1
Fifth stage
Psychiatry
Lec-1
الهام الجماس
4/10/2015
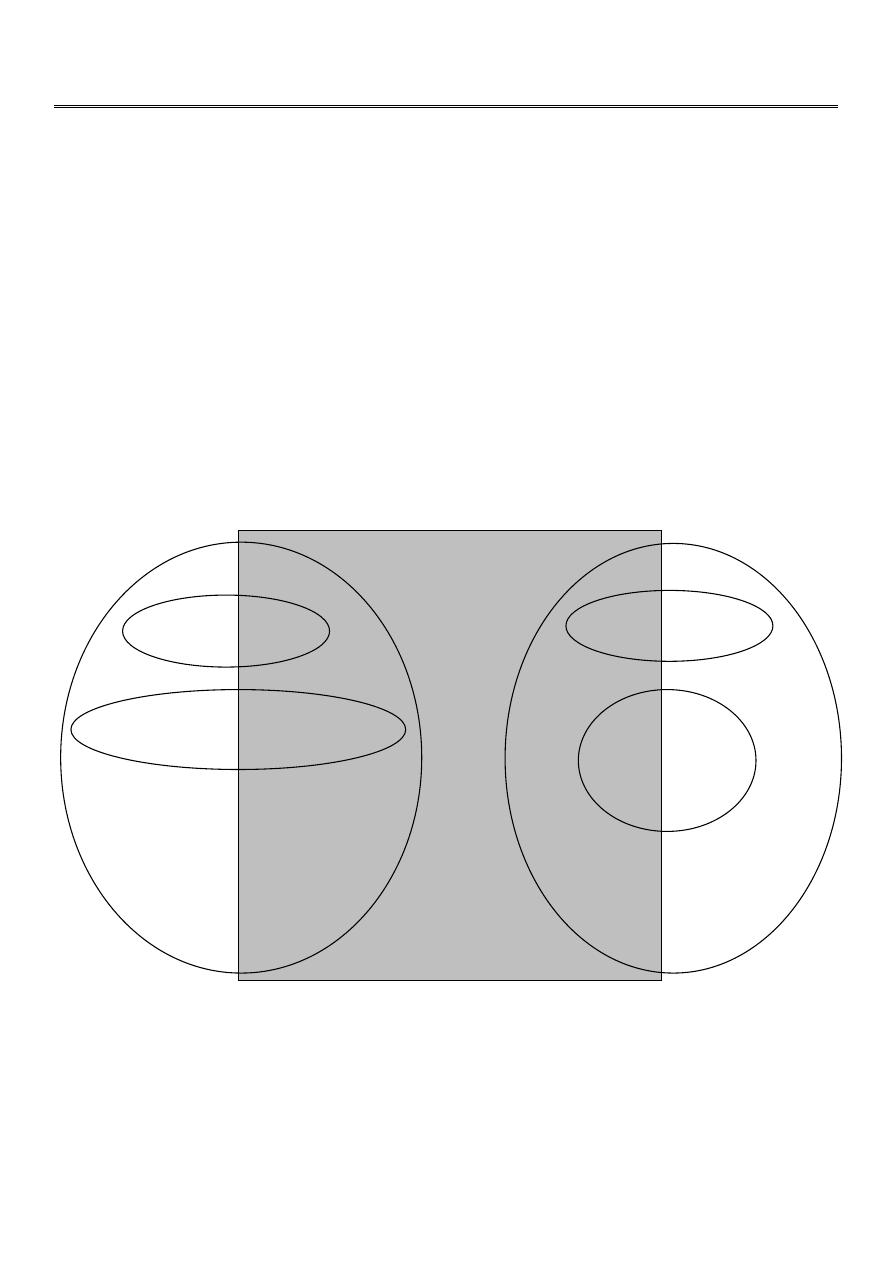
Psychosis
What is Psychosis?
Generic term
“Break with Reality”
Symptom, not an illness
Caused by a variety of conditions that affect the functioning of the brain.
