Infertility
Dr.Nadia Mudher Al-Hilli
FICOG
Department of Obs&Gyn
College of Medicine
University of babylon
Objectives
•
Know the definition of infertility
•
Understand what could cause infertility
•
Learn how to assess a couple with
infertility
•
Know the treatment options available for
infertility

Infertility
: failure to conceive within one year of
unprotected regular sexual intercourse.
Primary
in couples that have never conceived
together, or
secondary
in couples that have
previously conceived together (although either
partner may have conceived in a different
relationship, which requires further elucidation)
Infertility affects about 15 % of couples.
Male & female factors each account for 30% of cases
Male & female factors combined cause 20%
The remaining 20% of cases the cause is unknown
( unexplained)
Natural conception
A healthy couple having frequent intercourse have an
18
–20% chance of conceiving in a single menstrual
cycle.
a cumulative increase in pregnancy rates over time.
Within 6 months 70% of couples will have conceived,
after 12 months 80% and after 24 months 90%.
The most important factor affecting fertility is female
age, which is related to a decline in the quality and
quantity of eggs, fertility tends to fall sharply over the
age of 36, with a further dip after the age of 40.
Male age is also an important; semen quality fall in
men over the age of 50, while frequency of
intercourse tends to fall in men over the age of 40.
Factors that reduce the chance of
spontaneous conception:
age of the female >35 years.
Duration of infertility more than 3 years.
Low coital frequency.
No previous pregnancy.
Smoking.
Body mass index out side the range 19-29
kg/m
2
in women.
Low number of motile healthy sperms.
Drugs : NSAIDs, chemotherapy.
Causes of infertility
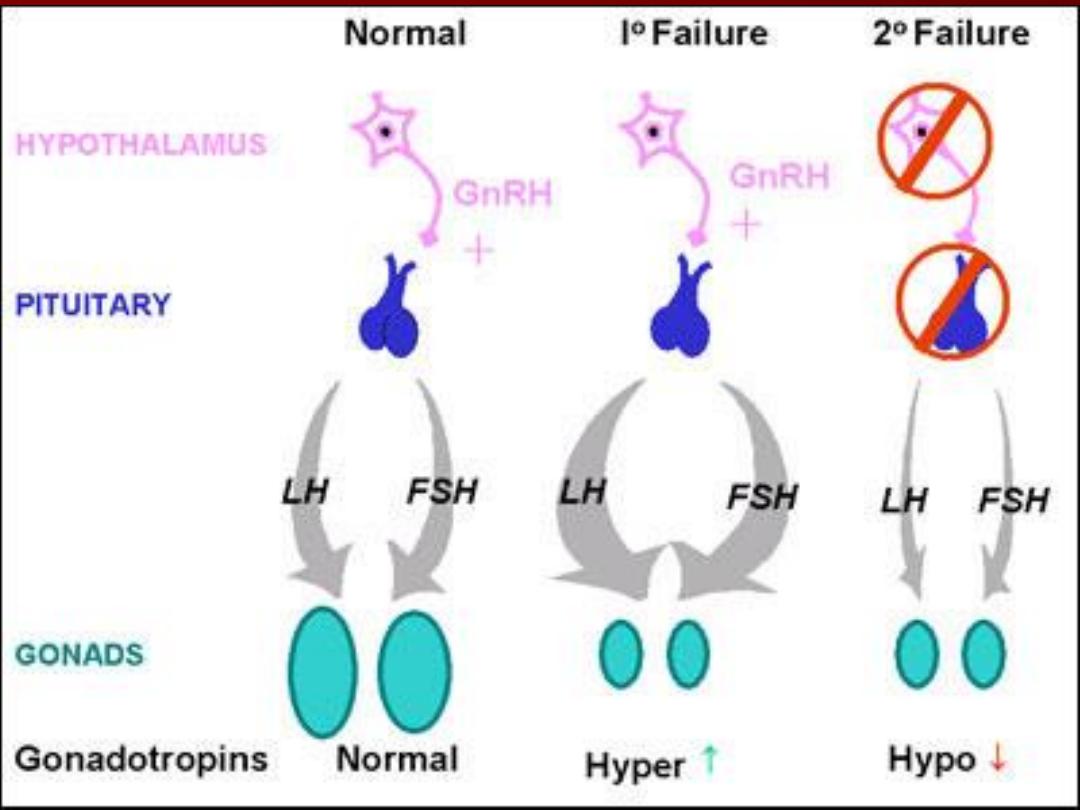
Ovulatory disorders: defect in the hypothalamus,
pituitary or the ovary.
WHO Classification:
Group
I
:
hypothalamic
pituitary
failure
(Hypogonadotrophic hypogonadism): conditions
cause failure of pituitary gland to produce
gonadotrophins & Factors that affect the
pulsatile release of GnRH.
•
Group II : Ovulation Dysfunction: polycystic
ovary syndrome (PCOS)
•
Women with PCOS who suffer from
oligomenorrhoea due to anovolution may
require treatment.
•
hormonal treatments taken by women to
regulate their periods or help hirsutism may
be incompatible with getting pregnant
Group III : Hypergonadotrophic
hypogonadism: Premature ovarian failure
when the ovaries fail before the age of 40
years.
