ال تقل أن الدنيا تعطيني ظهرها فربما أنت م
ن
تجلس بالعكس
.

-
تدريسي في كلية الطب
\
جامعة ذي
قار
2
-
طبيب
أختصاص
االمراض الباطنية في دائرة صحة ذي قار
3
-
دكتوراه اختصاص في وظيفة الكليتين
(
الفسلجه
الطبيه
)
\
جامعة الكوفة
4
-
ماجستير اختصاص في وظيفة الكليتين
(
الفسلجه
الطبيه
)
\
\
جامعة الكوفة
5
-
الدبلوم العالي في االمراض
الباطنيه
وامراض الكليتين
.
\
الجامعة المستنصرية
6
-
بكالوريوس في الطب
والجراحه
العامه
\
جامعة البصرة
.
7
-
عضو
الجمعيه
االوربيه
المراض
وزرع الكلى
\
ايطاليا
8
-
بكالوريوس في القانون وماجستير مهني في العالقات الدبلوماسية
(
اختصاص دقيق في اتكيت ر
ئيس الدولة
ووزير الخارجية
.
9
-
مستشار في حل المنازعات والتحكيم الدولي
\
جمهورية مصر
العربيه
وعضو االتحاد
االفرواسيوي
ل
لقانون
الدولي وتسوية المنازعات
.
رقم العضوية
572
10
-
مدرب معتمد في البورد األمريكي
_
الكندي والبورد االلماني وخبير معتمد
للتنميةالبشرية
ID762AII
و
CT5547
11
-
ميسر معتمد في أدب الحوار من قبل وزارة الصحة العراقية رقم الكتاب
279
في
27
\
12
\
2018
12
-
محاضر حول التخطيط
األستراتيجي
واألداره
العامه
.
13
-
مدير مستشفى الحبوبي التعليمي في ذي قار عام
2005
14
مدير قسم الكلية الصناعية في مستشفى الحسين التعليمي في ذي قار
2006
-
2009
15
نقيب اطباء محافظة ذي قار
.
16
–
نائب رئيس جمعية اطباء محافظة ذي قار وهي جمعية مسجلة في وزارة التعليم العالي
17
-
رئيس جمعية نقابة االطباء المجانية لمعا لجة المرضى المتعففين
18
-
كاتب قصصي للقصص القصيرة ذات المعرفة الطبية ومن مؤلفاتي مجموعة قصصية بعنوان طرا
ئف العيادة
19
-
عدد من المحاضرات في الصحة االلكترونية واهميتها في تحسين صحة المجتمع

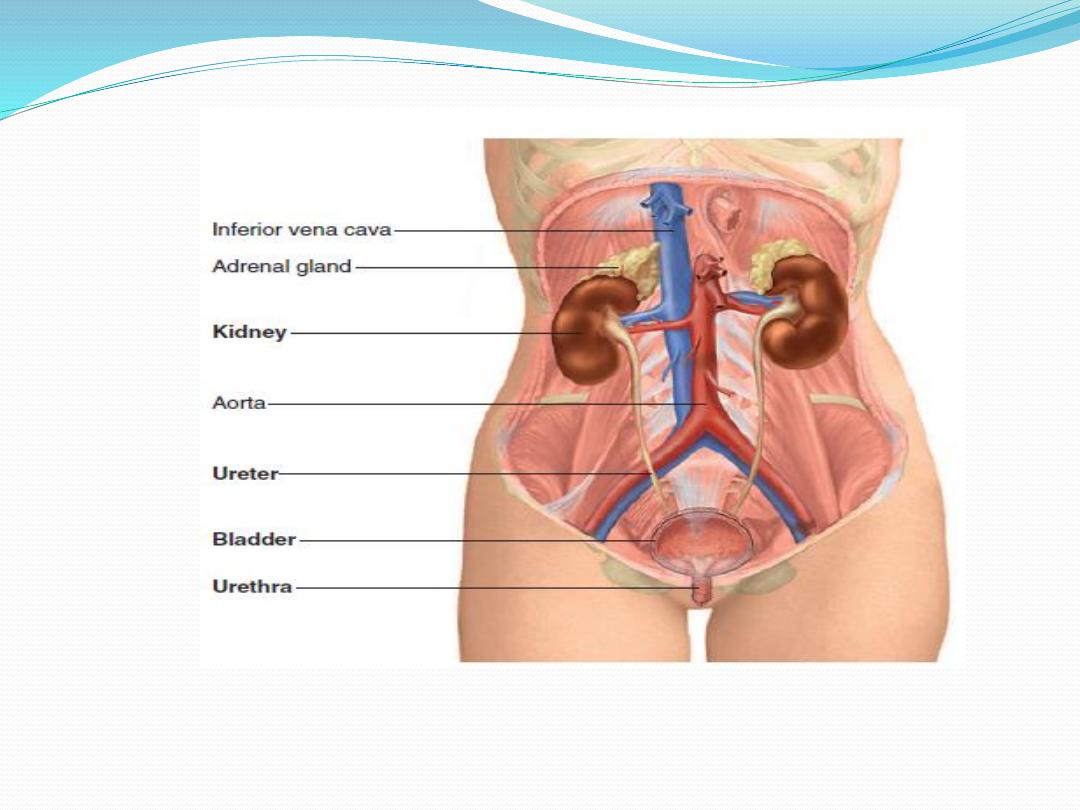
Physiological anatomy of urinary system
*The urinary system consists of two kidneys, two ureters, the bladder
and a single urethra. The paired kidneys are bean-shaped retroperitoneal
organs, each about 12-cm long and located on the posterior abdominal
wall. Each kidney of the adult human weighs about 150 grams and is
about the size of a clenched fist.
*The medial side of each kidney contains an indented region called
the hilum through which pass the renal artery and vein, lymphatics,
nerve supply, and ureter. Each kidney is surrounded by a tough,
fibrous capsule that protects its delicate inner structures. The
kidneys extending approximately from the last thoracic vertebrae (T
12
) to third lumbar vertebrae (L
3
) , receiving some protection from the
lower part of the rib cage. The right kidneys is slightly lower than the
left one.

