بسم الله الرحمن الرحيم
Respiratory medicine
2ed lecture ((2020-2021))
RESPIRATORY FAILURE
ObjectivesFamiliar with R F
Causes of R F.
Clinical presentation of R F.
Management of R F.
To know the epidemiology ,
Etiology.pathogenesis .
clinical presentation .
investigation .
diagnosis .
treatment .
complication .
Prognosis.
Respiratory failure
The term respiratory failure is used when pulmonary gas exchange fails to maintain normal arterial oxygen and carbon dioxide levels.
Its classification into types I and II relates to the absence or presence of hypercapnia (raised PaCO2).
The exact incidence of ALI/ARDS is not
known; its annual mortality rate has beenestimated to be .30 000 patients per year
in the USA.
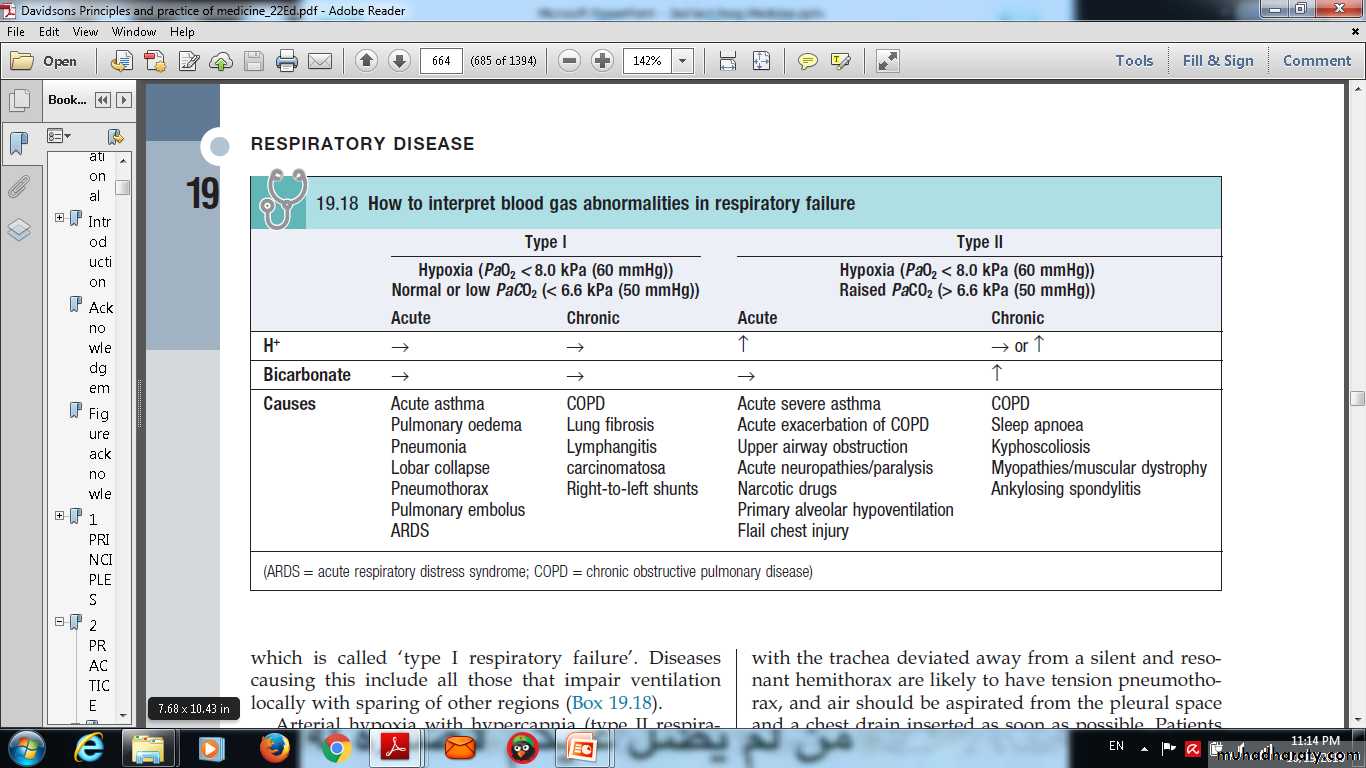
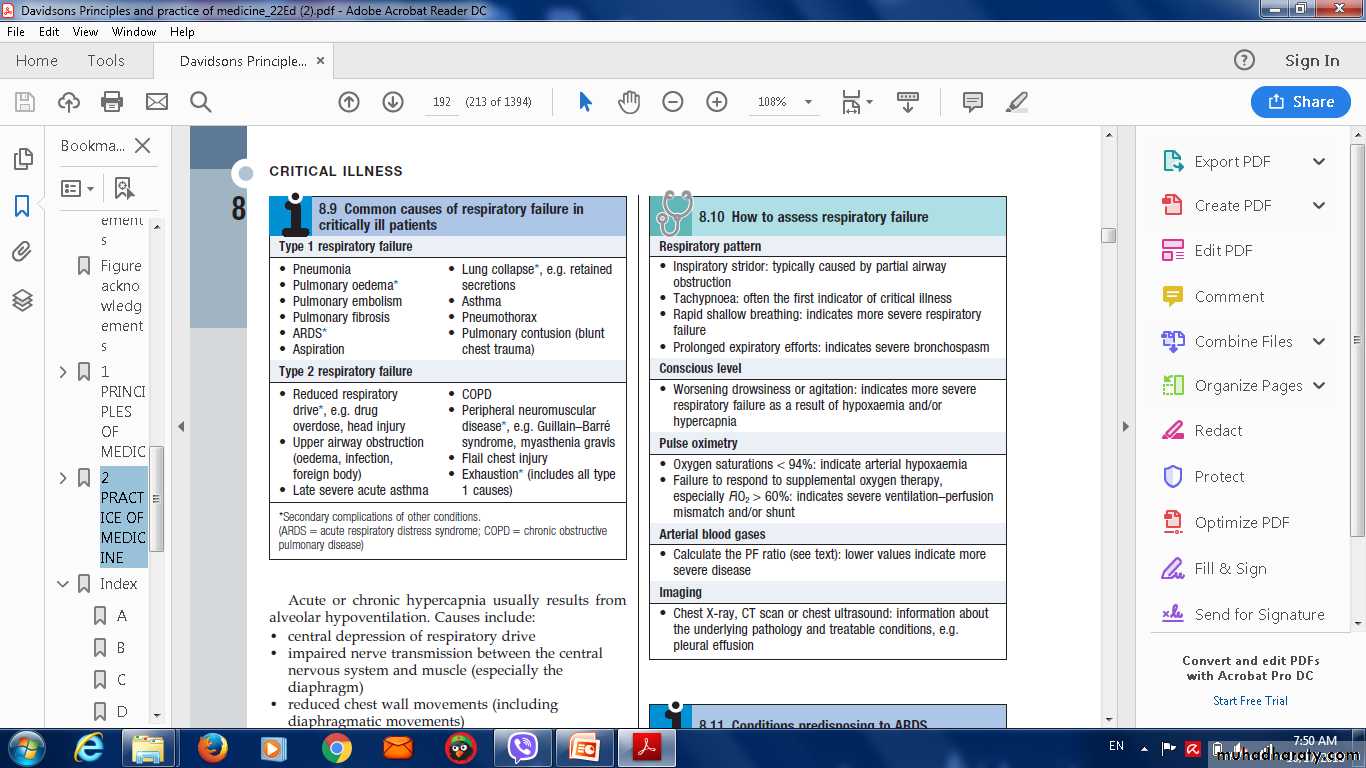
