Ischemic and rheumatic heart diseases
Dr. Ameer kadhim Hussein
M.B.Ch.B. FICMS
Ischemic heart diseases
In most western countries, 30% of all deaths in men,
25% in women are caused by IHDs.
Case fatality rate = 25–28% within 28 days (and 55%
within first hour). It eats about 3.4–9.4 years of life
expectancy of men, and even greater for women.
IHDs are a 'modern epidemic', one spread not from
person to person but due to a lifetime of bad habits.
After sweeping the developed countries, CHD is on
the decline (although still very prevalent) there, while
affecting more the developing countries.
Ischemic heart diseases
The ischemic heart diseases have a kind of ‘incubation
period’ of 10 years, i.e.the lag period between
behavioral change and onset of disease.
Risk factors of IHD
Risk factors of IHD
• Smoking.
• Hypertension (BP > 140/90 or any body on
antihypertensive drugs) .
• HDL < 40 mg/dl.
• Diabetes mellitus.
• Family history of IHD.
• Age (men > 45 years, women > 55 years).
• Obesity (BMI > 30), physical inactivity.
• Alcohol > 75 g/day.

Risk factors of IHD
Risk factors of IHD
• Male sex/ postmenopause/OCP intake.
• Type A personality.
• Lack of dietary fibers, high cholesterol diet, too soft
water, deficiency of polyunsaturated fatty acids, too
much salt.
Dyslipidemia
Of all lipids, LDL cholesterol is most directly related
to IHD. Current recommendation is to screen for
blood lipids in all adults over 20 years. The screen
should include a fasting lipid profile (total cholesterol,
triglycerides, LDL cholesterol and HDL cholesterol)
repeated every 5 years.
Apo B and Apo A are probably better indicators than
the lipoproteins themselves. Lipid goal. HDL > 45
mg/dl; LDL < 160 mg/dl; total cholesterol / HDL <
3.5.
Smoking
Smoking is an important, but reversible risk factor.
Smoking cause atherogenesis by releasing carbon
monoxide and ↑ sympathetic tone.

Hypertension
Hypertension
Is the strongest risk factor for IHD. CVD risk doubles for
every 10 mm Hg increase in DP or 20 mm Hg increase in
SP.
DM
Diabetes mellitus, insulin resistance and the metabolic
syndrome
Most patients of diabetes mellitus die from atherosclerosis
and its complications. The abnormal lipoprotein profile
associated with insulin resistance, known as ‘diabetic
dyslipidemia’, accounts for part of elevated cardiovascular
risk in patients with Type II diabetes.
DM
While diabetic patients often have LDL cholesterol
near average, the LDL particles are smaller, denser
and more atherogenic. There are also low HDL and
high triglycerides.
Hypertension often accompanies diabetes and indeed,
this cluster of risk factors is now known as the
‘metabolic syndrome’.
Diabetes mellitus may also cause ‘silent’ AMI. The
target is to keep sugar under 120 mg/dl at all times and
BP < 130/85.
Metabolic syndrome
The metabolic syndrome is any three risk factors of
the following:
• Abdominal obesity (waist circumference): Men >
102 cm, women > 88 cm.
• BMI > 30.
• Triglycerides > 150 mg/dl.
• HDL cholesterol: Men < 40, women < 50.
• Blood pressure > 130 or > 85 mm.
• Fasting glucose > 110 mg/dl.
Others
Male sex/postmenopausal state
Decades of observational studies have verified excess
coronary risk in men compared with premenopausal
women.
After menopause, both become equal. In this regard,
estrogen has been found to increase HDL and reduce
LDL.
Dysregulated coagulation or fibrinolysis.

Prevention
• Primordial prevention
1. Preserve traditional food habits, implement 'dietary
goals‘.
2. Avoid initiation of smoking, fast foods, colas and
candies. Schools play the most important role in
primordial prevention.
• Primary prevention (for every body in population)
1. Prudent diet (rich in fruits and vegetables)
2. Abstinence from smoking and alcohol.
3. Control of stress and hypertension.
Prevention
• Secondary prevention (for those with risk factors)
Screening for hypertension, hypercholesterolemia,
diabetes and medical management of such diseases.
Screening is recommended each 5 years in all adults
over 20 years.
• Tertiary prevention
Include lifelong β blockers and Aspirin, angioplasty.