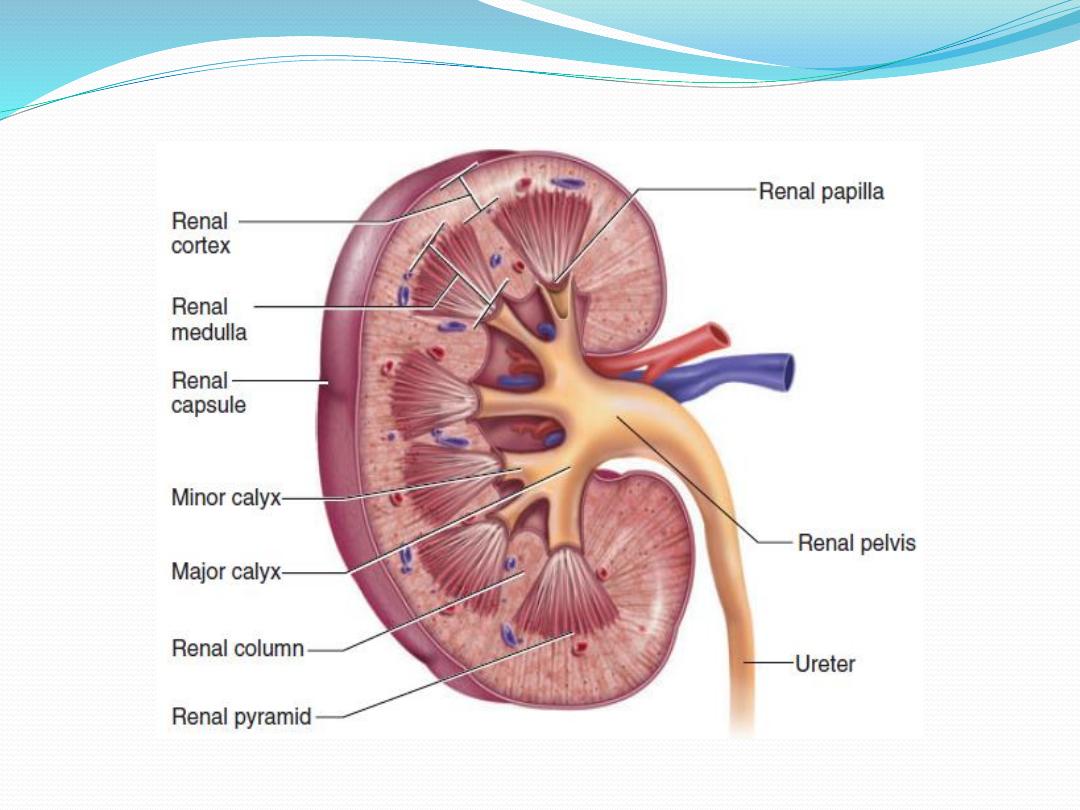
Structure of the Kidneys
*In cross section the kidney had an outer area called the cortex and
the inner region the medulla. The medulla is divided into multiple
cone-shaped masses of tissue called renal pyramids. The base of
pyramid directed to ward the cortex and the tip of pyramid( papilla)
projects into the funnel-shaped minor calyces of renal pelvis,.
*The minor calyces combine to form major calyces, which in turn
combine with each other to form the renal pelvis which represent
the upper dilated end of the ureter. The walls of the calyces, pelvis,
and ureter contain contractile elements that propel the urine toward
the bladder.

Functions of the Kidneys
1. They eliminate the waste products of metabolism, including urea
(the main nitrogen-containing end-product of protein
metabolism in humans), uric acid (an end-product of purine
metabolism), and creatinine (an end-product of muscle
metabolism) bilirubin, toxins and other foreign substances.
2. Regulation of water and electrolyte balances.
3. Regulation of arterial pressure; the kidneys play a dominant role
in long-term regulation of arterial pressure by excreting variable
amounts of sodium and water. The kidneys also contribute to short-
term arterial pressure regulation by
secreting vasoactive factors or substances, such as renin, that lead to
the formation of vasoactive products (e.g., angiotensin II).

4. Regulation of acid-base balance. The kidneys contribute to acid-base
regulation, along with the lungs and body fluid buffers, by excreting acids and
by regulating the body fluid buffer stores.
5. Regulation of Erythrocyte Production.
6. Regulation of 1,25-Dihydroxyvitamin D
3
Production.
7. Gluconeogenesis
8. They degrade several polypeptide hormones, including insulin, glucagon, and
parathyroid hormone.
ENDOCRINE FUNCTIONS OF THE KIDNEY
The kidney is a target organ for several hormones, including
antidiuretic hormone (ADH), angiotensin II, aldosterone, atrial
natriuretic peptide (ANP), and parathyroid hormone (PTH). The
kidney is also an endocrine organ that secretes renin,
erythropoietin (EPO), and the active form of vitamin D3, 1,25-
dihydroxycholecalciferol (1,25-(OH)2 vitamin D):
1.RENIN SECRETION
Renin is an enzyme released by the juxtaglomerular apparatus of
the kidney in response to a decrease in effective circulating blood
volume. Renin is released from the juxtaglomerular cells lining
the afferent arterioles, which respond to reduced renal perfusion,
and initiates a cascade of events that result in the production of
the hormones angiotensin II and aldosterone. The renin-
angiotensin-aldosterone system is the most important endocrine
axis in control of the extracellular fluid volume.

2. Erythropoietin (EPO) secretion.
EPO is a glycoprotein hormone produced by fibroblasts in the renal interstitium.
EPO is released in response to low renal interstitial PO2. It stimulates red blood
cell formation in the bone marrow to restore the O2- carrying capacity of blood.
About 80% of plasma EPO is produced in the kidney and the remainder is secreted
by the liver. The mechanism coupling low PO2 to EPO secretion involves increased
local production of prostaglandins. Patients with renal failure do not secrete
sufficient amounts of EPO and, therefore, they usually develop anemia. Clinically,
the main uses of EPO are related to treating anemia associated chronic renal
failure or to cancer
Chemotherapy
*However, EPO has also gained notoriety in the lay press as a “blood-doping”
agent that is used illegally by endurance athletes. In healthy individuals, injection
of EPO will lead to supraphysiologic levels of red blood cells (increased
hematocrit) and consequently an increase in O2-carrying capacity, a result that
boosts aerobic output in athletes during competition
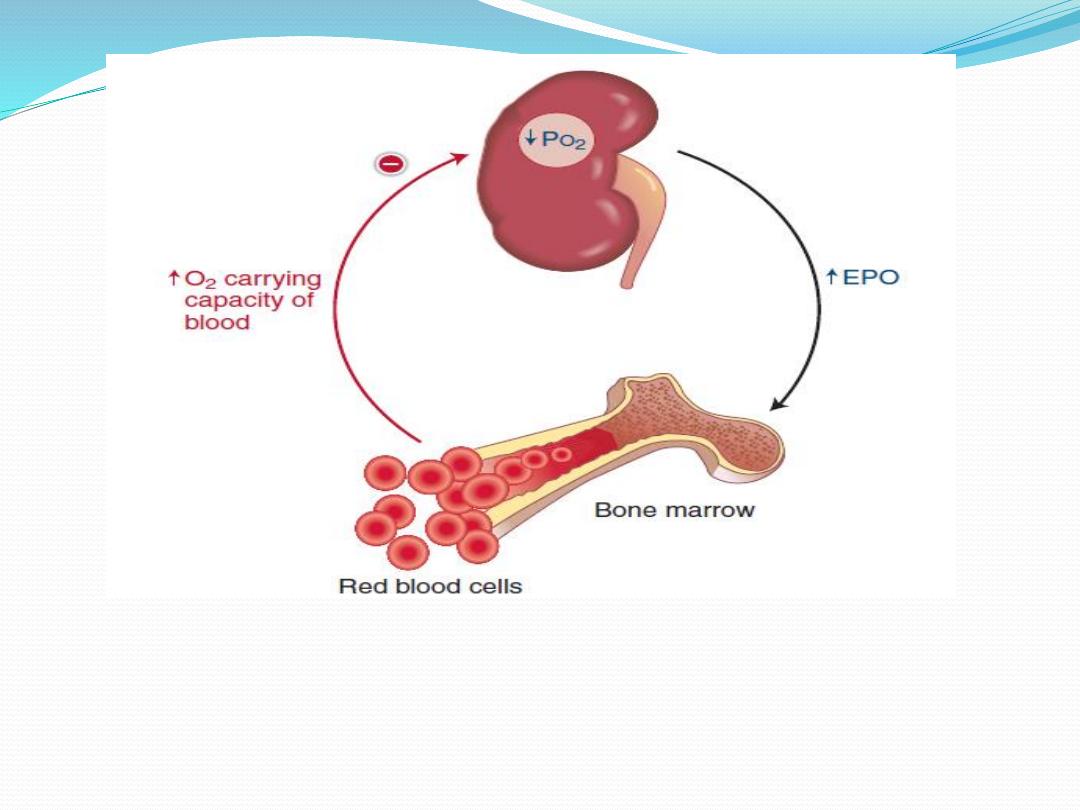
Figure 4: Negative feedback regulation of blood-O2 content via
erythropoietin (EPO) secretion

