بسم الله الرحمن الرحيم
27/12/20204th lecture
2020RESPIRATORY MEDICINE
Chronic obstructive pulmonary disease (COPD)
ObjectivesTo know the
Epidemiology .
Etiology.
Pathogenesis .
Clinical presentation.
Investigation .
Diagnosis .
Treatment .
Complication .
Prognosis.
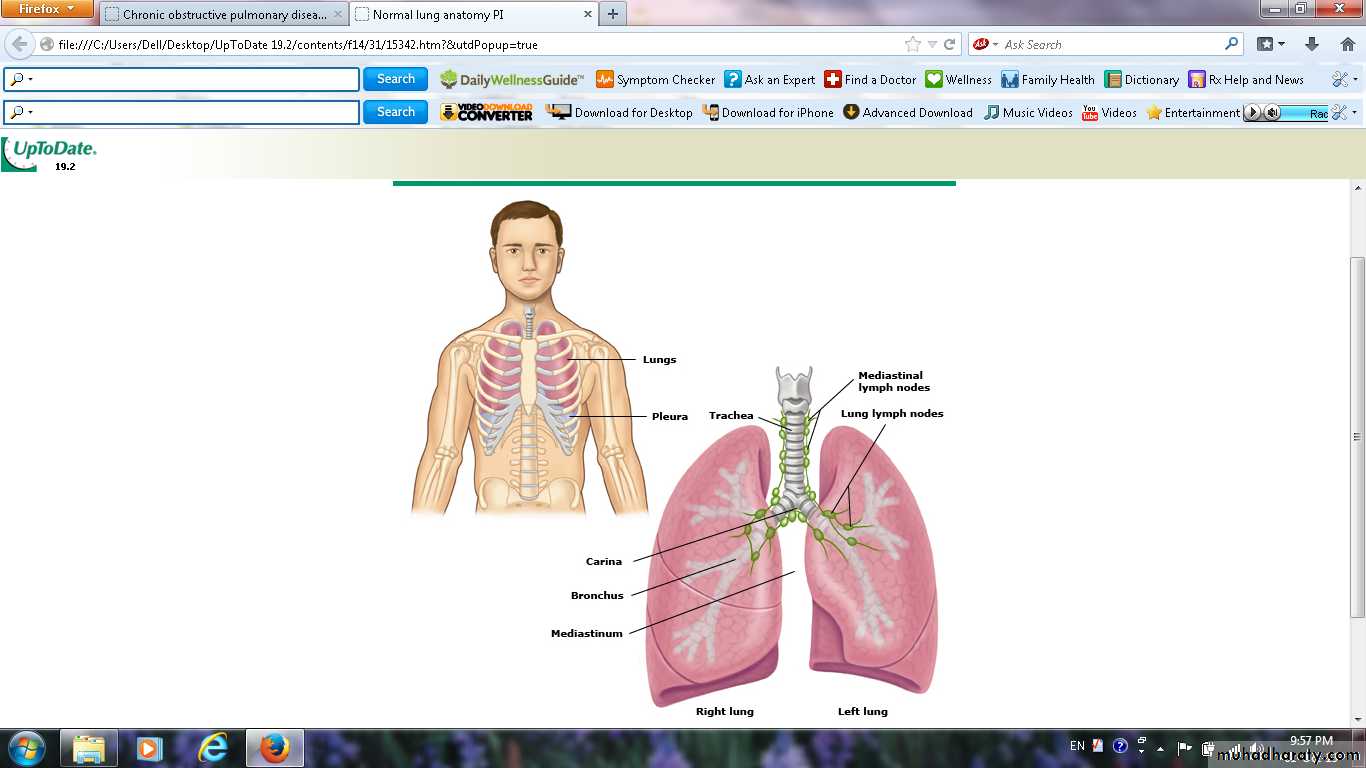
Definition
A preventable and treatable lung disease with some significant extrapulmonary effects that may contribute to the severity in individual patients.
The pulmonary component of COPD
Is characterised byairflow limitation that is not fully reversible.
usually progressive and associated with an abnormal inflammatory response of the lung to noxious particles or gases.
Extrapulmonary manifestations
Includeimpaired nutrition .
weight loss .
skeletal muscle dysfunction .
Related diagnoses include
Chronic bronchitisCough and sputum on most days for at least 3 consecutive months for at least 2 successive years)
Emphysema
Abnormal permanent enlargement of the air spaces distal to the terminal bronchioles, accompanied by destruction of their walls and without obvious fibrosis .Small airways disease
Airway less than 2 mm.
Epidemiology
80 million people world-wide suffer from moderate to severe disease.In 2005 more than 3 million deaths (5% of deaths globally).
2020 represent the third most important cause of death world-wide.
increasing tobacco consumption.
Aetiology
Cigarette smokingIt is unusual in those less than 10 pack years (1 pack year = 20 cigarettes/day/year)
individual susceptibility factors are important.
Risk factors for development of COPD
Exposures
Tobacco smoke: accounts for 95% of cases in UK
Biomass solid fuel fires: wood, animal dung, crop residues and coal lead to high levels of indoor air pollution
Occupation.
air pollution
Low birth weight.
childhood infections or maternal smoking
Infections.
Low socioeconomic status
Cannabis smoking
Host factors
Genetic factors: α1-antiproteinase deficiency .