Endocrine disorders: hypo &
hyperthyroidim & hyperprolactiemia
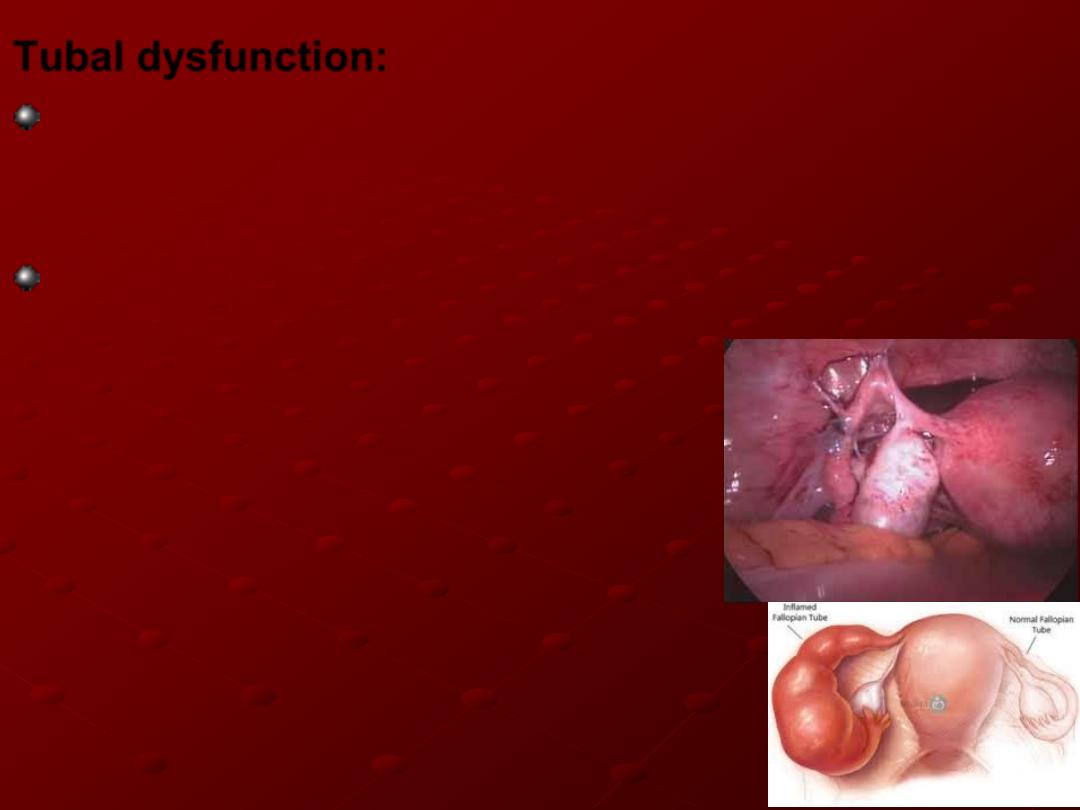
Tubal dysfunction:
Normal tubal function requires both patency & a
healthy anatomy and physiology for gamete and
embryo transport.
Tubal damage: blockage is usually associated with
inflammatory processes in the pelvis
e.g, pelvic infection, endometriosis or
pelvic surgery. Chlamydial infections
in particular can produce significant
degrees of tubal damage, resulting in
a hydrosalpinx
– a blocked Fallopian
tube, with a thickened wall, flattened
epithelial mucosa and peritubal adhesions
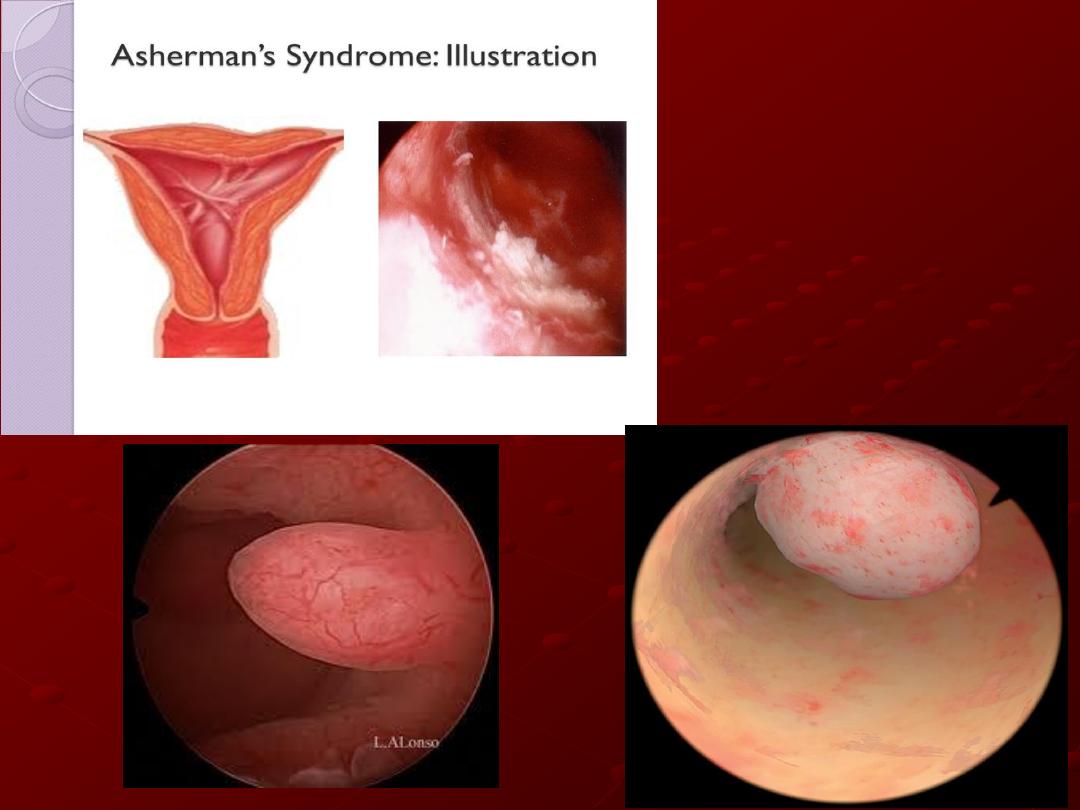
Uterine problems (Disorders of
implantation):
intramural fibroids larger than 5 cm may
effect fertility
defects related to endometrial
development or the production of growth &
adhesion molecules or submucous fibroid,
or endometrial polyps.