3.ACTIVATION OF VITAMIN D
Vitamin D is a steroid derived from precursors that are either ingested or
produced by the action of ultraviolet light on the skin. The active form of
vitamin D is 1,25-dihydroxycholecalciferol (1,25-(OH)2 vitamin D). The
liver produces 25-hydroxycholecalciferol (25-OH vitamin D), which is
converted to 1,25-(OH)2 vitamin D in the kidney under the control of
parathyroid hormone. Vitamin D3 promotes Ca2+ conservation in the
body by increasing intestinal Ca2+ absorption and also by reducing
urinary Ca2+ loss.
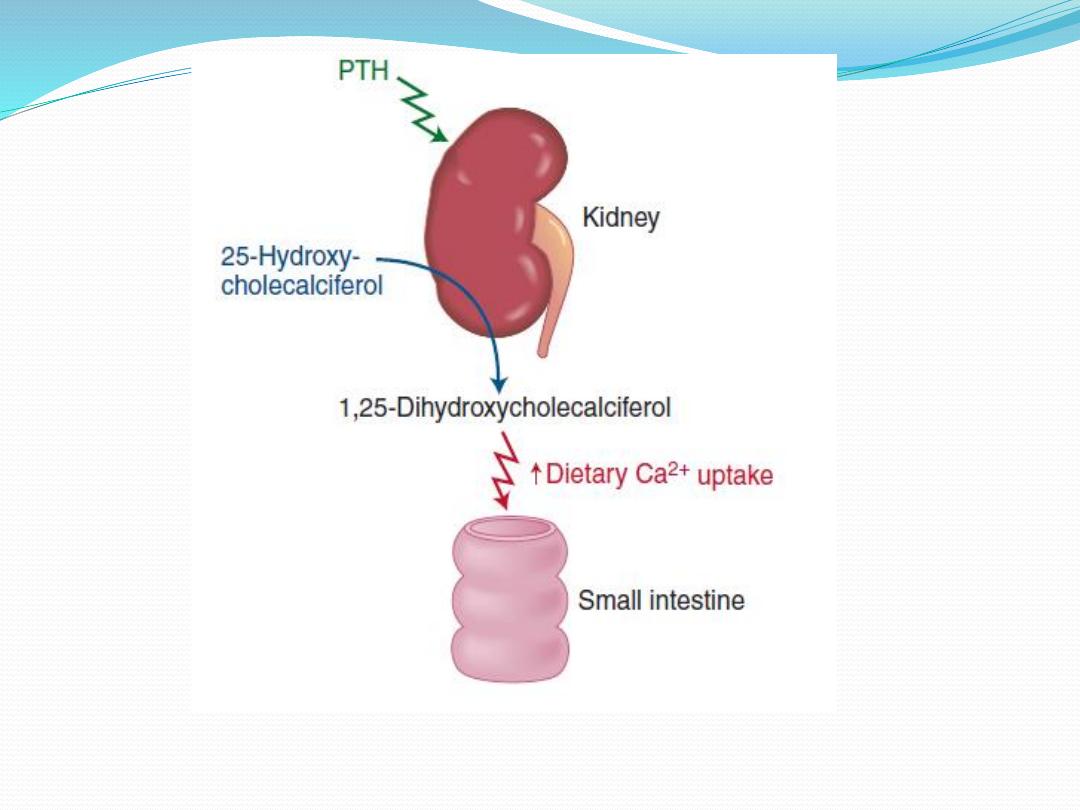
Figure 5: Renal activation of vitamin D.
Manifestations of chronic renal failure plague many of the body’s systems,
including bone. Osteitis fibrosa cystica (renal osteodystrophy) is the classic
bone disease related to chronic renal failure. The pathophysiologic cascade
begins in the kidneys and ends in the bones:
1. As the kidneys fail, so does the function of 1α-hydroxylase, the enzyme
that converts inactive 25-OH vitamin D to active 1,25-OH vitamin D,
resulting in vitamin D deficiency.
2. Vitamin D deficiency results in low serum Ca2+ due to impaired dietary
absorption.
3. Low serum Ca2+ stimulates the parathyroid glands to
increase PTH production (secondary hyperparathyroidism) .
4. PTH acts on bone to cause a high rate of bone turnover,
which releases Ca2+ back into the serum. The end result of this
cascade is that near normal plasma Ca2+ concentration is
maintained at the expense of chronic bone resorption resulting
from hyperparathyroidism.
* Osteitis fibrosa cystica is a condition characterized by fibrous
replacement of the marrow and cystic trabecular bone, which
renders the bones fragile and, therefore, increases the risk of
fracture.

The Nephron
The functional units of the kidney are nephrons. Each kidney contains
approximately 1 million nephrons. Each nephron consists of:
I. The renal corpuscle
consists of a compact tuft of interconnected
capillary loops, the glomerulus or glomerular capillaries, surrounded by
a balloon-like hollow capsule( Bowman's capsule). Blood is ultrafiltered
across the glomerular capillaries into Bowman's space, which is the first
step in urine formation.
II. Renal tubule
; a long tubule in which the filtered fluid is converted
into urine on its way to the pelvis of the kidney , the renal tubule
consist of:
1. the proximal tubule which lies in renal cortex. It drains Bowman's
capsule, and consists of a coiled segment—the proximal convoluted
tubule—followed by a straight segment—the proximal straight tubule—
which descends toward the medulla.
2.the loop of Henle,
it start at the end of proximal tubule and dips into the
renal medulla to varying depths. Each loop consists of a descending and an
ascending limb. The walls of the descending limb and the lower end of the
ascending limb are very thin and therefore are called the thin segment of the
loop of Henle. After the ascending limb of the loop has returned partway
back to the cortex, its wall becomes much thicker, forming the thick segment
of the ascending limb.
3. the distal convoluted tubule
, the thick ascending limb rises back into the
cortex to form the distal tubule that passes directly between the afferent and
efferent arterioles, as they enter and exit that renal corpuscle at its vascular
pole. There are special type of cells at the junction of the thick ascending
limb and the distal tubule known as the macula densa.

