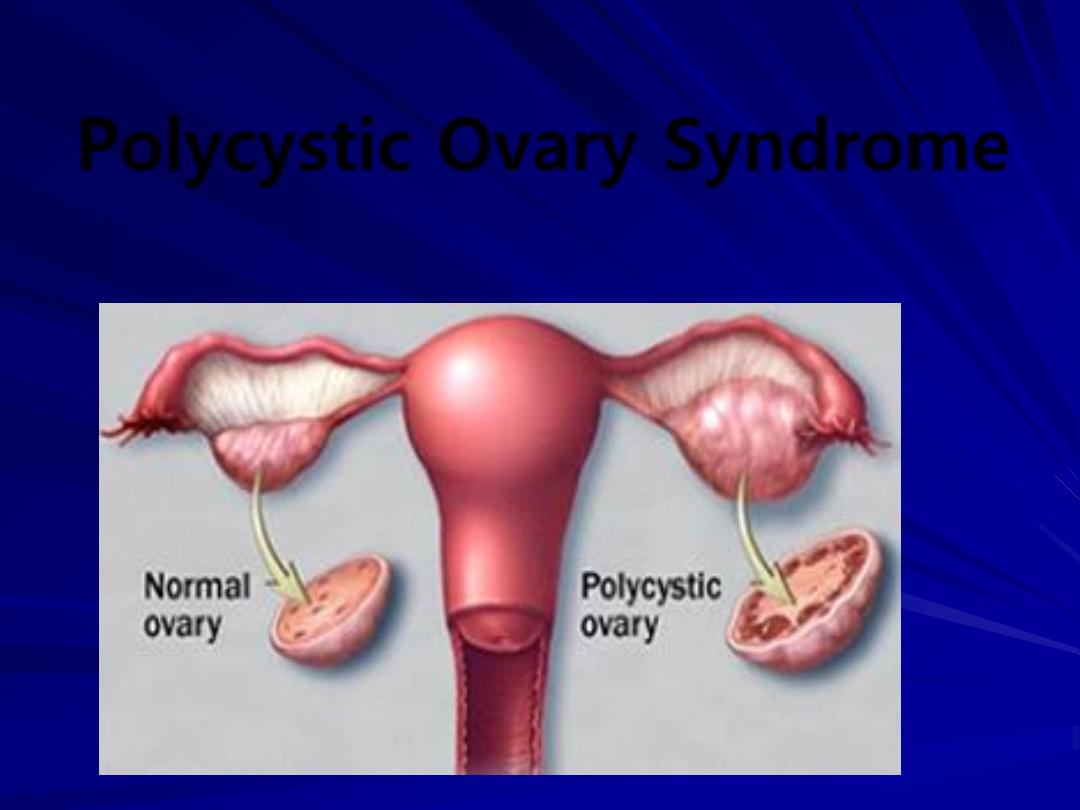
Polycystic Ovary Syndrome
Objectives of Lecture
To know what is PCOS & its underlying
pathophysiology
How to diagnose a patient with PCOS
How to counsel a patients with PCOS
Treament optios for PCOS
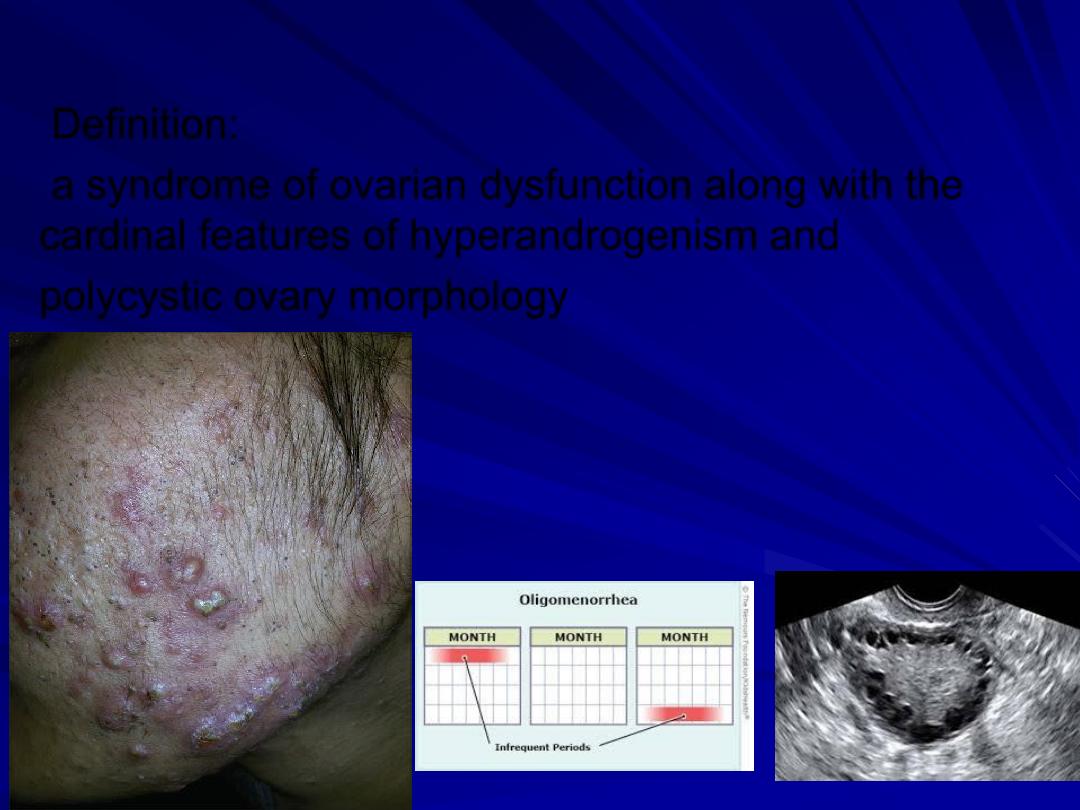
Definition:
a syndrome of ovarian dysfunction along with the
