Injuries of the upper limbs
Dr.Mushtaq Talib Hussein
F.I.B.M.S(ortho.) C.A.B.O(ortho.)
FRACTURES OF THE CLAVICLE
In children the clavicle fractures easily, but it almost invariably unites rapidly and without
complications In adults this can be a much more troublesome injury.
A fall on the shoulder or the outstretched hand may break the clavicle.
Clinical features
The arm is clasped to the chest to prevent movement. A subcutaneous lump may be obvious
and occasionally a sharp fragment threatens the skin.
Imaging
Radiographic analysis requires at least an anteroposterior view and another taken with
a 30 degree cephalic tilt.
Clavicle fractures are usually classified on the basis of their location: Group I (middle
third fractures), Group II (lateral third fractures) and Group III(medial third fractures).
Treatment
MIDDLE THIRD FRACTURES
There is general agreement that undisplaced fractures should be treated non-
operatively.
Non-operative management consists of applying a simple sling for comfort. It is subsides
(between 1–3 weeks) and the patient is then discarded once the pain encouraged to
mobilize the limb as pain allows.
LATERAL THIRD FRACTURES
non-operative management is usually appropriate for minimally displaced fractures
while Displaced lateral third fractures are associated with disruption of the
coracoclavicular ligaments and are therefore unstable injuries,
Surgery to stabilize the
fracture is often recommended.
Complications
EARLY
damage to the subclavian vessels and brachial plexus injuries are all very rare.
LATE
Non-union In displaced fractures of the shaft nonunion occurs in 1–15 per cent. Lateral
clavicle fractures have a higher rate of nonunion(11.5–40 per cent).
Malunion All displaced fractures heal in a nonanatomical position with some shortening
and angulation, however most do not produce symptoms.
Stiffness of the shoulder This is common but temporary; it results from fear of moving
the fracture.
FRACTURES OF THE SCAPULA
The body of the scapula is fractured by a crushing force, which usually also fractures
ribs and may dislocate the sternoclavicular joint.
The arm is held immobile and there
may be severe bruising over the scapula or the chest wall. Because of the energy
required to damage the scapula, fractures of the body of the scapula are often associated
with severe injuries to the chest, brachial plexus, spine, abdomen and head. Careful
neurological and vascular examinations are essential.
ACROMIOCLAVICULAR JOINT INJURIES
Acute injury of the acromioclavicular joint is common and usually follows direct trauma.
Chronic sprains, often associated with degenerative changes, are seen in people engaged
or occupations such as working with jack-hammers in athletic activities like
weightlifting and other heavy vibrating tools.
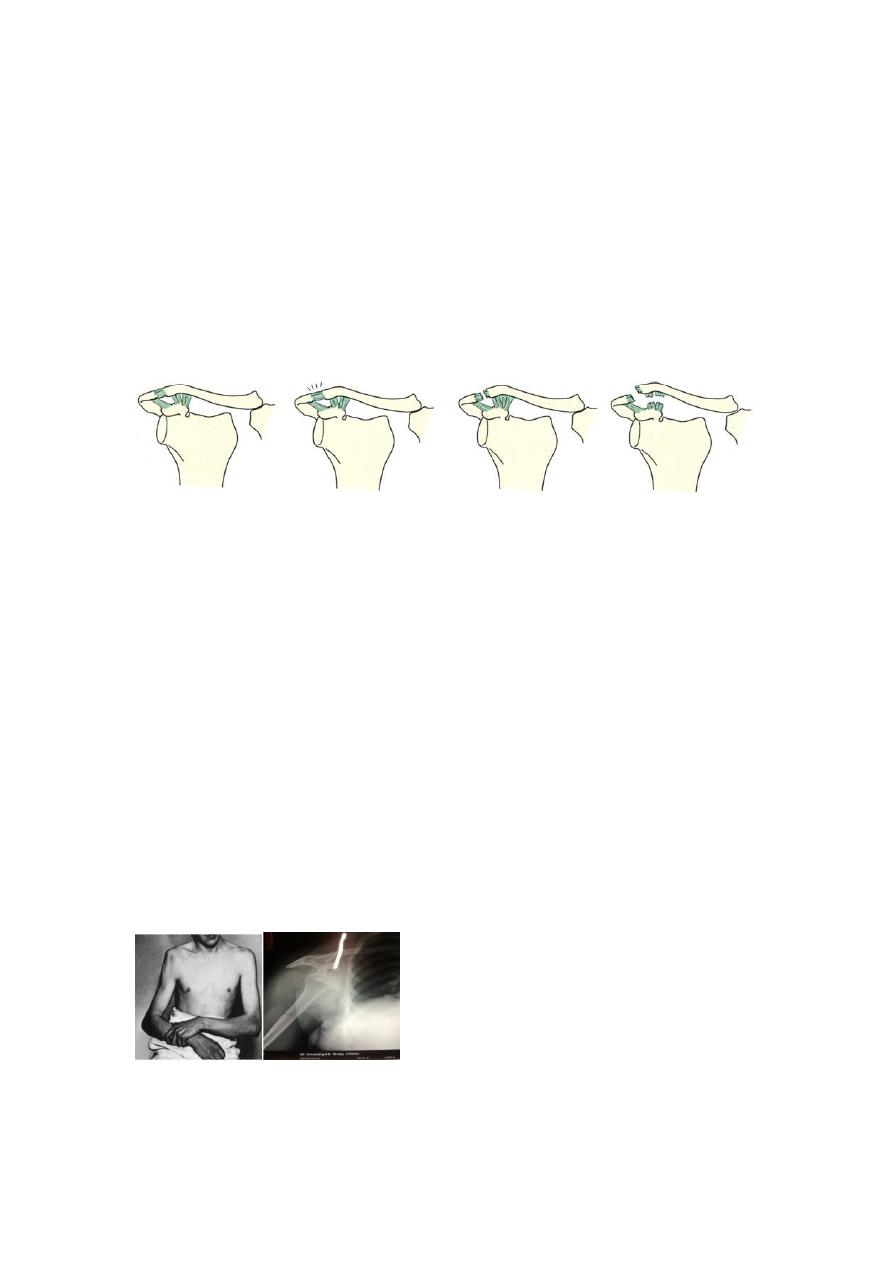
A b c d
Acromioclavicular joint injuries (a)
Normal joint.
(b)
Sprained acromioclavicular joint; no