Includes hallucinations, delusions and thought disorder
P
S
Y
C
H
O
S
I
S
“Functional” disorders
“Organic” mental disorders
Substance induced
Delirium
Dementia
Amnestic d/o
Mood disorders
Schizophrenia “spectrum” disorders
2
Differential Diagnosis
:
Workup of New-Onset Psychosis:
“Round up the usual suspects”
Good clinical history
Physical exam, ROS
Labs/Diagnostic tests:
Medical/surgical/ substance-induced:
Psychotic d/o due to GMC
Dementia
Delirium
Medications
Substance induced:
Amphetamines
Cocaine
Withdrawal states
Hallucinogens
Alcohol
Mood disorders:
Bipolar disorder
Major depression with psychotic features
Personality disorders:
Schizoid
Schizotypal
Paranoid
Borderline
Antisocial
Miscellaneous:
PTSD
Dissociative disorders
Malingering
Culturally specific phenomena:
Religious experiences
Meditative states
Belief in UFO’s, etc
Metabolic panel
CBC with diff
B12, Folate
RPR, VDRL
Serum Alcohol
Urinalysis
Thyroid profile
urine drug screen!!!
CSF/LP
HIV serology
CT or MRI
EEG

3
Talking Points:
Schizophrenia is not an excess of dopamine.
The differentiation between “functional” and “organic” is artificial.
Schizophrenia and other psychiatric illnesses are syndromes.
Definition:
The schizophrenic disorders are characterized in general by fundamental and
characteristic distortions of thinking and perception, and affects that are inappropriate
or blunted. Clear consciousness and intellectual capacity are usually maintained
although certain cognitive deficits may evolve in the course of time.
The most important psychopathological phenomena include:
1. thought echo
2. thought insertion or withdrawal
3. thought broadcasting
4. delusional perception and delusions of control
5. influence or passivity
6. hallucinatory voices commenting or discussing the patient in the third person
7. thought disorders and negative symptoms.
Talking Points:
1% prevalence
Early onset, M>F
Early, aggressive treatment decreases long-term problems
Multiple subtypes- catatonic, disorganized, paranoid, undifferentiated, residual

4
Schizophrenia Diagnostic features (1
st
Rank symptoms):
1950’s - Schneider’s 1st Rank Symptoms:
1.
Primary Delusion = ‘delusional percept’
2.
Own thoughts spoken aloud = ‘thought echo’
3.
Voices arguing or discussing
4.
running commentary voices
5.
thought withdrawal and/or thought block
6.
Thought insertion
7.
thought broadcasting (others are thinking it at the same time as you)
8.
Made to feel… ‘passivity of affect’
9.
Made to want… ‘passivity of impulse’
10. Made to do… ‘passivity of volition’
11. Done to my body ‘somatic passivity’ eg probed by aliens
Some may occur in illnesses other than schizophrenia eg mania
DSM-IV Diagnosis of Schizophrenia:
1. Psychotic symptoms (2 or more) for at least one month:
Hallucinations
Delusions
Disorganized speech
Disorganized or catatonic behavior
Negative symptoms
2. Impairment in social or occupational functioning
3. Duration of illness at least 6 mo.
4. Symptoms not due to mood disorder or schizoaffective disorder
5. Symptoms not due to medical, neurological, or substance-induced disorder

5
Formal Thought Disorders
Clinical features:
Neologisms
Tangentiality
Derailment
Loosening of associations (word salad)
Private word usage
Perseveration
Nonsequitors
Delusions
Clinical features:
Paranoid/persecutory
Ideas of reference
External locus of control
Thought broadcasting
Thought insertion, withdrawal
Jealousy
Guilt
Grandiosity
Religious delusions
Somatic delusions
Religious
delusions
Somatic
delusions
Hallucinations
Clinical features:
Auditory
Visual
Olfactory
Somatic/tactile
Gustatory
Behavior
Clinical features:
Bizarre dress, appearance
Catatonia
Poor impulse control
Anger, agitation
Stereotypies
Mood and Affect
Clinical features:
Inappropriate affect
Blunting of affect/mood
Flat affect
Isolation or dissociation of affect
Incongruent affect

6
Positive vs. negative symptoms:
Psychotic Disorders:
Onset
Symptoms
Course
Duration
Schizophrenia
Usually insidious
Many
Chronic
>6 months
Delusional
disorder
Varies
(usually insidious)
Delusion only
Chronic
>1 mo.