cardinal features of hyperandrogenism and
polycystic ovary morphology
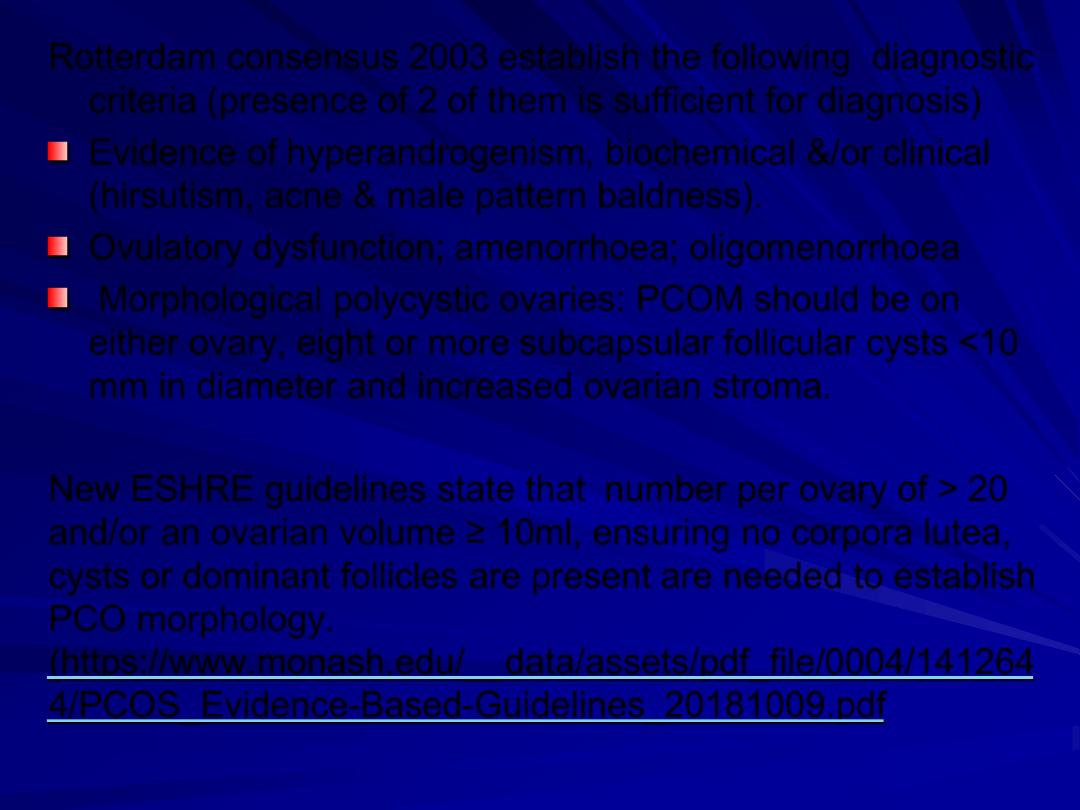
Rotterdam consensus 2003 establish the following diagnostic
criteria (presence of 2 of them is sufficient for diagnosis)
Evidence of hyperandrogenism, biochemical &/or clinical
(hirsutism, acne & male pattern baldness).
