Schistosomiasis
By
Dr. Ameer kadhim Hussein
M.B.Ch.B. FICMS (Community
Medicine)
Schistosomiasis (also known as bilharzia or snail fever)
is a collective name of parasitic disease caused by several
species of trematodes belonging to the genus Schistosoma.
Snail serve as the intermediary agent between
mammalian hosts.
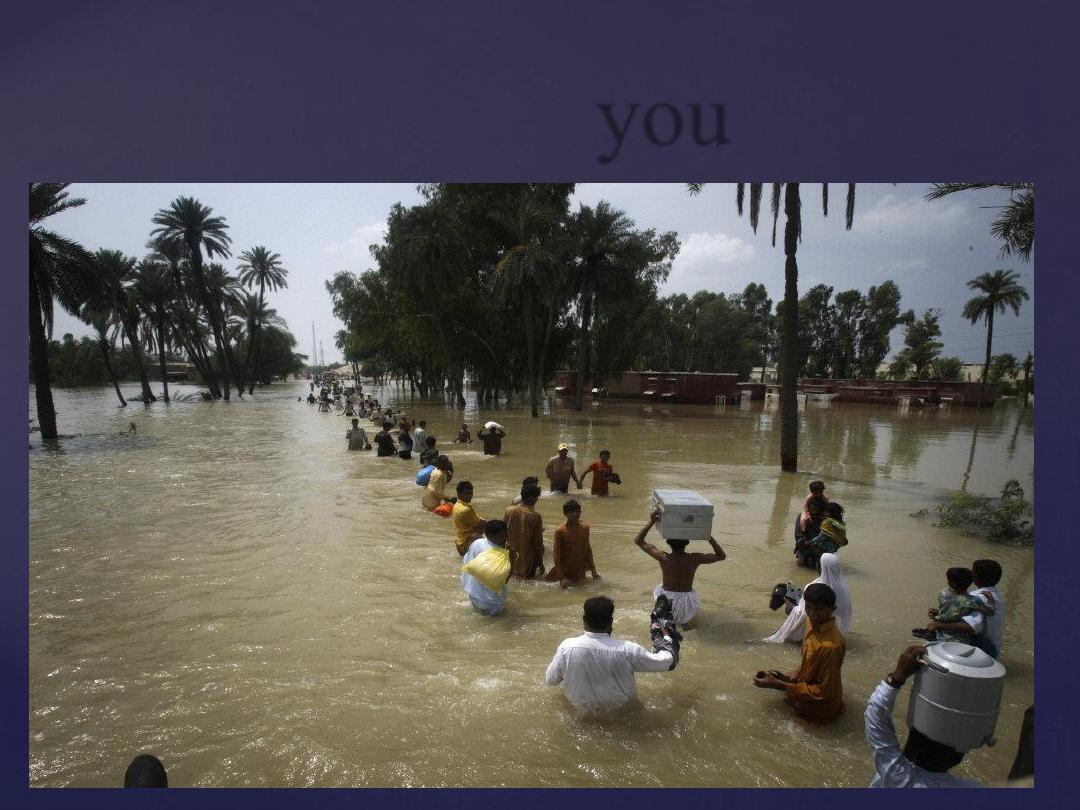
Individuals within developing countries who cannot afford
proper water and sanitation facilities are often exposed to
contaminated water containing the infected snails.
Schistosomiasis (Bilharzia)
Although it has a low mortality rate, schistosomiasis
often is a chronic illness that can damage internal
organs and, in children, impair growth and cognitive
development.
The urinary form of schistosomiasis is associated
with increased risks for bladder cancer in adults.
Schistosomiasis is the second most
socioeconomically devastating parasitic disease
after malaria.
Schistosomiasis (Bilharzia)
Schistosomiasis is known as bilharzia or bilharziosis in
many countries after German physician Theodor Bilharz
who first described the cause of urinary schistosomiasis
in 1851.
The first doctor who described the entire disease cycle was
Piraja da Silva in 1908.
It was a common cause of death for
Ancient Egyptians in the Greco-
Roman Period.
Later on disease seen in Japan, called
Katayama fever.
History
Schistosomiais is prevalent in tropical and sub-
tropical areas, especially in poor communities
without access to safe drinking water and
adequate sanitation.
It is estimated that at least 90% of those
requiring treatment for schistosomiasis live in
Africa.
There are two major forms of schistosomiasis
(intestinal and urogenital).
Epidemiology
Types
Species
Geographical distribution
Intestinal
schistosomiasis Schistosoma mansoni
Africa, the Middle East, the
Caribbean, Brazil, Venezuela and
Suriname
Schistosoma japonicum China, Indonesia, the Philippines
Schistosoma mekongi
Several districts of Cambodia and
the Lao People’s Democratic
Republic
Schistosoma guineensis
and related S.
intercalatum
Rain forest areas of central Africa
Urogenital
schistosomiasis
Schistosoma
haematobium
Africa, the Middle East, Corsica.

