
Gynecology 2nd trimester miscarriage Dr.Marwa
Definition
Miscarriage is a spontaneous pregnancy loss before the gestational age of fetal viability
Gestational age of fetal viability
• Viability implies the ability of fetus to survive extra uterine life
• this is generally considered to occur at 24 weeks gestation.
second trimester miscarriage
Is a spontaneous pregnancy loss occurs between 12and 24 weeks gestation
Incidence
—
2
nd
trimester miscarriage constitutes <3% of all pregnancy outcomes.
Etiology
• aetiology underlying late miscarriage varies with gestational age.
• Conditions associated with2nd trimester pregnancy loss overlap those of the 1
st
and third
trismeters.
• The predominant causes of losses at 12–16 weeks are those of first trimester miscarriage
Etiological factors
• Idiopathic
• Fetal
• maternal
Fetal factor
—
The predominant causes of losses at 12–16 weeks are fetal chromosomal and 'structural
anomalies
Maternal factor
—
Anatomical factors:
A- uterine anomaly :
-congenital(septate &bicornuate uterus).
-acquired: Asherman syndrome

B-cervical incompetent
—
Infection
—
Endocrine disease
—
Acute sever illness
—
Thrombophilia
—
Over distension of uterus
—
Abdominal, pelvic surgery
—
amniocentesis
Cervical incompetent
Is an inability of cervix to retain pregnancy in abscence of uterine contraction or labour.
Etiology of cervical incompetent
—
Congenital :Congenital exposure to DES in utero , connective tissue disorders
—
Acquired:(dilatation and curettage, conization, cauterization, or amputation,cx laceration
following SVD