Ovulatory dysfunction; amenorrhoea; oligomenorrhoea
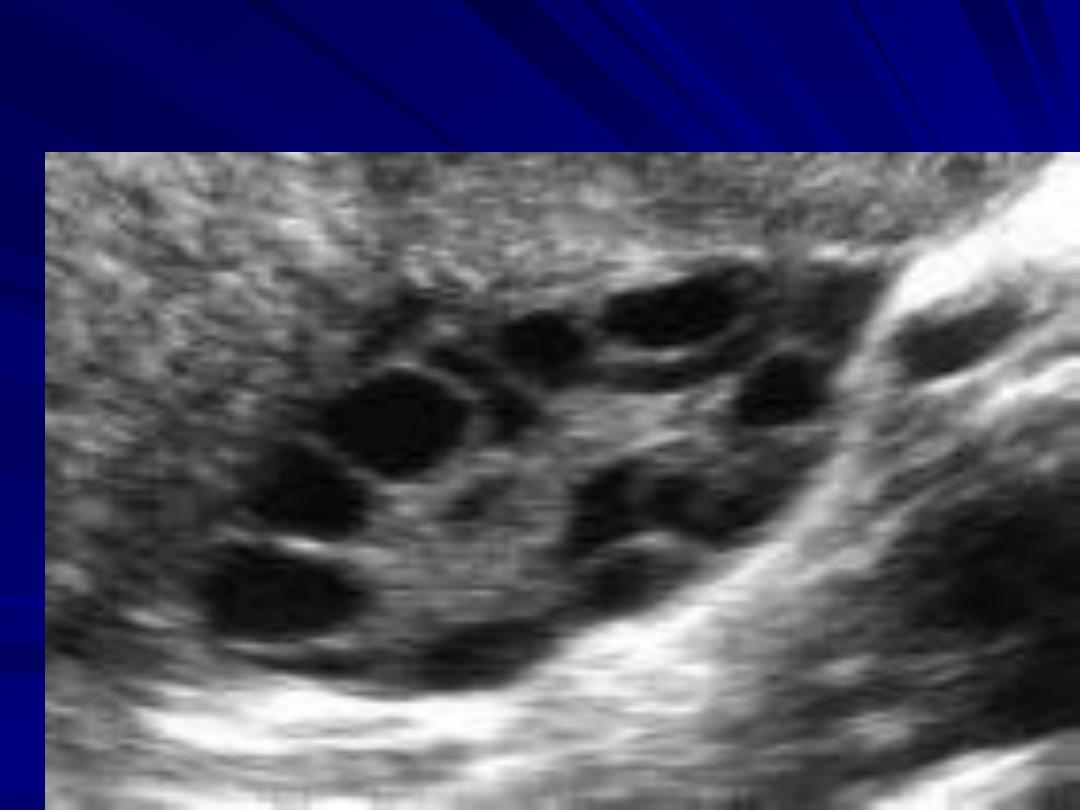
Morphological polycystic ovaries: PCOM should be on
either ovary, eight or more subcapsular follicular cysts <10
mm in diameter and increased ovarian stroma.
New ESHRE guidelines state that number per ovary of > 20
and/or an ovarian volume ≥ 10ml, ensuring no corpora lutea,
cysts or dominant follicles are present are needed to establish
PCO morphology.
PCOS is diagnosed in the presence of two
out of the three criteria and in the absence
of other aetiologies (thyroid dysfunction,
congenital adrenal hyperplasia,
hyperprolactinaemia, androgen-secreting
tumours and Cushing syndrome)
Aetiology:
Genetic factor: the prevalence in first
degree relatives is 5-6 times higher than in
the general population.