Reservoir
Species
Humans.
S. Haematobium
Mainly humans but also
reported in rodents.
S. Mansoni
Humans and domestic
animals like (dogs and cats)
and wild rodents.
S. japonicum
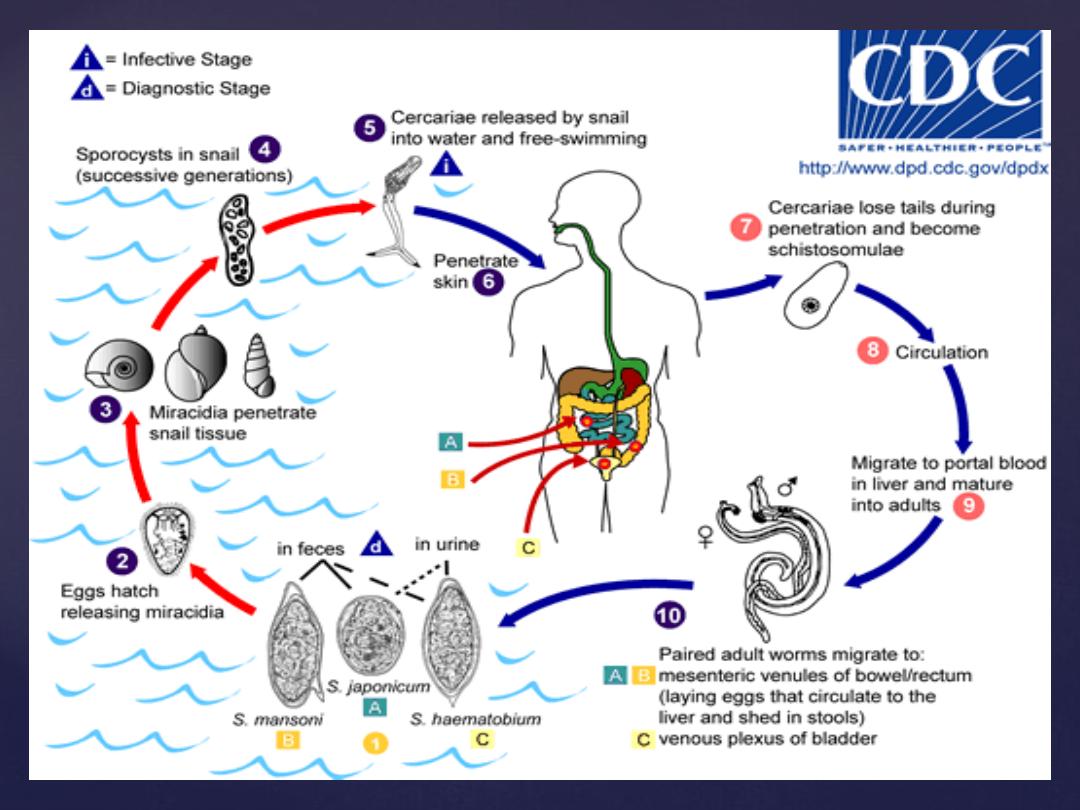
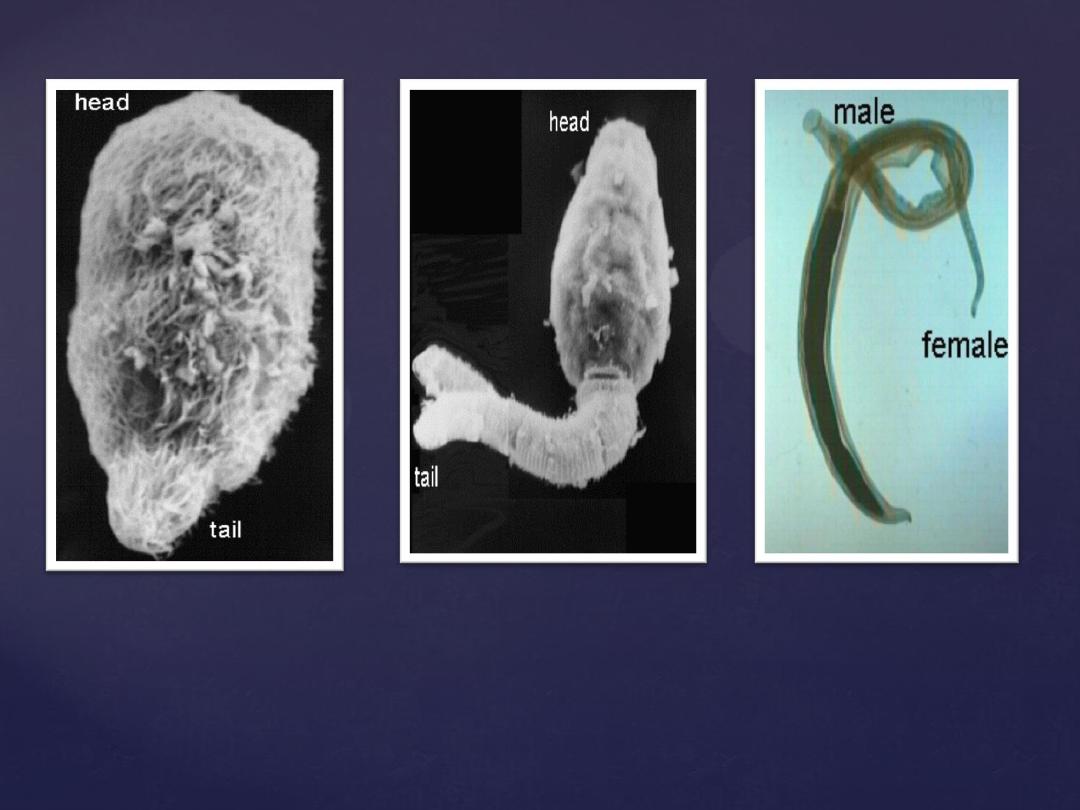
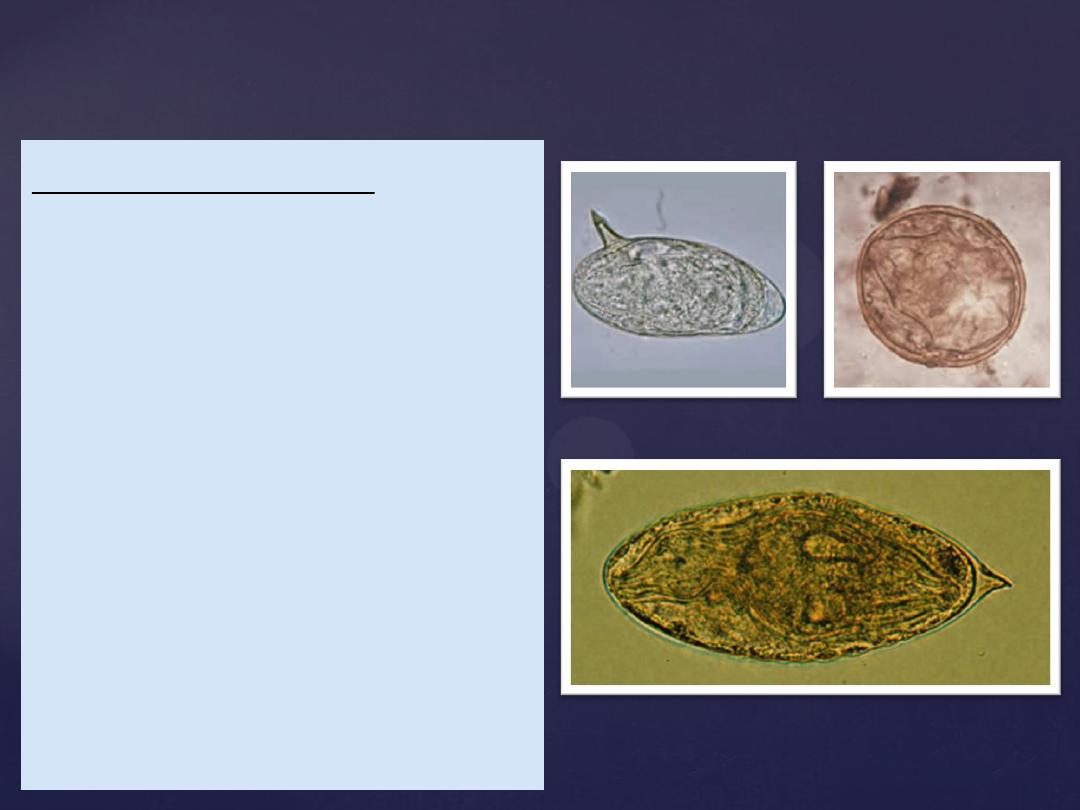
Miracidia larva with cilia
Paired male &
female
Cercariae with forked tail
A. For urinary schistosomiasis:
Suspected case: Visible hematuria or positive reagent strip
for hematuria
Confirmed case: eggs of S. haematobium in urine.
B. For intestinal schistosomiasis:
Suspected case: non specific abdominal symptoms,
blood in stool, hepatosplenomegaly.
Confirmed case: Presence of eggs in the stool.