Airway hyper-reactivity
Note
It is unusual to develop COPD with less than 10 pack years (1 pack year = 20 cigarettes/day/year)about 20% of smoker devlope this condition,Pathophysiology
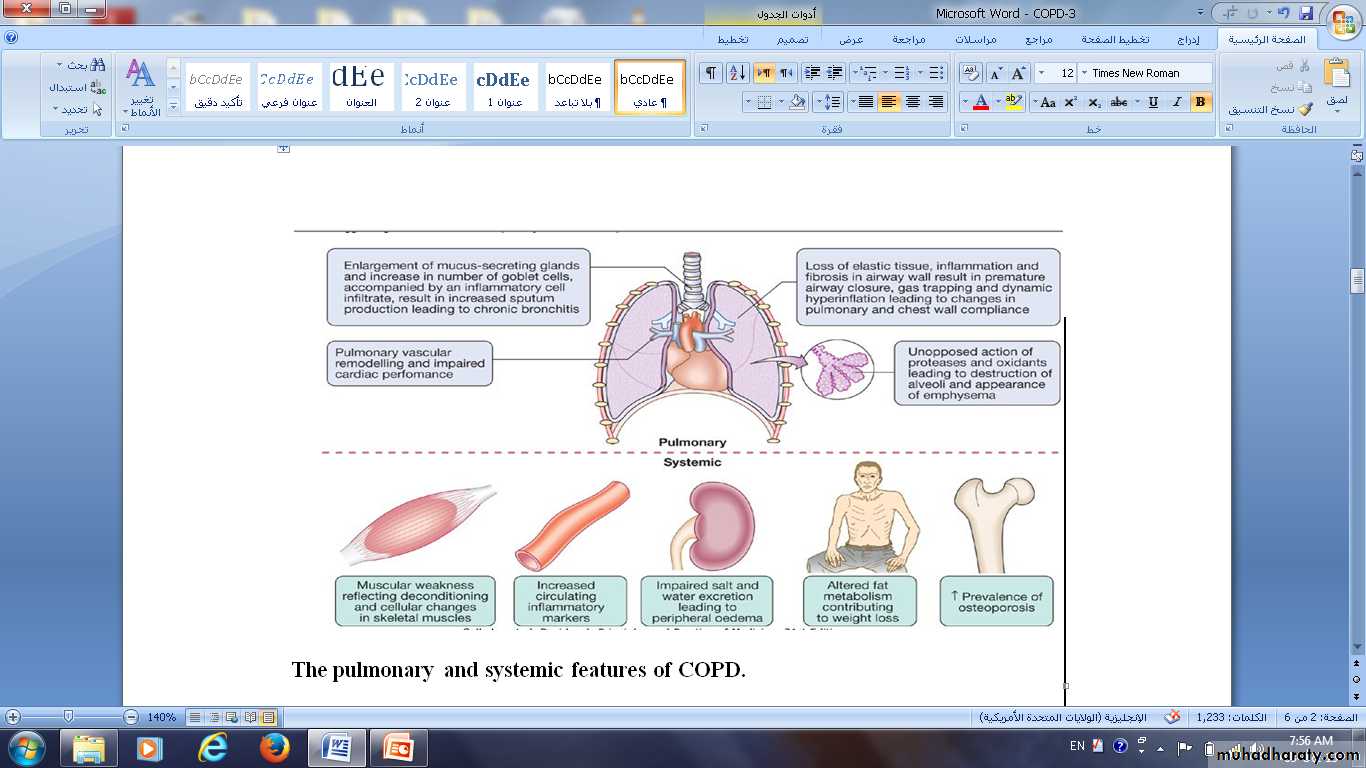
1-The changes in compliance mean that collapse of intrathoracic airways during expiration is exacerbated, during exercise as the time available for expiration shortens, resulting in dynamic hyperinflation.2-Increased V/Q mismatch
increases the dead space volume and wasted ventilation.3-Flattening of the diaphragmatic muscles and an increasingly horizontal alignment of the intercostal muscles.
4-The work of breathing is therefore markedly increased, first on exercise but, as the disease advances, at rest too.
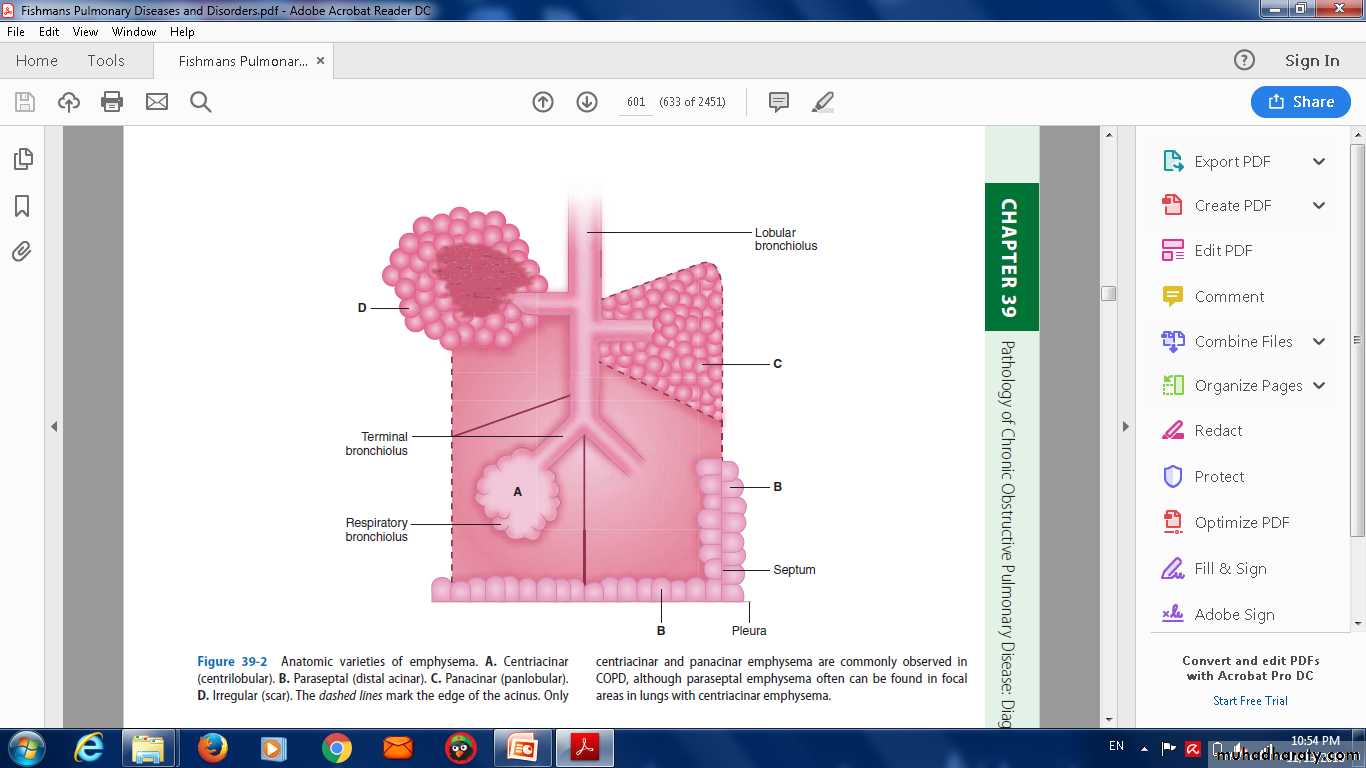
Pathophysiology of Emphysema
May be classified by the pattern of the enlarged airspaces:centriacinar,
panacinar
periacinar.
Bullae form in some individuals ,this results in impaired gas exchange and respiratory failure.
Anatomic varieties of emphysema. A. Centriacinar(centrilobular). B. Paraseptal (distal acinar). C. Panacinar (panlobular).D. Irregular (scar). The dashed lines mark the edge of the acinus.
Pathology of emphysema (A) NORMA(
Who has COPD ????
Clinical features
COPD should be suspected in any patient over the age of 40 years who presents with symptoms of chronic bronchitis and/or breathlessnessSYMPTOMS
Cough and associated sputum production are usually the first symptoms, often referred to as a 'smoker's cough'.Haemoptysis.