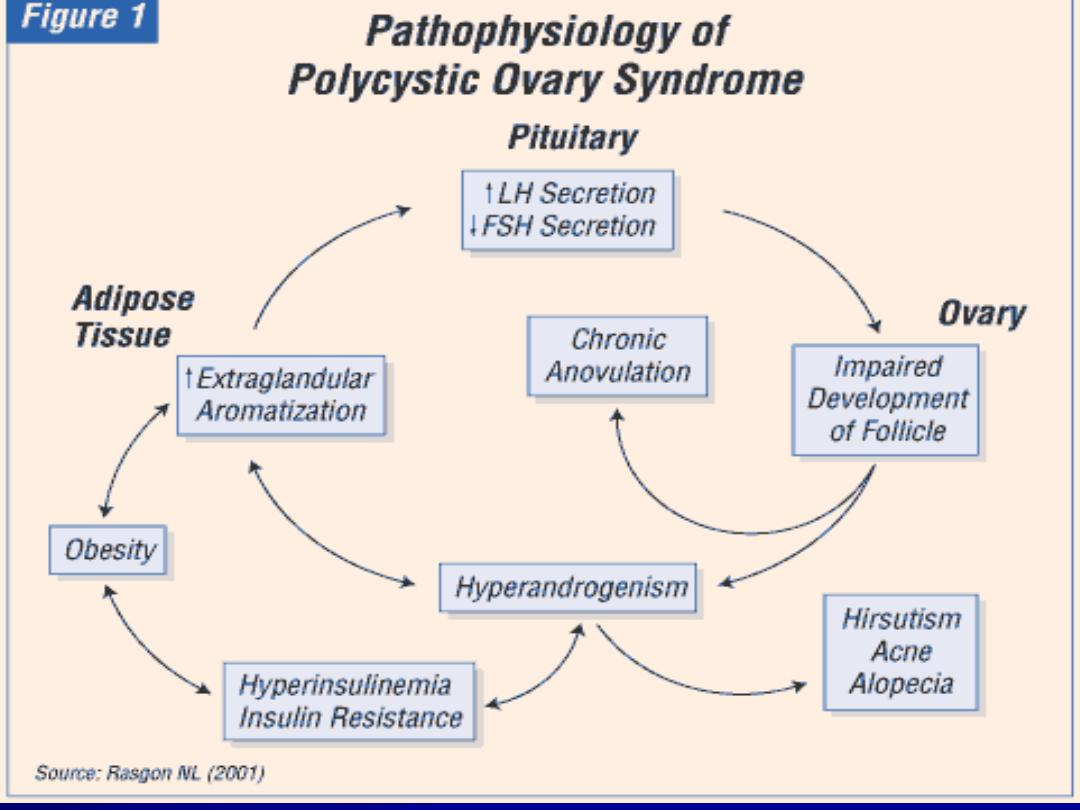
Hormonal factors:
Hypersecretion of LH
Hypersecretion of androgens.
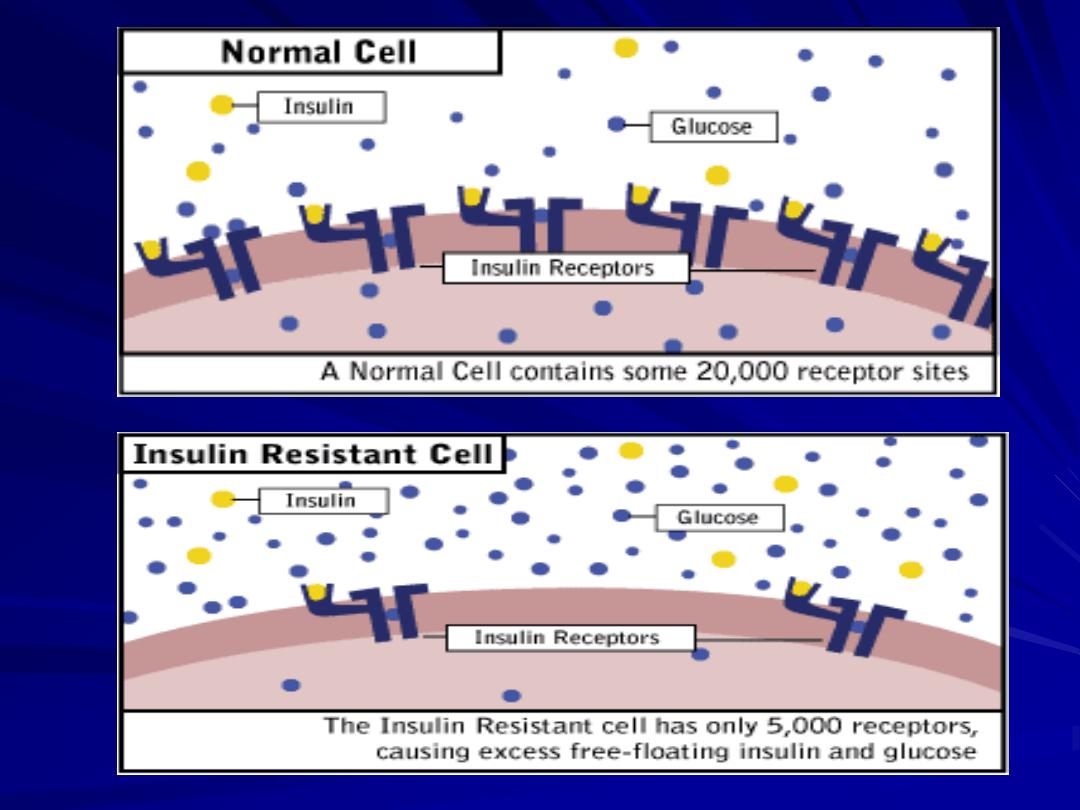
Insulin resistance especially in those with
high BMI. Lead to hyperinsulinaemia
Diagnosis:
Diagnosis of PCOS can only be made when
other aetiologies have been excluded
(thyroid dysfunction, congenital adrenal
hyperplasia, hyperprolactinaemia,
androgen-secreting tumours and Cushing
syndrome).