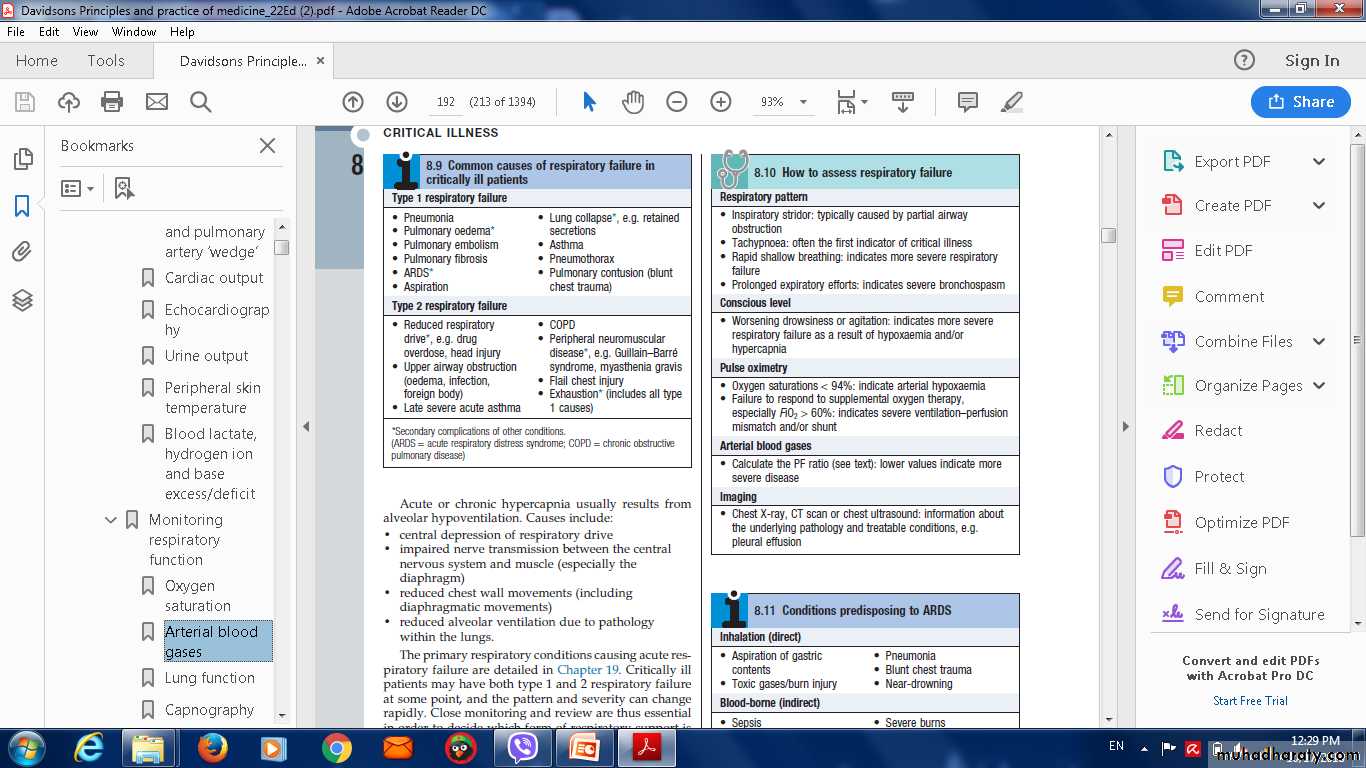
Types , features , causes of respiratory failure
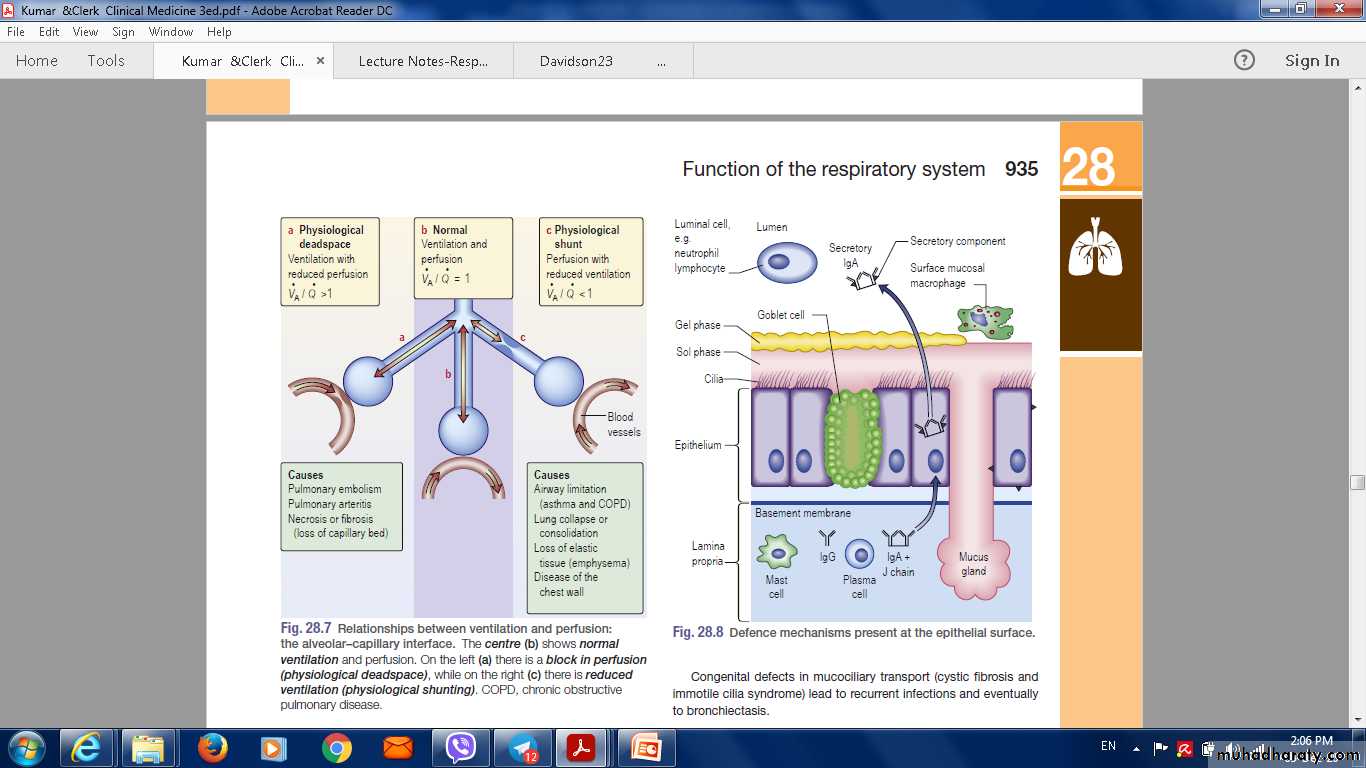
Ventilation perifusion relation
Pathophysiology Type I Respiratory failure
Disease impairs ventilation of part of a lung (e.g. in asthma or pneumonia),perfusion of that region results in hypoxic and CO2-laden blood entering the pulmonary veins.
Increased ventilation of neighbouring regions of normal lung can increase CO2 excretion, correcting arterial CO2 to normal, but cannot augment oxygen uptake because the haemoglobin flowing through these regions is already fully saturated.
Admixture of blood from the underventilated and normal regions thus results in hypoxia with normocapnia,
Diseases causing this include all those that impair ventilation locally with sparing of other regions .