WHO case definition in endemic area
Incubation period:
Acute systemic manifestation ( katayama fever) including
fever, urticaria, malaise and diarrhea may occur 2-6 weeks
after exposure which immediately preceding and during
initial egg deposition. This manifestation is un common but
can occur with S. haematobium.
Period of communicability:
Not communicable from one person to another. Persons
with S. may spread infection as long as excrete the eggs in
urine or stool to water bodies. It last in excess of 10 years in
S. haematobium and S. Mansoni. Infected snail persist in
release cercariae as long as they live (several weeks to
about 3 months).

Susceptibility:
is universal. Any immunity developing as result
of infection is variable and not yet fully
investigated.

Symptoms are related to the number and location of the
eggs in the human host. Intestinal S
.
(
mansoni and
japonicum
) give rise to hepatic and intestinal pathology
and symptoms include diarrhea, abdominal pain and
hepatosplenomegaly.
S. japonicum can cause CNS disease with seizures.
S. haematobium
give rise to urinary manifestations and
Symptoms include dysuria, frequency and hematuria at
end of urination. CNS disease rarely been reported.
Clinical manifestations
In intestinal forms:
1
. Liver fibrosis.
2. Portal hypertension.
3. Colorectal malignancy.
In urinary forms:
1. Obstructive uropathy and superimposed bacterial infection.
2. Infertility.
3. Bladder cancer.
Egg can also deposited at ectopic sites including the brain,
spinal cord, skin, pelvis and vulvo-vaginal areas.
Swimmer’s itch:
it is type of dermatitis occur when S. larvae
penetrate the human skin.
Complication
Diagnosis
Microscopic Detection
Demonstration of eggs in stool
or urine sample.
S. haematobium
eggs are oval
and have a spike at the tip.
S. japonicum
eggs small and
almost spherical with tiny
spine.
S. mansoni
eggs have a spike
on the side
.
Immunological tests including
ELISA and IFA are useful in
diagnosis.
S. mansoni
S.
japonicum
S. haematobium
Praziquantel is drug of choice in treatment of
Schistosomiasis.
Praziquantel extremely well tolerated with few side effects.
It is broad-spectrum anti-helminthic drug cures
schistosomiasis in 80–90% of patients with 90% reduction
in egg excretion in those not cured. Resistance has been
reported in Egypt and Senegal.
Others:
Metrifonate against
S. haematobium.
Niridazole against
S. japonicum.
Oxamniquine against
S. mansoni.
Treatment
Swimmer’s itch and Katayama Fever are usually
treated symptomatically.
Drugs ineffective when fibrosis has developed,
treatment is then focused on managing the
complications (e.g. portal hypertension).
Anticonvulsants may be needed in patients with
CNS complications (
S. japonicum
).
Treatment
A. Preventive measures:
1. Treat patients in endemic areas with praziquantel to
relieve suffering and prevent disease progression.
Regularly treat high risk groups such as school age
children, women of childbearing age and special
occupational groups in endemic areas with presumptive
curative doses.
2. Educate the public in endemic areas to seek treatment
early and regularly and to protect themselves.
3. Dispose of feces and urine so that viable eggs will not
reach bodies of freshwater containing intermediate snail
hosts.
Methods of controls

4. Improve irrigation and agriculture practices reduce snail habitats
by removing vegetation or by draining and filling or by lining canals
with concrete.
5. Treat snail breeding sites with molluskicides. Cost may limit the
use of these agents.
6. Individual protection: prevent exposure to contaminated water by
wearing rubber boots. To minimize cercarial penetration after
accidental water exposure dry skin and apply 70% alcohol
immediately to the skin to kill surface cercariae.
7. Provide water for drinking, bathing and washing clothes from
sources free of cercariae or treated to kill them. Effective measures
for inactivating cercariae include water treatment with iodine or
chlorine. Allowing water to sand 48-72 hours before use is also
effective.
8. Travelers visiting endemic areas should be advised of the risks
and informed about preventive measures.
B. Control patient, contacts and immediate
environment :
1.Report to local health authorities.
2.Isolation, quarantine, immunization of contacts: Not applicable.
3. Concurrent disinfection: Sanitary disposal of feces and urine.
4. investigation of contacts and source of infection: Examine
contacts for infection from a common source.
5. Specific treatment: Praziquentel is drug of choice for all
species. Alternative drugs are oxamniquine for
S. mansoni
and
metrifonate for
S. haematobium
.
1. Examine for schistosomiasis and treat all infected
especially those with moderate to heavy intensity of
infection (children).
2. Provide clean water, avoid water contamination and
warn people about risk of contact with contaminated
water.
3. Treat areas that have high snail density with
molluskicides.
Epidemic measures
Thank
you
