MANDIBULAR FRACTURES
INCIDENCEThe mandible is the second most commonly fractured part of the maxillofacial skeleton because of its position and prominence. The location and pattern of the fractures are determined by the mechanism of injury and the direction of the vector of the force. In addition to this, the patient’s age, the presence of teeth, and the physical properties of the causing agent also have a direct effect on the characteristics of the resulting injury.
Mandibular fractures are among the most common bone injuries in facial trauma, and they account for 23–97% of all facial fractures.
The most common causes of mandibular fractures are car and motorbike accidents (52%), severe assaults (25%), and falls (13%).
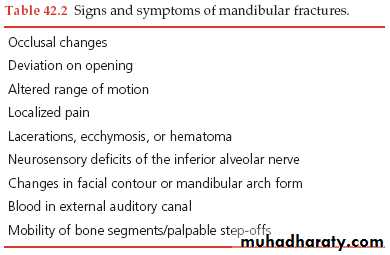
CLINICAL PRESENTATION
— pain and swelling— deranged occlusion
— paraesthesia in distribution area of inferior alveolar nerve
— floor of mouth haematoma
CLINICAL INVESTIGATION
* Tongue blade test* Palpation
Radiographic examination
When an isolated mandibular fracture is suspected, the routine radiographic assessment may consist of a panoramic radiograph and one additional postero-anterior view of the mandible, usually an open-mouth Towne’s radiograph.Additional periapical or occlusal radiographs are often helpful in viewing specific areas of concern in more detail, especially when dental or alveolar fractures are suspected.
CLASSIFICATION
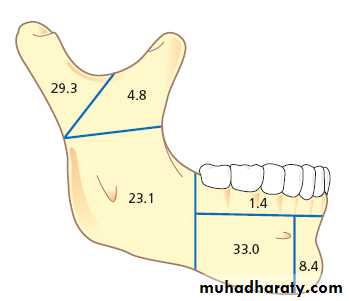
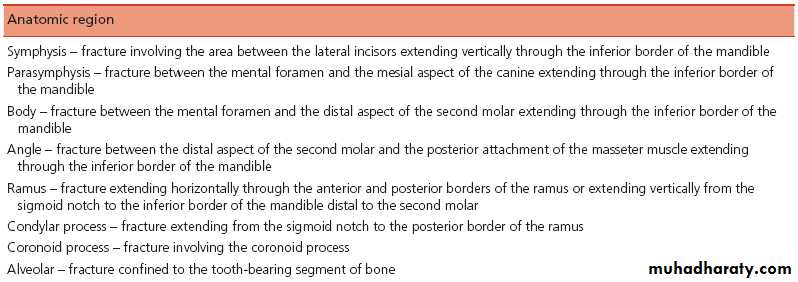
A. Anatomic LocationCommon sites of fracture in the mandible
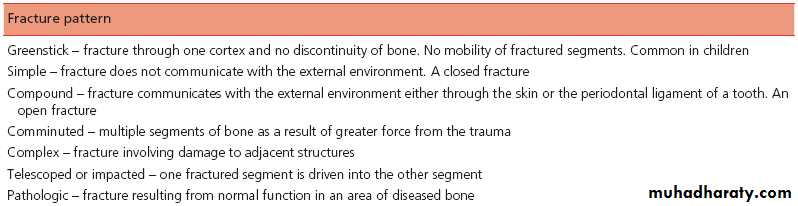
B. Pattern of Fracture
• Simple fracture:............• Compound fracture:.............
• Greenstick fracture: This type of fracture frequently occurs in children and involves incomplete loss of continuity of the bone. Usually one cortex is fractured and the other is bent, leading to
distortion without complete section. There is no mobility between the proximal and distal fragments.
• Comminuted fractures:...........
• Complex or complicated fracture:..............
• Telescoped or impacted fracture: is rarely seen in the mandible, but it implies that one bony fragment is forcibly driven into the other. This type of injury must be disimpacted
before clinical movement between the fragments is detectable.
• Indirect fracture:.............
• Pathologic fracture
* Displaced fracture: Displacement is defined as
movement of the condylar fragment in relation to the mandibular segment with movement at the fracture site.* Dislocated fracture: A dislocation occurs when the head of the condyle moves in such a way that it no longer articulates with the glenoid fossa. When this is associated with a fracture of the condyle, it is termed a fracture dislocation.
