Premalignant condition of the cervix= CIN
Preinvasive disease of cervixProf.dr. Alaa al- Naser
Objectives
1. recognize anatomy and histology of cervix, define SCJ,TZ, understand the changes occur during the reproductive life and metaplastic process.
2. Understand the central role of human papilloma virus in the etiology of cervical intraepithelial neoplasia.
3. Understand the principles of organizing population screening.
4. Be confident about interpreting cervical cytology reports and counseling women accordingly.
The cervix is composed from 2 embryonic sites
From mullerian duct-lined by columnar epithelium.From urogenital plate-lined by stratified squamous epithelium.
(point at which columnar squamous epithelium meet is called as original Sq.-columnar junction which usually at ecto cervix)
The cervix represent the lower cylindrical distal portion of the uterus, it divided into(ectocervix projecting into vagina 3cm length open through an orifice called external os/endocervix luminal cavity within cervix forming a passageway between the external os and internal os which mean the upper limit of endocervical canal =isthmus =transition from the endocervix to endometrium).
Endo cervical canal fusiform shape measure 7-8mm at its widest.
It is composed of stromal ts. Which is lined by squamous epithelium in the vagina(ectocervix) and columnar epithelium whithin the cervical canal(endocervix).
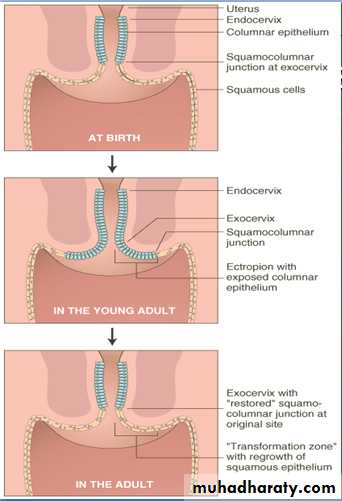
The position of SCJ(meeting of 2 epithelium) changes throughout the reproductive years(uterine growth, cervical enlargement and hormonal status).
At birth and premenarchal years, it lies at or very close to the external os
At puberty and pregnancy is located at variable distances from external os. .(an eversion onto the ectocervix of theSCJ along with large portions of columnar epithelium is referred as ectropian, through the process of metaplasia the ectropian is replaced by meta plastic squamous epithelium)
Metaplasia is a reaction of the exposed evereted columnar epithelium(ectropian) to irritation by acidic vaginal enviromrnt.
In postmenopausal woman SCJ is not visible and receded into endocervix.
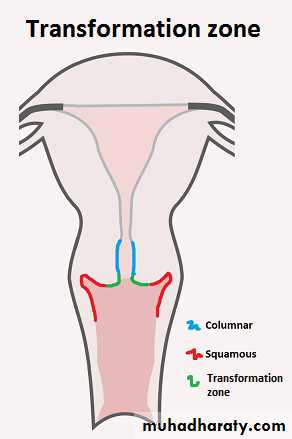
Transformation zone:
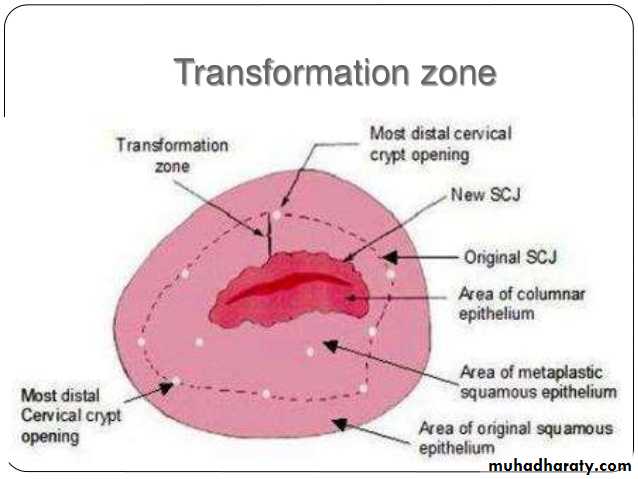
Is an important area on the cervix which is defined as the area where the original SCJ was to the current SCJ and includes area of metaplasia.
When the mucous columunar epithelium is covered by squamous epithelium there is retention of mucus this is called a nabothian follicle
.
The transformation zone is the site where pre-malignancy and malignancy develop.
Metaplasia: change of normal type of epith. to another also normal. It is physiological process the columnar epithelium change to Sq . one in response to acid environment of the vagina.Dysplasia : change normal type epithelium to abnormal one. It is histological term describing architectural abnormalities with in tissue(mild, moderate, sever)
Hypertrophy : increased in the size of cell.
Hyperplasia : increased in the number of cells.
Dyskaryosis : cytological term describe nuclear abnormalities not synonymous with dysplasia.
Benign disease of cervix(cervical erosion, ectropian, tears, cyst endometriotic cyst, nabothianand mesonephric cyst, endocervical plop, inflammatory conditions of cervix).