Male factor:
Disorders of spermatogenesis.
Impaired sperm transport.
Ejaculatory dysfunction.
Immunological & infective factors.
Management:
History & examination:
medical & surgical history. Drug history,
life style coital frequency & any difficulties
of coitus.
menstrual cycle
cervical smear, body weight & blood
pressure.
Examination of both partners is essential
to ensure normal reproductive organs.

Investigations:
assessment of ovulation, Fallopian tube
patency, uterine cavity & seminal fluid
analysis.
Early follicular phase (day 2-5 of menstrual
cycle) measurement of FSH, LH &
estradiole to assess ovarian function.
Mid-luteal progesterone level to confirm
ovulation.
Marker of ovarian reserve :
Ovarian reserve declines after the age of 35 in an
average healthy woman, or at an earlier age due to
genetic predisposition, surgery or following exposure
to toxins, such as chemotherapy
.
•
anti-Müllerian hormone (AMH) is produced by
the granulosa cells. It reflect the size of follicular
pool. Need to be measured in pt with advanced
age or conditions affecting follicle number
•
Antral Follicle count: measured by TV US, (<4
predicting low response, >16 high response).
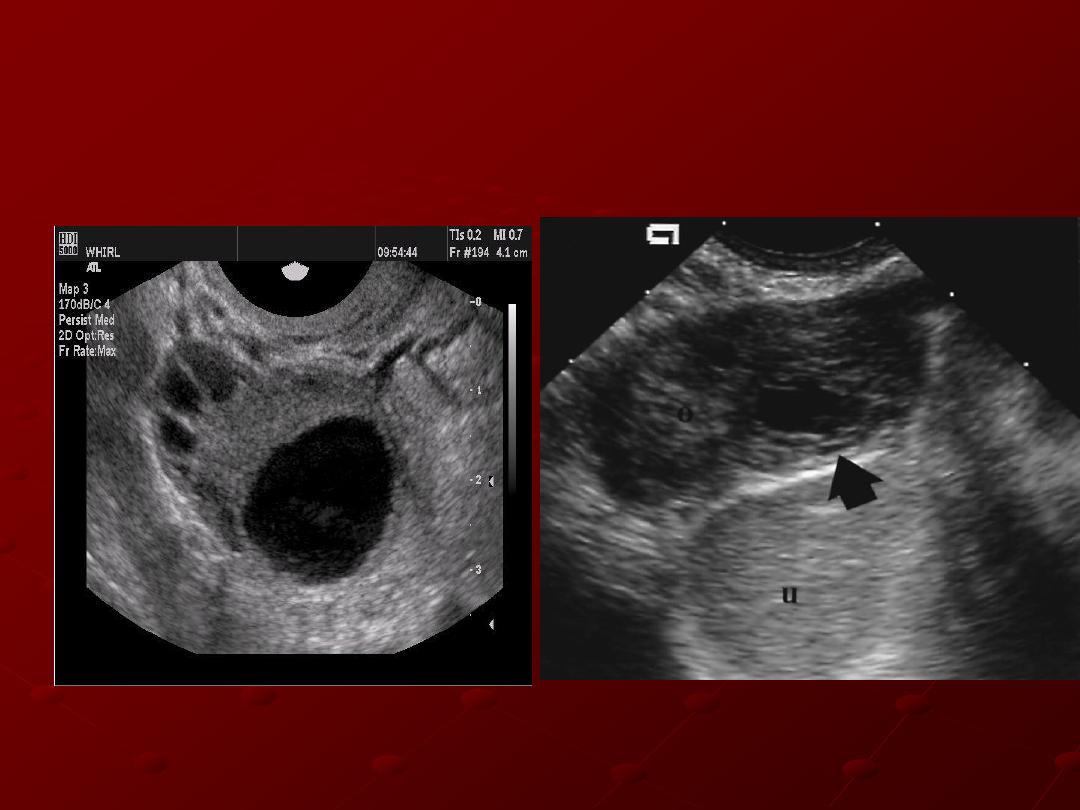
Serial follicle tracking by transvaginal ultrasound
(TV US) in the midcycle can be used to confirm
ovulation.