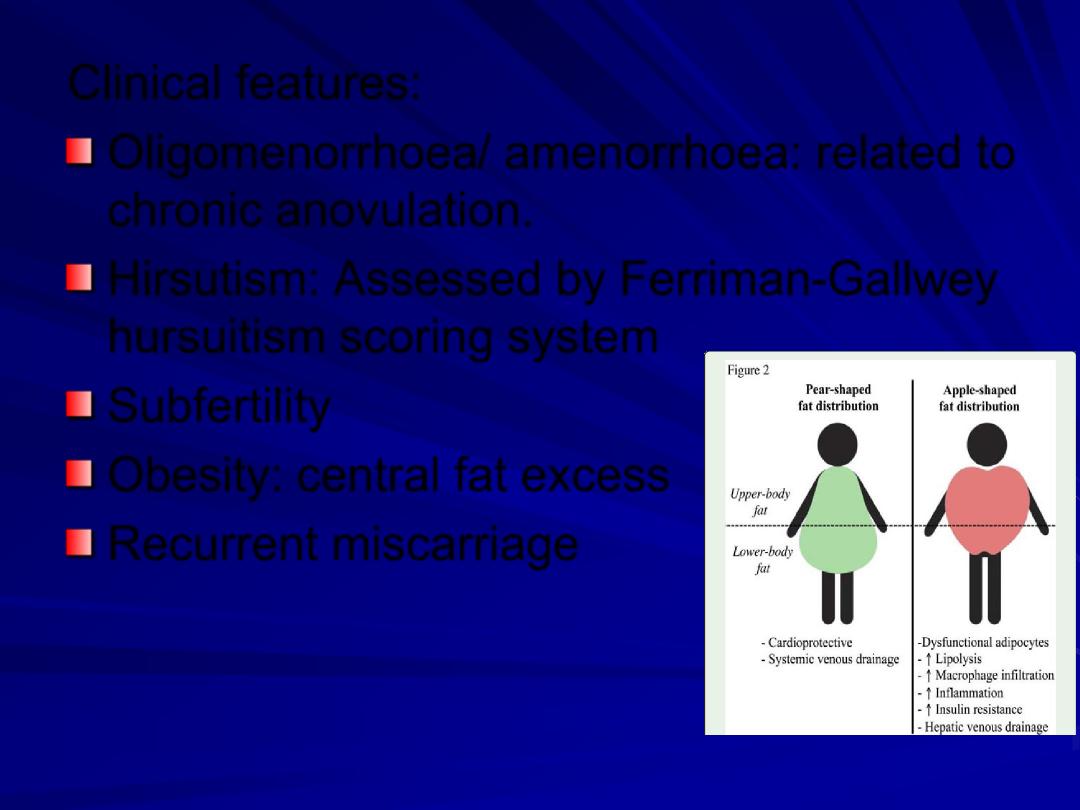
Clinical features:
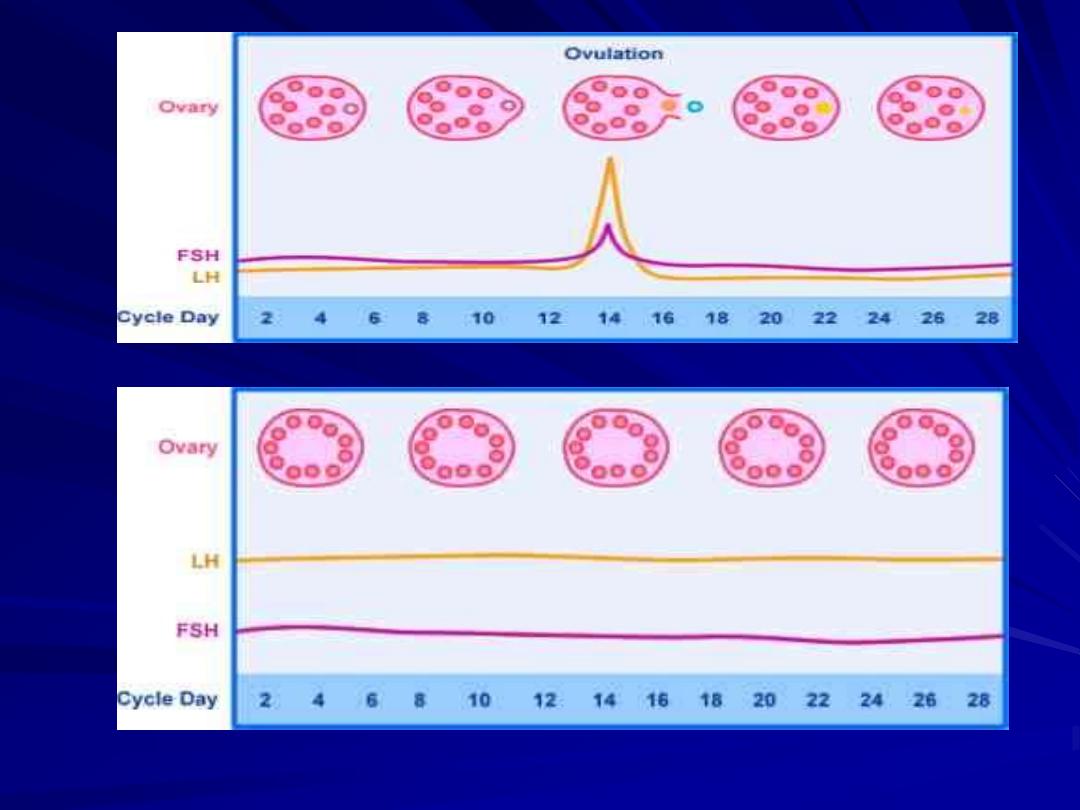
Oligomenorrhoea/ amenorrhoea: related to
chronic anovulation.
Hirsutism: Assessed by Ferriman-Gallwey
hursuitism scoring system
Subfertility
Obesity: central fat excess
Recurrent miscarriage

• Acanthosis nigricance: areas of
increased skin pigmentation
occur in axillae & other flexures
Laboratory test:
A raised LH / FSH ratio is no longer a
diagnostic criteria for PCOS owing to its
inconsistency
The recommended baseline screening tests
are
thyroid function tests: normal or mild
derangement
serum prolactin: mild elevation.
free androgen index (total testosterone
divided by sex hormone binding globulin
(SHBG) x 100 to give a calculated free
testosterone level)
Long-term health implications of PCOS
:
Increased incidence of multiple pregnancy,
gestational diabetes & pregnancy-induced
hypertension.
Increased incidence of type II diabetes mellitus,
hypertension & hyperlipidaemia due to insulin
resistance & hyperandrogenism respectively
and thus increased risk of cardiovascular
disease.
Increased incidence of endometrial hyperplasia
& endometrial carcinoma due to unopposed
estrogen stimulation.
Overweight and obese women with PCOS,
regardless of age, should have a fasting lipid profile
(cholesterol, LDL, HDL and triglyceride level at
diagnosis).
An oral glucose tolerance test (OGTT), fasting
plasma glucose or HbA1c should be performed to
assess glycaemic status.
A 75-g OGTT should be offered in all women with
PCOS preconception when planning pregnancy or
seeking fertility treatment.
If not performed preconception, an OGTT should be
offered at < 20 weeks gestation, and all women with
PCOS should be offered the test at 24-28 weeks
gestation.
Treatment:
Obesity:
Change in lifestyle with altered diet & exercise
might be effective.
use of insulin-sensitising agents (metformin)
in patients with insulin resistance.
Use of weight-reduction drugs may be helpful
in reducing insulin resistance through weight
loss.
Example: Orlistat

Oligomenorrhoea/amenorrhoea:
because of chronic anovulation there is
increased risk of endometrial cancer
cyclical progesterone is useful to induce
withdrawal bleeds & to protect the
endometrium.
Alternatively for those who do not want to
conceive oral contraceptive pills can be
used.

Infertility:
Weight loss : improve both spontaneous & drug
induced ovulation.
