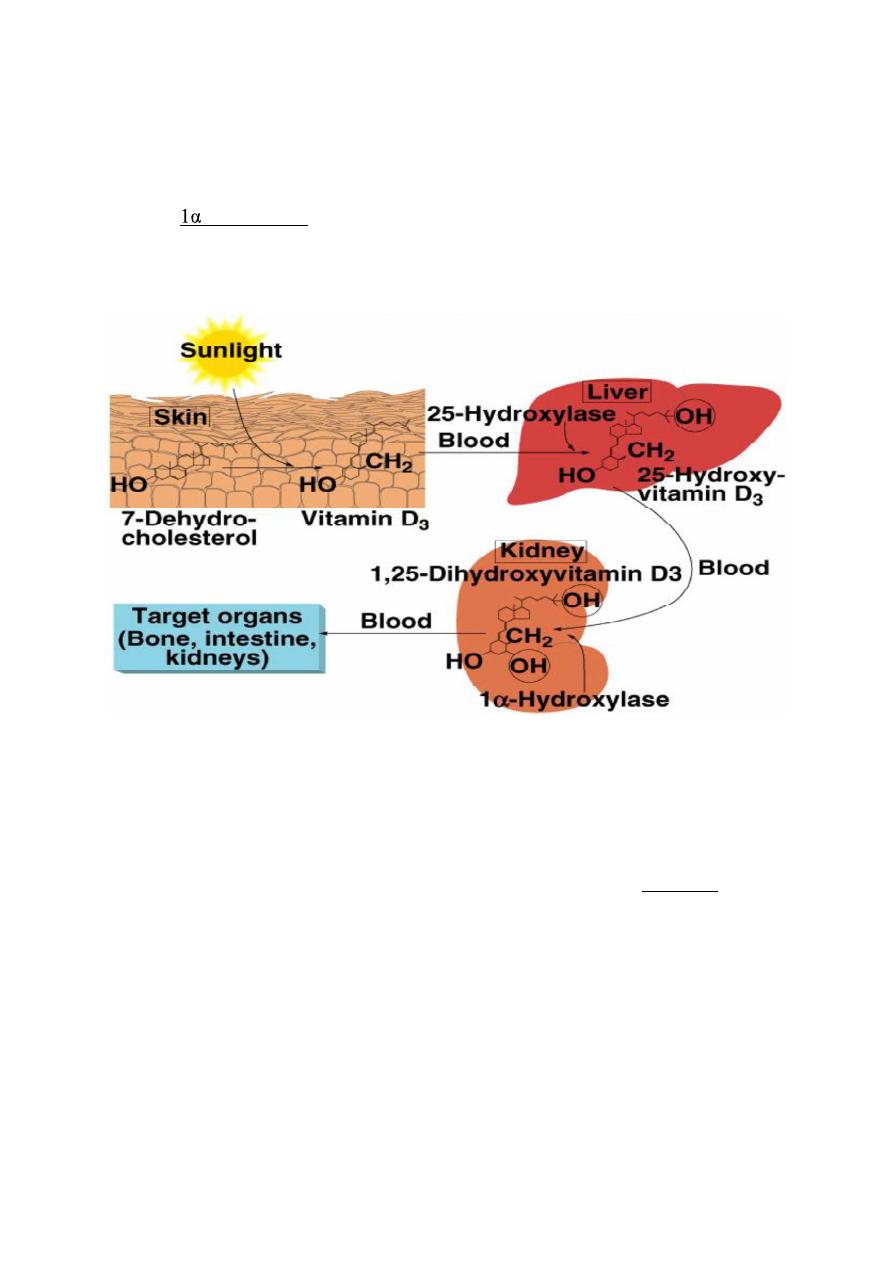
Medical physiology Endocrinology
Dr: ABDULHASAN ALNIYAZI
Ph.D. Medical Physiology
_____________________________________________________________________________________
30
enzyme
-hydroxylase, which is regulated by several factors, including the
plasma Ca
2+
concentration and PTH.
Actions of Calcitriol
Vitamin D acts to raise plasma Ca
2+
and phosphate. Thus, vitamin D promotes
bone deposition. This is accomplished by
1. Calcitriol increases the absorption of Ca
2+
and phosphate by the intestinal
mucosa by increasing the production of the Ca
2+
-binding protein calbindin.
2. Calcitriol enhances PTH's action at the renal distal tubule.
Sex steroids and bone
Medical physiology Endocrinology
Dr: ABDULHASAN ALNIYAZI
Ph.D. Medical Physiology
_____________________________________________________________________________________
31
The sex steroids estradiol (in females) and testosterone (in males) are required for
maintenance of normal bone mass. In postmenopausal women, there is a marked
decline in estradiol levels, which is associated with a loss of bone mass, called
osteoporosis, and a corresponding increase in bone fractures. Osteoporosis is less
common in males due to a smaller and more gradual decline in testosterone levels
with age.
Rickets
A deficiency of vitamin D during childhood causes a bone deformity called rickets,
which is due to the poor mineralization of bone. Classic clinical finding is bowing
of the lower legs.