displacement.
(c)
Torn capsule and subluxation but coracoclavicular ligaments intact.
(d)
Dislocation
with torn coracoclavicular ligaments.
DISLOCATION OF THE SHOULDER
Of the large joints, the shoulder is the one that most commonly dislocates. This is due to
a number of factors: the shallowness of the glenoid socket; the extraordinary range of
movement; underlying conditions such as ligamentous laxity or glenoid dysplasia;
and the sheer vulnerability of the joint during stressful activities of the upper limb.
ANTERIOR DISLOCATION
Mechanism of injury
Dislocation is usually caused by a fall on the hand. The head of the humerus is driven
forward, tearing the capsule and producing avulsion of the glenoid labrum (the Bankart
lesion).
Clinical features
Pain is severe. The patient supports the arm with the opposite hand and is loathe to
permit any kind of examination. The lateral outline of the shoulder may be flattened and,
if the patient is not too muscular, a bulge may be felt just below the clavicle. The arm
must always be examined for nerve and vessel injury before reduction is attempted.
X-Ray
The anteroposterior x-ray will show the overlapping shadows of the humeral head and
glenoid fossa, with the head usually lying below and medial to the socket.
Treatment
Various methods of reduction have been described, some of them now of no more than
historical interest. In a patient who has had previous dislocations, simple traction on the
arm may be successful. Usually, sedation and occasionally general anaesthesia is
required.
With Stimson’s technique, the patient is left prone with the arm hanging over the side of
the bed. After15 or 20 minutes the shoulder may reduce.
In the Hippocratic method, gently increasing traction is applied to the arm with the
shoulder in slight abduction, while an assistant applies firm counter traction to the body
(a towel slung around the patient’s chest, under the axilla, is helpful).
An x-ray is taken to confirm reduction and exclude
a
fracture. When the patient is fully
awake, active abduction is gently tested to exclude an axillary nerve injury and rotator
cuff tear. The median, radial, ulnar and musculocutaneous nerves are also tested and the
pulse is felt. The arm is rested in a sling for about three weeks in those under 30 years of
age (who are most prone to recurrence) and for only a week in those over 30 (who are
most prone to stiffness).
Complications
EARLY
Rotator cuff tear This commonly accompanies anterior dislocation, particularly in older
people.
Nerve injury The axillary nerve is most commonly injured; the patient is unable to
contract the deltoid muscle and there may be a small patch of anaesthesia over the
muscle.
Vascular injury The axillary artery may be damaged, particularly in old patients with
fragile vessels.
Fracture-dislocation If there is an associated fracture of the proximal humerus, open
reduction and internal fixation may be necessary.