Brief psychotic
disorder
Sudden
Varies
Limited
<1 mo.
Psychosocial Factors:
Expressed emotion
Stressful life events
Low socioeconomic class
Limited social network
Some factors rejected as causal
“Schizophrenogenic Mother”
“Skewed” family structure
Genetic factors: (The evidence mounts…)
Monozygotic twins (31%-78%) vs dizygotic twins
4-9% risk in first degree relatives of schizophrenics
Adoption studies
Linkage, molecular studies
Positive symptoms
Delusions
Hallucinations
Behavioral dyscontrol
Thought disorder
Negative symptoms (Remember Andreasen’s “A”s)
Affective flattening
Alogia
Avolition
Anhedonia
Attentional impairment

7
Genetics of Schizophrenia:
The take-home message
Vulnerability to schizophrenia is likely inherited
“Heritability” is probably 60-90%
Schizophrenia probably involves dysfunction of many genes
Anatomical abnormalities:
Enlargement of lateral ventricles
Smaller than normal total brain volume
Cortical atrophy
Widening of third ventricle
Smaller hippocampus
Physiologic studies:
PET and SPECT
Generally normal global cerebral flow
Hypofrontality
Failure to activate dorsolateral prefrontal cortex (problem-solving, adaptation, coping
with changes)
Biochemical factors:
The dopamine hypothesis
All typical antipsychotics block D
2
with varying affinities
Dopamine agonists can precipitate a psychosis
o
Amphetamines
o
Cocaine
o
L-dopa
8
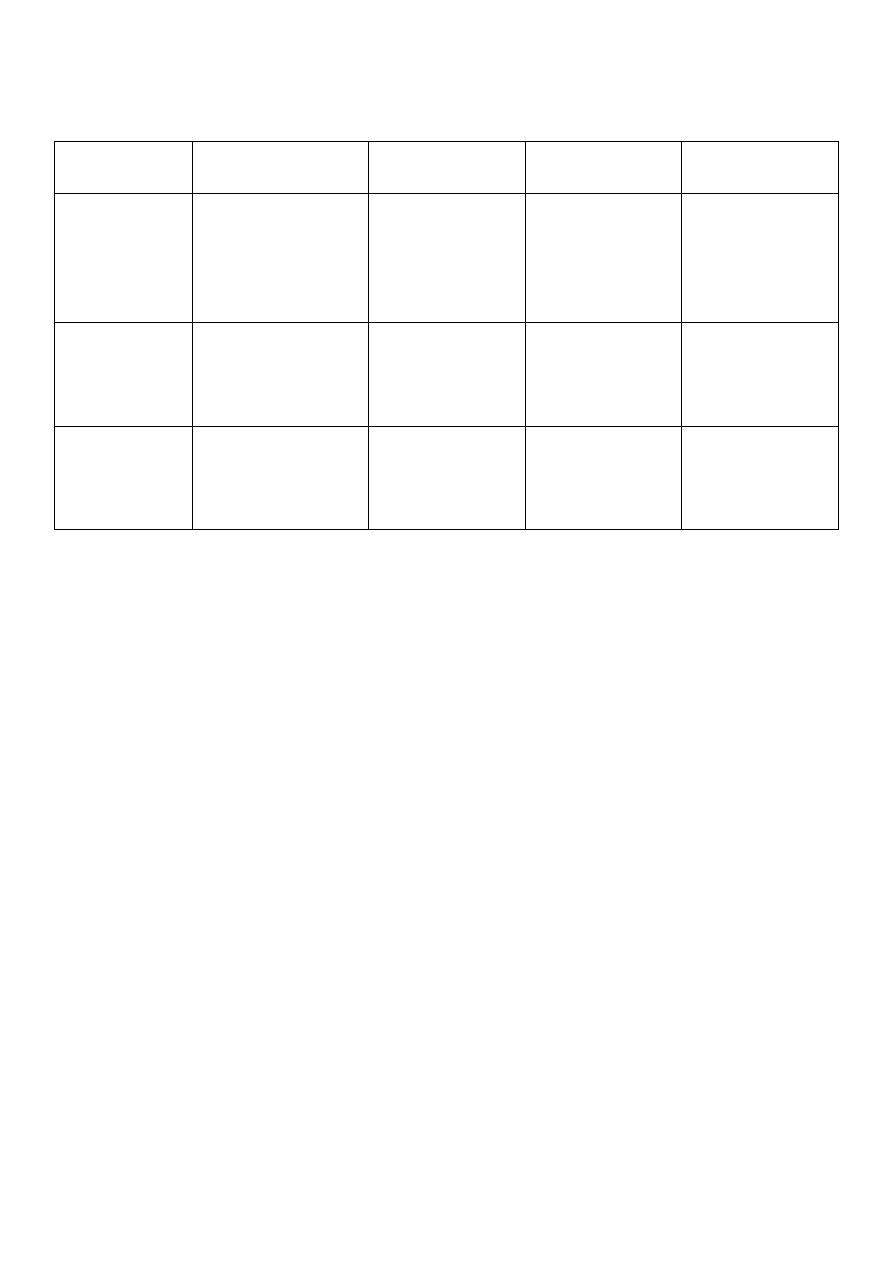
Dopamine systems:
Cell bodies
Projections
Function
Clinical
implications
Nigro-striatal Substantia nigra
Caudate and
putamen