4.the cortical collecting tubule,
which lead to the cortical collecting duct.
Several nephrons drain into a cortical collecting duct.The cortical collecting
ducts join to form a single larger collecting duct that runs downward into the
medulla and becomes the medullary collecting duct.
5.The medullary collecting duct;
the medullary collecting duct passes
through outer medulla then through the inner medulla. In the inner medulla,
the inner medullary collecting ducts unite to form large papillary ducts, that
eventually empty into the renal pelvis through the tips of the renal papillae. In
each kidney, there are about 250 of the very large collecting ducts
(Bellini
duct),
each of which collects urine from about 4000 nephrons.
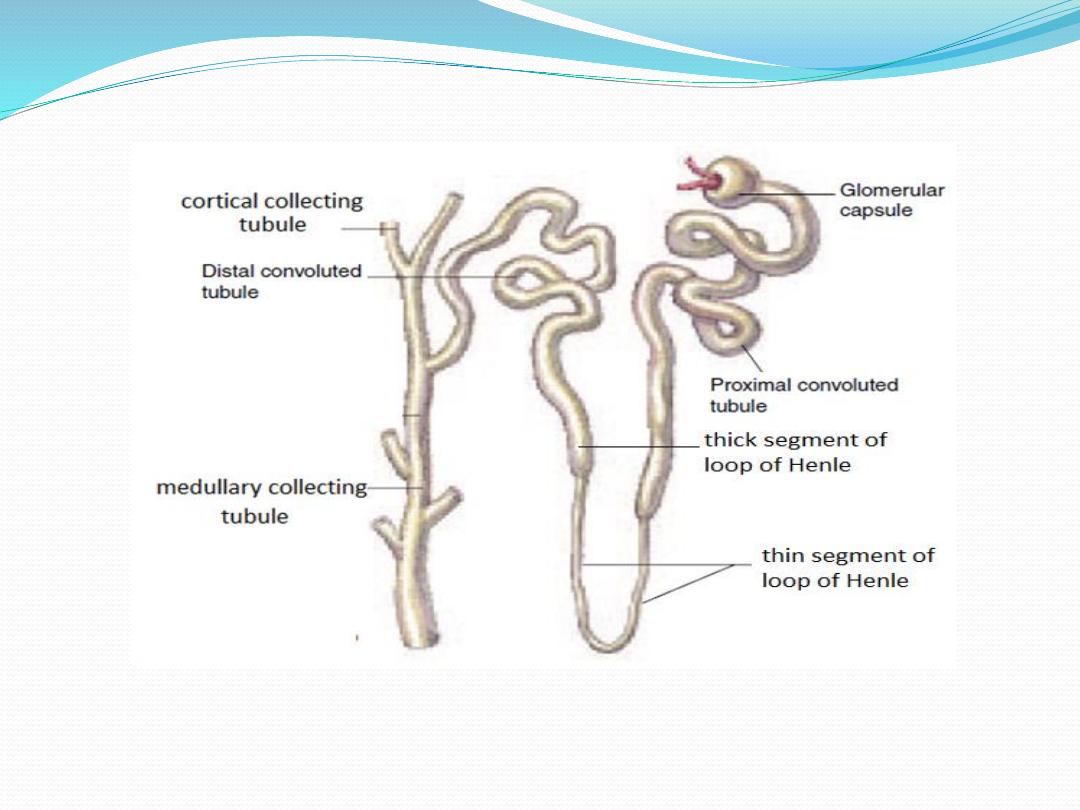
Figure 6:The nephron
.

Cortical and juxtamedullary nephrons
Two groups of nephrons are distinguished, based on the
location of their glomeruli in the cortex: cortical, and
juxtamedullary nephrons. The superficial cortical
nephrons have their glomeruli in the outer
cortex Cortical nephrons represent 85% of the nephrons
in the kidneys. These nephrons have relatively short loops
of Henle, which descend only into the outer medulla. The
juxtamedullary nephrons have their glomeruli near the
corticomedullary border. The glomeruli of the
juxtamedullary nephrons are larger than those of the
superficial cortical nephrons and, accordingly, have
higher glomerular filtration rates
.

The juxtamedullary nephrons are characterized by
long loops of Henle that descend deep into the
inner medulla and papilla and are essential for the
concentration of urine. The peritubular capillary of
the juxtamedullary nephrons called vasa recta.
The juxtaglomerular apparatus (JGA),
located at the junction of thick ascending limb of the loop of Henle and distal
tubule,where they touches the vascular pole of the glomerulus ( against the
afferent arteriole and the efferent arteriole). The juxtaglomerular apparatus
(JGA) comprised of
The macula densa (dense spot) consists of densely crowded tubular epithelial
cells on the side of the thick ascending limb that faces the glomerular tuft;
these cells monitor the composition of the fluid in the tubule lumen at this
point.
The extraglomerular mesangial cells are continuous with mesangial cells of the
glomerulus; they may transmit information from macula densa cells to the
granular cells.
The granular cells are modified vascular smooth muscle cells with an
epithelioid appearance, located mainly in the afferent arterioles close to the
These cells synthesize and release renin, a proteolytic enzyme that results in
angiotensin glomerulus.
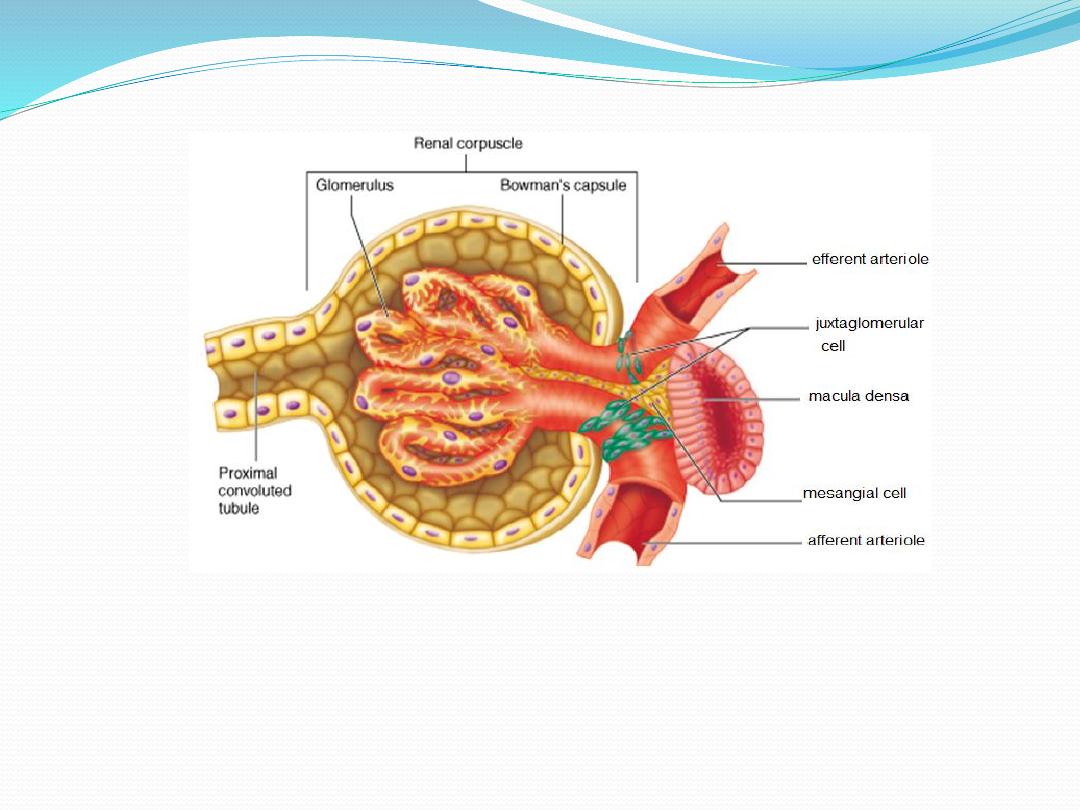
juxtaglomerular apparatus