* Special situations: like grossly comminuted fractures or fractures involving adjacent bony structures, such as the glenoid fossa or tympanic plate; open or compound fractures; and fractures in which a combination of several different types of fractures exist....gunshot injuries.
BIOMECHANICAL CONSIDERATIONS
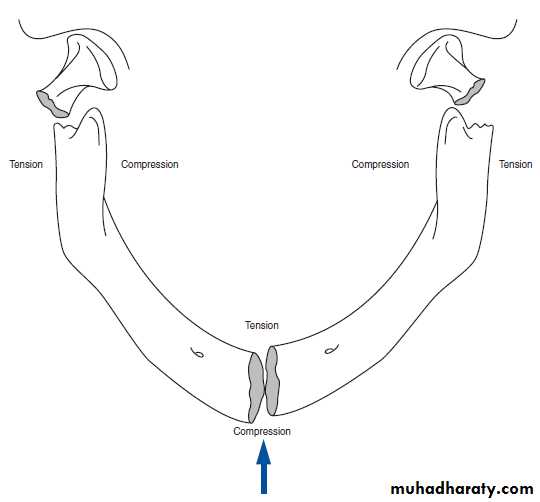
In response to loading, the mandible is
similar to an arch because it distributes the
force of impact throughout its length
When a force is directed along the parasymphysis-body region of the mandible, compressive strain develops along the buccal aspect, whereas tensile strain develops along the lingual aspect.
This produces a fracture that begins in the lingual region and spreads toward the buccal aspect.
At this point, tension develops along the lateral aspect of the contralateral condylar neck, and a fracture occurs. If greater force is applied to the parasymphysis- body region, not only will tension develop along the contralateral condylar neck leading to fracture in this area, but continued medial movement of the smaller ipsilateral mandibular segment will lead to bending and tension forces along the lateral aspect and subsequent fracture of the condylar process on the ipsilateral side.
MODIFYING FACTORS
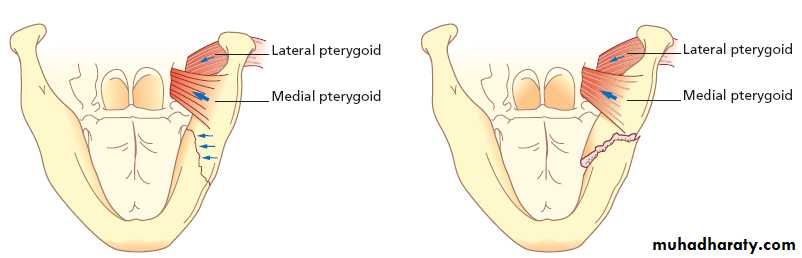
* The presence of specific teeth, particularly impacted third molars, has been shown to markedly affect the incidence of mandibular fractures.* The relative degree of mandibular opening at the time of impact plays an important role in the type of fracture that occurs. Not only is the incidence of fracture higher when the mouth is open, but the level of fracture varies with degree of opening. When the mouth is opened, the fractures tend to be located more in the condylar neck or condylar head region, whereas when it is closed, fractures are in the subcondylar area.
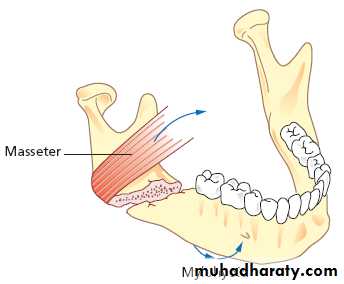
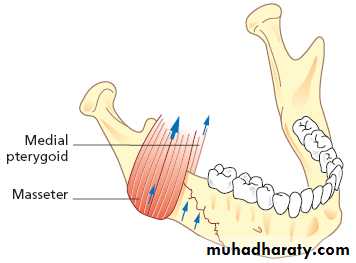
A fracture is favorable in a horizontal plane if the fracture resists the superior pull of the proximal fracture segment by the masseter and temporalis muscles. A fracture is favorable in the vertical plane if the fracture resists the medial pull of the proximal segment by the medial pterygoid muscle.