CERVICAL INTRAEPITHELIAL NEOPLASIA
CIN is premalignant disease of the cervix=cervical dysplasia or cervical interstitial neoplasia, it is not cancer and usually curable, most cases remain stable or eliminated by host immune system, small % progress to cervical cancer.
mild, moderate, and severe dysplasia were the terms used to describe premalignant squamous cervical cellular changes. This nomenclature, although still in use, has generally been replaced by the term CIN, which is used to describe histologic changes (those detected with biopsy). CIN has 3 grades:
CIN 1 is considered a low grade lesion. It refers to mildly atypical cellular changes in the lower third of the epithelium (formerly called mild dysplasia). HPV viral cytopathic effect (koilocytotic atypia) is often present.
CIN 2 is considered a high grade lesion. It refers to moderately atypical cellular changes confined to the basal two-thirds of the epithelium (formerly called moderate dysplasia) with preservation of epithelial maturation.
CIN 3 is also considered a high grade lesion. It refers to severely atypical cellular changes encompassing greater than two-thirds of the epithelial thickness, and includes full-thickness lesions (formerly called severe dysplasia or carcinoma in situ)
Cytological finding of dysplasia
1.increased nuclear cytoplasmic ratio.
2. Increased mitotic figure.
3.isopokilocytosis different size and shape of cells
4.dysarrangment of cell.
5.hypervascularization reflect malignancy.
LSIL is equivalent to CIN1 and HSIL comprises either CIN 2 or 3. When HSIL terms are used
INCIDENCE — The estimated annual incidence of CIN among women who undergo cervical cancer screening is 4 percent for CIN 1 and 5 percent for CIN 2,3.
The sq. epithelium of cervix appears as a featureless, smooth, pale pink surface, blood vessels below this layer not visible(colposcopy).
The columnar epithelium is k.k by infolding or cleft and referred as glandular(not true gland).
Squamocolumnar junction
During emberyogenesis junction upward migration of stratified squamous epithelium from urogenital sinus and vaginal plate to replace mullerian epithelium, this process usually end at sq. columnar junction, the location of SCJ vary with age, hormonal status, it evert outward during adolescent pregnancy and OCCP. It regress to endocervical canal in menapouse, prolong lactation, use of minipills.
The rise in estrogen at puberty lead to glycogenation of non keratinized sq. epith. glycogen provide CHO sourse to lactobacilli(lacticacid lower PH), the exposure of columnar epith. to low PH lead to sq. metaplasia, this occure at SCJ forming a transformation zone TZ nearly all neoplasia occure at TZ (velnerable to oncogenic virus)
,
ROLE OF HUMAN PAPILLOMAVIRUS
sexual activity as the dominant risk factor for occurrence of cervical neoplasia; cervical cancer and its precursors are almost nonexistent in women who have not had any sexual relationship. The major factor causing these disorders is infection with the human papillomavirus (HPV) The association between HPV and cervical neoplasia is so strong that most other behavioral, sexual, and socioeconomic covariables have been found to be dependent upon HPV infection.
Most HPV infections occur in young women and are transient, over 50 percent of new infections are cleared in 6 to 18 months, and 80 to 90 percent will have resolved within two to five years.
Latent infection without physical, cytological, or histological manifestations.
Actively replicating HPV produces characteristic cellular changes, such as nuclear enlargement, multinucleation, hyperchromasia, and perinuclear cytoplasmic clearing (halos). On average, these changes occur two to eight months after the woman is first infected.
Factors associated with development of high grade lesions and cancer
1. Environmental factors (eg, cigarette smoking).
2. immunologic influences also appear to play a role3. Subtype — There are over 100 HPV subtypes; approximately 40 types are specific for the anogenital epithelium and have varying potentials to cause malignant change.
Low-risk subtypes, such as HPV 6 and 11, do not integrate into the host genome and only cause low grade lesions (eg, LSIL and CIN 1) and benign condylomatous genital warts.
High risk HPV subtypes, such as 16 and 18, are strongly associated with high grade lesions (HSIL and CIN 2,3), persistence, and progression to invasive cancer
clinical laboratories report HPV tests as either "positive," meaning one or more high risk oncogenic subtypes was detected or "negative," meaning none of the high risk HPV types that the laboratory tested for was detected.
Persistence
Persistent infection with high oncogenic risk HPV subtypes is a key factor in development of high grade cervical lesions and cervical cancer, while clearance of HPV infection predicts regression of CIN. A persistent HPV infection is variably defined as one that is present at least 6 to 12 monthspersistence is related to several factors
Older age ,Viral load, Molecular mechanism ,host's immune system.
Risk factors for cervical neoplasia
1.age median age for ca. cervix is middle to late forties, decade later than CIN. HPV in old age tend to be persistant, more mutation, lack the need for prenatal screening,contraception.2.behavior infrequent or abscent cancer screening pap smear, early coitrache, multiple sexual partner, male partner promiscuity.
3.tobacco smoking increase the risk of ca.cervix among HPV positive , nicotine and its metabolite found in the semen of men how smoke and in the cervical mucus, cause neoplastic changes, also smoking at menarche causing such.