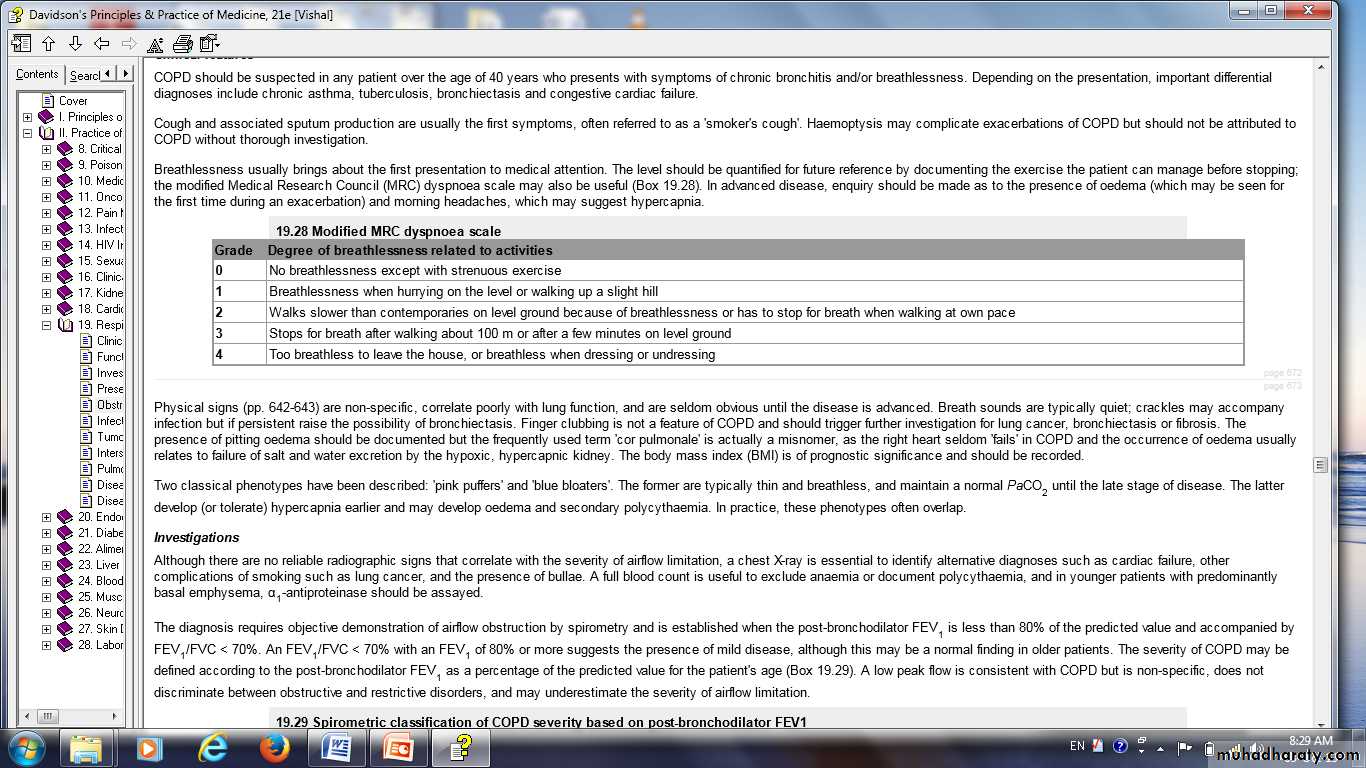
Breathlessness : the modified Medical Research Council (MRC) dyspnoea scale.
morning headaches, which may suggest hypercapnia.
Physical signs
non-specific,Breath sounds are typically quiet;
crackles.
pitting oedema
The body mass index (BMI) is of prognostic significance
Tobacco 'tar'-stained fingers
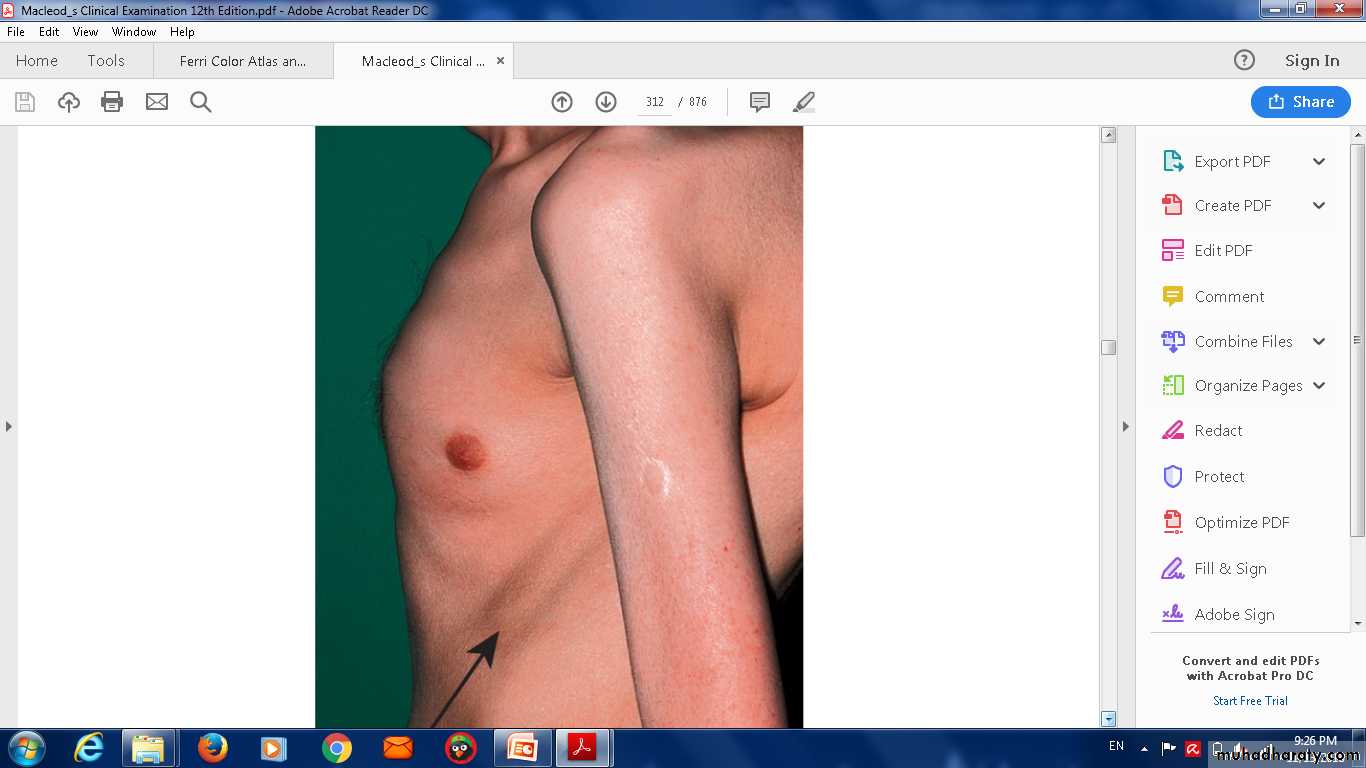
Hyperinflation
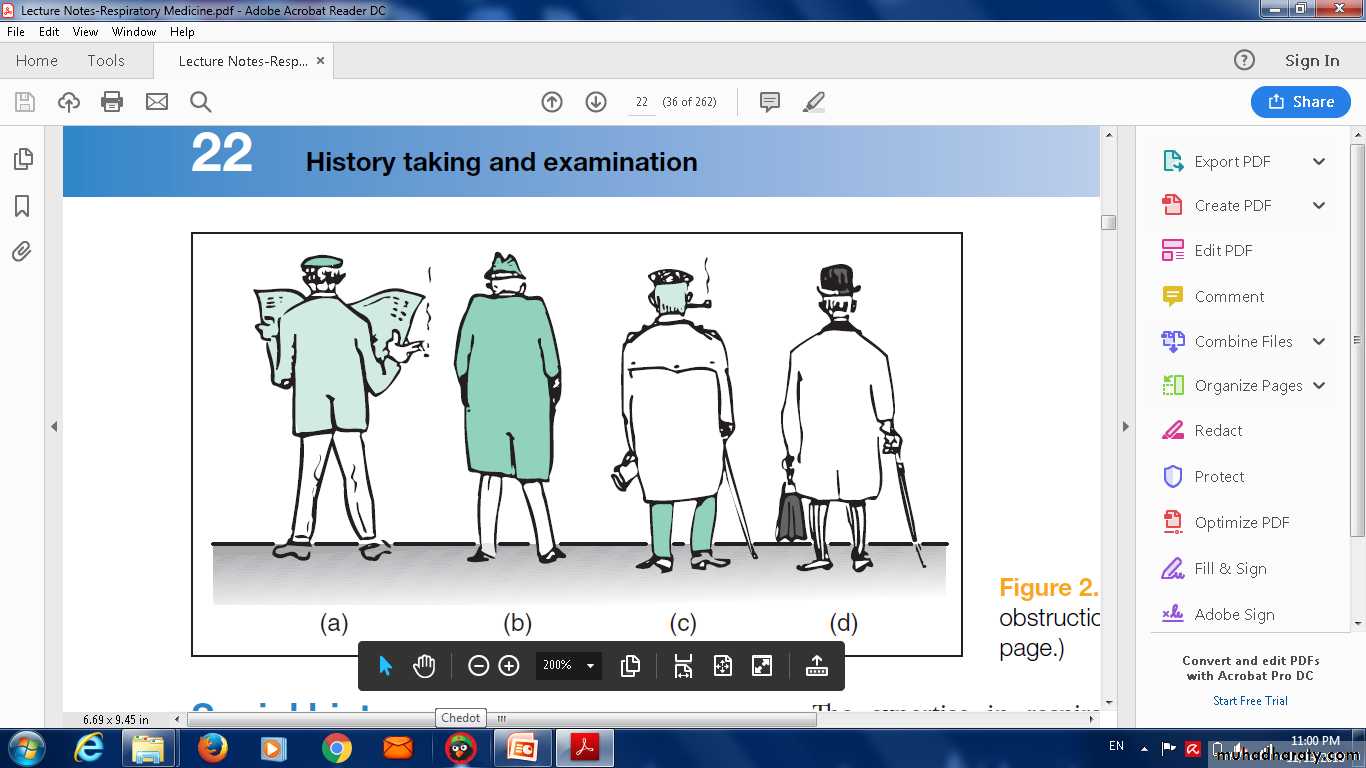