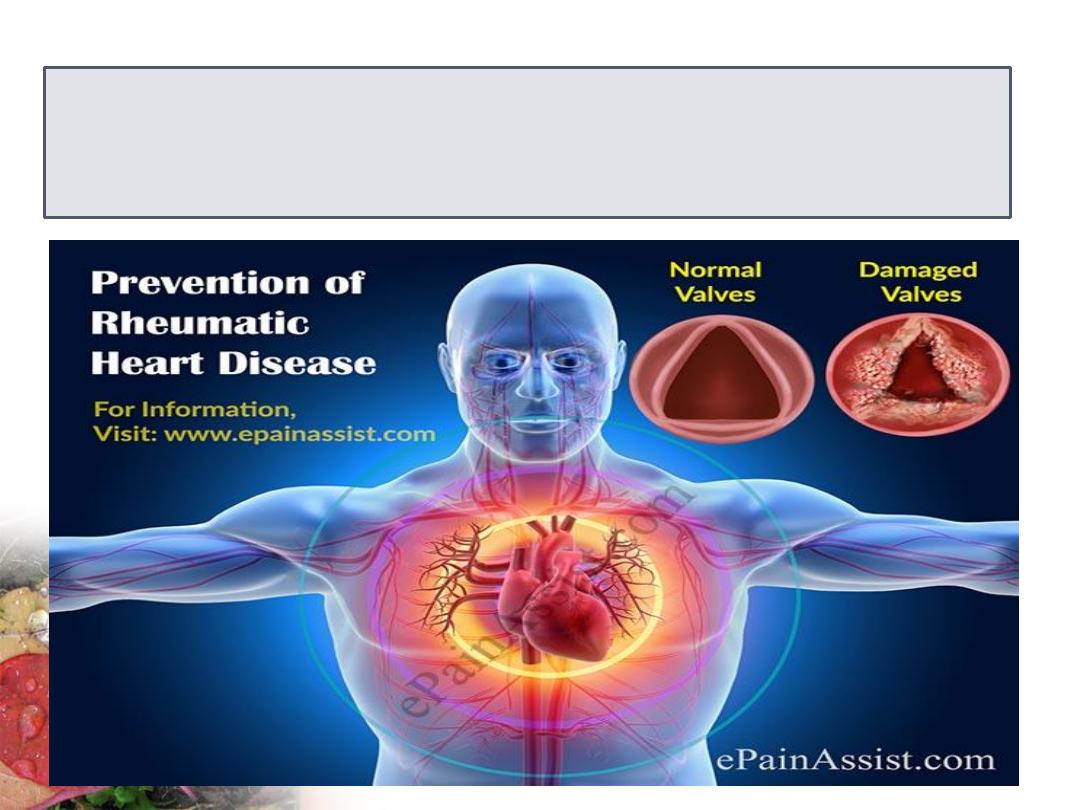
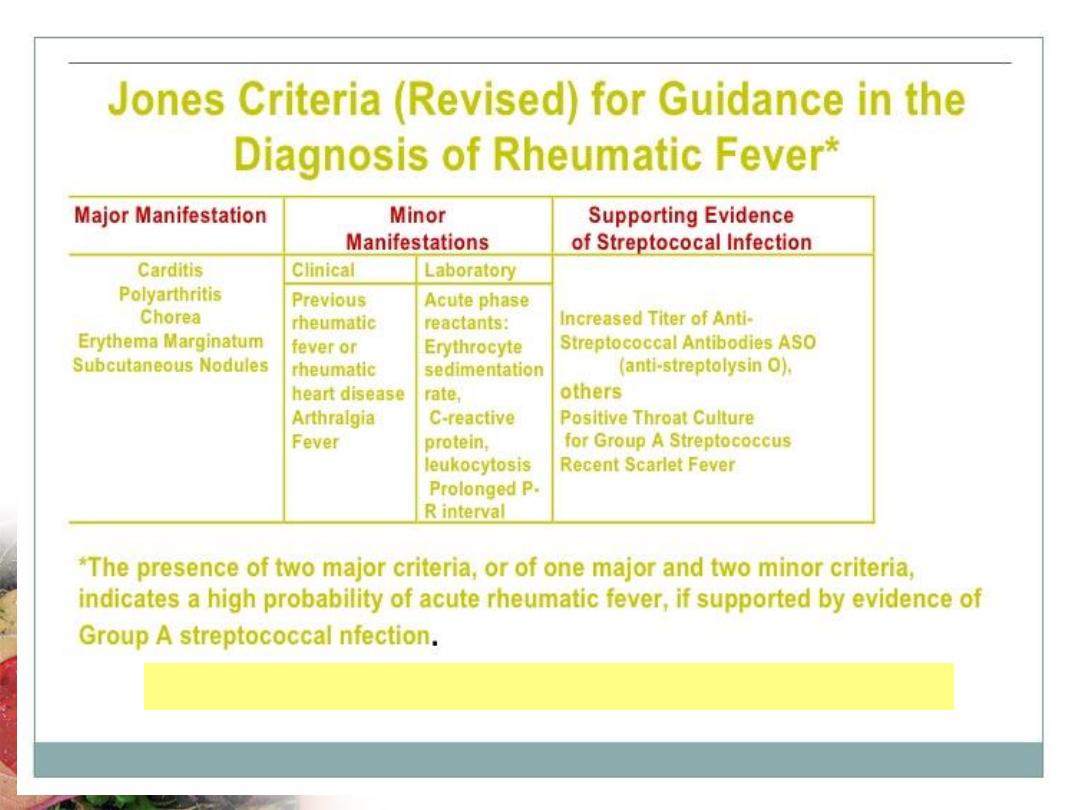
RHEUMATIC HEART DISEASE
Introduction
Rheumatic heart disease (RHD) is the ultimate, sequelae and
crippling stage of rheumatic (Rh) fever, which in turn is the
result of streptococcal pharyngitis.