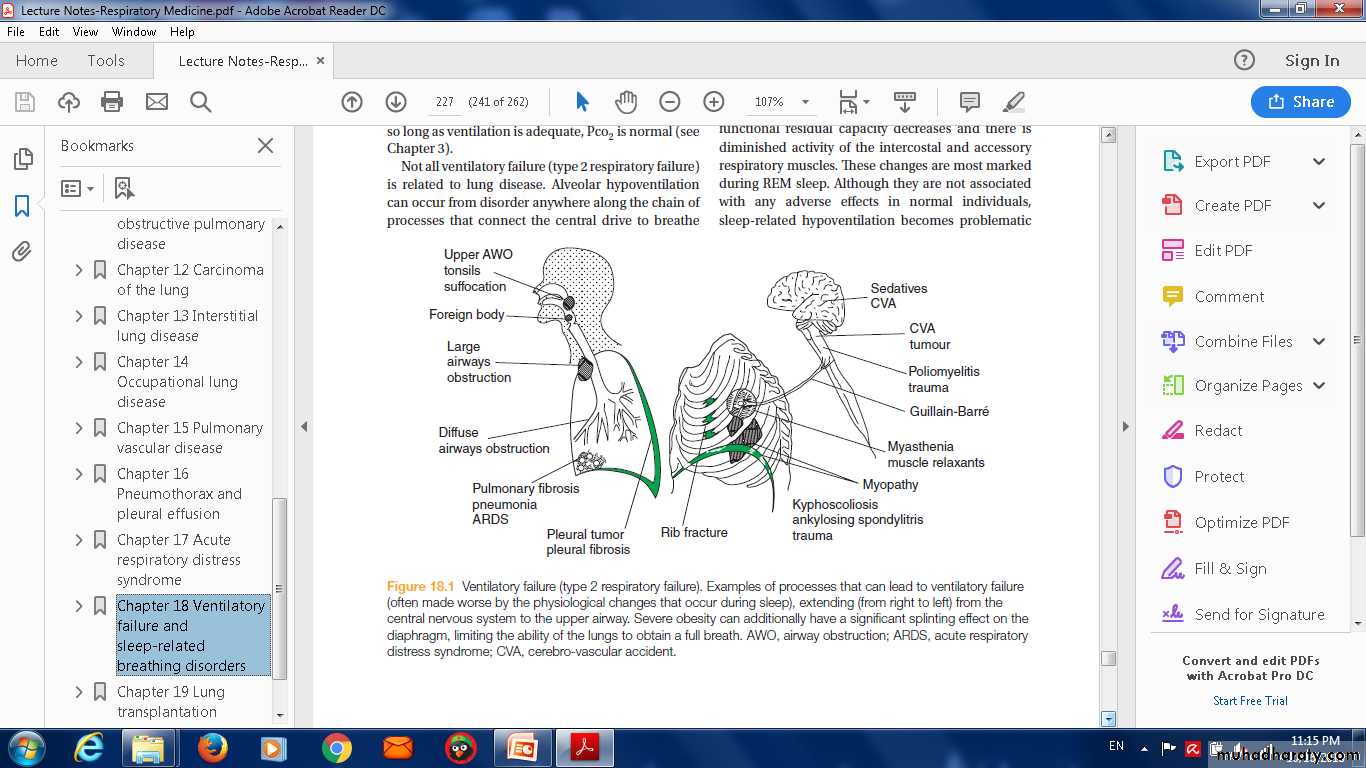
Ventilatory failure (type 2 respiratory failure).
Type II respiratoryfailure
Arterial hypoxia with hypercapnia.is seen in conditions that cause generalised,
severe ventilation–perfusion mismatch,
leaving insufficient normal lung to correct PaCO2, a disease that reduces total ventilation.
The latter includes not just diseases of the lung but also disorders affecting any part of the neuromuscular mechanism of ventilation
Pathophysiology
'type I respiratory failure' disease impairs ventilation of part of a lung (e.g. in asthma or pneumoniatype II respiratory failure Diseases causing this abnormality include any that impair ventilation locally, with sparing of other regions. Arterial hypoxia with hypercapnia .
The diagnosis of respiratory failure is not
clinical but based on arterial gas
assessment: it is defined by a PaO2
,60mmHg and/or PaCO2 .45 mmHg.
Features of Hypoxia ( CNS DYSFUCTION ,Cardiac)
Management of acute respiratory failure
Prompt diagnosis and management of the underlying causeIn type I respiratory failure,
high concentrations of oxygen (40-60% by mask).mechanical ventilation may be needed.
Patients who need high concentrations of oxygen for more than a few hours should receive humidified oxygen.
Acute type II respiratory failure
An emergency, requires immediate intervention.distinguish between patients with
1- high ventilatory drive (rapid respiratory rate and accessory muscle recruitment) .
2- Reduced or inadequate respiratory effort.