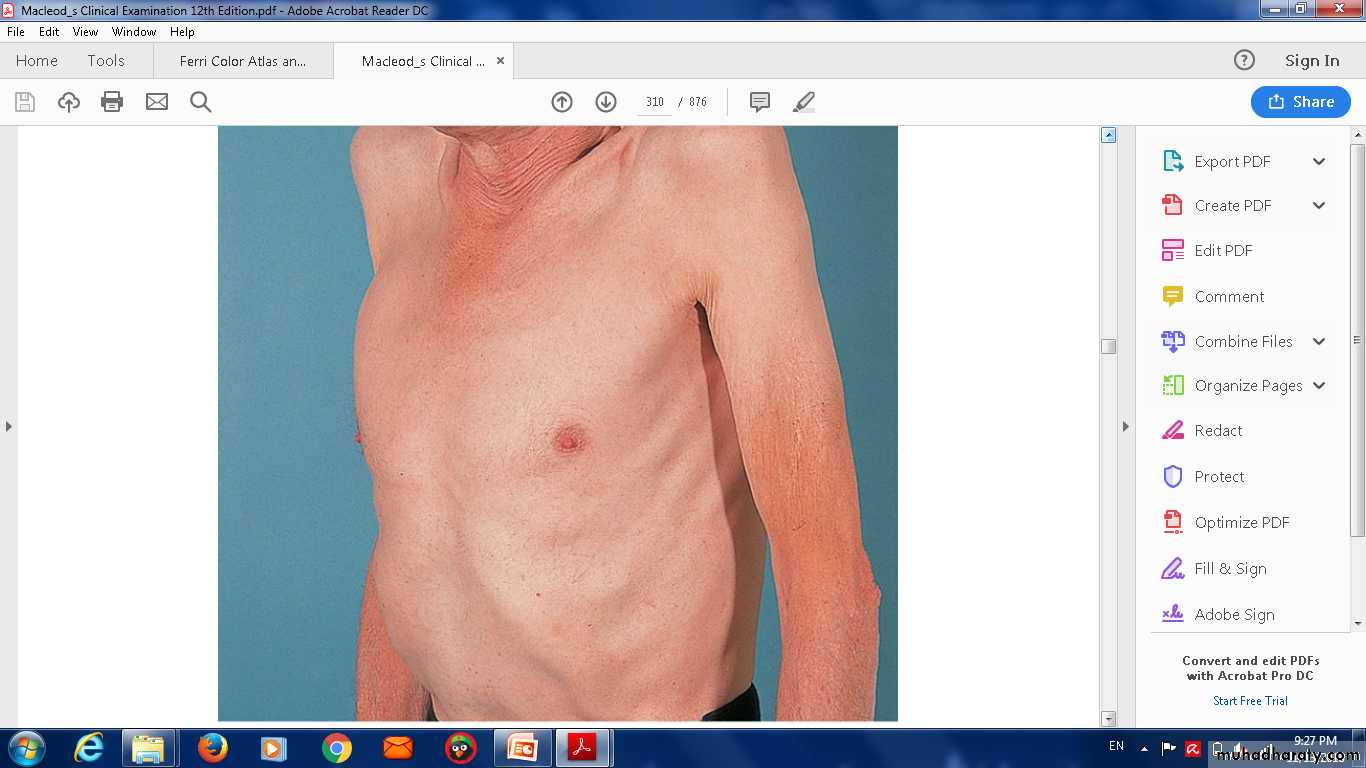
Blue bloater’ (top) and ‘pink puffer’(bottom).
Two classical phenotypes have been described
'pink puffers' are typically thin and breathless, and maintain a normal PaCO2 until the late stage of disease.The 'blue bloaters' develop (or tolerate) hypercapnia earlier and may develop oedema and secondary polycythaemia.
In practice, these phenotypes often overlap.