Rheumatic fever is an acute febrile disease, affecting the
connective tissues particularly in the heart and joints, which
occurs following the infection of throat (pharynx) by group A
beta-hemolytic streptococci. Thus although Rh fever is a non
communicable disease, it results from communicable pharyngitis.
About 20 percent of all sore throats among children are due to
streptococcal infection and of these about 2 percent result in
rheumatic fever. Almost 80 percent of those who get Rh fever,
end up with Rh heart disease.
Introduction
RHD is the late sequel of Rh fever, which in turn is the
result of the infection of tonsils, pharynx, adenoids, etc.
caused by Group A, β-hemolytic streptococci (also
called S. pyogenes). Reservoir of infection include all
the cases and the carriers of streptococcal pharyngitis.
Among the carriers, both temporary and chronic carrier
state occurs.
Cases of strep. pharyngitis are at a greater risk of
developing Rh. fever than the carriers. Incidence is
maximum among school children, in the age group of 5
to 15.It is equal in both the sexes.
Immunity
There has been an immunological basis for the
development of Rh fever and RHD.
According to toxic immunological hypothesis,
the streptococci have certain toxic products
leading to immunological process, resulting in
Rh fever.
Another concept is that it requires repeated
exposure to precipitate the illness. Another
belief is that RHD is an autoimmune disease.
Predisposing factors
Rh fever and RHD is considered as ‘Social disease’, because
many social factors are responsible for the prevalence of this
disease such as poverty, poor housing, undernutrition, illiteracy,
ignorance, large families, over crowding, etc.
Prevalence declines sharply as the standard of living improves.
Recommendations of the American Heart Association

Prevention of Rheumatic Fever and
Rheumatic Heart Disease
Health Promotion
Measures necessary for primordial prevention are:
• Improvement in the living conditions.
• Improvement of sanitation in and around the house.
• Prevention of overcrowding.
• Prevention of malnutrition among children.
• Improvement in the socioeconomic condition.
• Health education of the people regarding dangers of
sore throat.
• ‘Health-Fair’ should be conducted in the schools to
make the children health conscious.
Specific Protection
• No vaccine is available.
• Chemoprophylaxis of the contacts of a case of
pharyngitis or scarlet fever with Benzathine penicillin.
• ‘Secondary prophylaxis’ is given for all cases of Rh
fever to prevent RHD with 1.2 million units of
Benzathine Penicillin, once in 3 weeks, regularly for 5
years or until the age of 18 years. If they have
developed RHD, prophylaxis is continued for life.
Early Diagnosis and Treatment
• By conducting periodical ‘School health
survey’, to detect the cases of sore throat.
• By surveillance of ‘high-risk’ groups such as
slum dwellers.
• Detected cases of sore throat (or acute
pharyngitis) are treated by 1 dose of 1.2 million
units of Benzathine penicillin, a long acting
one. This essentially prevents the subsequent
development of Rh fever and RHD.
Disability Limitation and
Rehabilitation
This consists of limiting the development of disability in an
individual who has already developed RHD. This consists of
giving intensive treatment with Aspirin for joint pains and
prednisolone for carditis, life long Benzathine Penicillin, 1.2
million units, once in 3 weeks and Balloon valvotomy or valve
replacement. Rehabilitation by social, vocational and
psychological measures of those who are suffering from RHD.