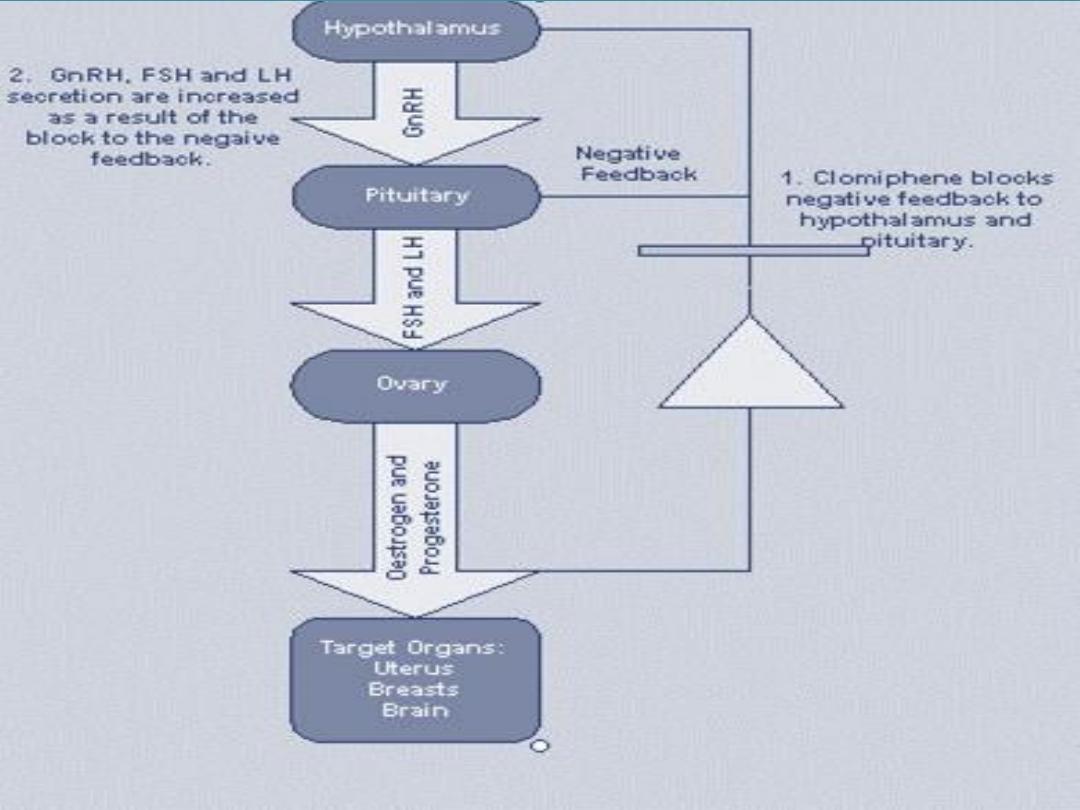
Clomiphene citrate: anti-estrogen used for
ovulation induction by blocking estrogen receptors
with a resultant increase in endogenous FSH
production.
used for six months only.
Recently letrozole become superior to clomiphene
citrate for ovulation induction by oral agents in
PCOS patients
Metformin: biguanide inhibit the production
of hepatic glucose & enhances the
sensitivity of peripheral tissues to insulin,
thereby reducing insulin secretion.
Metformin may also improve menstrual
regularity & improve ovarian response to
clomiphene.
Gonadotrophin therapy:
recombinant
FSH & human menopausal gonadotrophin
Because the PCO is very sensitive to exogenous
hormones, there is increased risk of developing
ovarian hyperstimulation syndrome (OHSS).
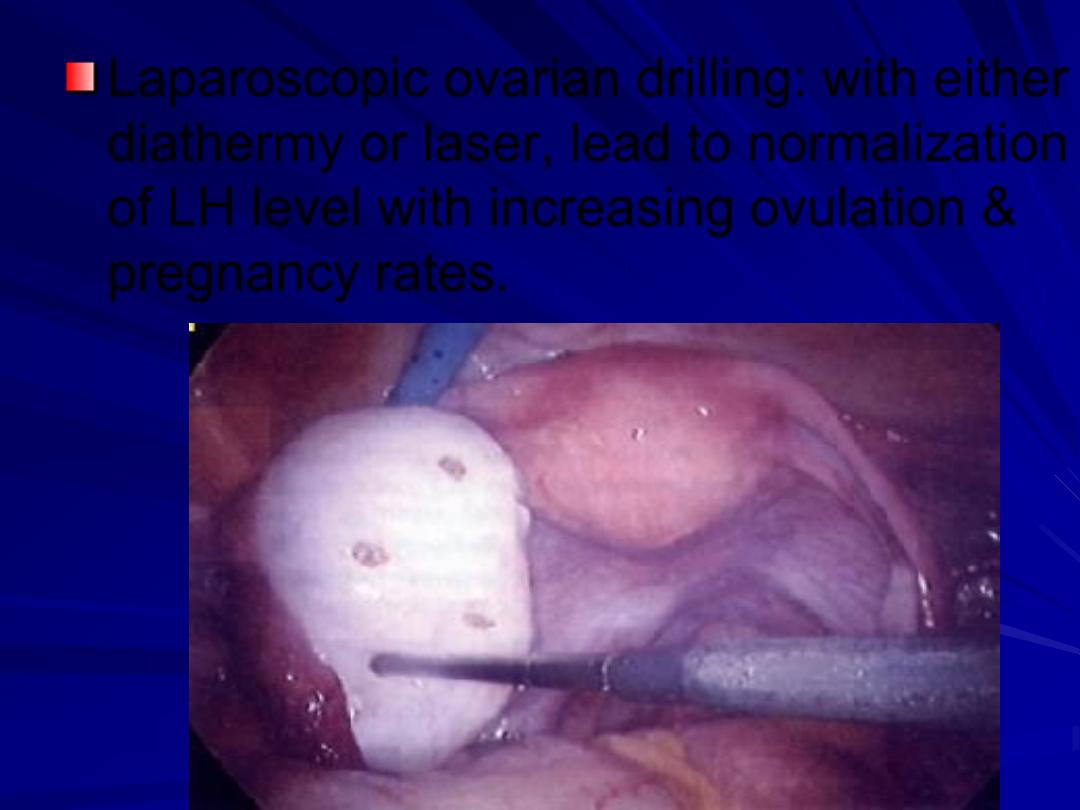
Laparoscopic ovarian drilling: with either
diathermy or laser, lead to normalization
of LH level with increasing ovulation &
pregnancy rates.