Goals of mandibular fracture repair
Some patients may present with a mandibular fracture yet require no treatment. In these cases the occlusion is stable, the fracture is non-displaced, a favorable fracture pattern exists, and the patient is motivated to be compliant. Management in these rare instances consists of close observation, a liquid diet, and limited physical activity. The surgeon must remain prepared to change the treatment plan should any change in the clinical situation arise.CONSERVATIVE TREATMENT
Indications for closed reduction techniques of mandibular fractures.
Closed reduction
Pediatric patients can be placed into IMF with circummandibular and piriform rim wires.
INTERMAXILLARY FIXATIONFixation of the mandible and maxilla together (mandibular-maxillary fixation) is commonly referred to as IMF. The teeth are used to check the correct reduction of the fracture and then used for fixation. The occlusion will, therefore, be accurately re-established and the technique is straightforward, although it would be described as producing non-rigid fixation. IMF may be achieved through a variety of means:
* Direct interdental wiring. Simple rapid immobilisation
of jaws is achieved with stainless steel wire placed aboutthe neck of tooth and the two ends twisted together to produce
a tail, which in turn can be twisted with another tail
of the opposing arch to effect IMF. Rarely used today.
* Eyelet wiring. Pre-prepared wires with loops, to facilitate
placement of separate IMF tie wires, are applied topairs of teeth.
* Arch bars. These may be commercially produced bars
that are cut to length and bent to shape or custom-madearch bars can be prepared for the individual patient
from dental impressions. The bars have cleats that facilitate
IMF tie wires. They also allow the ready placement
of elastic traction should that be required, which is not
possible with direct interdental wiring or eyelets. The
bars are fixed to the teeth by interdental wiring.
* Bonded brackets. Brackets bonded to teeth result in
less soft tissue trauma; such trauma can potentially be apostoperative problem with dental wires and arch bars.
* Screws.
IMF IN EDENTULOUS
There have been several methods to restore occlusion to edentulous patients which include Gunning’s splint and the application of an arch bar into the denture. Unfortunately, these 2 techniques are very time consuming and require laboratory procedures to apply these to the dentures.Skeletal anchorage system (SAS), which is a simple and relatively easy method to conduct.
The SAS provides anchorage to both the bone and the maxillo-mandibular fixation and also can be performed without severe modification of the patient’s denture.
After making holes in the dentures, the dentures are adapted to the jaws of the patient. The SAS screws can be placed into the holes providing denture stability and the anchorage for the intermaxillary fixation. Once the fracture treatments are completed the patients may continue to use their dentures, which only require minimal repairs after the procedure.
Disadvantages
* Dependent on the patient’s denture conditions. In the case of old dentures, the attrition of the artificial teeth may be severe and also may not be able to provide stable occlusion.* Some patients having excessive alveolar bone loss may also have problems with the angulation of the SAS screws.
* In some cases, the denture flange may not be able to cover the alveolar bone, such that applying the SAS system will be difficult.
* For patients with excessive alveolar bone loss, placing the SAS screws can prove to be difficult because of the proximity of the alveolar nerve canal and the screw, which can result in damage to the nerve.
DISADVANTAGES OF IMF FIXATION
• The airway is partially compromised and is at increased risk in the event of postoperative swelling, regurgitation or vomiting. Opioid analgesia and other central nervous system depressants should be avoided to minimise respiratory depression and nausea.
• There is reduced tidal volume.
• Patients are unable to take solid diet. Patients should receive 3 litres of fluid and 2500 calories each day, and some encouragement will be required initially to achieve this when a patient is in IMF.• It is difficult to maintain good oral hygiene. Tooth brushing of lingual aspects of teeth is not possible; therefore, the patient must compensate with copious mouthrinsing and the use of a chlorhexidine rinse.
• There is poor patient tolerance of IMF fixation.
• Post-treatment stiffness of the temporomandibular joint can occur and there is a risk of ankylosis.• Inhalers for asthma therapy are difficult to use.
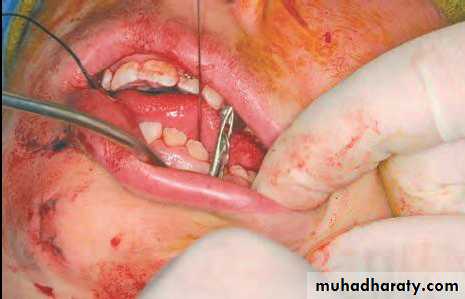
EXTERNAL FIXATOROpen reduction with internal fixation implies surgical exposure, visualization, and manipulation with the placement of a stabilization device directly along the bone segments involved in the fracture.