Clinical presentation
Cx dilatationand effacement in the 2
nd
trimester with fetal membrane visible at or beyond the
ext.osin absence of contraction
Dignosis
—
before pregnancy:
-Historical features:
1. Hx of tow or more 2
nd
trimester pregnancy loss
2. Hx of pregnancy loss at an earlier gestational age
3. HX of painless cx dilatation up to4-6 cm
4. Absence of clinical finding consistent with placenta abruptio
5. Hx of cx trauma
Investigation
—
Before pregnancy
1. Easily passing of 8 Hegar dilator through cx with no resistence
2. Funneling of IO on HSG
—
During pregnancy:TVU of cx:
1. Short cx: <25mm before 24 weeks
2. Funneling of membrane through IO
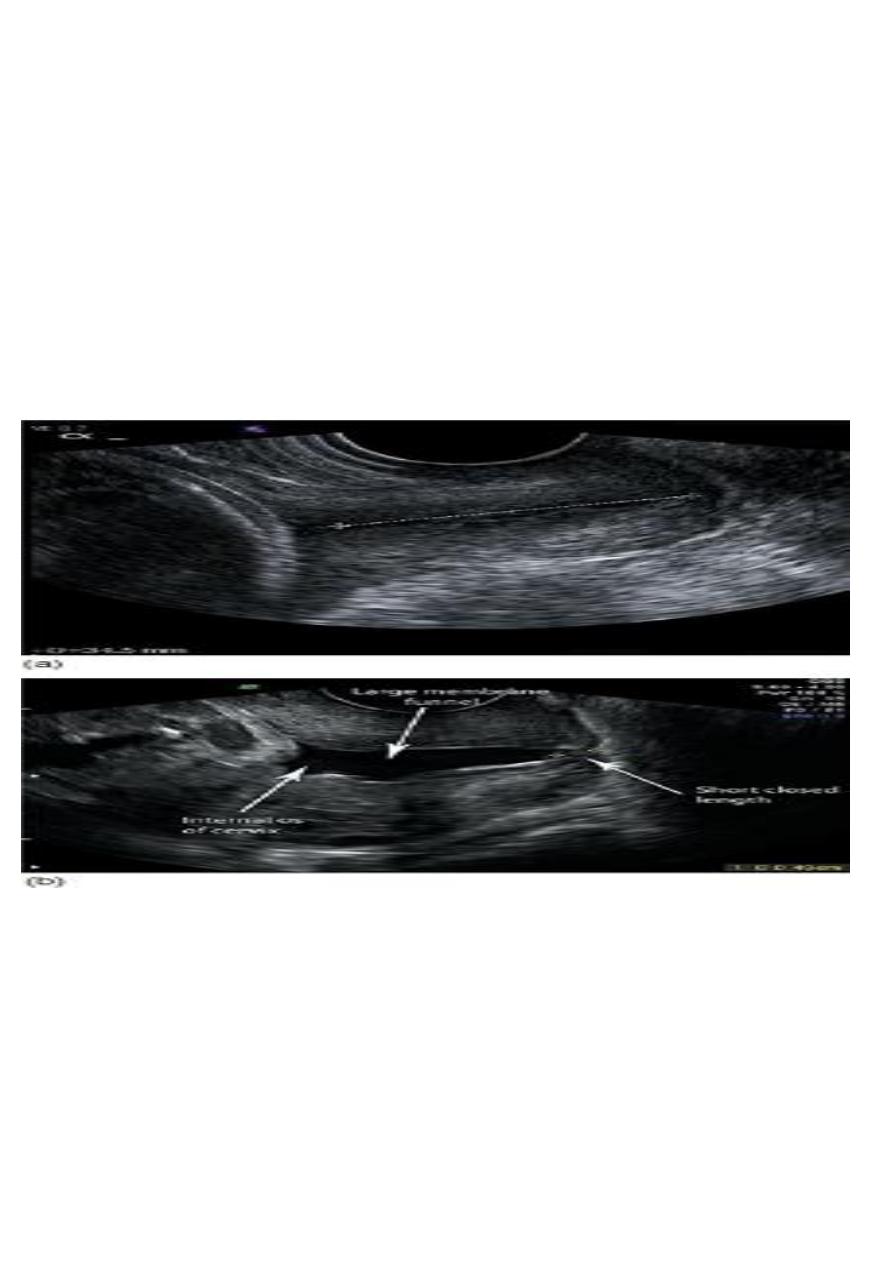
Normal CX(a) shortcx(b)
Treatment approach
Cervical cerclage
surgically reinforces a weak cervix by some type of purse-string suturing
Types according to indication
1. Prophylactic cx cerclage
cerclage should be offered to women with three or more previous preterm births and/or
second-trimester losses
Women with a history of one or more spontaneous mid-trimester losses or preterm births who
are undergoing transvaginal sonographic surveillance of cervical length should be offered an
cerclage if the cervix is 25 mm or less and before 24 weeks of gestation.
2-Rescue cx cerclage
Insertion of cerclage as a salvage measure in the case of premature cervical dilatation with
exposed fetal membranes in the vagina in absence of ut.contraction.
Types according to surgical approach
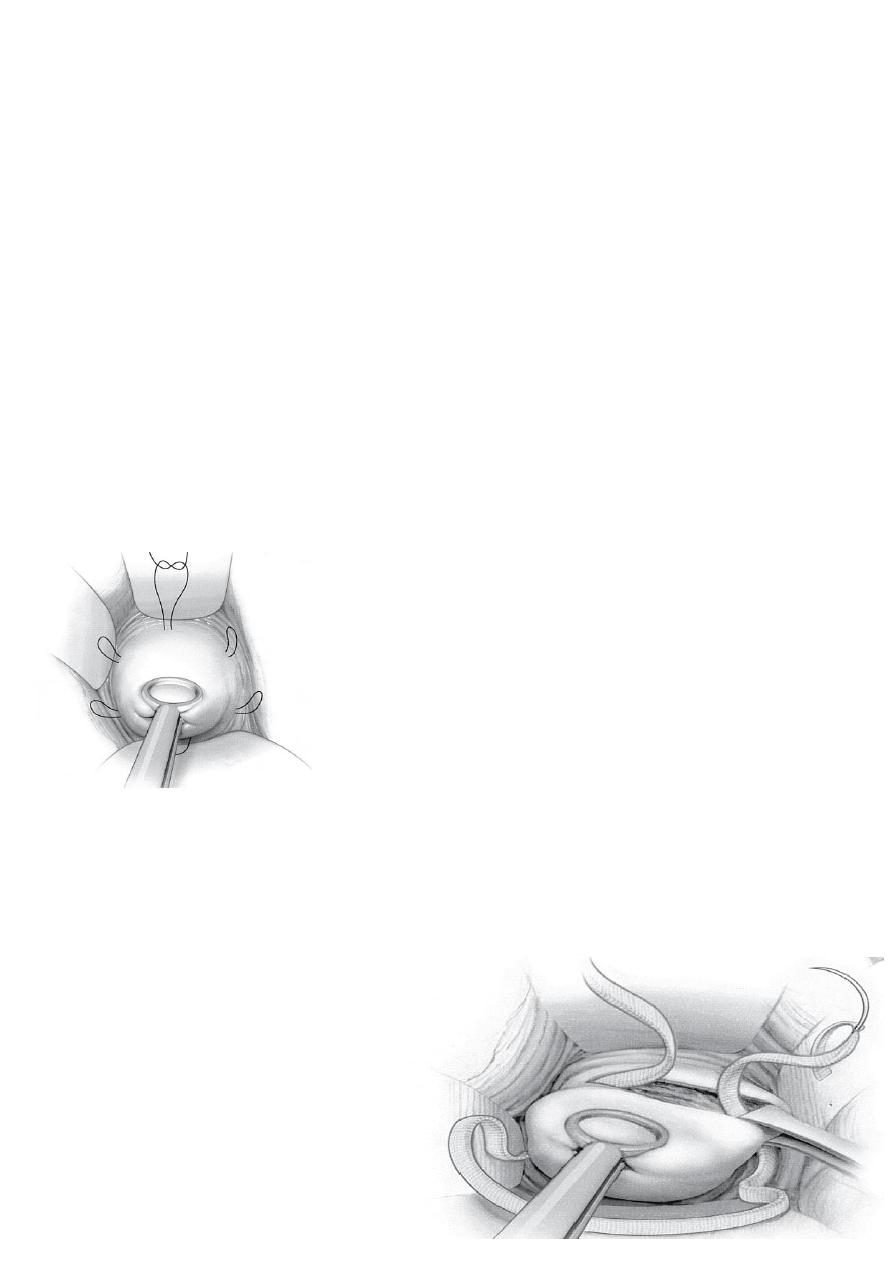
1-Transvaginal cerclage (McDonald)