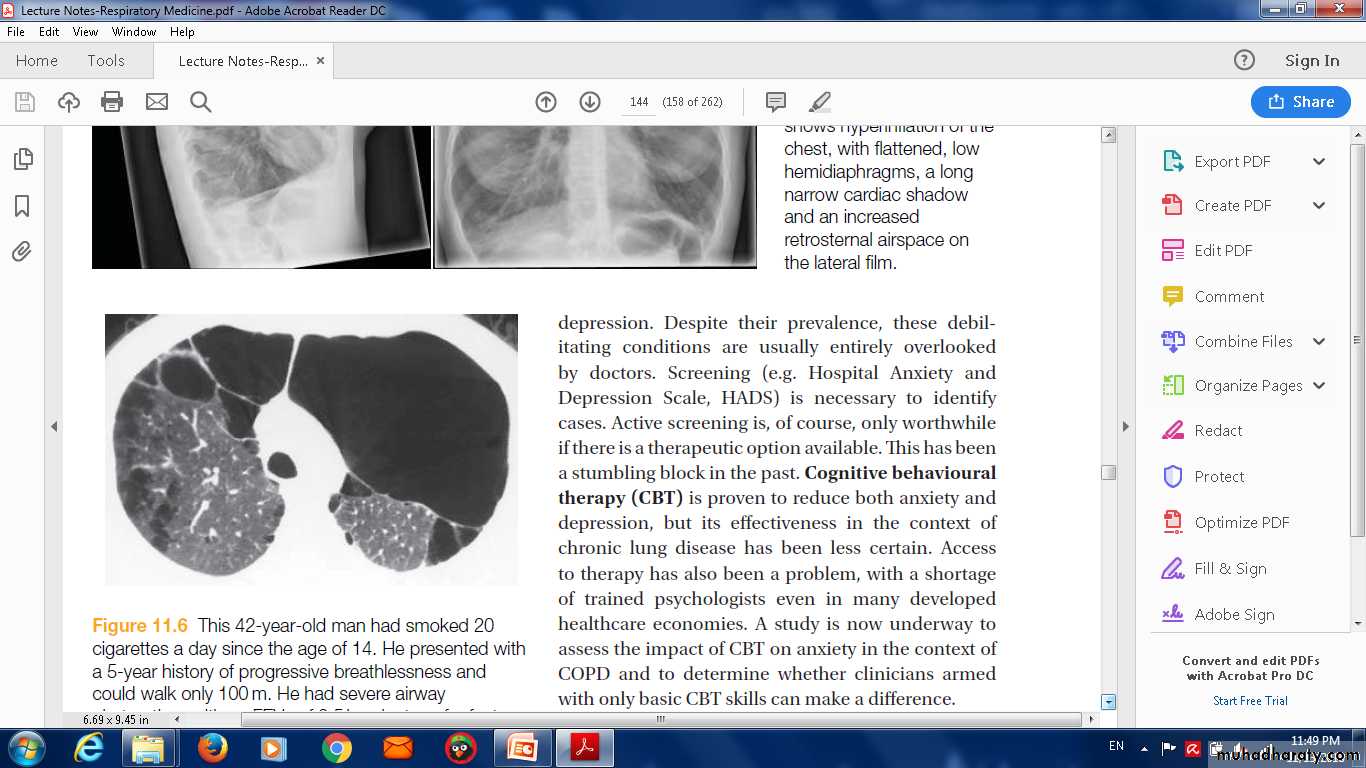
This 42-year-old man had smoked 20 cigarettes a day since the age of 14. He presented with a 5-year history of progressive breathlessness and could walk only 100 m. He had severe airway
obstruction, with an FEV1 of 0.5 l and a transfer factor for carbon monoxide and transfer coefficient reduced to 30% of predicted values. High-resolution CT shows extensive emphysematous bullae with dilated distal airspaces, cysts and destruction of alveolar
architecture. Levels of ????1-antitrypsin were unrecordable.
Investigations
1-a chest X-ray is essential to identify alternative diagnoses such ascardiac failure,
lung cancer.
2-A full blood count is useful to exclude
anaemia.
polycythaemia.
3- α1-antiproteinase younger patients with predominantly basal emphysema,.
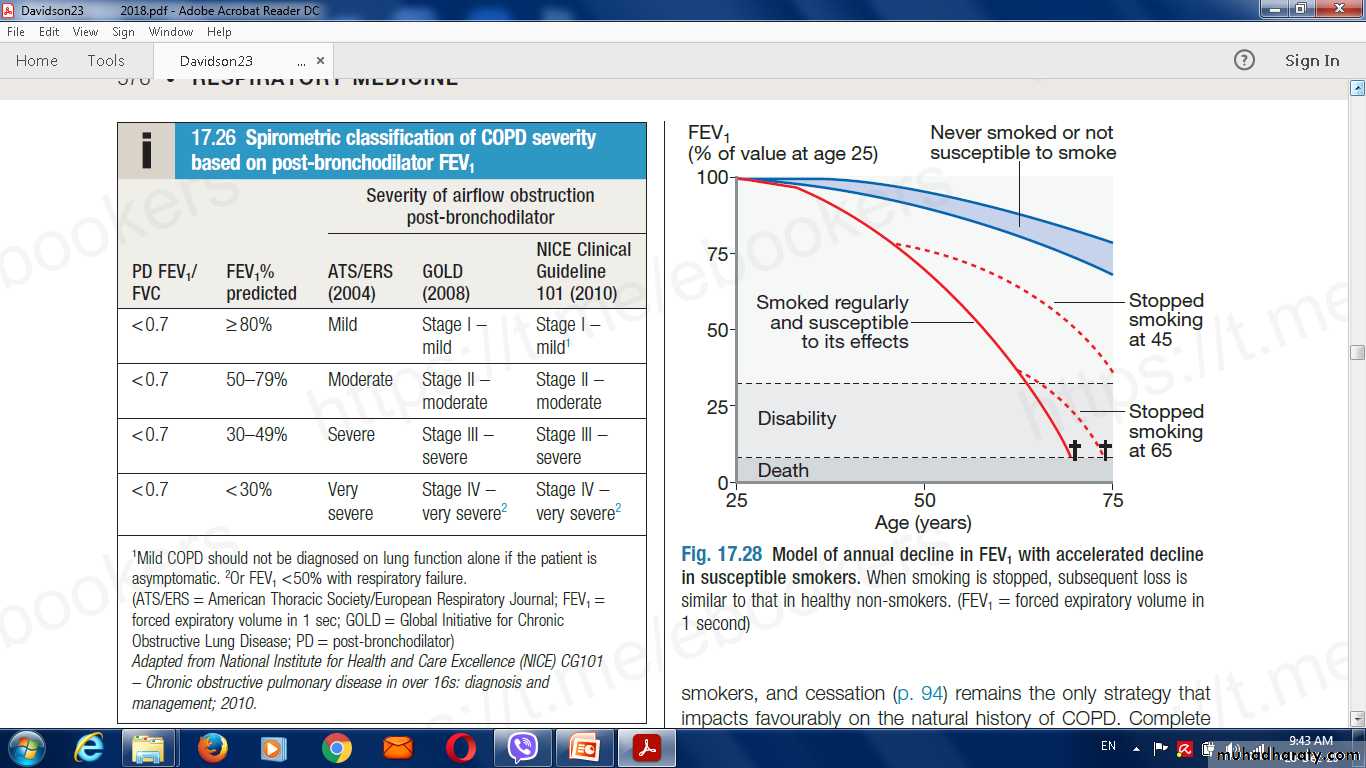
4-Spirometry the post-bronchodilator FEV1 is less than 80% of the predicted value and accompanied by FEV1/FVC < 70%.
5- peak flow low is consistent with COPD .
6-Measurement of lung volumes by body plethysmography.