Open reduction
Indications for open reduction techniques of mandibular fractures
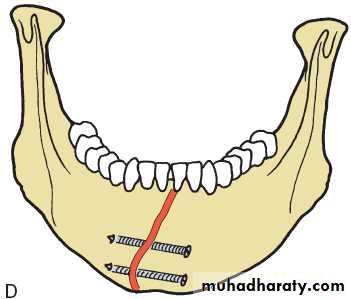
Simple wiring technique.Figure-of-eight wire.
Transosseous circum-mandibular wire
DIRECT INTEROSSEOUS WIRING
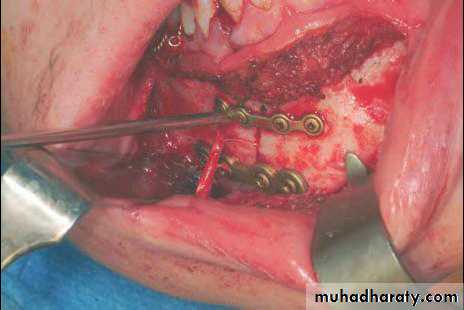
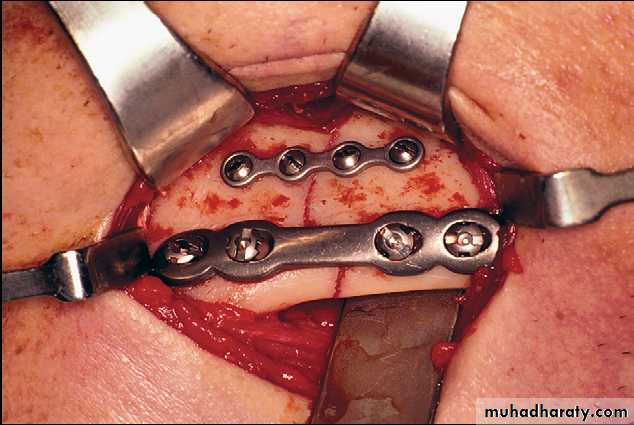
Bone plates
Bone screws
CONDYLAR FRACTURES
* Fractures of the mandibular condyle are common and account for 9% to 45% of all mandibular fractures.* Most cases can be managed conservatively.
RESULTS OF CONSERVATIVE TREATMENT
Mandibular movement is increased at 6 months despite the slight disturbance in lateral excursion to the nonfractured side and the presence of deviation on mouth opening. Occlusal area and occlusal force improve at 6 months.Techniques of open treatment of condylar fractures.
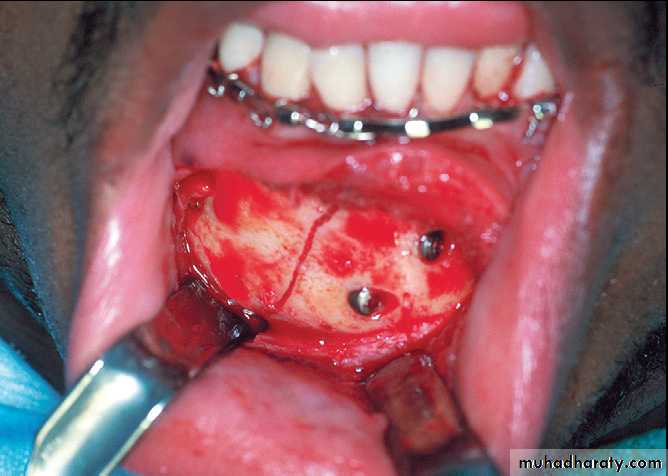
* Miniplate fixation is an established technique. However, a risk of complications is associated with the surgical approach. After extraoral (preauricular, retromandibular, and submandibular) approaches, salivary fistulas, visible scars, and temporary or permanent facial nerve damage have been reported as complications.* Transoral approach.