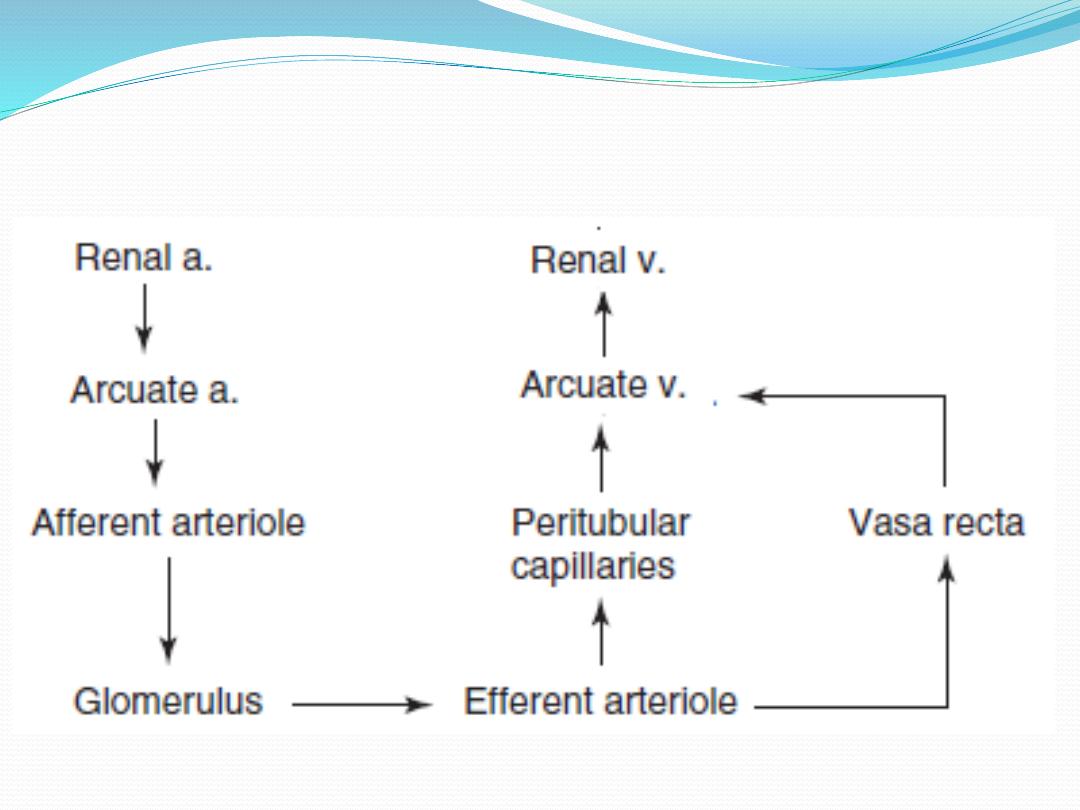
Renal Blood Supply
Blood flow to the two kidneys is normally about 22 % of the cardiac output, or
1100 ml/min. The renal arteries issue at right angles from the abdominal aorta;
because the aorta lies to the left of the midline, the right renal artery is longer
than the left. As it approaches a kidney, each renal artery divides into five
segmental arteries. Within the renal sinus, each segmental artery branches
further to form several interlobar arteries. At the medulla-cortex junction, the
interlobar arteries branch into the arcuate arteries that arch over the bases of
the medullary pyramids, arcuate arteries. Small interlobular arteries(also called
radial arteries) radiate from the arcuate arteries and project into the renal
cortex. Microscopic afferent glomerular arterioles arise from branches of the
interlobular arteries which lead to the glomerular capillaries. The distal ends
of the capillaries of each glomerulus coalesce to form the efferent arteriole,
which leads to a second capillary network, the peritubular capillaries, that
surrounds the renal tubules.

The renal circulation has two capillary beds, the glomerular and
peritubular capillaries, the hydrostatic pressure in the glomerular
capillaries is high (about 60 mm Hg) to enhance fluid filtration, on
the other hand the hydrostatic pressure in the peritubular capillaries
is low (about 13 mm Hg) to permits rapid fluid reabsorption. The
peritubular capillaries empty into the vessels of the venous
system, which run parallel to the arteriolar vessels and
progressively form the interlobular vein, arcuate vein, interlobar
vein, and renal vein, which leaves the kidney beside the renal
artery and ureter. The renal cortex, receives more than 95% of the
kidney's blood flow. Blood flow in the renal medulla accounts for
less than 5% of the total renal blood flow. The high blood flow to
the kidneys is necessary for a high GFR and is not due to
excessive metabolic demands.

Blood flows from high pressure to low pressure ,two
factors determine blood flow, pressure gradient and
resistance:
Flow (Q) = pressure gradient / resistance (R)
Accordingly two factors can decrease blood flow
Decreasing the pressure gradient .
Increasing resistance .

When an arteriole vasoconstricts (resistance increases), 2
changes to consider:
• Flow across the entire circuit decreases
• Pressure increases before the point of
resistance(upstream) and pressure decreases after the
point of resistance(downstream).
When an arteriole vasodilate (resistance decreases), 2
changes to consider:
• Flow across the entire circuit increases
• Pressure decreases before the point of
dilation(upstream) and pressure increases after the point
of dilation (downstream
).
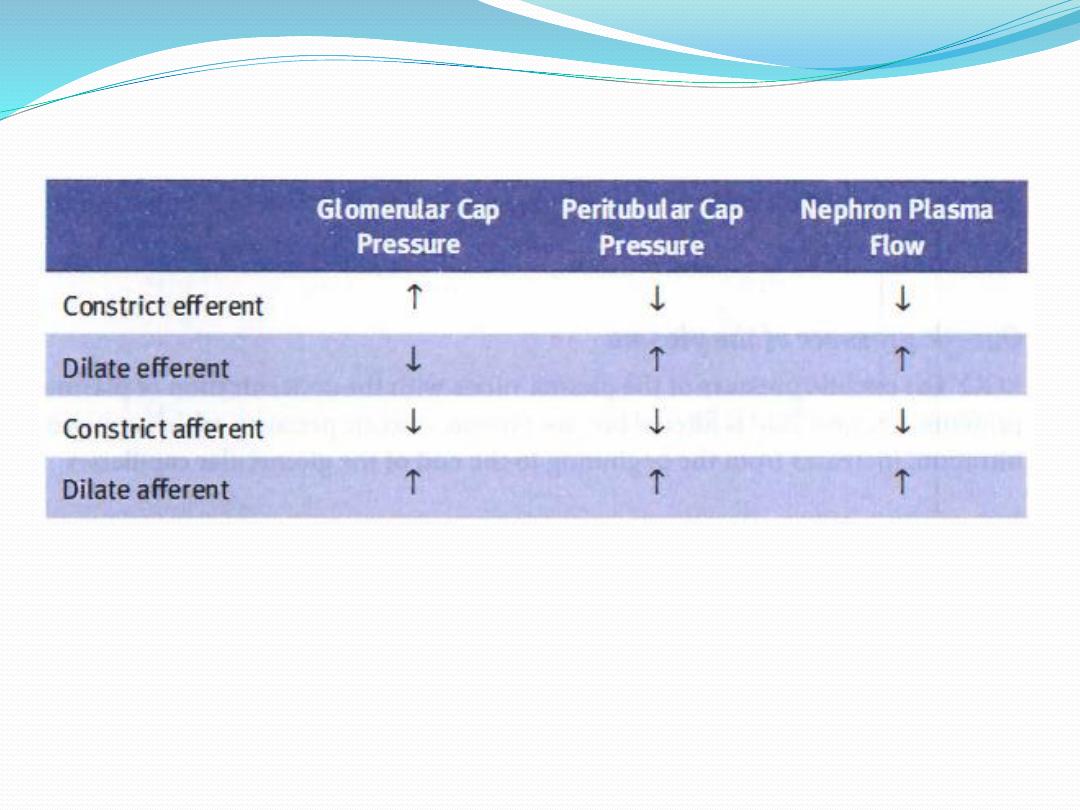
Table -1. Consequences of constrictions or dilations of the afferent and efferent
arterioles


Glomerular Filtration
Urine formation begins with glomerular filtration, the bulk flow of
fluid from the glomerular capillaries into Bowman's capsule. The
glomerular filtrate (ie, the fluid within Bowman's capsule) is very
much like blood plasma. However, plasma proteins, blood cells and
protein binding substance like fatty acid are virtually excluded from
moving through the filtration barrier. The filtrate contains most
inorganic ions and low-molecular-weight organic solutes in virtually
the same concentrations as in the plasma. Substances that are
present in the filtrate at the same concentration as found in the
plasma are said to be freely filtered.