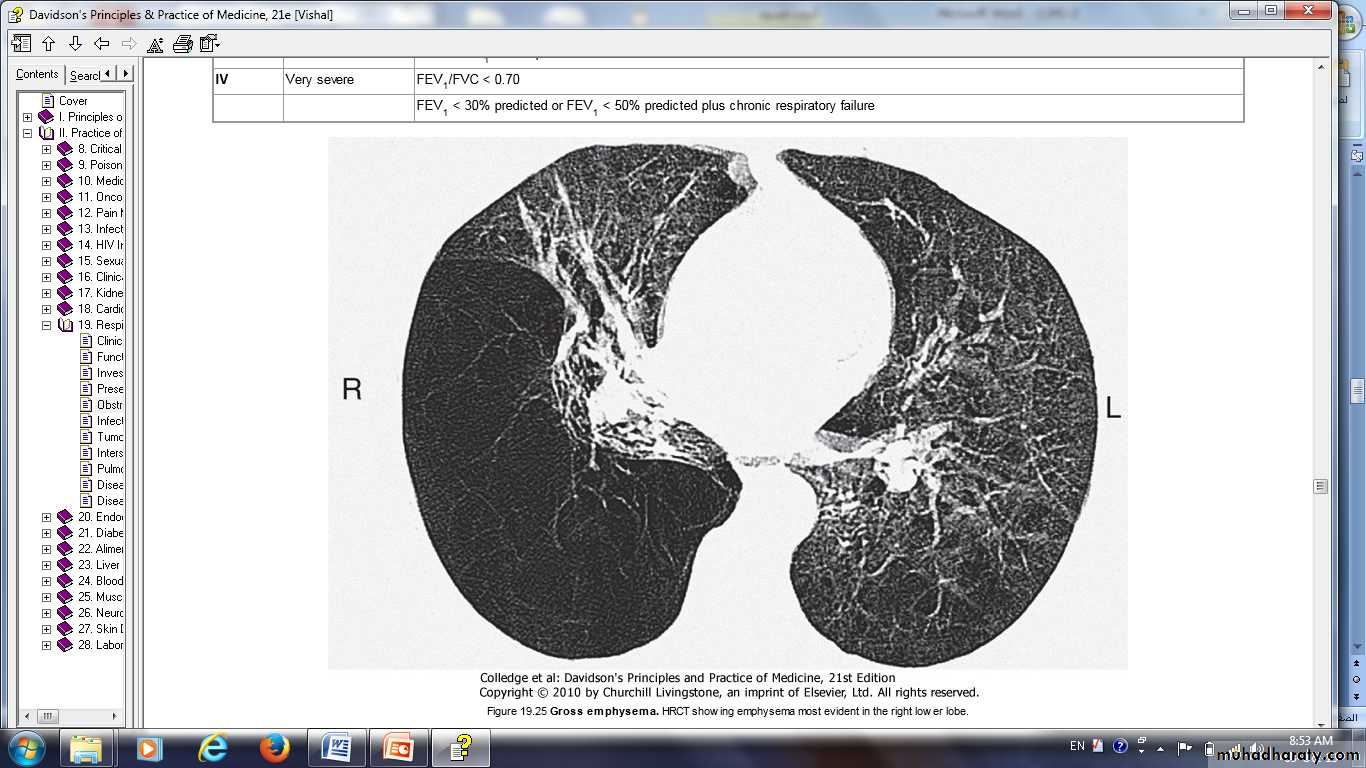
7-The low gas transfer factor suggeste presence of emphysema.
5- Exercise tests.
6- Pulse oximetry
Gross emphysema. HRCT showing emphysema most evident in the right lower lobe.
Management
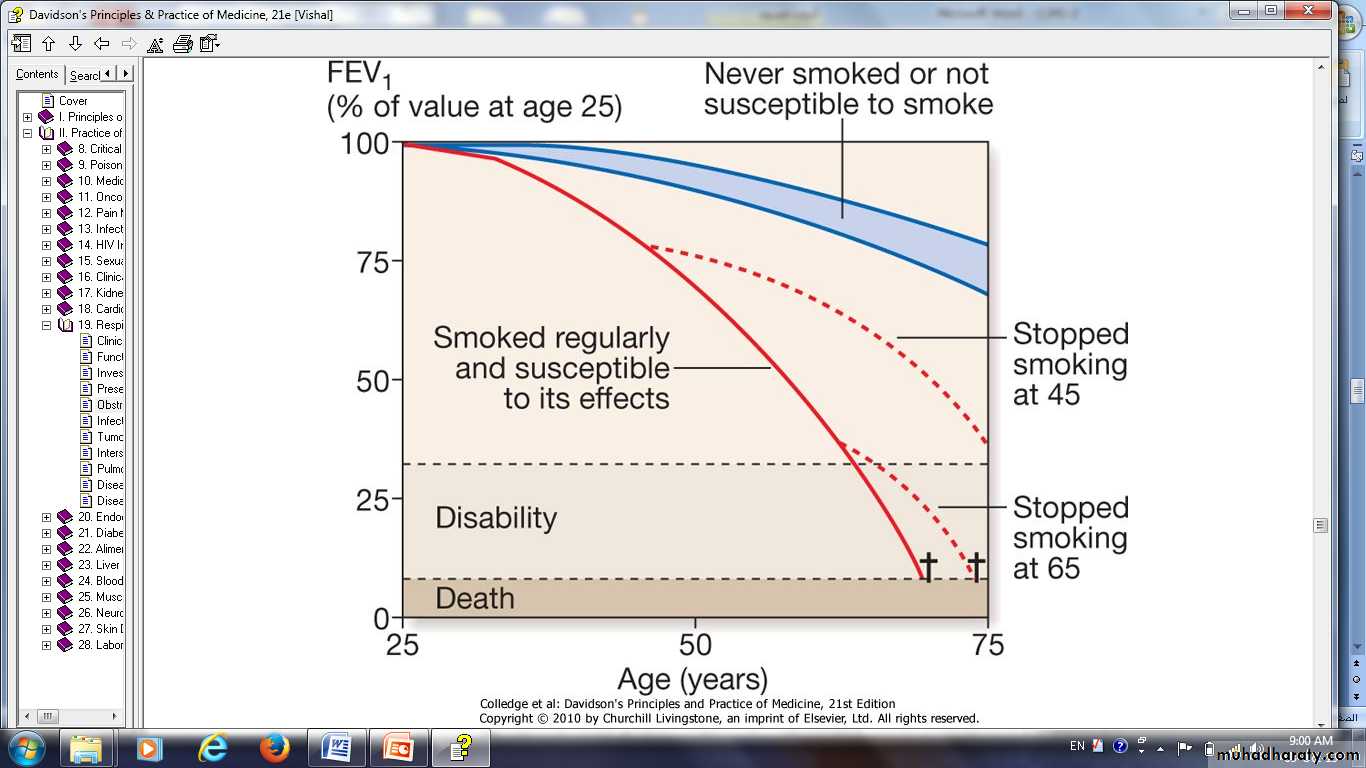
I---Smoking cessation and COPD'Sustained smoking cessation in mild to moderate COPD is accompanied by a reduced decline in FEV1 compared to persistent smokers.'