4.dietary deficiency of cetain vitamins like A,C,E,beta carotene and folic acid.
5.Immunosuppression , immunosup. therapy.
6.Herpes simplex virus and chlamydia.
7.COCCP, parity increase parity cause neoplasia(truma during delivery).
8. Familial, dietary, and endogenous hormonal factors
9.inadquet screening
Prevention
1.behavioral intervention(sex. abstinence, delaying coitrache, limiting sex. Partner)
2.condoms
3.vaccines(prophylactic or therapeutic vaccines)
4.Screening program
3years after onset of vaginal intercourse, no later than age 21.
Introduction of screening
Age <30 anuual
Age >30 every 2-3 years after 3- negative sample
Screen intervals for woman at average risk
HIV or other immune compremised state: 2 test in the first year then anuualy
Screening interval at high risk women
Age 70 if 3 negative result in prior 10 years, continue if screen hx. Uncertain, hx. Of cervical cancer,DES, recentHPV, HIV, other immunocopremised conditions
Discontinuation of screen
Not indicated if removal confirmed for benign indication, STAH, DES, hx. Of cervical cancer continue screening
Screening after hysterectomy
DIAGNOSIS
1. The Pap test aims to identify abnormal cells sampled from the transformation zone, the junction of the ecto- and endocervix, where cervical dysplasia and cancers arise, using wooden spatula and place on glass slide and fixed. This was examined by a cytologist for the immature squamous cells sheds from area of CIN.Liquid base cytology small brush is used to sample cells from TZ, then brush head place in fixative spun dowen and read by cytologist(N=small nuclieflattened and pyknotic, Abn= large nuclei, cytological atypia and high N/C ratio.
Abnormal smear show cells in different degree of maturity(dyskaryosis).
2.HPV testing: detection of HPV in serum, high risk subtypes.
3.Colposcopy: inspection of cervix with low powered microscope,magnified cervix 4-20 times. Inspection cervix and vasculature,use green filter abnormal vascularity includes punctuation and mosaicism.
Acetic acid test 3% stained(nucleoprotein coagulate by acetic acid) the abnormal area the degree of staining correlate with severity due to increased turn over.
Schiller test application of lugols iodine stain normal cervix brown, lack intracellular glycoprotein glycogen stained yellow.
Colposcopy give clinical diagnosis
Punch biopsy from abnormal area gives a histopathlogical dx.
4.Biopsy
MANAGEMENT
The aim of treatment is to make the post treatment negative test negative while minimizing harm to patient.
There are two general management approaches to CIN: expectant versus immediate treatment
Management of CIN is based upon correlation of the cervical cytology findings, colposcopic impression, cervical biopsy results, and individual patient characteristics, such as age, pregnancy, and the likelihood of compliance with treatment recommendations. Since treatment can adversely affect future pregnancy outcome, this risk also needs to be considered when deciding upon an interventional or expectant approach.
Treatment is never performed based upon a cytologic diagnosis alone, but is sometimes initiated at the time of colposcopy/biopsy in women who are at high risk of loss to follow-up.
Ablation and excision — There are two general approaches to treatment of CIN: ablative methods (eg, cryotherapy or laser ablation) and excisional methods (eg, cold knife [scalpel] or laser conization, loop electrosurgical excision {LEEP, LLETZ}.
See-and-treat protocols — See-and-treat protocols are performed in an office excisional procedure in at-risk populations based upon findings at colposcopy, rather than having the patient await biopsy results and make a return visit.
1. high risk adult patient
2. high grade cytology corresponding to colposcopic finding
3. unsatisfactory colposcopy.
4. recommended to exclude presence of occult high grade CIN or invasive cancer.
This approach is an attempt to lower the 20 to 40 percent loss-to-follow-up rate with the traditional multi-visit management of CIN.
The see-and-treat approach appears to be most valuable in women with high grade lesions in whom reliable follow-up is compromised and overtreatment is least likely.
Other treatments — such techniques include photodynamic therapy, cyclooxygenase-2 inhibitors, vaccines, and environmental alterations, use of topical agents (eg, difluoromethylornithine, all-trans retinoic acid, and oral agents.Topical treatment of CIN with cidofovir.
CIN 1 can be observed indefiniteiy, especially in adolescents, or treated if it is persists for at least 2 year. This is also the case for CIN 2 lesion in adolescents. However CIN 2 in adult women and CIN 3 are treated by excision or ablation except in special circumstances.
Hysterectomy is unacceptable as primary therapy for CIN 1, 2 OR 3. However it may be considered:
1. Conization margin positive for CIN2,3 specially if complete child bearing and expected poor compliance and follow up.
2. Repeat excisional biopsy not feasible or scarred cervix or vagina, considering performing frozen core in order to avoid performing in appropriate simple hysterectomy in patient with occult invasive cancer.
3. Presence of coexistence pathology required hysterectomy.
4. patient request.
5. Persistent or recurrent CIN2,3.