Assessment of tubal patency: in addition to
assessing uterine cavity
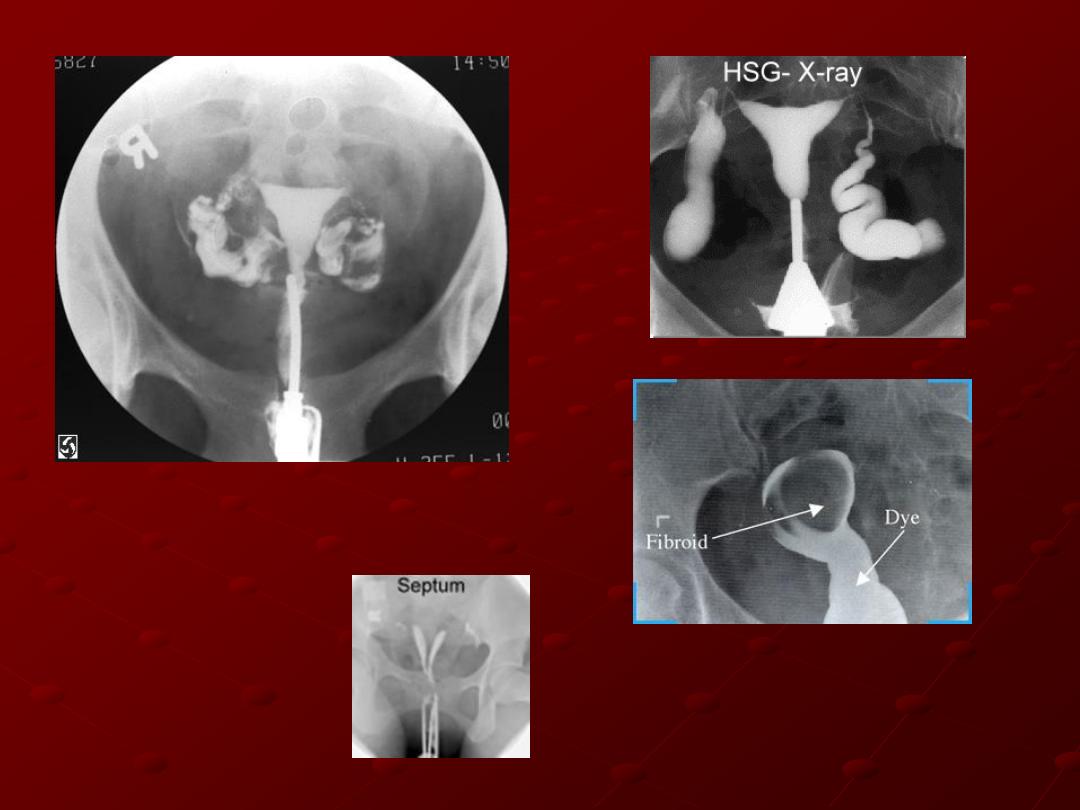
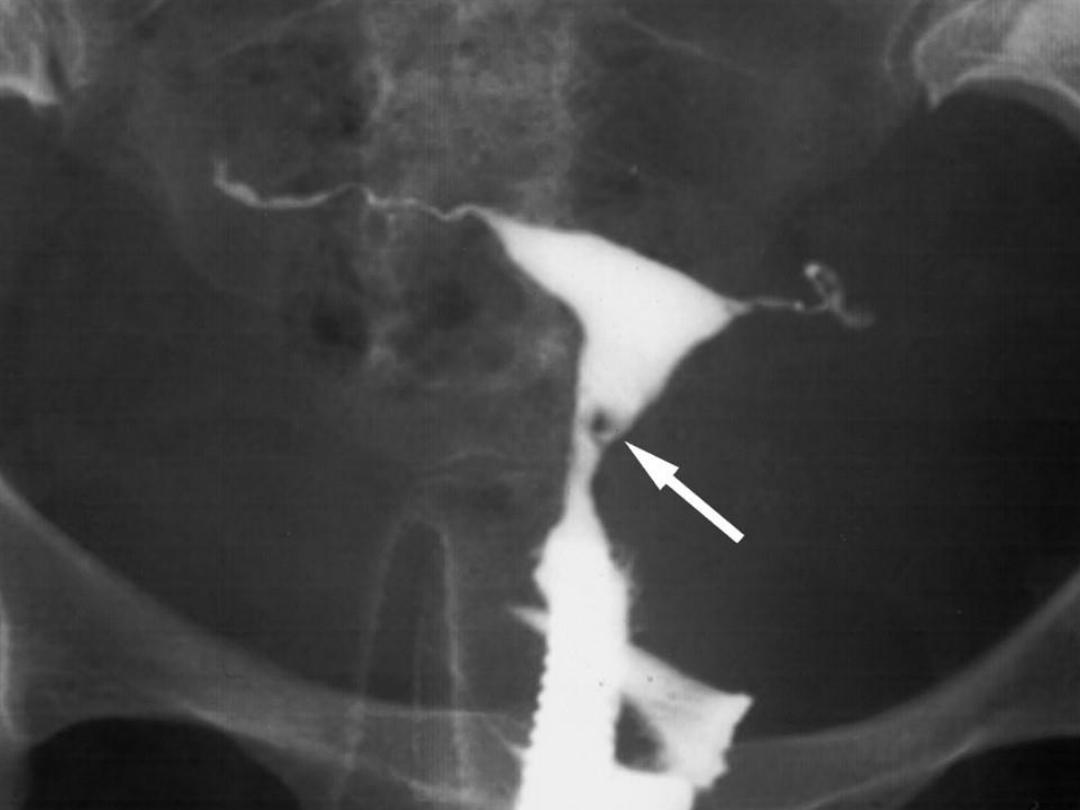
Hysterosalpingogram: offered for women
who are not known to have comorbidities
(such as pelvic inflammatory disease,
previous ectopic pregnancy or
endometriosis)
o
When the dye flows freely into the
abdominal cavity it confirms patency.