As glomeular filtrate leaves Bowman's capsule and passes
through the renal tubules, its composition is modified by
reabsorption of water and specific solutes back into the
blood or by secretion of other substances from the
peritubular capillaries into the tubules. The volume of filtrate
formed per unit time is known as the glomerular filtration
rate (GFR). In a normal young adult male, the GFR is an
incredible 180 L/day (125 mL/min). When we recall that the
average total volume of plasma in humans is approximately 3
L, it follows that the entire plasma volume is filtered by the
kidneys some 60 times a day. The opportunity to filter such
huge volumes of plasma enables the kidneys to excrete large
quantities of waste products and to regulate the constituents
of the internal environment very precisely.

Glomerular Capillary Membrane
The filtered substances must pass from blood into bowman capsule through
glomerular membrane. The total area of glomerular capillary endothelium
across which filtration occurs in humans is about 0.8 m
2
. The glomerular
capillary membrane has had three major layers:
1.The endothelial cells of the capillaries, is perforated by many large
fenestrae ("windows"), like a slice of Swiss cheese. and rich with fixed
negative charges .
2.The basement membrane: The thickness of the basement membrane
about 50 nm, it consist of glycoproteins and proteoglycans. The
proteoglycans have a net negative charge. In minimal change nephropathy
the negative charges on the basement membrane are lost , as a result
proteins, especially albumin, are filtered and appear in the urine, a condition
known as proteinuria or albuminuria.
3.The epithelial cells ( podocytes); the podocytes have an unusual
octopus-like structure called pedicels (or foot processes), extend from
each arm of the podocyte and are embedded in the basement
membrane. Pedicels from adjacent podocytes interdigitate forming
slits through which the filtrate enter Bowman's space. Podocyte
membranes also have a high density of negative charge .
The glomerulus also contain mesangial cells which are interstitial cells
,they act as phagocytes and remove trapped material from the
basement membrane. They also contain myofilaments and can
contract .Contraction of the mesangial cells could augment the
resistance of the arterioles and possibly change the number of open
capillary loops in the glomerular tuft.
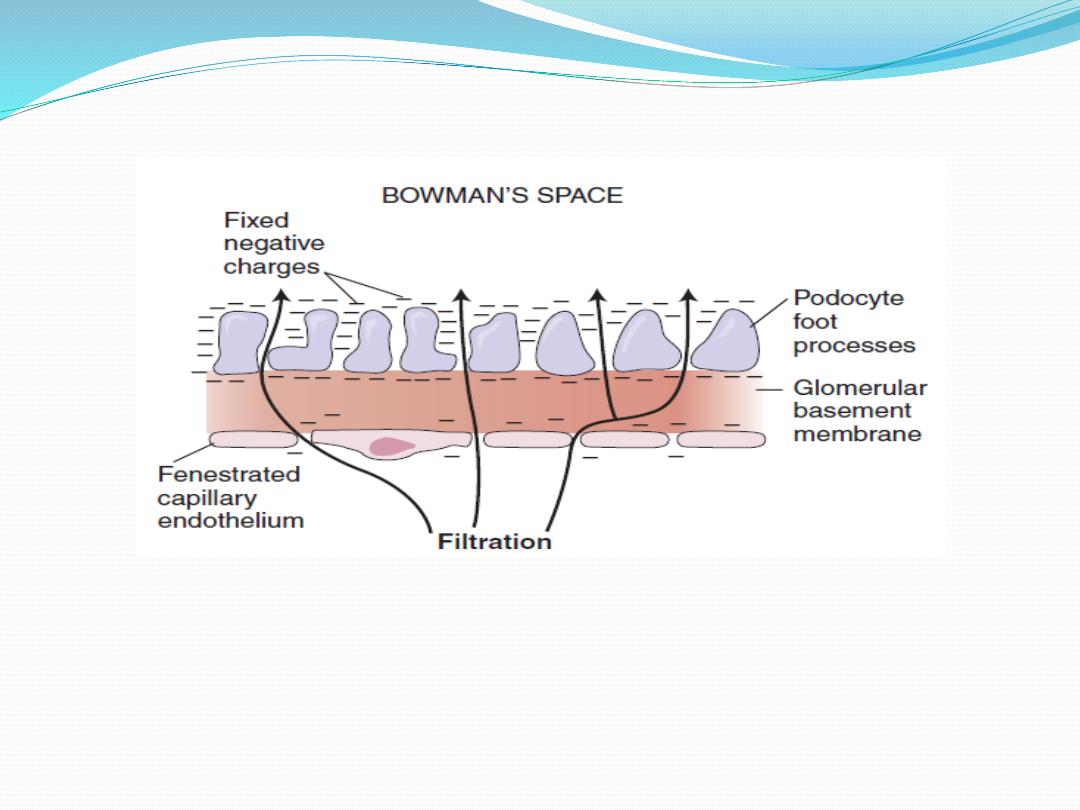
The glomerular membrane.