1- high ventilatory drive (rapid respiratory rate and accessory muscle recruitment)
A-Upper airway obstructioninspiratory stridor is present acute upper airway obstruction from
Causes
• foreign body inhalation ( treated by Heimlich maneuver )
• laryngeal obstruction (angioedema, carcinoma or vocal cord paralysis)
Rx immediate intubation or emergency tracheostomy may be life-saving.
B-lungs disease
Severe generalised bronchial obstruction from
COPD
Asthma
ARDS
Tension pneumothorax.
Rx In all such cases, high-concentration (e.g. 60%) oxygen should be administered
Non-invasive ventilation (NIV), which has been shown to reduce the need for intubation and shorten hospital stay.
Indications to supported ventilation
• Failure to respond to initial treatment,• declining conscious level .
• worsening respiratory acidosis .
Hypoxic drive
A small percentage of patients with severe chronic COPD and type II respiratory failure develop abnormal tolerance to raised PaCO2 and may become dependent on hypoxic drive to breathe.lower concentrations of oxygen (24-28% by Venturi mask).
In all cases, regular monitoring of arterial blood gases is important to assess progress.
2- Reduced or inadequate respiratory effort:
Reduced drive or conscious level may be suffering from• sedative poisoning.
• CO2 narcosis .
• a primary failure of neurological drive (e.g. following intracerebral haemorrhage or head injury).
Chronic and 'acute on chronic' type II respiratory failure
causes
• The most common cause is severe COPD.
• CO2 may be persistently raised.
• no persisting acidaemia.
Assessment and management of 'acute on chronic' type II respiratory failure
Initial assessment
Patient may not appear distressed despite being critically illConscious level (response to commands, ability to cough)
CO2 retention (warm periphery, bounding pulses, flapping tremor)
Airways obstruction (wheeze, prolonged expiration, hyperinflation, intercostal indrawing, pursed lips)
Cor pulmonale (peripheral oedema, raised JVP, hepatomegaly, ascites)
Background functional status and quality of life
Signs of precipitating cause .
Investigations
Pulse oximeter(O2 saturation)
Arterial blood gases (severity of hypoxaemia, hypercapnia, acidaemia, bicarbonate)
Chest X-ray
Treatment
Maintenance of airway
Treat specific precipitating cause