o
If the dye spill appear to be loculated or no
spillage, peritubal adhesion or obstruction
are likely.
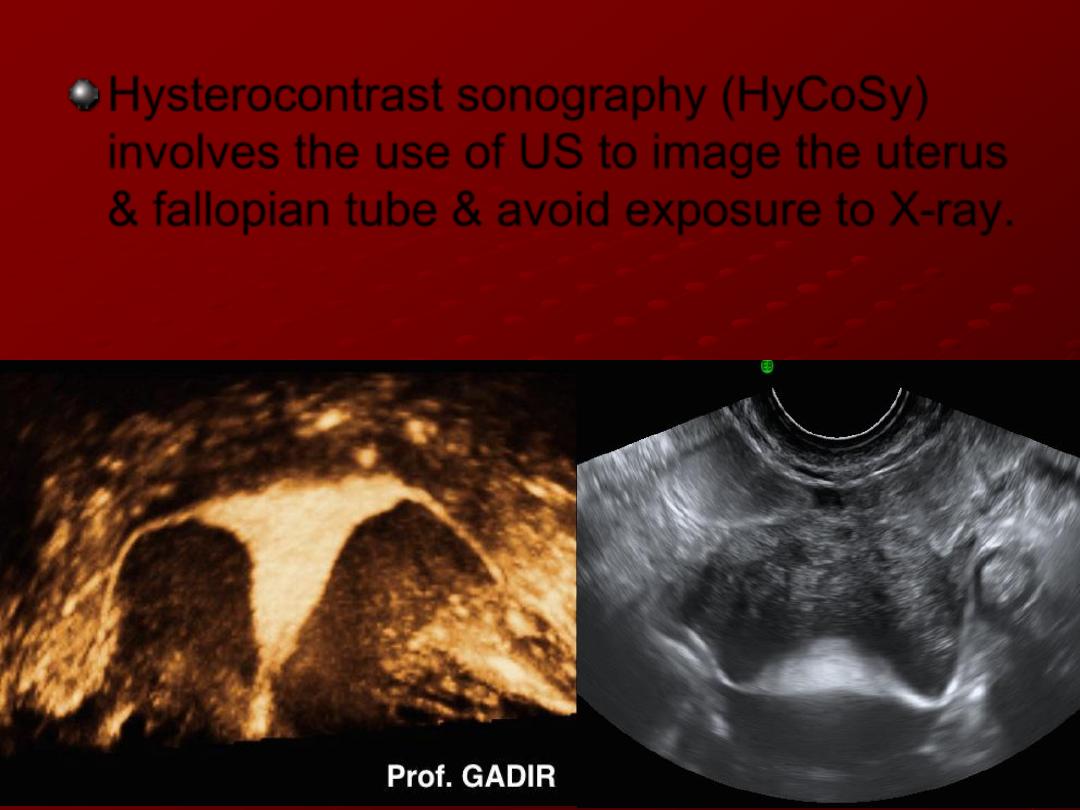
Hysterocontrast sonography (HyCoSy)
involves the use of US to image the uterus
& fallopian tube & avoid exposure to X-ray.