.Size, shape, and electrical charge affect the filterability of
molecules
The glomerular capillary membrane is thicker than most other
capillaries, but it is also much more porous and therefore filters fluid at
a high rate. The filtration rate, of any substance depend on:
1.Molecular size; Functionally, the glomerular membrane permits the
free passage of neutral substances up to 4 nm in diameter and almost
totally excludes those with diameters greater than 8 nm. Most plasma
proteins are large molecules, so they are not appreciably filtered.
2.Electrical charge, glomerular endothelial cells, podocytes, and the
basement membrane all have a negatively charge. They impede the
passage of negatively charged molecules by electrostatic repulsion and
favor the passage of positively charged molecules by electrostatic
attraction.
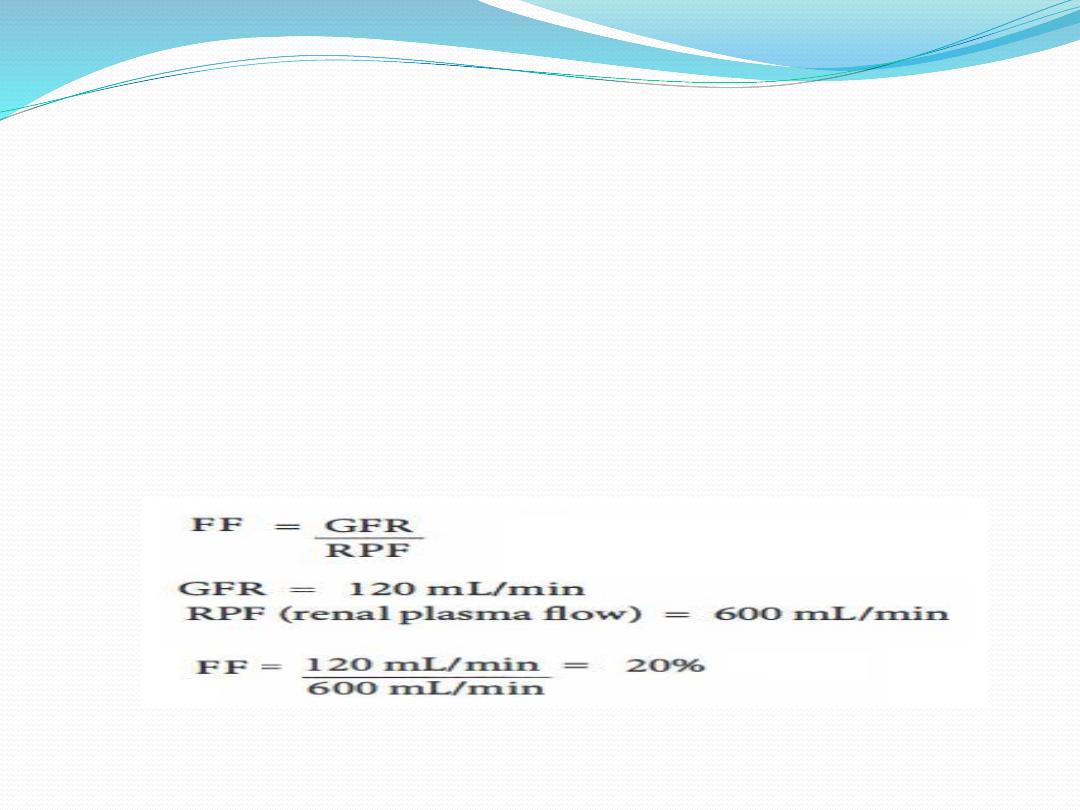
Filtration fraction(FF)
The fraction of the renal plasma flow that is filtered (the
filtration fraction) averages about 0.2; this means that about
20 per cent of the plasma flowing through the kidney is filtered
through the glomerular capillaries. The filtration fraction is
calculated as follows:

Determinants of the GFR
The pressures that drive fluid movement across the glomerular
capillary wall are the Starling forces(pressures). There are four
Starling pressures: two hydrostatic pressures (one in glomerular
capillary and called Glomerular hydrostatic pressure PG and one
in Bowman’s capsul called th Bowman’s capsule hydrostatic
pressure PB) and two colloid osmotic pressures (one in
glomerular capillary and called Glomerular capillary colloid
osmotic pressure πG and one in Bowman's space and called
Bowman’s capsule colloid osmotic pressure πB). According to the
Starling equation the GFR is the product of Filtration coefficient
(K
f
) and the net ultrafiltration pressure. The net filtration
pressure, is the algebraic sum of the four Starling pressures as in
the following equation:

The net filtration = Forces Favoring Filtration - Forces Opposing
Filtration
Forces Favoring Filtration (mm Hg)
Glomerular hydrostatic pressure 60
Bowman’s capsule colloid osmotic pressure 0
Forces Opposing Filtration (mm Hg)
Bowman’s capsule hydrostatic pressure 18
Glomerular capillary colloid osmotic pressure 32
Thus the net filtration = [(60 + 0-(18+32)] = 10 mmHg.
According to the Starling equation
GFR =Kf x 10
where GFR is the Glomerular filtration rate (mL/min), K
f
is Filtration
coefficient (mL/min . mm Hg) , P
G
is Hydrostatic pressure in glomerular
capillary (mm Hg) , P
B
is Hydrostatic pressure in Bowman's space (mm
Hg), π
G
is colloid osmotic pressure in glomerular capillary (mm Hg)
and π
B
is colloid osmotic pressure in Bowman's space.
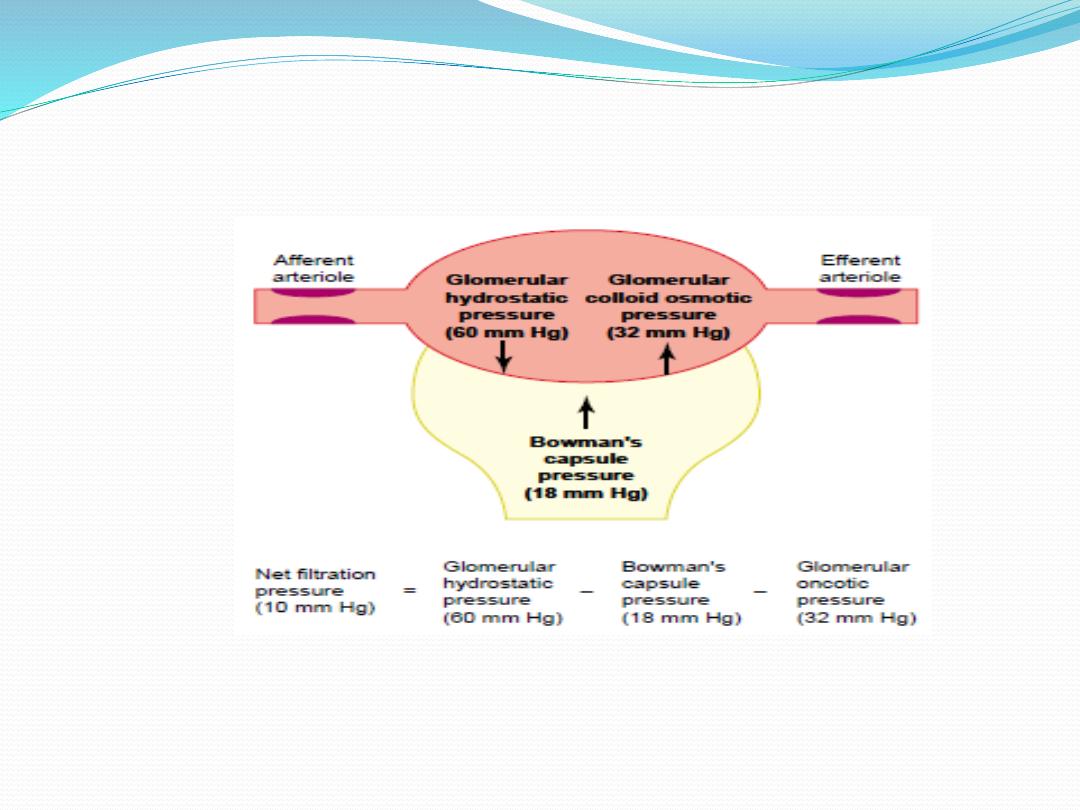
The forces causing filtration by the glomerular capillaries.

For glomerular capillaries, the net ultrafiltration pressure is 10
mmHg in favors of filtration, so that the direction of fluid
movement is always out of the capillaries. The greater the net
pressure, the higher the rate of glomerular filtration.
Filtration coefficient(K
f
)
The K
f
is the water permeability or hydraulic conductance of the
glomerular capillary wall. The two factors that contribute to K
f
are the
water permeability of glomerular capillary per unit of surface area time
the total surface area of the glomerular capillary. K
f
is calculated from
GFR and the net filtration pressure , normally the GFR is about 125
ml/min and the net filtration pressure is 10 mm Hg,
K
f
= GFR/ net filtration pressure
Kf = 125/10 =12.5 ml/min/mm Hg

The normal K
f
is calculated to be about 12.5
ml/min/mm Hg of filtration pressure for both kidneys.
When K
f
is expressed per 100 grams of kidney weight,
it averages about 4.2 ml/min/mm Hg. The of Kf of
renal capillary glomeruli is about 400 times as high as
the K
f
of most other capillary systems of the body; the
average K
f
of many other tissues in the body is only
about 0.01 ml/min/mm Hg per 100 grams. This high K
f
for
the
glomerular
capillaries
contributes
tremendously to their rapid rate of fluid filtration.