2- High transvaginal cerclage (Shirodkar)
3- Transabdominal cerclage
1-Transvaginal cerclage (McDonald)
A transvaginal purse-string suture placed at the cervicovaginal junction, without bladder
mobilisation.
High transvaginal cerclage (Shirodkar)
A transvaginal purse-string suture
placed following bladder mobilisation, to
allow insertion above the level of
the cardinal ligaments.

3- Transabdominal cerclage
A suture performed via a laparotomy or laparoscopy, placing the suture at the cervicoisthmic
junction.
Time of application
• Transabdominal cerclage can be performed preconceptually or in early pregnancy.
• Trans vaginal cerclage at 14-16 weeks
Time of removing
• A transvaginal cervical cerclage should be removed :
• between 36+1 and 37+0 weeks
• Labour
• PROM
• IUD
All women with a transabdominal cerclage require delivery by caesarean section, and the
abdominalsuture may be left in place following delivery.
Contraindications for cx cerclage
• active preterm labour
• clinical evidence of chorioamnionitis
• continuing vaginal bleeding
• PPROM
• evidence of fetal compromise
• lethal fetal defect
• fetal death.
Complications of cx cerclage
-1-during insertion of cervical cerclage.
small risk of:
• intraoperative bladder damage,
• cervical trauma,
• membrane rupture and bleeding
2- Shirodkar cerclage usually requires anaesthesia for removal and therefore carries the risk of
anadditional anaesthetic.
3- Cervical cerclage may be associated with a risk of cervical laceration/trauma if there is
spontaneouslabour with the suture in place.