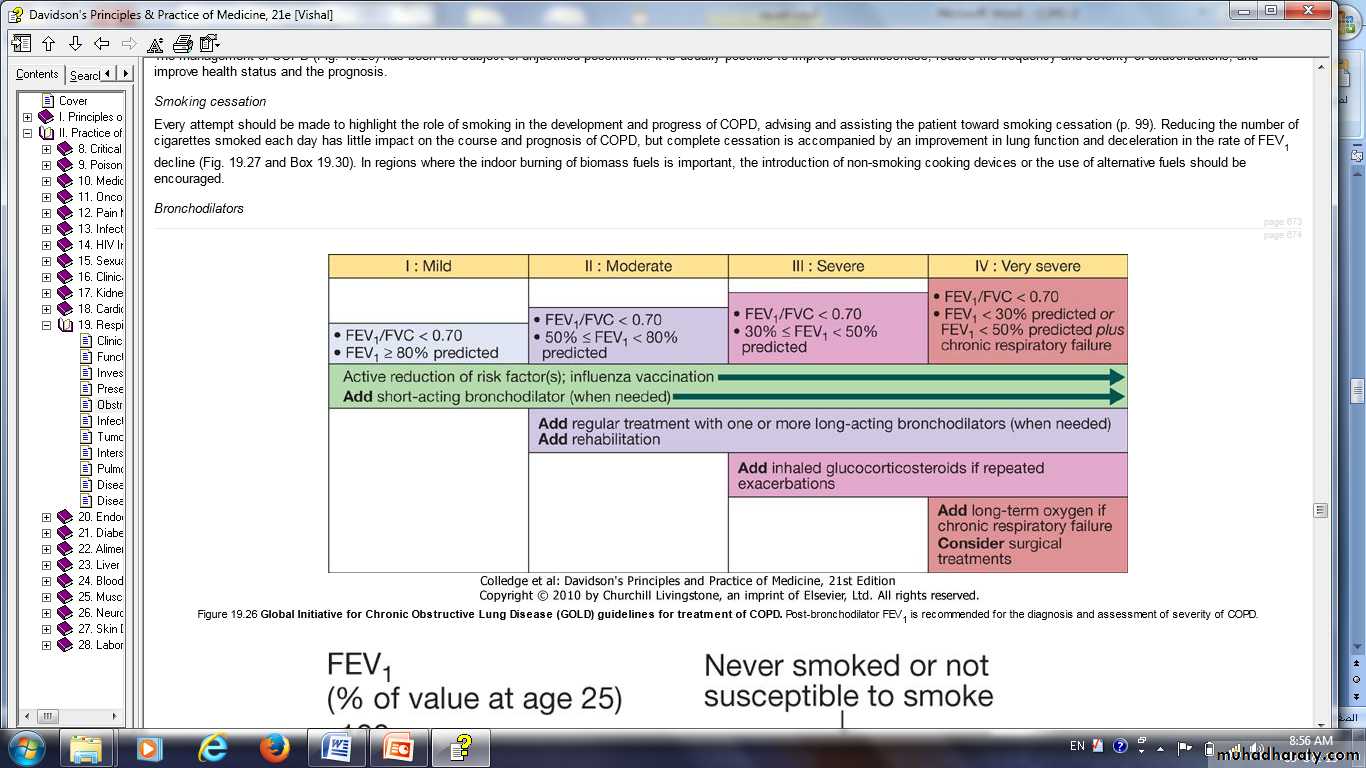
II-Bronchodilator
central to the management of breathlessness.The inhaler
Mild disease.
Short-acting bronchodilators .
β2-agonists salbutamol and terbutaline.
the anticholinergic ipratropium bromide.
moderate to severe disease.
Longer-acting bronchodilators,the β2-agonists salmeterol and formoterol.
the anticholinergic tiotropium bromide.
Oral bronchodilator
.Theophylline preparations improve breathlessness and quality of life,
Bambuterol , a pro-drug of terbutaline, is used on occasion.
phosphodiesterase inhibitors
Corticosteroids
Inhaled corticosteroids (ICS).
SE : Pneumonia
Oral corticosteroids are useful during exacerbations.
Pulmonary rehabilitation
Oxygen therapy Long-term domiciliary oxygen therapy (LTOT)
Arterial blood gases measured in clinically stable patients on optimal medical therapy on at least two occasions 3 weeks apart:
PaO2 < 7.3 kPa (55 mmHg) irrespective of PaCO2 and FEV1 < 1.5 L
PaO2 7.3-8 kPa (55-60 mmHg) plus pulmonary hypertension, peripheral oedema or nocturnal hypoxaemia
patient stopped smoking.
Use at least 15 hours/day at 2-4 L/min to achieve a PaO2 > 8 kPa (60 mmHg) without unacceptable rise in PaCO2.
Surgical intervention
bullectomy.lung volume reduction surgery (LVRS).
Lung transplantation .
Other measures
an annual influenza vaccinationpneumococcal vaccination.
Treat
Obesity.
Poor nutrition.
Depression.
Mucolytic therapy such as acetylcysteine,
Antioxidant agents.
Palliative care
Morphine preparations
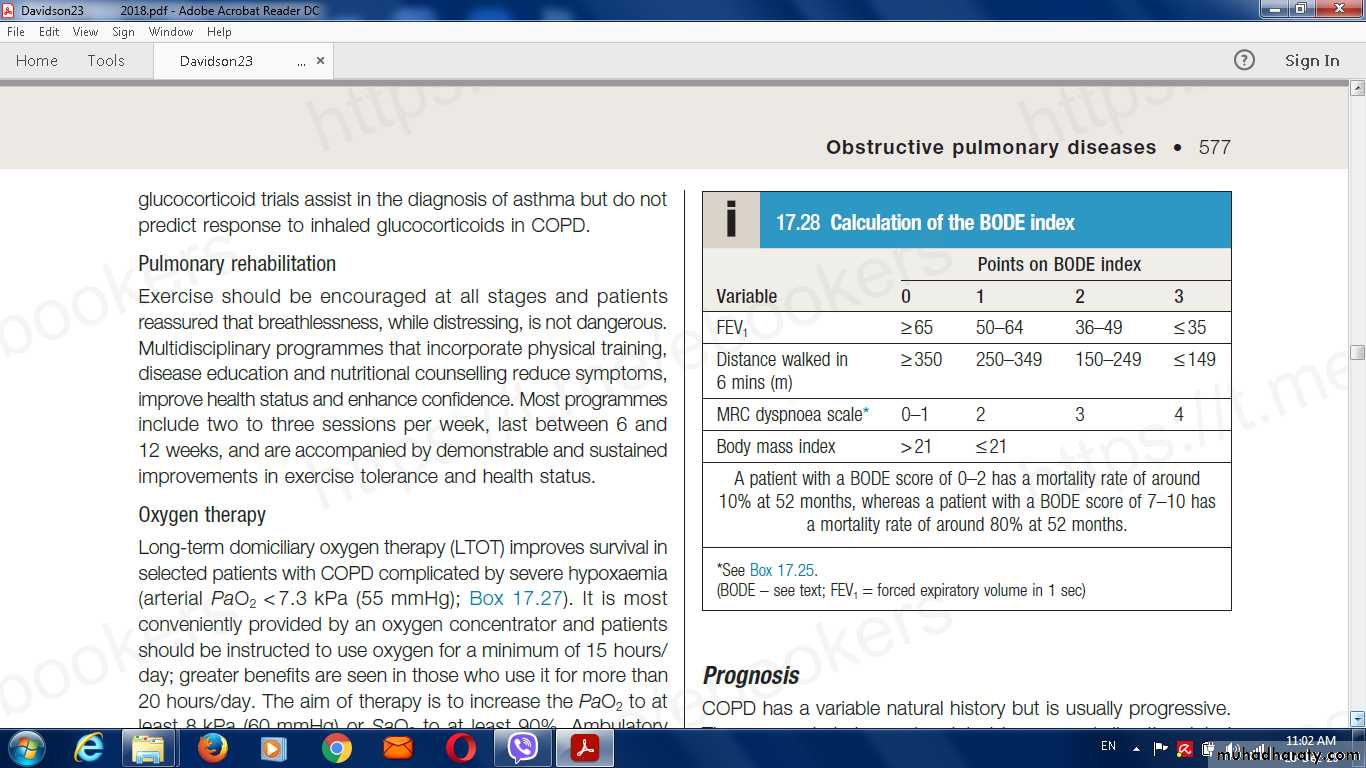
benzodiazepines in low dose may reduce anxiety.Prognosis
COPD usually progressive.