LATE
Shoulder stiffness Prolonged immobilization may lead to stiffness of the shoulder,
especially in patients over the age of 40.
Unreduced dislocation Surprisingly, a dislocation of the shoulder sometimes remains
undiagnosed. This is more likely if the patient is either unconscious or very old.
Recurrent dislocation If an anterior dislocation tears the shoulder capsule, repair
occurs spontaneously following reduction and the dislocation may not recur; but if the
glenoid labrum is detached, or the capsule is stripped off the front of the neck of the
glenoid, repair is less likely and recurrence is more common.
POSTERIOR DISLOCATION OF THE SHOULDER
Posterior dislocation is rare, accounting for less than 2 per cent of all dislocations
around the shoulder.
Indirect force producing marked internal rotation and adduction needs be very severe
to cause a dislocation. This happens most commonly during a fit or convulsion, or with
an electric shock.
The diagnosis is frequently missed – partly because reliance is placed
on a single anteroposterior x-ray(which may look almost normal) and partly because
those attending to the patient fail to think of it.
INFERIOR DISLOCATION OF THE SHOULDER (LUXATIO ERECTA)
Inferior dislocation is rare but it demands early recognition because the consequences
are potentially very serious. Dislocation occurs with the arm in nearly full
abduction/elevation. The humeral head is levered out of its socket and pokes into the
axilla; the arm remains fixed in abduction.

FRACTURES OF THE PROXIMAL HUMERUS
Fractures of the proximal humerus usually occur after middle age and most of the
patients are osteoporotic, postmenopausal women.
Fracture usually follows a fall on the out-stretched arm – the type of injury which, in
younger people ,might cause dislocation of the shoulder. Sometimes, indeed, there is
both a fracture and a dislocation.
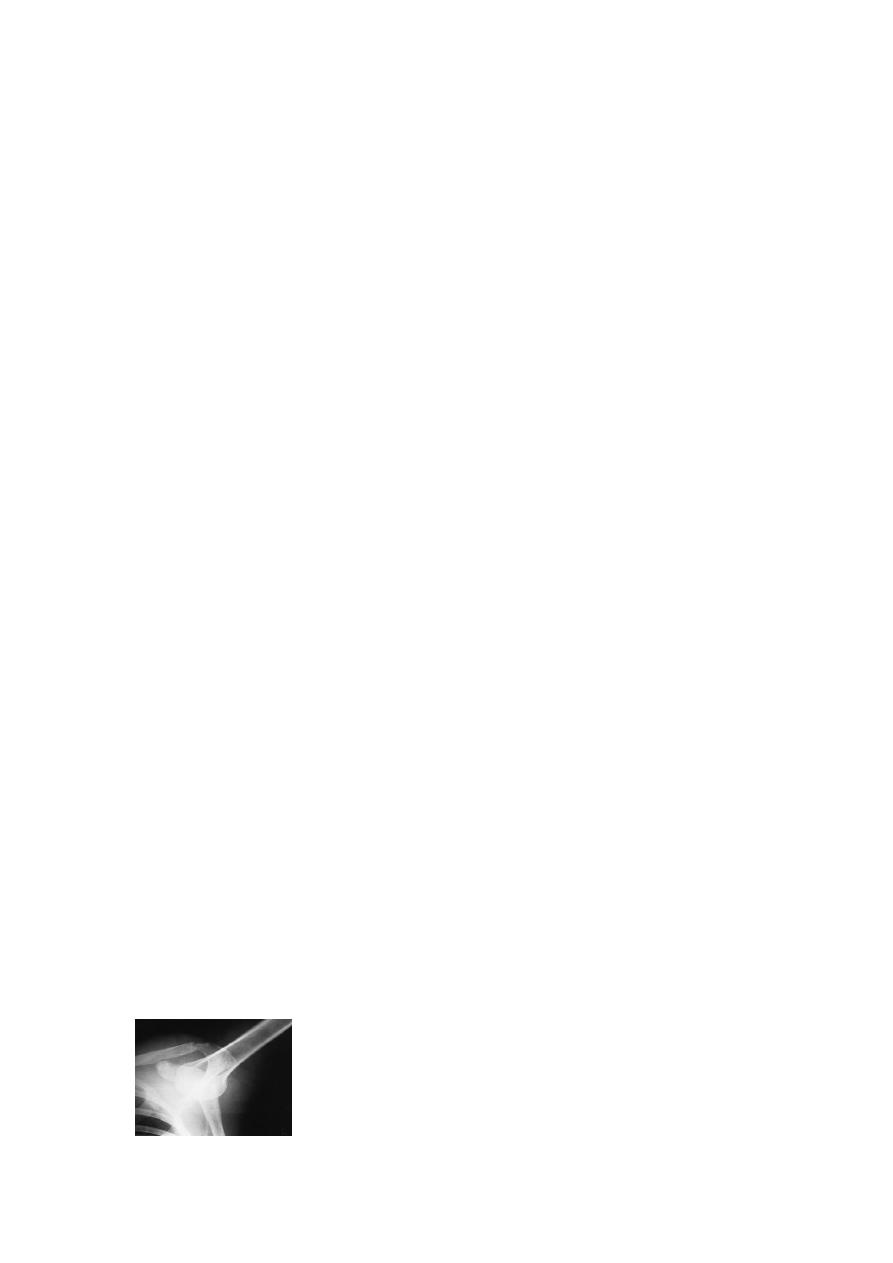
A b c d
X-rays of proximal humeral fractures
Classification is all very well, but x-rays are more difficult to
interpret than line drawings.