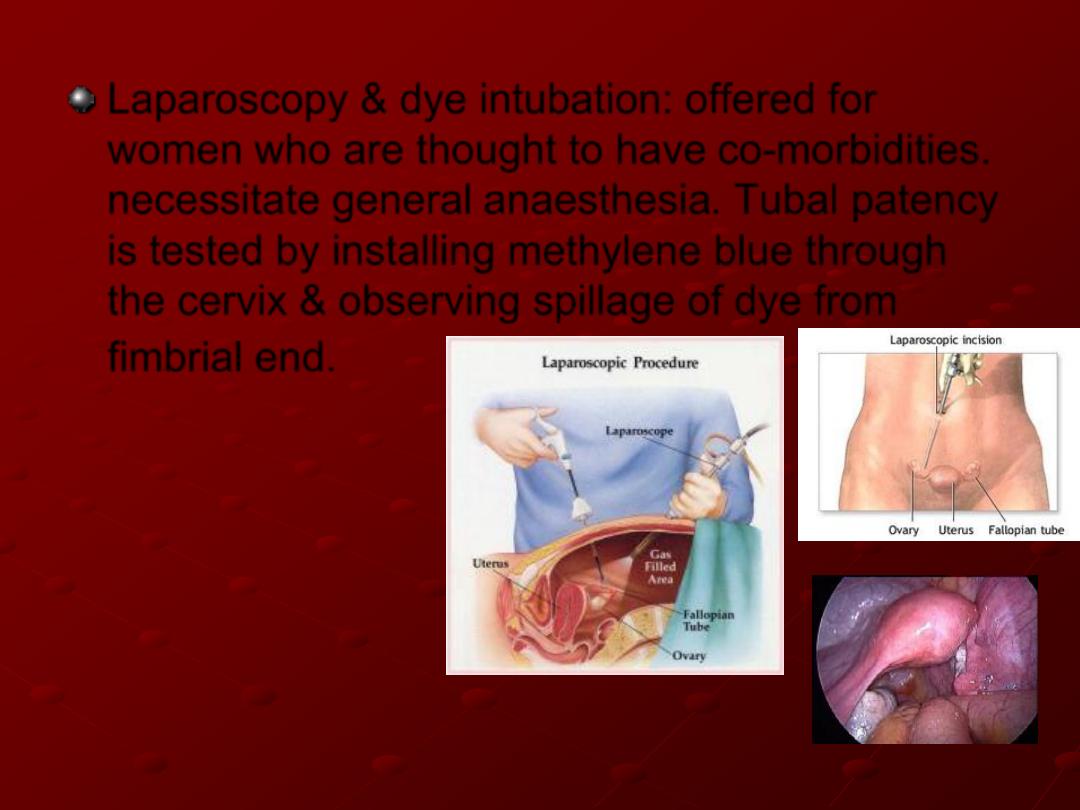
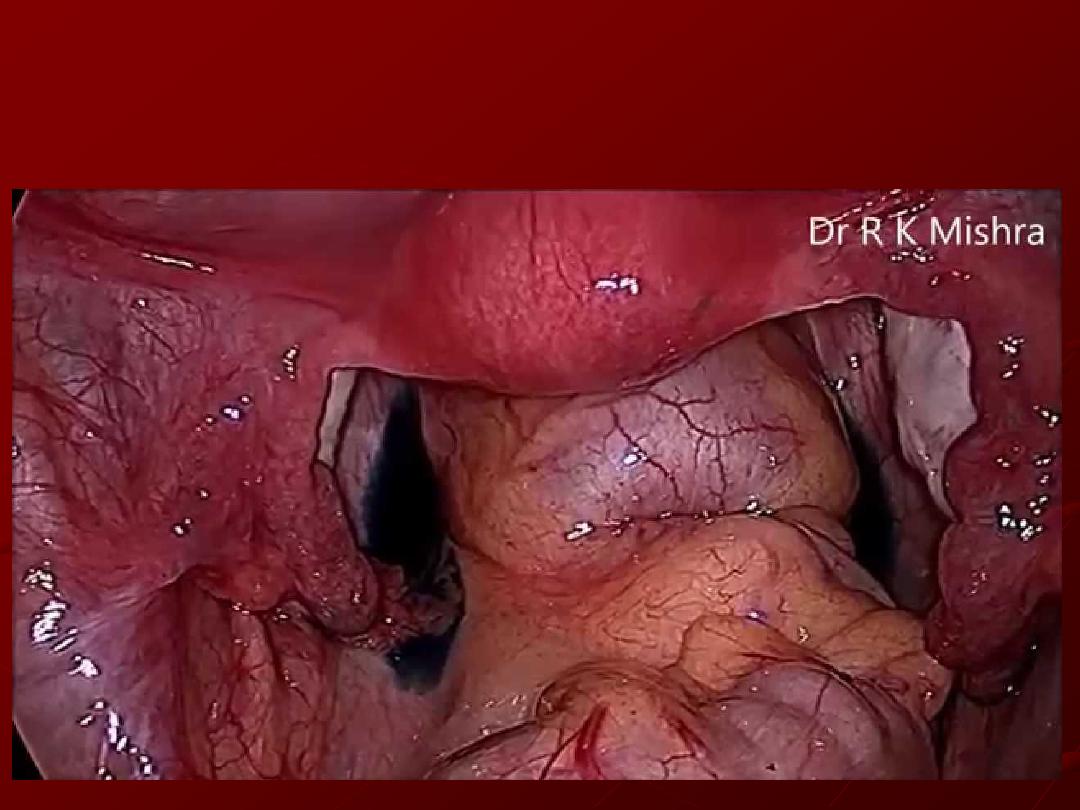
Laparoscopy & dye intubation: offered for
women who are thought to have co-morbidities.
necessitate general anaesthesia. Tubal patency
is tested by installing methylene blue through
the cervix & observing spillage of dye from
fimbrial end.