Movement
Extrapyramidal
symptoms,
dystonias,
Tardive
dyskinesia
Meso-limbic
Ventral
tegmentalarea,
subst. nigra
Accumbens
amygdala
olfactory
tubercle
Emotion, affect,
memory
Positive
symptoms
Meso-cortical Ventral tegmental
area
Prefrontal
cortex
Thought,
volition,
memory
Blockade here
can worsen
negative
symptoms
Typical Neuroleptics
Neuroleptic (typicals) Side effects:
1.
Acute dystonia
2. Parkinsonian side effects (EPS)
3. Akathisia
4. Tardive dyskinesia
5. Sedation, orthostasis, QTC prolongation, anticholinergic, lower seizure threshold,
increased prolactin
Low potency:
o Chlorpromazine
o Thioridazine
o Mesoridazine
High potency:
Haloperidol
Fluphenazine
Thiothixene
Loxapine (mid)
High potency:
o Haloperidol
o Fluphenazine
o Thiothixene
o Loxapine (mid)

9
Atypical Antipsychotics:
Risperidone
Olanzapine
Quetiapine
Clozapine
Ziprasidone
Aripiprazole (new-partial DA agonist)
Atypical antipsychotics:
Broader spectrum of receptor activity (Serotonin, dopamine, GABA)
May be better at alleviating negative symptoms and cognitive dysfunction
Clozaril (clozapine) associated with agranulocytosis, seizures
Atypical Antipsychotics (Side Effects):
1. Sedation
2. Hyperglycemia, new-onset diabetes
3. Anticholinergic effects
4. Less prolactin elevation
5. QTC prolongation
6. Some EPS
7. Increased lipids
Psychosocial Treatment:
Education, compliance #1
Hospitalize for acute loss of functioning
Outpatient treatment is rehabilitative
Psychoanalysis, exploratory therapies have limited value
Families should be involved