Factors that decrease GFR
1.decreased K
f
lead to decrease GFR, as in uncontrolled
hypertension and diabetes mellitus which results in increasing
the thickness of the glomerular capillary basement membrane
and, eventually, by damaging the capillaries
2. Increased bowman's capsule hydrostatic pressure decreases
GFR. This can be produced by obstructing urine flow (e.g.,
ureteral stone )
3. Increased glomerular capillary colloid osmotic pressure
decreases GFR.
4. constriction of the afferent arteriole, in which afferent
arteriolar resistance increases. This will lead to decreases
glomerular Hydrostatic Pressure and also decreases GFR
.
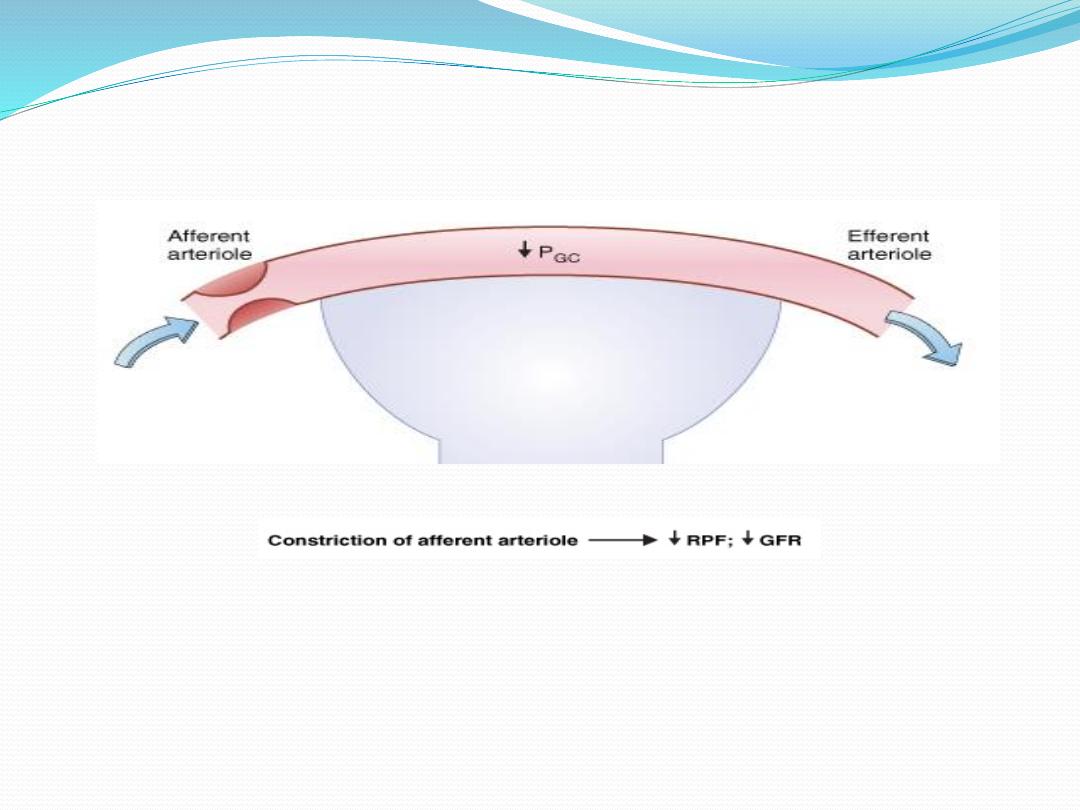
decrease GFR due to constriction of the afferent arteriole

Factors that increase GFR
The main factors that can increase GFR are
1. Increased glomerular capillary hydrostatic pressure
increases GFR
as in case of increase arterial pressure, or increase efferent
arteriolar resistance.
2. decreases in plasma protein concentration (e.g.,
nephrotic syndrome, in which large amounts of protein are
lost in urine) produce decreases in glomerular capillary
colloid osmotic pressure (π
GC
), which increase both net
ultrafiltration pressure and GFR.
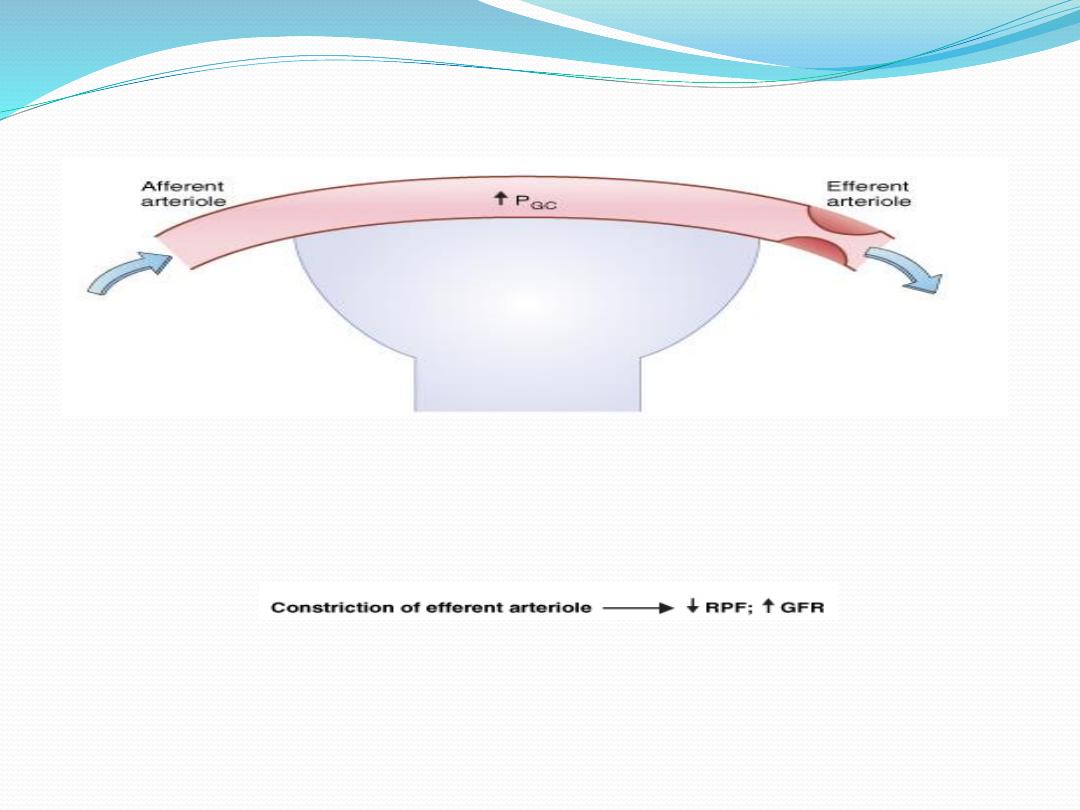
increase GFR due to constriction of the efferent arteriole