Frequent physiotherapy ± pharyngeal suction
Nebulised bronchodilators
Controlled oxygen therapy
Start with 24% Venturi mask
Aim for a normal PaO2
Antibiotics
Diuretics
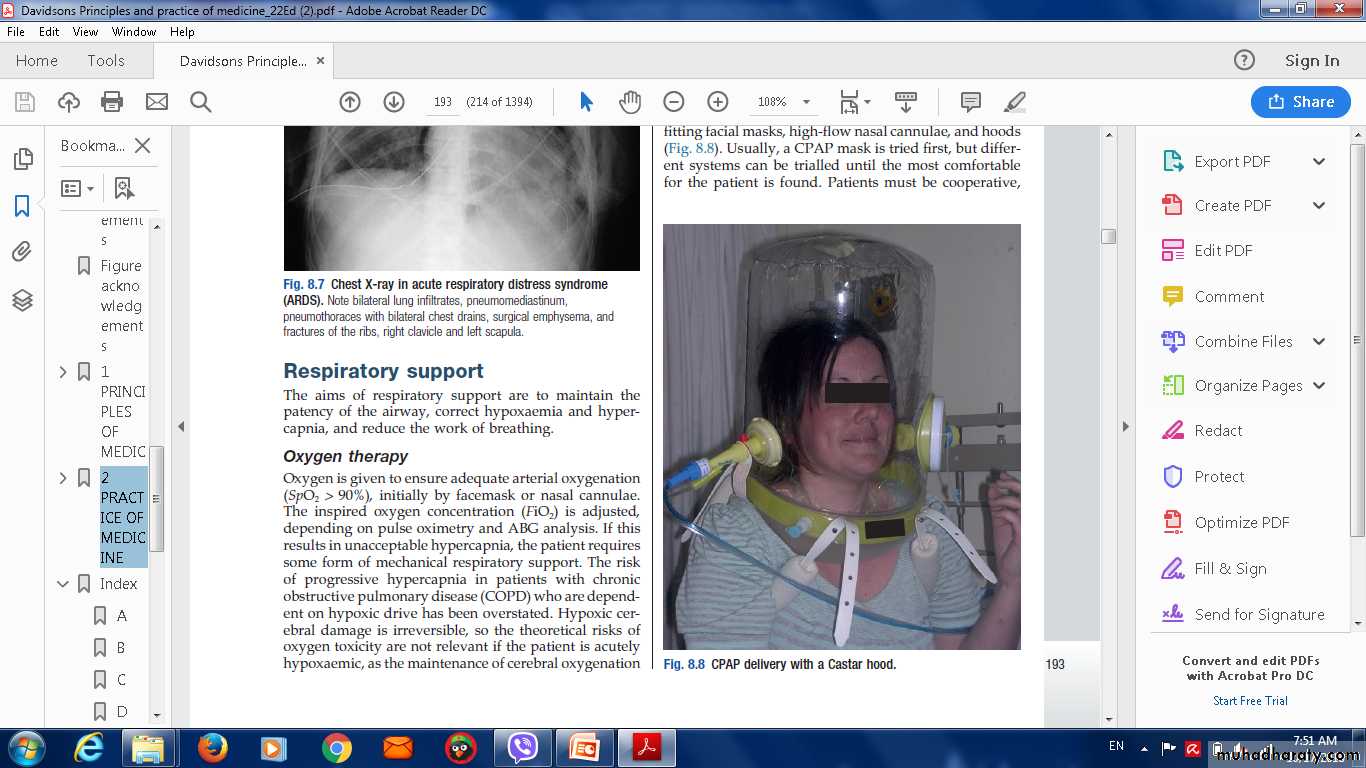
CPAP delivery with a Castar hood.
severe hypoxaemia
lead to potentially fatal arrhythmias or severe cerebral complications
Doxapramis a respiratory stimulant
Non-invasive respiratory supportNon-invasive respiratory support includes techniques that do not require sedation or an endotracheal or tracheostomy tube.
This helps preserve the patient’s respiratory muscle activity and reduces complications such as nosocomial infection.
Non-invasive respiratory Types of
Continuous positive airway pressure (CPAP) alone (non-invasive ventilation, or NIV).
BIPAP plus additional support, in the form of pressure applied to the breathing circuit during inspiration
Lung transplantation
Indications for lung transplantationParenchymal lung diseas
Cystic fibrosis
Emphysema
Pulmonary fibrosis.
Pulmonary vascular disease
Primary pulmonary hypertensionThromboembolic pulmonary hypertension
Types of transplants
Single-lung transplantationbilateral lung transplantation .
Combined heart-lung transplantation.
The prognosis
following lung transplantation is improving steadily with modern immunosuppressive drugsA 65-year-old man is found collapsed in the ward. On
examination there is no evidence of stridor, respiratory rateis 4 breaths/min and oxygen saturations are 82% on air.
His pulse is 120 beats/min and regular, blood pressure (BP)
90/60 mmHg, Glasgow Coma Scale is 3/15 and he has
bilateral pupillary constriction and no focal neurological
defi cit.
What is the most likely diagnosis?
a. Anaphylaxis
b. Myocardial infarction
c. Opiate toxicity
d. Pulmonary embolus
e. Raised intracranial pressure
A 57-year-old woman has just undergone fibreoptic
bronchoscopy. Monitoring shows her oxygen saturations
to have fallen to 86% on 2 L/min oxygen. On examination
her pulse is 88 beats/min, BP 146/84 mmHg, respiratory
rate 5 breaths/min. Chest examination reveals trachea –
midline, expansion right = left, percussion right = left,
breath sounds vesicular, nil added.
Which of the following is the most likely complication
that has occurred following bronchoscopy?
a. Bleeding
b. Bronchospasm
c. Infection
d. Oversedation
e. Pneumothorax
Thank you
QQUIZE