Hirsuitism:
The aim of treatment is to reduce the
androgen level, increase sex hormone-
binding globulin or reduce the activity of
5
α-reductase enzyme at the level of the
hair follicle.
Oral contraceptive pills
Cyproteron acetate
Eflornithine cream
Spironolactone
Finasteride
Physical methods of hair removal
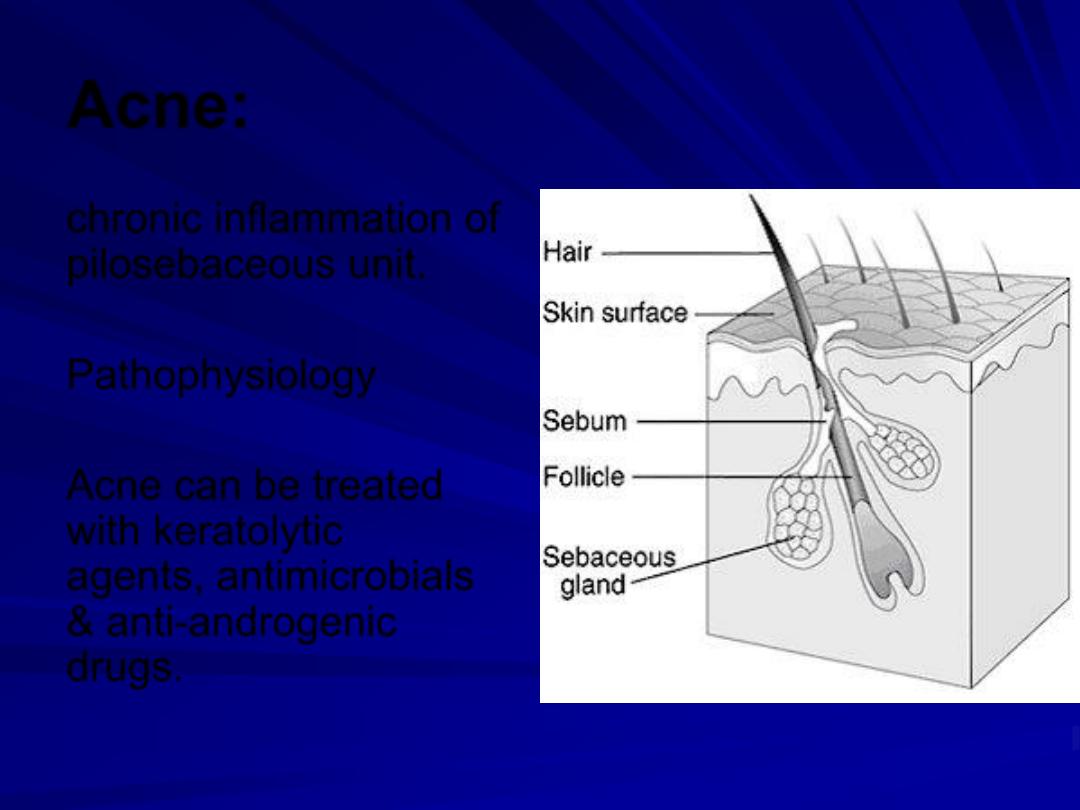
Acne:
chronic inflammation of
pilosebaceous unit.
Pathophysiology
Acne can be treated
with keratolytic
agents, antimicrobials
& anti-androgenic
drugs.
