5th stage Dr.Khalid Ali Orthopaedics
Dislocation of the Shoulder JointThe shoulder joint is a ball-and-socket joint. The ball is on the top of the arm bone (the humorous), and this fits into a socket of the shoulder blade (the scapula) called the glenoid.
No joint in the body allows more motion than the shoulder joint. Unfortunately, the shoulder is not as stable as other joints.
Of the large joints, the shoulder is the one that most commonly dislocates:
Shallowness of the glenoid socket.
Extremely wide range of movements.
Traumatic dislocation of the shoulder is exceedingly rare in children.
Types:
1. Anterior: the head of humerus lie infront of glenoid. (˃ 95%).2. Posterior: the head of humerus lie behind the glenoid. (˂ 2%).
3. Inferior: the head of humerus lie beneath the glenoid. (LuxatioErecta). Extremely rare
Mechanism: It usually occurs due to fall on the hand. The head of humerus will displace forward tearing the capsule and producing avulsion of the glenoid labrum (Bankart lesion).
The posterolateral part of the head of humerus may be crushed by the anterior edge of the glenoid, with repeated dislocations; an excavation may be formed in the back of the head (Hill-Sachs lesion) shoulder instability
Clinical Features: there is severe pain, the patient supports the arm with the opposite hand with slight abduction, and never permit any kind of examination. The outer shoulder contour is flattened, and a bulge may be felt just below the clavicle.
X-ray: AP view usually show the head of humerus lying below and medial to the glenoid fossa.
Treatment:
REDUCTIONBefore reduction
the limb must be examined for any nerve and vessel injury. Then closed reduction must be done as early as possible.
Axillary Nerve at great risk.
Closed reduction:
under sedation and occasionally under GA.:
Stimson’s technique: the patient is left prone with the arm hanging over the side of the bed. After 20-30 minutes shoulder may reduce.
Hippocrate method: increasing traction is applied to the arm with the shoulder in abduction, while the assistant applies firm counter-traction.
Sitting on a well-padded chair and gentle traction of the arm over the back of the chair.
In a patient with previous dislocation, simple traction on the arm may be successful.
Kocher’ method: it carries risk of vessel, nerve and bone injury and it is not recommended. the elbow bent to 90 degrees then arm is gradually externally rotated without traction then lifted forwards followed by medial rotation.
After reduction:
X-ray is taken to confirm the reduction and exclude a fracture.Assess the peripheral pulse.
When the patient fully awake, active abduction is gently tested for an axillary nerve injury and rotator cuff tear.
Examination for other peripheral nerve (median, radial, ulnar, and musculocutaneous nerves).
The arm is rested in a sling for about three weeks in patient under 30-yearold (most prone to recurrent dislocation), and for a week or two for patient over 30-year-old (most prone to stiffness).
Complications:
Early:
Rotator cuff tear.
Nerve injury: the axillary nerve.
Vascular injury: axillary artery.
Fracture dislocation.
Late:
Shoulder stiffness.
Unreduced dislocation: up to 6 weeks, closed reduction. After 6 weeks open reduction is indicated only in young patient. In elderly patient ‘Active neglect’ is a better option.
Recurrent dislocation or recurrent subluxation (instability).
Posterior shoulder dislocation
It is rare accounting for less than 2% of cases. It can be caused by indirect force producing severe internal rotation and adduction, as in fit or electric shock. It may be caused by direct force as a direct blow to the front of the shoulder or fall on an outstretched hand.Diagnosis:
it is frequently missed; about two thirds of cases are not diagnosed initially. The main clinical sign, the arm is held in internal rotation and is locked in this position.
In x-ray the AP view show the humeral head is medially rotated, looks abnormal in shape (like an electric light bulb), and it stands away somewhat from the glenoid fossa (the ‘empty glenoid’ sign). The lateral or axillary view is necessary for diagnosis and sometimes CT scan is indicated to confirm the diagnosis.
Treatment:
the acute dislocation can be reduced by closed method: pulling on the arm with the shoulder in adduction for few minutes and then the arm gently rotated laterally, while the humeral head pushed forwards.Inferior shoulder dislocation
(LuxatioErecta)
It is rare, occurs due to a hyper-abduction force, pushing the humeral head out of its socket into the axilla.
Diagnosis:
The starling picture is often diagnostic: the patient’s arm locked in almost full abduction.It is very important to look for associated fractures or neurovascular injury.
The x-ray show that the humeral shaft is in abduction position with humeral head sitting below the glenoid.
Treatment: It can be reduced by pulling upwards in the line of the abducted arm, with countertraction.
Sternoclavicular Joint Dislocation
SCJ can be sprained, subluxed, or dislocated.It is uncommon injury:
Anterior type: caused by lateral compression of the shoulders.
Posterior type: rare, it follows a direct blow to the front of the joint.
Clinical Features:
Anterior dislocation: prominent lump over the sternoclavicular joint. The condition is painful but not serious.Posterior dislocation: it is rare but serious, it might cause compression on the trachea or large vessels, causing venous congestion of the neck and arm.
X-ray:may be difficult to interpret, although the condition is obvious clinically. CT scan is the ideal method.
Treatment:
Anterior dislocation: The joint can be reduced by closed method. Surgery is very dangerous and not necessary.
Posterior dislocation: It should be reduced as soon as possible. Patient lying supine and apply traction on the shoulder with the arm abducted and extended, the joint reduces with snap.
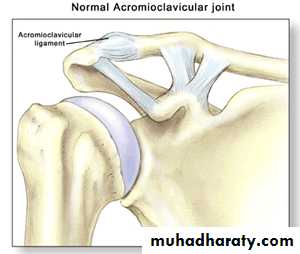
Dislocations in the Acromioclavicular joint
An AC joint injury is an injury to the ligaments that hold the acromioclavicular joint together.
Acute injury to ACJ is common and usually follows direct trauma or fall on the shoulder with the arm adducted.
Pathological Anatomy:
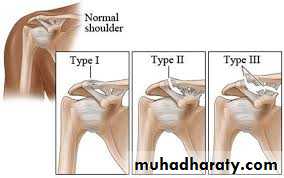
Strain or tear of the acromioclavicular ligament may lead to subluxation of the ACJ. But, if the coracoclavicular ligament also torn, this will lead to complete dislocation of the joint creating a visible and palpable ‘step’.
Clinical Features:
There is localized pain, which will be worse when trying to move the arm above the shoulder. Tenderness, and bruising over the joint. Prominent “step”.X-ray:
AP view with cephalic tilt and axillary view are advisable. Stress view sometimes necessary.
Treatment:
Strain and subluxation need only arm sling, analgesia, and early exercises.
Surgical treatment: if there is complete joint dislocation.
Surgery: Reduction, Holding, Ligaments reconstruction.
Complications:
Supraspinatous tendinitis.
Unreduced dislocation.
Ossification of coracoclavicular ligament.
Secondary osteoarthritis.
Scapulothoracic Dissociation:
It is a high energy injury, the scapula and arm are wrenched away from the chest, rupturing the subclavian vessels and brachial plexus. Many patients die.Clinical features: the patient may be shocked with flail ischemic limb. There is swelling above the clavicle from the expanding haematoma.
X-ray: Distraction of more than 1 cm of a fractured clavicle should give rise to suspicion of this injury.
Treatment: the priority is for patient resuscitation. The outcome of the limb is very poor.