The reduction and fixation of condylar fractures using
extra- and intraoral approaches is a technically demandingsurgical procedure, and miniplate fractures occur in up to 35% of the reported cases. Nevertheless, good functional results have been achieved after open reduction and fixation
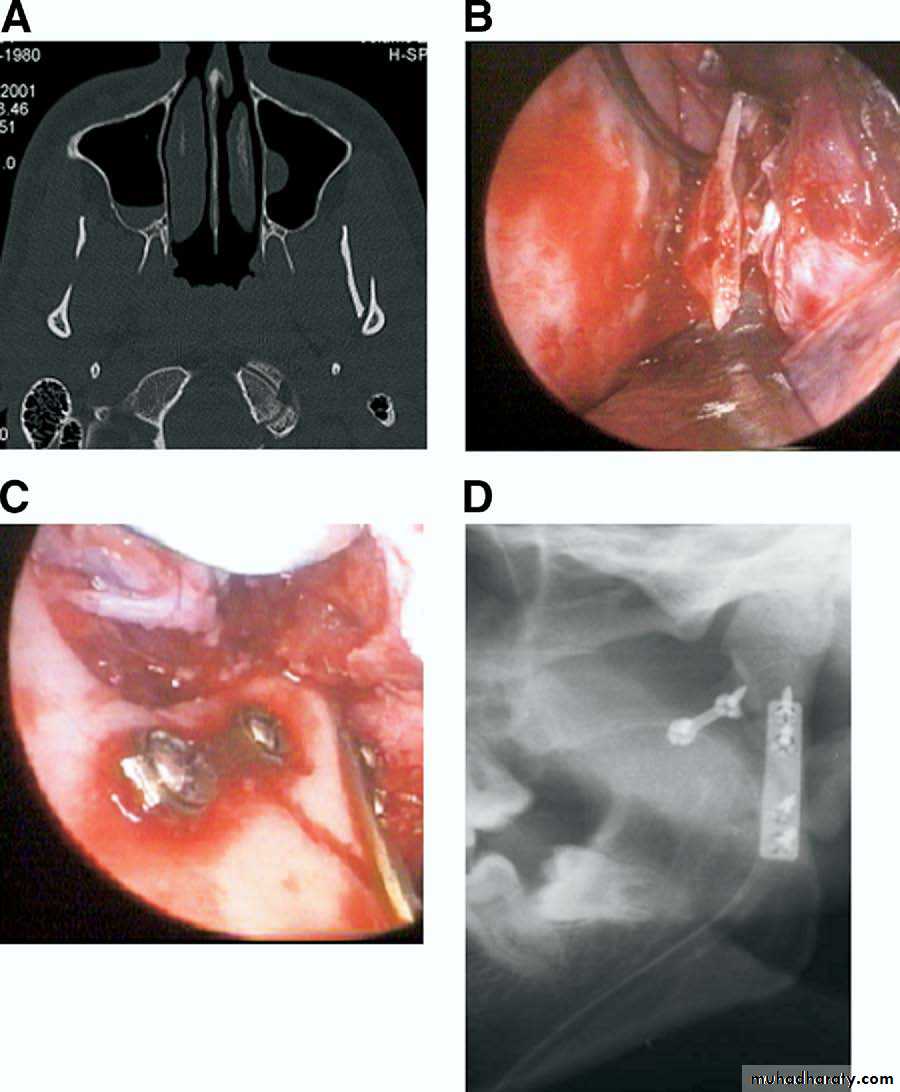
* Endoscopic reduction
The endoscopically assisted approach for open reduction and miniplate fixation of condylar mandibular fractures is a technique that allows fracture treatment with a limited transoral incision. Using an endoscope, superior visibility in areas of limited exposure can be obtained. In conjunction with the transoral approach, the scars are invisible, the risk of facial nerve damage is minimal, and, with subperiosteal preparation, the masseter muscle is not dissected. However, the procedure can be time-consuming. A steep learning curve for this technique has been reported.Open or closed ??
Fractures with a deviation of 10° to 45°,or a shortening of the ascending ramus 2 mm,
should be treated with ORIF,
irrespective of level of the fracture.
Management of teeth in the line of the fracture
1. Teeth grossly loosened, showing evidence of periapical pathology or significant periodontal disease2. Partially erupted third molars with pericoronitis or associated cyst
3. Teeth that prevent reduction of fractures
4. Teeth with fractured roots
5. Teeth with exposed root apices or entire root surface from the apex to the gingival margin
6. An excessive delay from the time of fracture to definite treatment