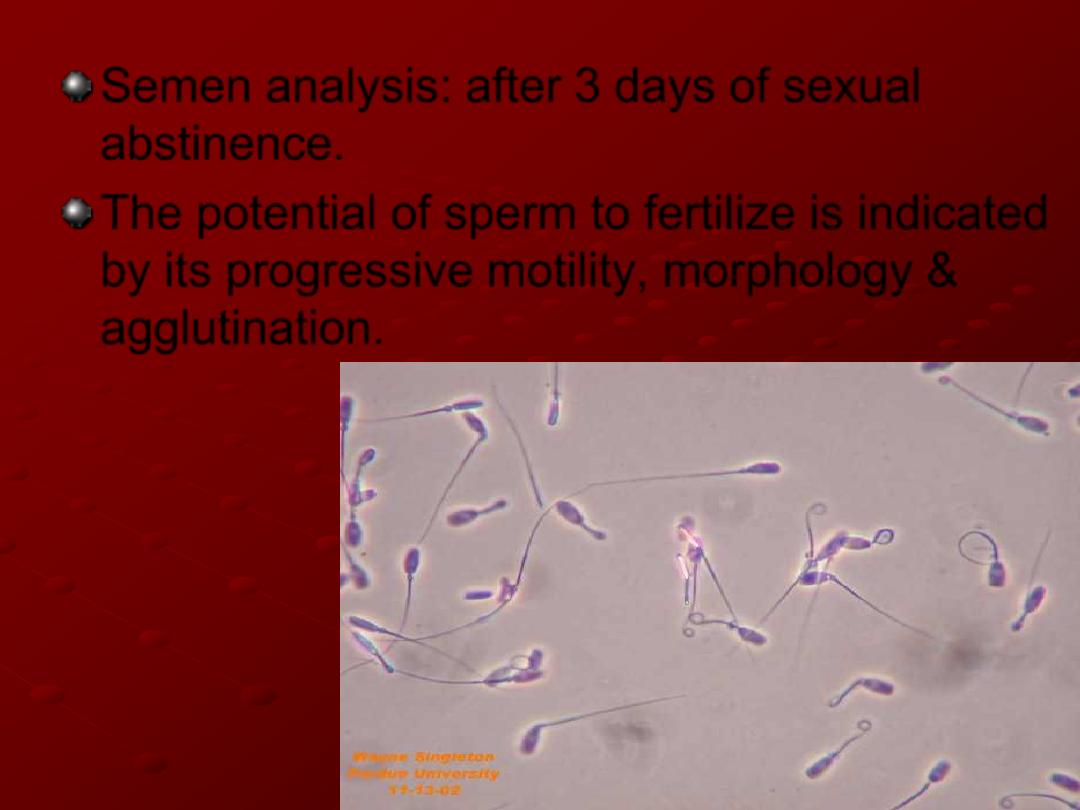
Semen analysis: after 3 days of sexual
abstinence.
The potential of sperm to fertilize is indicated
by its progressive motility, morphology &
agglutination.
In men with very low sperm counts, an
endocrine profile (LH, FSH, testosterone &
prolactin is indicated.
Treatment:
Ovulatory disorders:
Hypothalamic disorder: optimize patient
weight & avoid stressful lifestyle.
If hyperprolactinaemia: dopaminergic
agonists (e.g bromocriptin, cabergolin).
If PCOS: …
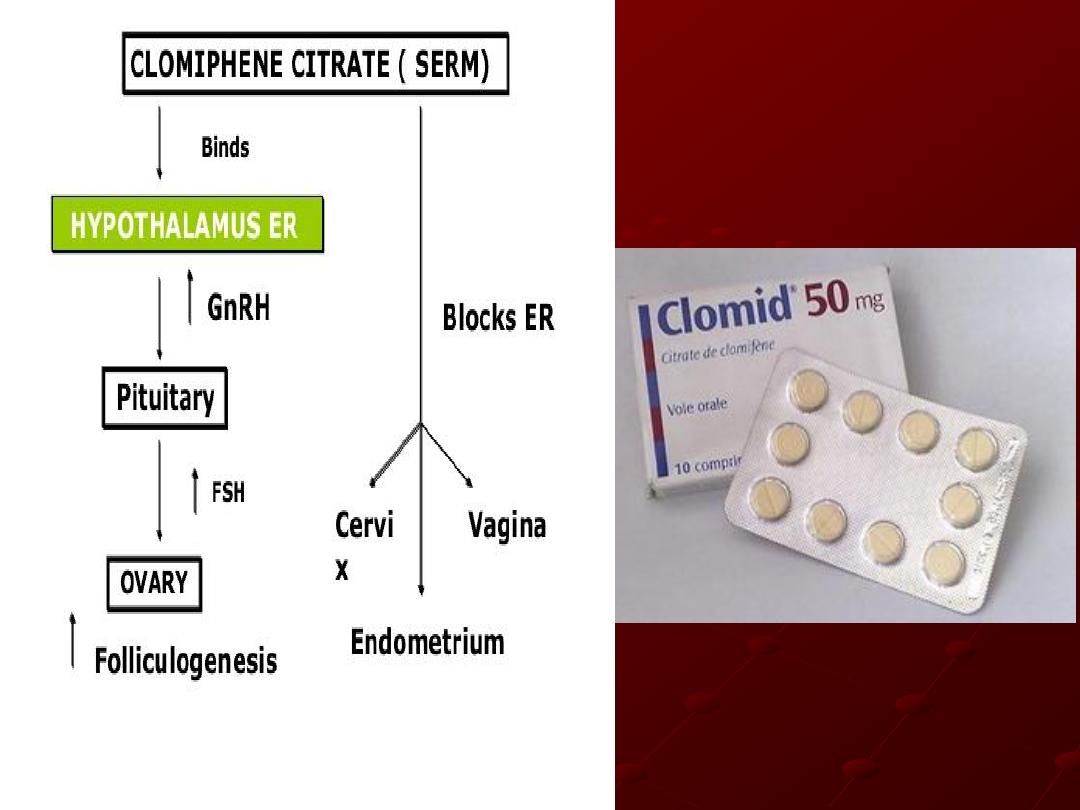
Ovulation induction:
Clomiphene citrate: acts by increasing
gonadotrophin release from the pituitary.