Inversely related to age
Directly related to the post-bronchodilator FEV1.
poor prognostic indicators
Weight loss
Pulmonary hypertension.
A (BODE index) the include following variables
the body mass index (B),the degree of airflow obstruction FEV1 (O),
a measurement of MRC dyspnoea scale (D)
Distance walked in 6 min (m)exercise capacity (E).
Causes of death
Respiratory failure.cardiac disease.
lung cancer.
Acute exacerbations of COPD
Characterised byAn increase in symptoms .
Deterioration in lung function and health status.
are usually triggered by bacteria, viruses or a change in air quality.
Respiratory failure and/or fluid retention and represent an important cause of death.
Indication of refferal to hospital
The presence of cyanosis.
Peripheral oedema.
An alteration in consciousness should prompt referral to hospital.
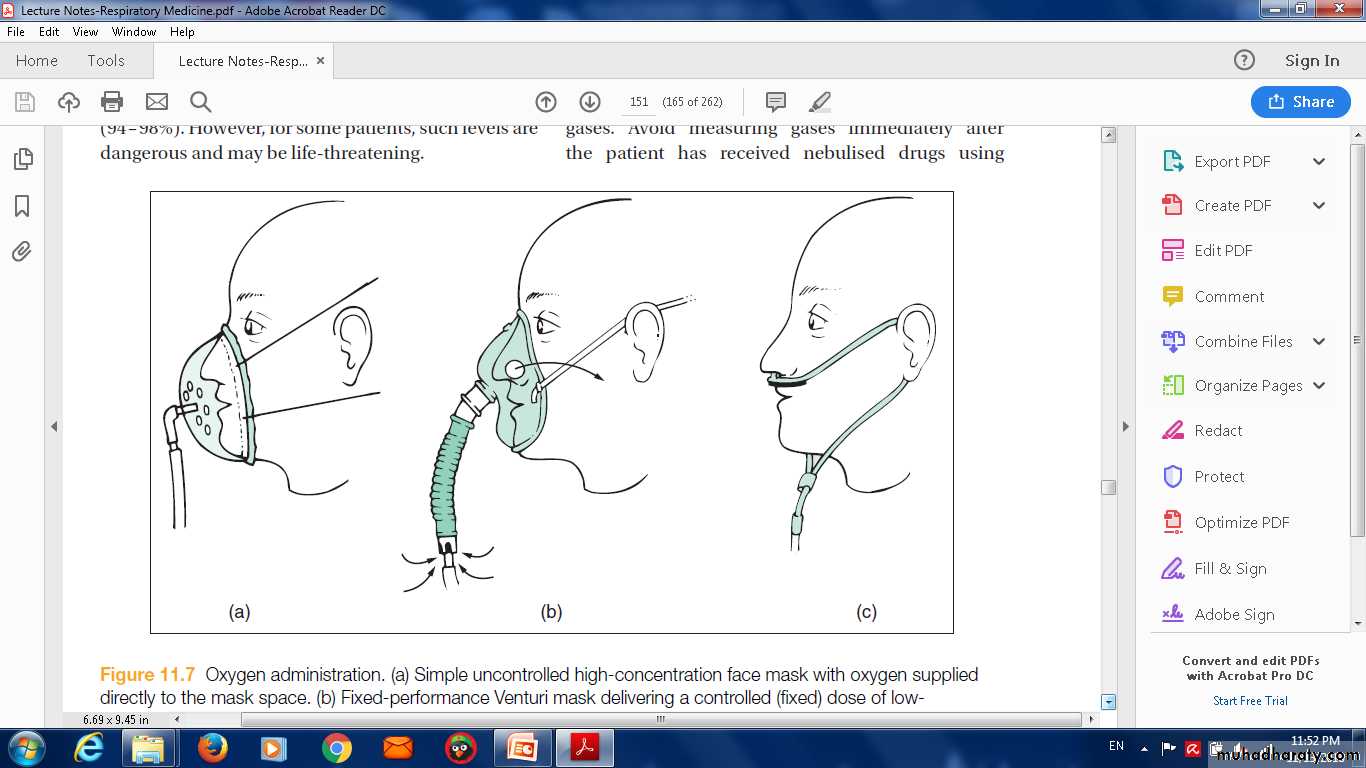
Oxygen therapy
In patients with an exacerbation of severe COPD, high concentrations of oxygen may cause respiratory depression and worsening acidosis.
Controlled oxygen at 24% or 28% should be used with the aim of maintaining a PaO2 > 8 kPa (60 mmHg) (or an SaO2 > 90%) without worsening acidosis.
1-Bronchodilators
Nebulised short-acting β2-agonists combined with an anticholinergic agent (e.g. salbutamol with ipratropium).usually safe to drive nebulisers with oxygen, but if concern nebulisers may be driven by compressed air and supplemental oxygen delivered by nasal cannula.
2-Corticosteroids
Oral prednisolone reduces symptoms and improves lung function.Currently, doses of 30 mg for 10 days are recommended but shorter courses may be acceptable .
Prophylaxis against osteoporosis .
3-Antibiotic therapy
little evidence for the routine administration of antibiotics.They recommended for patients reporting an increase in sputum purulence.
Breathlessness.
Choice
An aminopenicillin
A macrolide.
Co-amoxiclav.
4-Non-invasive ventilation
If, despite the above measures, the patient remains tachypnoeic and acidotic (H+ ≥ 45/pH < 7.35), then NIV should be commenced .
Mechanical ventilation.
5-Additional therapy
peripheral oedema; responds to diuretics.the respiratory stimulant doxapram.
Discharge
clinically stable.THANK YOU
Q
QUIZE