(a)
Two-part fracture.
(b)
Three-part fracture involving the neck and the
greater tuberosity.
(c)
Four-part fracture. (1=shaft of humerus; 2=head of humerus; 3=greater tuberosity;
4=lesser tuberosity).
(d)
X-ray showing fracture -dislocation of the shoulder.
Clinical features
Because the fracture is often firmly impacted, pain may not be severe. However, the
appearance of a large bruise on the upper part of the arm is suspicious. Signs of axillary
nerve or brachial plexus injury should be sought.
X-ray
In elderly patients there often appears to be a single, impacted fracture extending across
the surgical neck.
Neer’s classification (as shown above)when based on plain x-rays
criteria for displacement (distance >1 cm, angulation >45 degrees) help clarify the
pathoanatomy of the different fracture patterns.
The advent of three-dimensional CT reconstruction has helped to reduce the degree of
inter- and intra-observer error.
Treatment
Minimally displaced fractures, which comprise the vast majority. They need no
treatment apart from a week or two period of rest with the arm in a sling until the pain
subsides, and then gentle passive movements of the shoulder.
Displaced fractures need surgical intervention , while fracture- dislocation in elderly
osteoporotic patients(especially four-part), prosthetic replacement is recommended.
FRACTURED SHAFT OF HUMERUS
Mechanism of injury
A fall on the hand may twist the humerus, causing a spiral fracture. A fall on the elbow
with the arm abducted exerts a bending force, resulting in an oblique or transverse
fracture. A direct blow to the arm causes a fracture which is either transverse or
comminuted. Fracture of the shaft in an elderly patient may be due to a metastasis.
Clinical features
The arm is painful, bruised and swollen. It is important to test for radial nerve function
before and after treatment.
X-ray
The site of the fracture, its line (transverse, spiral or comminuted) and any displacement
are readily seen.
The possibility that the fracture may be pathological should be remembered.
Treatment
Fractures of the humerus heal readily. They require neither perfect reduction nor
immobilization; the weight of the arm with an external cast is usually enough to pull the
fragments into alignment. A ‘hanging cast’ is applied from shoulder to wrist with the
elbow flexed 90 degrees, and the forearm section is suspended by a sling around the

patient’s neck. This cast may be replaced after 2–3 weeks by a short(shoulder to elbow)
cast or a functional polypropylene brace which is worn for a further 6 weeks.
There are, nevertheless, some well defined indications for surgery:
(1)severe multiple injuries, (2) an open fracture,(3) segmental fractures,(4) displaced
intra-articular extension of the fracture,(5) a pathological fracture,(6) a ‘floating elbow’
(simultaneous unstable humeral and forearm fractures),(7) radial nerve palsy after
manipulation,(8) non-union,(9) problems with nursing care in a dependent person.
Complications
EARLY
Vascular injury If there are signs of vascular insufficiency in the limb, brachial artery
damage must be excluded.
Nerve injury Radial nerve palsy (wrist drop and paralysis of the metacarpophalangeal
extensors) may occur with shaft fractures, particularly oblique fracturesat the junction
of the middle and distal thirds of the bone (Holstein–Lewis fracture).
LATE
Delayed union and non-union Transverse fractures sometimes take months to unite,
especially if excessive traction has been used (a hanging cast must not be too heavy).
Joint stiffness Joint stiffness is common. It can be minimized by early activity.