Response monitored by ultrasound.to
avoid multiple pregnancy.
Adverse anti-oestrogenic effects of
clomiphene citrate include thickening of
cervical mucus & hot flushes, others
include abdominal distension & pain,
nausea, vomiting, breast tenderness &
reversible hair loss.

aromatase inhibitors : letrozole is
nowadays used for OI as first line
espetially for patients with PCOS. It inhibit
aromatization of testosterone to estradiole
& decrease level of estrogen decrease
negative feedback on pituitary thus
increaseing FSH secretion.
Gonadotrophins (FSH): are given by daily
injection from the beginning of the cycle.
monitored by US assessment of the
number & size of follicles.
Human menopausal gonadotrophin,
urinary follicle-stimulating hormone and
recombinant follicle-stimulating hormone
are equally effective in achieving
pregnancy
Ovulation is triggered by injection of
human chorionic gonadotrophin (hCG
which binds to LH receptors) when 1-3
follicles are 18 mm in diameter.
If more than three follicles are present, the
couples are asked to avoid sexual
intercourse & hCG is withheld.
Tubal disease:
Treatment aims to restore normal
anatomy.
The success depends on severity, location
of damage & skills of the surgeon.
In-vitro fertilization is an alternative to
surgery.
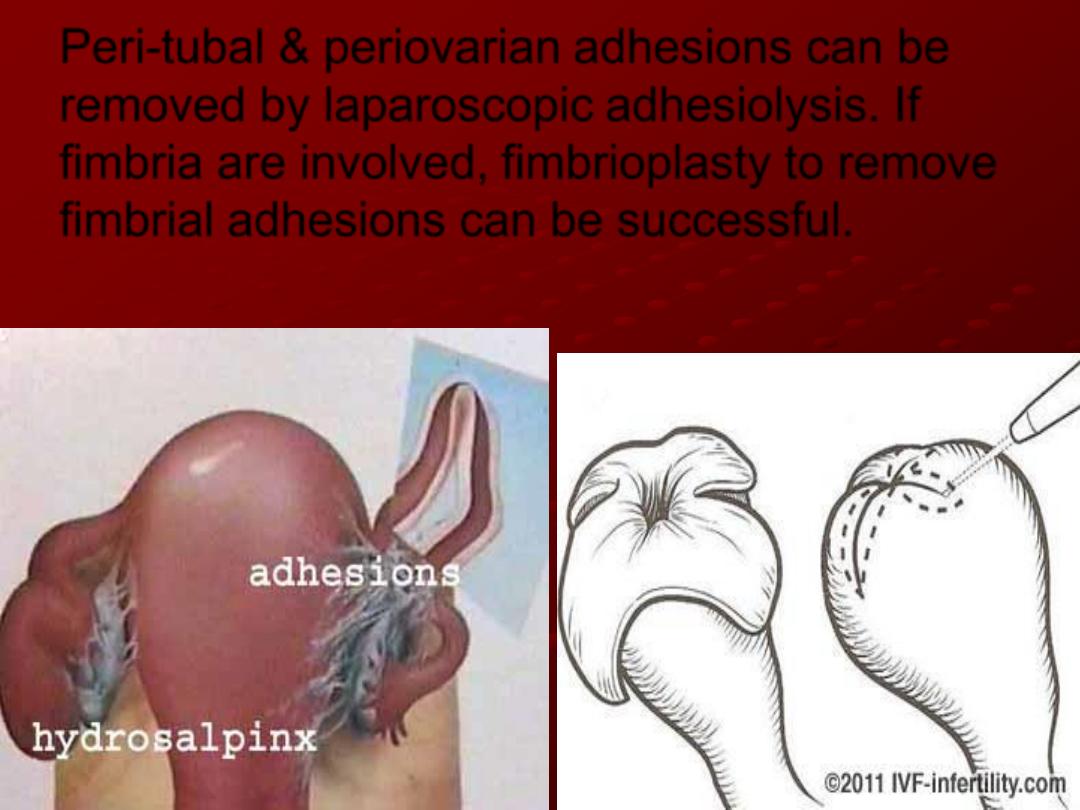
Peri-tubal & periovarian adhesions can be
removed by laparoscopic adhesiolysis. If
fimbria are involved, fimbrioplasty to remove
fimbrial adhesions can be successful.
Reversal of sterilization produce good
conception rate as the mucosal damage is
limited & the woman has proven fertility.
In case of hydrosalpinges, better to
remove the affected Fallopian tube prior to
IVF as they affect implantation adversely.
